Explanatory notes
The ‘Lead clinician’ – will be the clinician primarily responsible for care of CYP with epilepsy. In Paediatric services, this may be a Community Consultant Paediatrician, Secondary care Consultant Paediatrician (including those with particular interest in Epilepsy), Tertiary Paediatric Neurologist or Consultant in Neurodisability supported by an Epilepsy Specialist nurse or Community Paediatric Nurse specialist.
In Adult services, most commonly the Lead Clinician will be the GP or a Consultant Neurologist in Secondary or Tertiary epilepsy services. However in some services, the Lead Clinician may include a Consultant Psychiatrist in Learning disability (with close links to a local Consultant Neurologist), Community Consultant Psychiatrist or Consultant Neuropsychiatrist. Epilepsy Specialist Nurses may be the Lead Clinician in services with established clinical supervision from a Consultant Neurologist.
Accessible text version
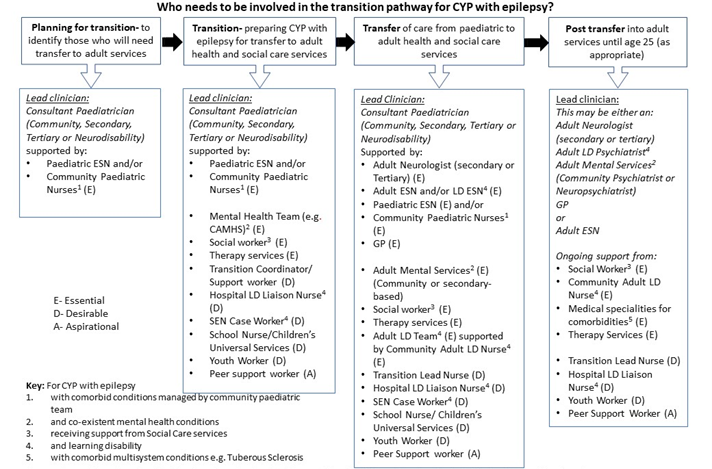
This flow chart aims to recognise that CYP with epilepsy may have multiple comorbid conditions and needs. All professionals and services involved whilst the CYP in is paediatric services should be involved in planning for transition and, where possible, co-ordinate transfer to their adult service counterparts.
The following appendix contains a diagram of a suggested approach of who should be involved when a child or young person with epilepsy transitions from paediatric to adult epilepsy services. It contains a list of key professionals who are considered either essential, desirable or aspirational to be involved in the transition process. This flow chart aims to recognise that CYP with epilepsy may have multiple comorbid conditions and needs. All professionals and services involved whilst the CYP in is paediatric services should be involved in planning for transition and, where possible, co-ordinate transfer to their adult service counterparts. The precise configuration of professionals and services involved in transition should be tailored to the individual patient and local service arrangements. Transition and transfer arrangements between services may involve joint consultations, MDT meeting or direct communication.
The initial stage in the flowchart is planning for transition. When planning for transition, it will be important to identify those who need to transfer into adult services. This identification should be by a lead clinician who will be the clinician primarily responsible for care of the CYP with epilepsy. This may be a consultant paediatrician from the community, secondary, tertiary or neurodisability service. It is considered essential that they should be supported by a peadiatric epilepsy specialist nurse and/or a community paediatric nurse if the CYP has comorbid conditions managed by the community paediatric team.
Following this stage, there should be a transition stage. This is the stage of preparing the CYP with epilepsy for transfer to adult health and social care services. There should be a lead clinician who will be the clinician primarily responsible for care of the CYP with epilepsy. This may be a consultant paediatrician from the community, secondary, tertiary or neurodisability service. It is considered essential that they should be supported by a peadiatric epilepsy specialist nurse and/or a community paediatric nurse if the CYP has comorbid conditions managed by the community paediatric team. For CYP with co-existent mental health conditions, it is considered essential that the mental health team (for example the CAMHS team) should also be involved. For CYP receiving support from social care services, it is considered essential that a social worker should be involved. It is also considered essential that any therapy services involved in the care of the CYP should also be involved during this preparation process. It is desirable to also include a transition co-ordinator or support worker in this stage. If the CYP has learning disability, it is desirable to include a hospital learning disability liaison nurse or a SEN case worker. It is also desirable for CYP with epilepsy to be supported in this stage by a school nurse or Children’s Universal Services, as well as a youth worker. It is aspirational during this stage for the CYP with epilepsy to be supported by a peer support worker.
