Executive summary
1. Pressure has continued in emergency departments across the country, with 2.1 million attendances and 524,000 emergency admissions in August 2023. Ambulance services also faced an extremely busy month but response times for both category one and category two incidents improved on July 2023.
2. Continuing industrial action in the NHS has had a significant impact on patients, with almost 400,000 appointments having to be rescheduled during June, July and August 2023 as a result of strikes by junior doctors, consultants, dentists and radiographers.
3. Despite disruption caused by strikes, NHS staff are working hard to reduce the longest waits for care. In August 2023, there were 7,289 waiting more than 78 weeks, down by almost 85% from a peak of 124,911 in September 2021.
4. The NHS continues to increase support to those outside of hospital. Urgent Community Response helps avoid hospital admissions by providing urgent care to people in their homes. Integrated care boards (ICBs) now have full coverage and the latest data shows that nationally 84% of patients were seen within the 2-hour standard, with every region exceeding or meeting the 70% target in the Planning Guidance.
5. In diagnostics, the NHS has increased community access and overall activity levels, and in July, more than 2.2 million tests and checks were carried out. Over the past 12 months (August 2022 – July 2023) more than 25.3 million checks and scans have been carried out.
6. Demand for cancer services continued at record levels in July 2023, with the number of urgent suspected cancer referrals at 130% of pre-pandemic levels. Treatment is also at record levels and cancer deaths are around 10% lower in the UK compared to just 5 years ago.
7. Good progress continues to be made in activity levels in general practice. In July 2023, 27.8 million GP appointments took place. 43.6% of appointments in June took place on the same day that they were booked, and 68.3% were carried out face to face.
8. The NHS continues to expand mental health services to meet rising demand. More people than ever before now receive NHS support for their mental health, with five million patients accessing care in 2022/23, an increase of over one million in five years.
Urgent and emergency care
Pressure on urgent and emergency care (UEC) services continued in August.
There were 2,106,146 attendances in A&Es across England, an average of 67,940 per day. This means there were a total of 6,522,000 attendances in June, July and August making it the busiest summer ever [1].
Despite this demand and further periods of industrial action, NHS staff managed to maintain progress against the ambitions set out in the UEC Recovery Plan.
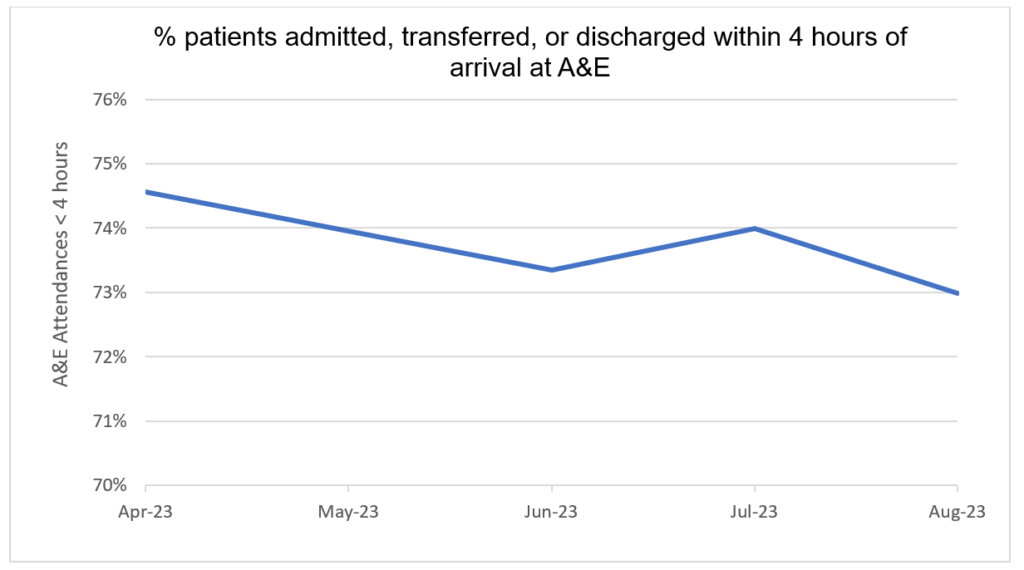
73% of patients attending A&E were admitted, transferred or discharged within hour hours. This compares to 71.7% in August 2022.
