Accessible text version
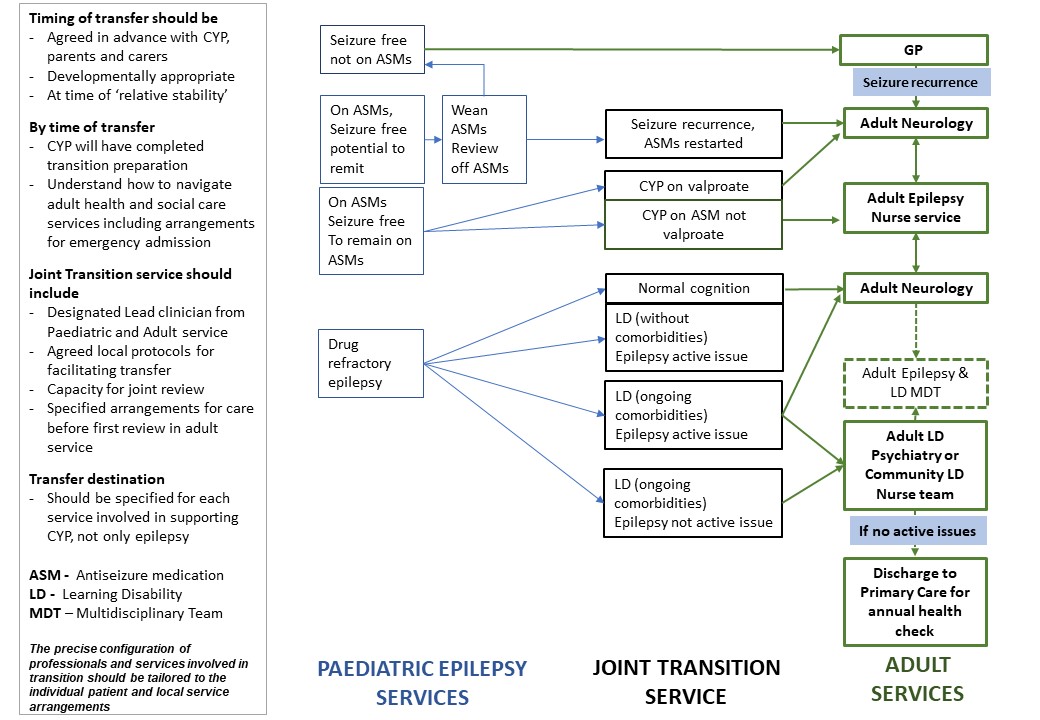
The following appendix contains a flowchart of a suggested approach for where CYP with epilepsy should be transferred to when moving from paediatric epilepsy services to adult epilepsy services.
Timing of transfer should be agreed in advance with CYP, parents and carers, be developmentally appropriate and at time of ‘relative stability’.
By time of transfer the CYP should have completed transition preparation and understand how to navigate adult health and social care services including arrangements for emergency admission
A Joint Transition service should include 1) designated lead clinician from Paediatric and Adult services, 2) agreed local protocols for facilitating transfer, 3) capacity for joint review and 4) specified arrangements for care before first review in adult service.
The transfer destination should be specified for each service involved in supporting the CYP, not only for epilepsy services.
The flowchart shows the possible transfer destinations, determined by if the patient is seizure free, on antiseizure medication or if they have drug refractory epilepsy i.e. not seizure free.
If a patient is seizure free and not on antiseizure medication, their care can be transferred from paediatric services to their GP. If in future, there is a seizure recurrence, the GP should refer the person to the local adult neurology service.
If the CYP is on antiseizure medication, but has an epilepsy syndrome that is known to remit in childhood, the paediatric services should attempt antiseizure medication withdrawal before considering transfer and review the patient off antiseizure medication. If the patient remains free off antiseizure medication they can be transferred to their GP. If seizures recur, antiseizure medication should be restarted and the patient should be transferred to the adult neurology service.
For those CYP with epilepsy who are seizure free and remaining on antiseizure medication, transfer of care should be to the adult neurology service or adult epilepsy nurse service. All CYP with epilepsy who are seizure free on sodium valproate should be transferred to the adult neurology service for ongoing monitoring. CYP with epilepsy on antiseizure medications, not on sodium valproate and seizure free are referred to the adult epilepsy nurse service. On transfer to adult services, the CYP with epilepsy may move between the adult neurology and Adult Epilepsy Nurse services as appropriate.
For CYP with drug refractory epilepsy, transfer destination is influenced by the presence of learning disability and associated comorbidities, and whether the epilepsy is an active issue or not. CYP with drug refractory epilepsy and normal cognition should be referred to adult neurology, who may also refer to the adult epilepsy nurse service. CYP with Learning disability, without additional comorbidities in whom epilepsy is the active medical issue, should be referred to adult neurology. CYP with learning disability and ongoing comorbidities, with active epilepsy should be transferred to adult neurology and adult learning disability services which could include adult LD psychiatry or community adult LD nurse team. CYP with learning disability and ongoing comorbidities in whom epilepsy is not an active issue, should be referred to adult learning disability services which could include adult LD psychiatry or community adult LD nurse team. There should be an Adult LD and epilepsy MDT between the Adult LD services and adult neurology services for discussion of patients with LD and epilepsy. After transfer to the Adult LD services, there are no ongoing active issues relating to epilepsy or LD comorbidities, the patient can be transferred to their GP with ongoing annual LD health check.