The next stage is the transfer stage. This is where the CYP with epilepsy is transferred from paediatric to adult health and social care services. During this stage, there should be a lead clinician. This will be the clinician primarily responsible for care of CYP with epilepsy. In Paediatric services, this may be a Community Consultant Paediatrician or Secondary Care Consultant Paediatrician, Tertiary Paediatric Neurologist or Consultant in Neurodisability. During this stage, it is considered essential that CYP with epilepsy should be supported by an adult neurologist from either secondary or tertiary care. It is considered essential that an adult epilepsy specialist nurse and/or a learning disability epilepsy specialist nurse is involved. It is considered essential that the CYP should be supported by a peadiatric epilepsy specialist nurse and/or a community paediatric nurse if the CYP has comorbid conditions managed by the community paediatric team. It is considered essential for the GP to be involved in this stage. For CYP with epilepsy and co-existent mental health conditions, it is considered essential that the adult mental health services (either community or secondary-care based) is involved. It is considered essential that for CYP with epilepsy receiving support from social care services, the social worker is involved. It is also considered essential that any therapy services involved in the care of the CYP should also be involved. For CYP with epilepsy and a learning disability, is considered essential that the adult learning disability team, supported by a community adult learning disability nurse is involved. It is desirable for a transition lead nurse to be involved. For CYP with epilepsy and a learning disability, it is considered desirable for the hospital learning disability liaison nurse to be involved and for a SEN case worker to be involved. It is also considered desirable for a school nurse or children’s universal services and a youth worker to be involved. It is considered aspirational for a peer support worker to be involved.
The next stage is the post-transfer stage, where the following professionals listed may be involved in the transition process into adult services until age 25, as appropriate. During this stage, there should be a lead clinician who may be either an adult neurologist (secondary or tertiary), or an adult learning disability psychiatrist for young people with epilepsy and a learning disability, or an adult mental health services (community psychiatrist or neuropsychiatrist) for young people with epilepsy and co-existent mental health conditions, or a GP, or an adult epilepsy specialist nurse. It is considered essential that during this stage there is ongoing support from a social worker. For young people with epilepsy and a learning disability, it is considered essential that there is ongoing support from a community adult learning disability nurse. For young people with epilepsy and with comorbid multisystem conditions (e.g. Tuberous Sclerosis), it is considered essential that there is ongoing support from medical specialities for comorbidities. It is considered essential that any therapy services involved in the care of CYP with epilepsy are providing ongoing support. It is considered desirable that young people with epilepsy have ongoing support from a transition lead nurse. It is considered desirable that young people with epilepsy and a learning disability receive ongoing support from a hospital learning disability liaison nurse. It is considered desirable that young people with epilepsy receive ongoing support from a youth worker. It is considered aspirational that young people with epilepsy receive ongoing support from a peer support worker.
Further explanatory notes on lead clinician: The ‘Lead clinician’ – will be the clinician primarily responsible for care of CYP with epilepsy. In Paediatric services, this may be a Community Consultant Paediatrician or Secondary Care Consultant Paediatrician, Tertiary Paediatric Neurologist or Consultant in Neurodisability supported by an Epilepsy Specialist nurse or Community Paediatric Nurse specialist. In Adult services, most commonly the Lead Clinician will be the GP or a Consultant Neurologist in Secondary or Tertiary epilepsy services. However in some services, the Lead Clinician may include a Consultant Psychiatrist in Learning disability (with close links to a local Consultant Neurologist), Community Consultant Psychiatrist or Consultant Neuropsychiatrist. Epilepsy Specialist Nurses may be the Lead Clinician in services with established clinical supervision from a Consultant Neurologist.