Executive summary
Unavoidable pressures from winter viruses mixed with six days of industrial action inevitably impacted urgent and emergency care (UEC) in January, however the NHS was able to manage demand.
There were 99,529 core general and acute beds available in January, meaning the NHS successfully delivered on the UEC recovery plan ambition to open an additional 5,000 core beds.
Ambulance services answered 828,345 calls to 999 in January 2024, or 26,721 per day, which was 22% more than in January 2023.
The NHS has continued to make progress in reducing long waits for patients in December. That month, 1,254,166 patients started treatment, an increase of 3% from the same point last year. The number of patients who were waiting more than 65 weeks for treatment is down by 41% compared to the same month last year.
The total waiting list reduced for a third consecutive month. As of the end of December, there were 7.60 million waits for procedures and appointments and an estimated 6.37 million people waiting for care.
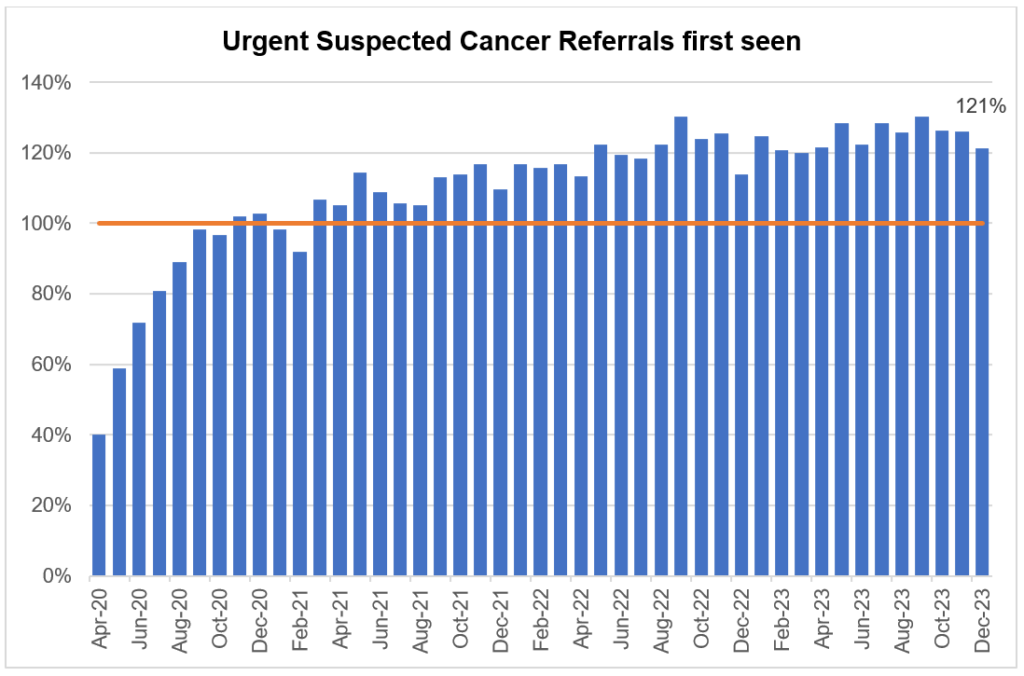
Demand for cancer services continued at record levels in December with the number of urgent suspected cancer referrals at 121% of pre-pandemic levels. To meet high demand, treatment is also at record levels and there has been a reduction in the 62-day cancer backlog as a result.