Percentage of patients admitted, transferred, or discharged within 4 hours of arrival at A&E
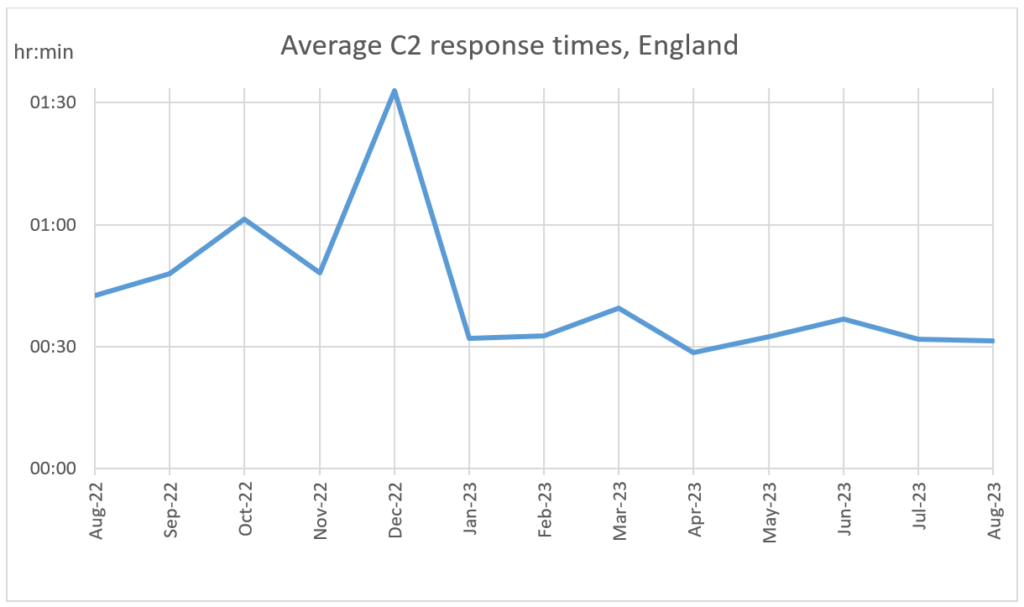
The average ambulance response time for a category two call was 31 minutes and 30 seconds – a faster response time of 11 minutes and 7 seconds compared to August 2022 [2]. Ambulance services answered 770,251 999 calls, 24,847 per day, and responded to 706,639 incidents.
Average C2 response times, England
An essential aim in the UEC recovery plan is to deliver an increase of 5,000 staffed and sustainable (core) beds.
New data published this month shows there were 98,959 general and acute beds open in August. 97.8% of these were core beds and 2.2% were escalation beds – beds that the NHS temporarily opens to cope with immediate or growing operational pressure.
Increasing the number of core beds is one of the ways the NHS is preparing for winter, with more than 99,000 core beds expected to be in place across the country by December 2023.
We are also focussed on improving in-hospital flow by reducing length of stay and bringing forward discharge processes. In August, the average number of patients who were in a hospital bed for 14 or more days decreased by over 13% since January [3].
Elective recovery
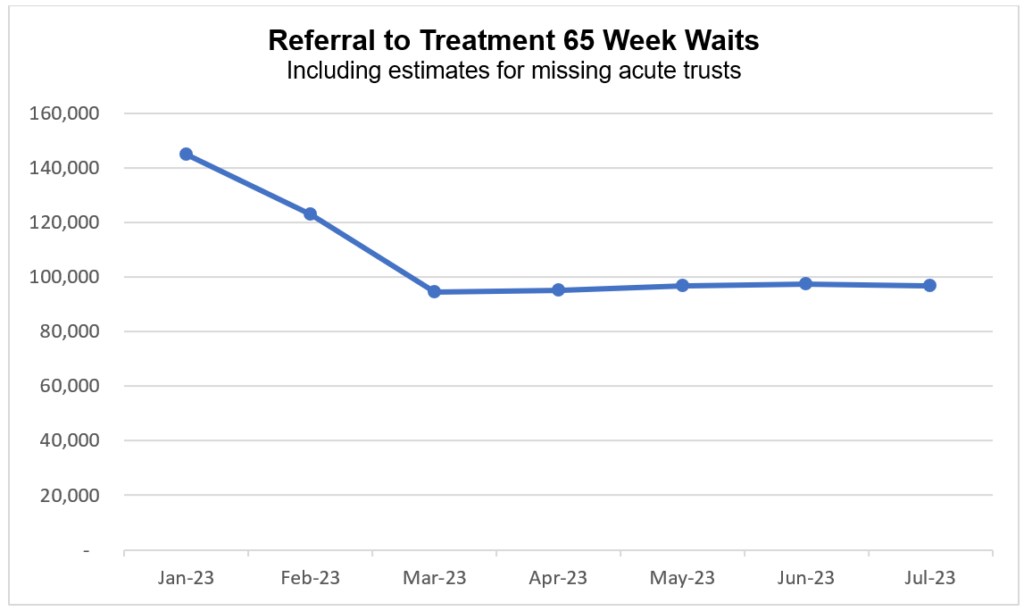
Continuing industrial action had a significant impact on planned care in July. However, despite nine days of strikes, staffing pressures and increased demand [4], the NHS continued to hold delivery on reducing the longest waits for elective care.
As of the end of July, 96,722 (1.3%) patients were waiting more than 65 weeks for treatment. This is down by 41.8% since the start of the year [5].
Referral to treatment 65 week waits
Including estimates for missing acute trusts
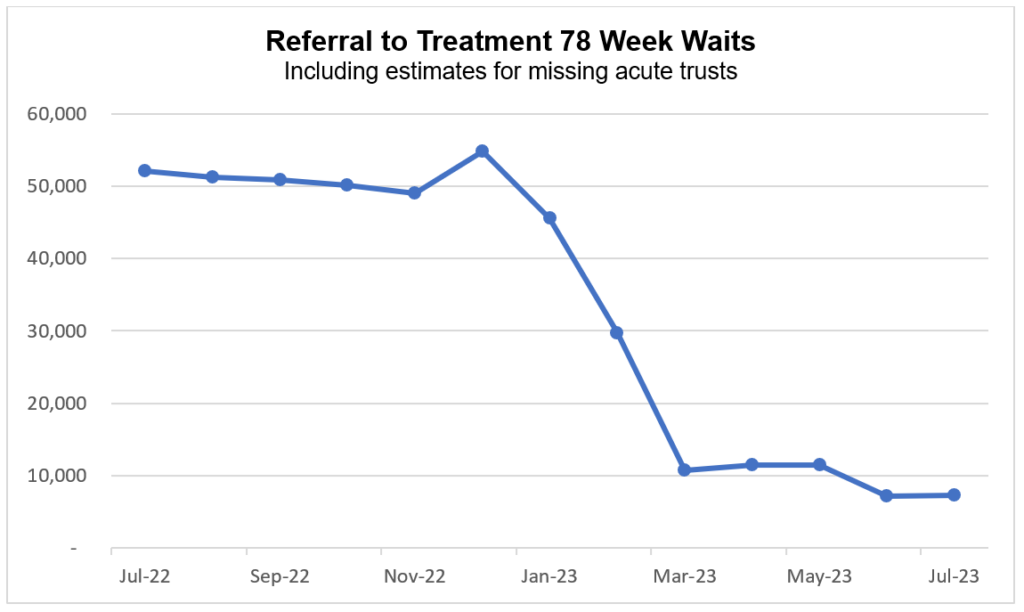
7,289 patients were waiting more than 78 weeks for treatment. This is a reduction of 44,859 (86%) since July 2022.
Referral to treatment 78 week waits
Including estimates for missing acute trusts
Fewer than 280 patients were waiting more than 104 weeks for treatment. This has reduced by 77% since the start of the year [6].
The NHS also carried out 2,214,141 tests and checks in July, up 7% on the same month pre-pandemic [7]. The average waiting time for diagnostic tests and procedures was 3.1 weeks.
Additional diagnostic capacity has been created through 111 Community Diagnostic Centres (CDCs) which have already provided millions of diagnostic tests, checks and scans.