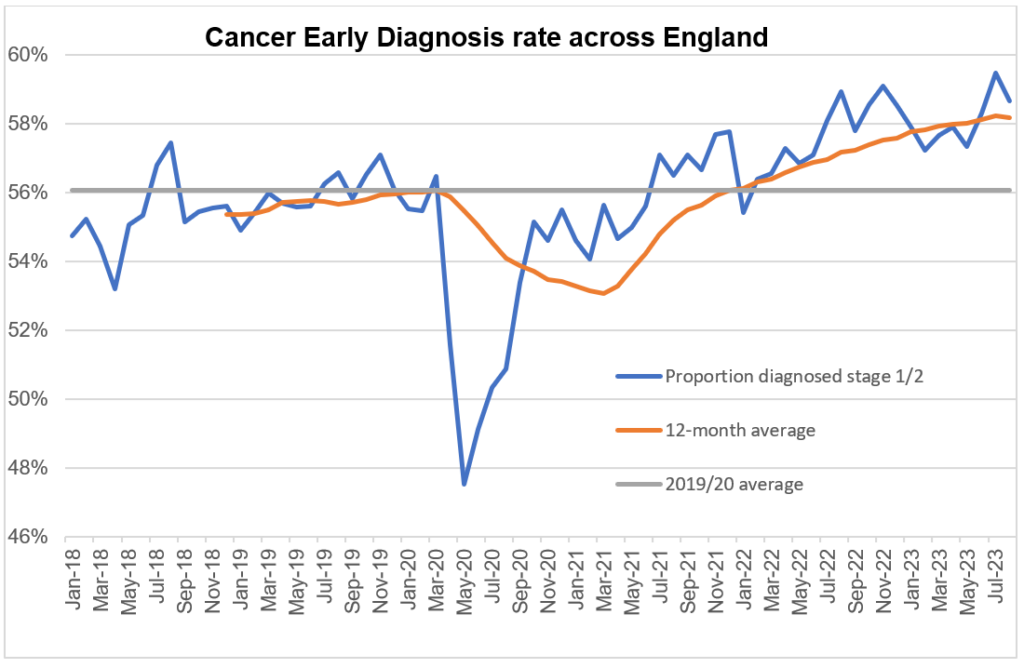
Over 336,000 people received treatment for cancer over the last year between January 2023 and December 2023 – the highest year on record, and up by more than 23,000 on the same period pre-pandemic. We are diagnosing a higher proportion of cancers at an early stage now than ever before. Survival is also at an all-time high.
More people than ever before now receive NHS support for their mental health, with almost five million patients accessing care in 2022/23, an increase of more than one million compared to 2016/17.
Urgent and emergency care
Unavoidable pressures from winter viruses mixed with six days of industrial action inevitably impacted urgent and emergency care (UEC) in January. However, despite sustained challenges on services, and thanks to staff working to boost capacity, the NHS was able to manage demand.
There were 99,529 core general and acute beds available in January, meaning the NHS successfully delivered on the UEC recovery plan ambition to open an additional 5,000 core beds.
Ambulance services answered 828,345 calls to 999, or 26,721 per day, which was 22% more than in the same period last year. They handled 755,276 incidents.
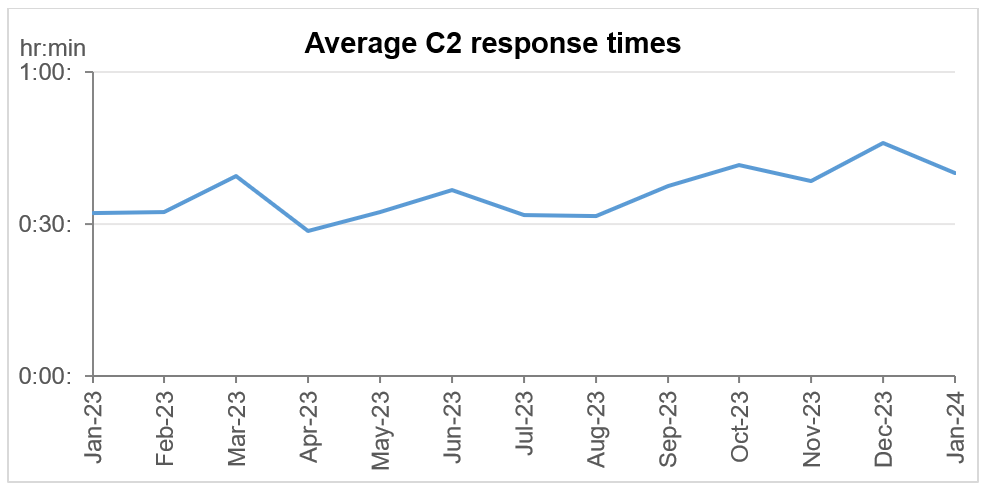
The average ambulance response time for a category 2 call was 40 minutes and 6 seconds. This is 5 minutes and 51 seconds faster compared to December 2023.