CDCs are an essential focus of the elective recovery delivery plan. The aim is open 160 centres by March 2025, so patients get tested faster and more conveniently.
Cancer
Demand for cancer services continued at record levels in July 2023, with the number of urgent suspected cancer referrals at 130% of pre-pandemic levels. To meet high demand, treatment is also at record levels.
Urgent suspected cancer referrals first seen
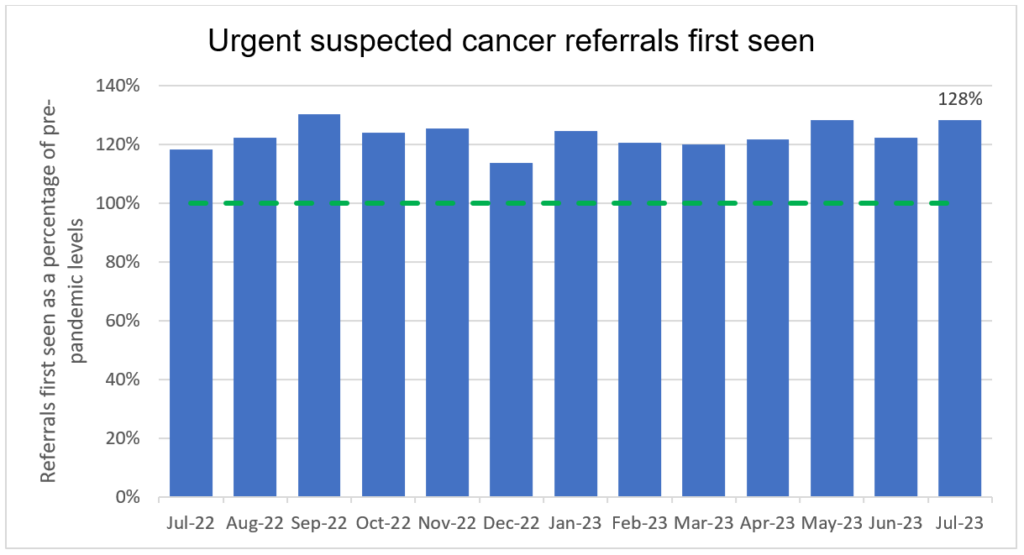
Over 335,000 people received treatment for cancer over the last year between August 2022 and July 2023 – the highest year on record, and up by more than 22,000 on the same period pre-pandemic.
GPs have been referring people for urgent cancer checks in record numbers since March 2021. Since then, NHS staff have seen over 970,000 more people than in the same period prior to the pandemic.
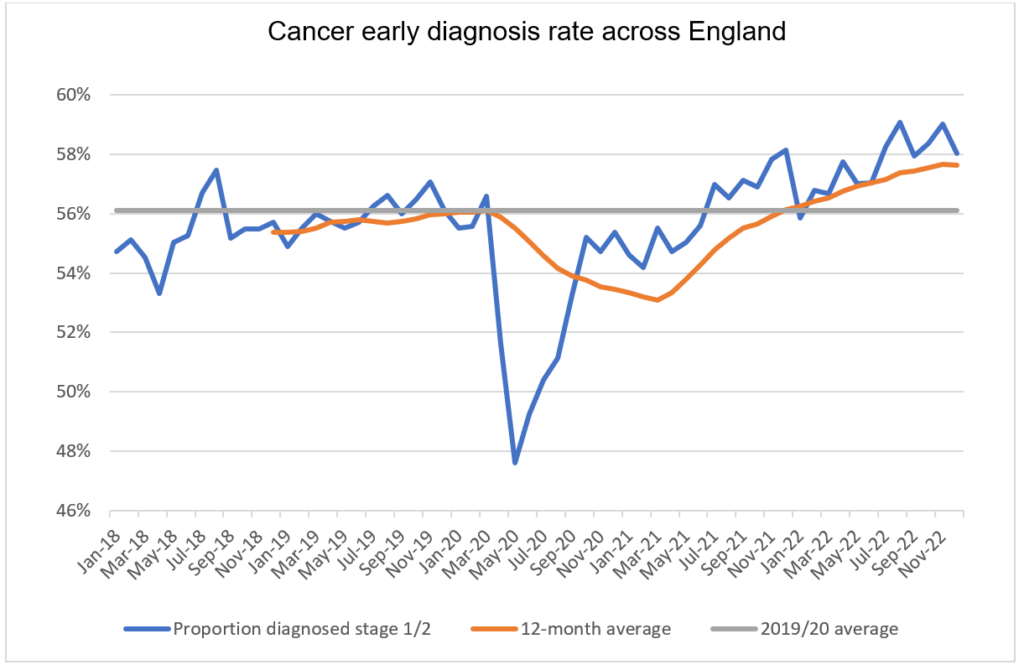
The increase in referrals has contributed to the NHS diagnosing more cancer at an early stage than ever before. We are diagnosing a higher proportion of cancers at an early stage now than ever before – about 2% higher than before the pandemic. Survival is also at an all-time high.
In 2023, the Annals of Oncology published findings showing that cancer deaths are around 10% lower in the UK compared to just 5 years ago.
Cancer early diagnosis rate across England
The NHS is working hard to keep up with this increase in demand. It has been accelerating the installation of new diagnostic capacity, much of it in Community Diagnostic Centres.
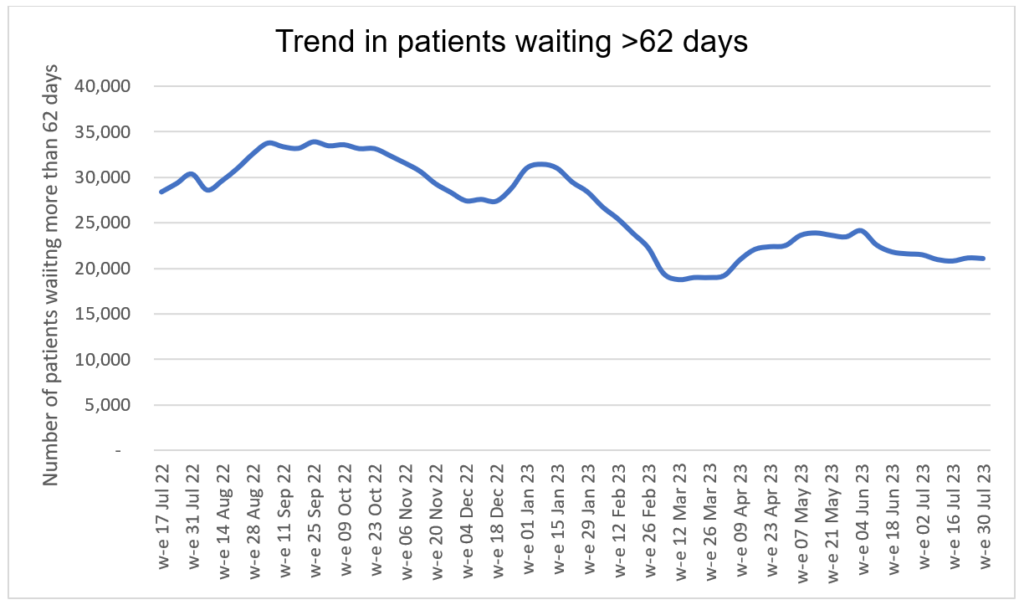
The backlog has already reduced by 14,000 people since its peak last summer, and despite the recent seasonal increase, NHS staff remain focused on ensuring that people who have been waiting longest or who need care most urgently are seen first.
Trend in patients waiting more than 62 days
Mental health
More people than ever before now receive NHS support for their mental health, with five million patients accessing care in 2022/23, an increase of more than one million in five years.
Services across the country have made great efforts to improve access and reduce waiting times against a backdrop of increased needs and complex conditions. This is particularly the case for children and young people, with one in six now facing a potential mental health problem compared to one in nine in 2017.
The pandemic and its aftermath have exacerbated the factors that contribute to poor mental health and demand for mental health care is at an all-time high, with bed occupancy still above 95% across NHS mental health hospitals.