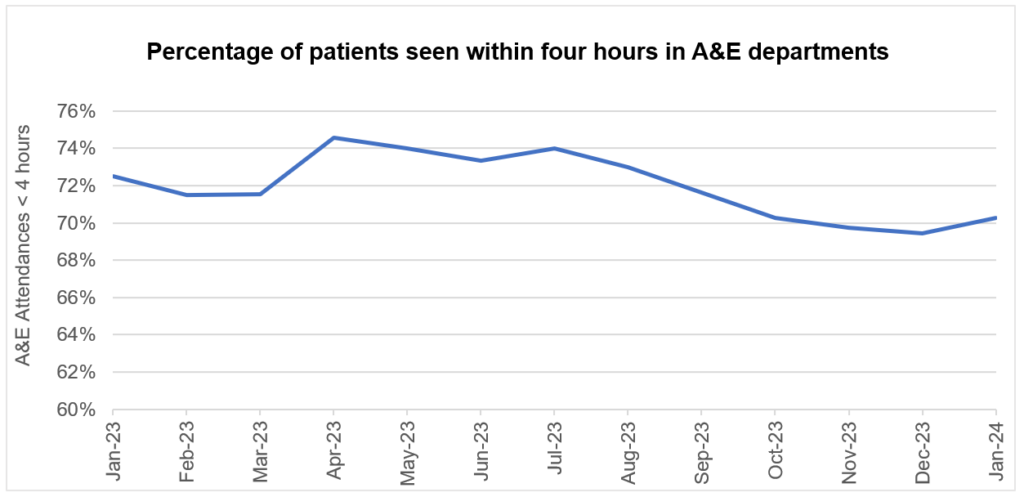
There were 2,225,035 attendances at A&Es across England, an average of 71,775 per day. This is 13% higher than in January 2023. 70.3% of patients attending A&E were admitted, transferred or discharged within four hours. This compares to 69.4% in December 2023
Elective recovery
The NHS made progress in reducing long waits for patients in December. This is despite staff dealing with widespread disruption from three days of industrial action, ending two days before Christmas, and winter demand.
1,254,166 patients started treatment, an increase of 3% from the same point last year.
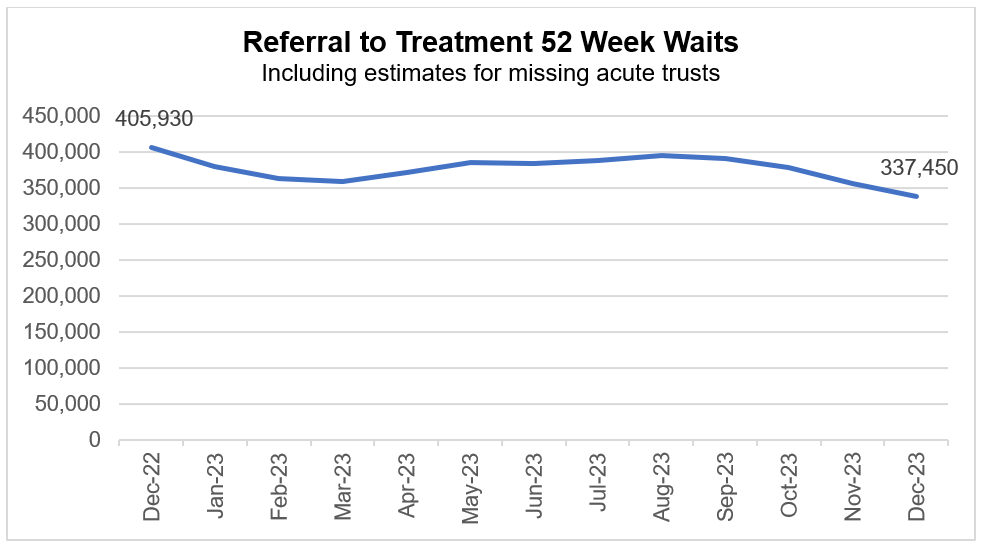
As of the end of December, 337,450 (4%) patients were waiting more than 52 weeks for treatment. This is down from 355,412 (5%) in November and down by 17% compared to the same month last year (405,930 patients were waiting more than 52 weeks for treatment in December 2022).