The NHS is working hard to reduce this treatment gap and expand its mental health offer, supported by an extra £2.3bn a year. This includes expanding and transforming community services for adults and older adults with severe mental illness (SMI) such as eating disorders, schizophrenia or bipolar disorder, with the aim of offering patients access to personalised and holistic care as close to home as possible.
In June 2023, over half a million people with SMI (547,156 in total) had received an assessment and started treatment in community mental health services in the previous 12 months.
Improving dementia care is also a key focus of the NHS. Assessment and diagnosis begin in a memory clinic where people with symptoms and their carers can access a multi-disciplinary team for advice, information, and support.
In June 2023 there was a 28% increase in new referrals to memory clinics (3566 referrals in total) as services work around the clock to clear pandemic backlogs.
New referrals to a memory clinic
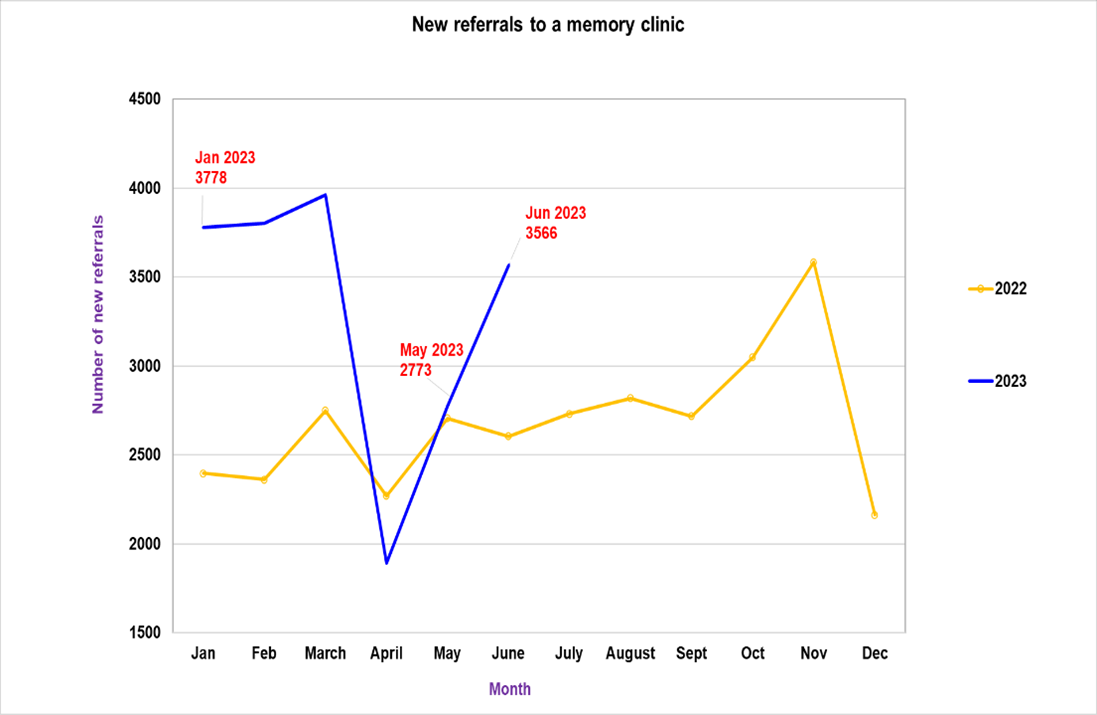
With potential new treatments for Alzheimer’s disease on the horizon, we are stepping up and accelerating preparation for potential rollout. This includes establishing a dedicated programme team for early Alzheimer’s treatments working across the NHS in collaboration with industry partners and patient groups.
Footnotes
[1] The previous high was 6,498,472 in 2019. Summer: June, July and August.
[2] In August 2022, the average ambulance response time for a category two call was 42 minutes and 37 seconds.
[3] In January 2023, the average number of patients in a bed for 14 or more days was 50,355. In August 2023 it was 44,980 patients on average per day.
[4] There were 129,833 more new RTT periods in July 2023 compared to July 2022.
[5] 166,201 patients were waiting more than 65 weeks at the end of 2022.
[6] 1,222 patients were waiting more than 104 weeks for treatment at the end of 2022.
[7] 2,064,497 diagnostic tests were carried out in July 2019.