98,374 (1%) patients were waiting more than 65 weeks for treatment. This is down by 41% compared to the same month last year (166,201 patients were waiting more than 65 weeks for treatment in December 2022).
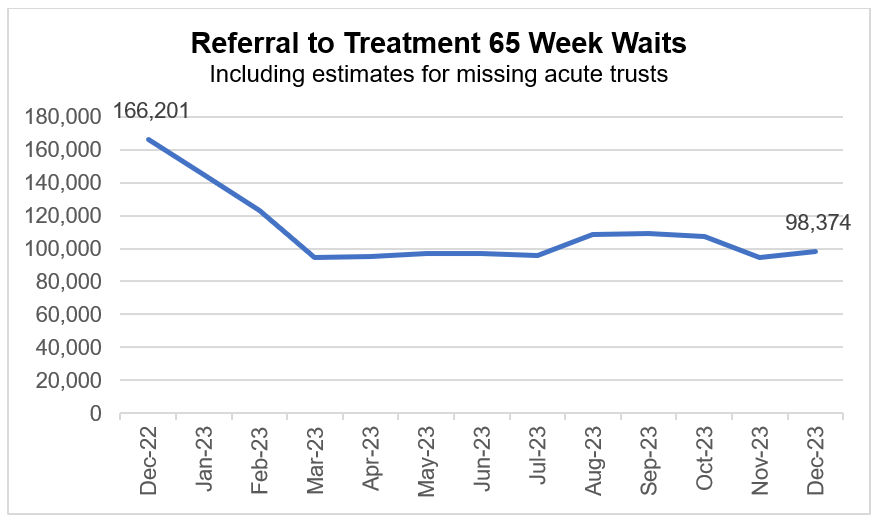
The total waiting list reduced for a third consecutive month. As of the end of December, there were 7.60 million waits for procedures and appointments and an estimated 6.37 million people waiting for care.
Cancer
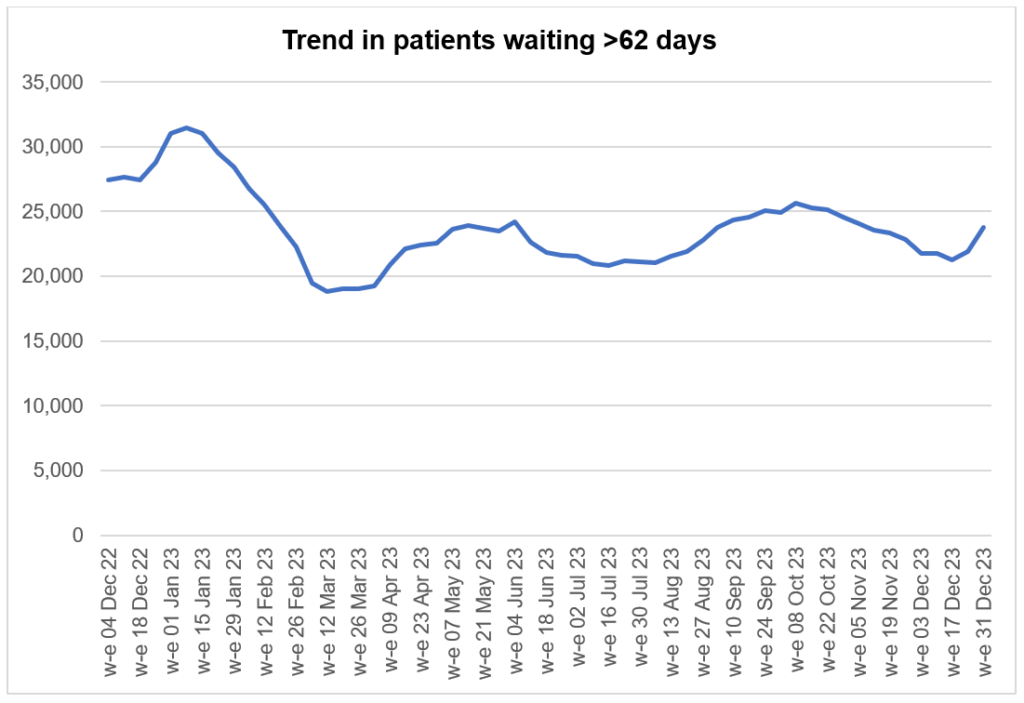
Demand for cancer services continued at record levels in December with the number of urgent suspected cancer referrals at 121% of pre-pandemic levels. To meet high demand, treatment is also at record levels and there has been a reduction in the 62-day cancer backlog as a result.
Over 336,000 people received treatment for cancer over the last year between January 2023 and December 2023 – the highest year on record, and up by more than 23,000 on the same period pre-pandemic.
GPs have been referring people for urgent cancer checks in record numbers since March 2021. Since then, NHS staff have seen over a million more people than in the same period prior to the pandemic. The increase in referrals has contributed to the NHS diagnosing more cancer at an early stage than ever before. We are diagnosing a higher proportion of cancers at an early stage now than ever before – about 2% higher than before the pandemic. Survival is also at an all-time high. In 2023, the Annals of Oncology published findings showing that cancer deaths are around 10% lower in the UK compared to just 5 years ago.
The NHS is working hard to keep up with this increase in demand. It has been accelerating the installation of new diagnostic capacity, much of it in Community Diagnostic Centres. The backlog has already reduced over 10,000 people since its peak last summer, and despite the recent seasonal increase, NHS staff remain focused on ensuring that people who have been waiting longest or who need care most urgently are seen first.
Mental health
More people than ever before now receive NHS support for their mental health, with almost five million patients accessing care in 2022/23, an increase of more than one million compared to 2016/17.
For the period October 2023 to December 2023 3,537 people were counted as starting treatment on the EIP pathway, of whom 71.3% were seen within two weeks. The national RTT element of the access and waiting time standard for EIP services is therefore being met, exceeding the target of 60% of people starting treatment on the EIP pathway within two weeks. This standard has been continuously exceeded since the introduction of the 60% target in 2020.
Longer periods of mental health inpatient care are a key factor in systems needing to place people in out of area placements. These are in turn linked to the bed pressures that inpatient mental health services have experienced in recent years. The two metrics below focus on long length of stay in adult acute mental health inpatient settings. They mirror Long Term Plan priorities for mental health, which aim to drive a reduction in long lengths of stay in hospital for working-age adults and older adults. Data for December 2023 shows:
- Between October 2023 to December 2023, there were 9.5 people per 100,000 population in England aged between 18-64 with a length of stay of 60 days or more, which is 1.5 more than for October 2022 to December 2022 (8).
- Between October 2023 to December 2023 there were 11 people per 100,000 population in England aged 65 or over, with a length of stay of 90 days or more, which is the same as for October 2022 to December 2022.
The current threshold for both metrics is 8 people per 100,000 population. Services are committed to improving the situation to align with or below the national threshold, which will be a key focus for action in 24/25.