1. Introduction
The National GP Retention Scheme is a package of financial and educational support to help eligible doctors, who might otherwise leave the profession, remain in clinical general practice.
The scheme supports both the retained GP (RGP) and the practice employing them by offering financial support in recognition of the fact that this role is different to a ‘regular’ part time, salaried GP post, offering greater flexibility and educational support. RGPs may be on the scheme for a maximum of five years with an annual review each year to ensure that the RGP remains in need of the scheme and that the practice is meeting its obligations.
From 1 April 2023, the formal four-session cap that a retained GP can work per week has been removed. Reimbursement will remain for up to four sessions but this does not preclude a contractor from directly employing or engaging a member of the GP Retention Scheme, at their own expense, for service sessions which are in addition to the maximum four sessions for which the contractor is eligible for payment under the Scheme. This scheme enables a doctor to remain in clinical practice which includes protected time for continuing professional development and with educational support.
Doctors applying for the scheme must be in good standing with the General Medical Council (GMC) without GMC conditions or undertakings – except those relating solely to health matters. The scheme is not intended for the purpose of supporting a doctor’s remediation and where the relevant NHS England Responsible Officer has concerns, the doctor would not usually be eligible for the scheme.
Following the merger of NHS England and Health Education England (HEE), the scheme is now managed by NHS England, where previously the scheme was jointly managed by Health Education England (HEE) through the designated HEE RGP Scheme Lead and NHS England. The scheme is funded through the Primary Medical Care Allocation and payment provisions to GP practices are contained within the General Medical Services Statement of Financial Entitlements Amendment Directions 2017, paragraph 20A.2.
2. Eligibility criteria for doctors
The scheme is open to doctors who meet ALL of the following criteria:
1. Where a doctor is seriously considering leaving or has left general practice (but is still on the National Medical Performers List) due to:
- Personal reasons – such as caring responsibilities for family members (children or adults) or personal health reasons, or
- Approaching retirement, or
- Require greater flexibility in order to undertake other work either within or outside of general practice.
2. And when a regular part-time role does not meet the doctor’s need for flexibility, for example the requirement for short clinics or annualised hours.
3. And where there is a need for additional educational supervision. For example, a newly qualified doctor needing to work 1-4 sessions a week due to caring responsibilities or those working only 1-2 sessions where pro-rata study leave allowance is inadequate to maintain continuing professional development and professional networks.
Doctors must hold full registration and a licence to practice with the GMC and be on the National Medical Performers List.
Evidence to ascertain whether a doctor is seriously looking to leave general practice may include:
- Proof from appraisal
- Letter of resignation
- Accessing or intention to take pension payment
- Statement of intent to leave
Doctors may wish to return to a more substantive role when they come to the end of the scheme, although this is not a requirement of the scheme.
RGPs (Retained GPs) can do other paid GP work outside of their RGP post.
RGPs are permitted to undertake (with no upper limit):
- GP out-of-hours work and urgent care work
- Other kinds of Non-GP clinical work (e.g. family planning, dermatology, occupational health etc.) which allows them to retain or extend their skills outside of general practice
- Other kinds of non-clinical work (e.g. education, appraisal, management etc.) which enables them to retain or extend their skills.
- in hours GP work out with their retained GP post, in the same or a different practice
There are many benefits to this flexibility
- Permits a graded exposure to more hours without long term commitment to them (testing the water). Give the doctor control to manage this.
- Can help to facilitate additional working during term-time for RGPs who have responsibilities during school holidays.
- Enables the doctor to gain confidence by trying out new practices and organisations.
- Can help ease the transition to moving off the scheme if RGPs can try expanding their commitment.
- May increase participation in the workforce of those who felt restricted by the 4-session cap
- Aid transition to a new practice or a different variety of primary care work (e.g. walk in centre, vanguard etc. ).
They may also undertake other kinds of clinical (e.g. family planning, dermatology, occupational health etc.) or non-clinical work (education, appraisal, management etc.) This has proven benefit for retention and enables them to retain or extend their skills. For some doctors joining the scheme, it may allow them to retain GP skills whilst undertaking other substantive posts such as (but not limited to) senior management roles and education. Retainers must notify the designated NHS RGP Scheme Lead (previously HEE RGP Scheme Lead) at their annual review of all work roles with the RGP sessions, as this will be part of the discussion around evaluating continued need and eligibility for the scheme.
All changes in the job plan worked on the scheme should be discussed and approved by the NHS RGP Scheme Lead (HEE RGP lead).
This allows RGPs to maintain a portfolio career while undertaking a GP role within the bounds of the scheme. The RGP must notify the designated NHS RGP Scheme Lead if working more than four sessions, if not declared previously on application form.
Employment law states that ‘all employees have the legal right to request flexible working (not just parents and carers) and that employers must deal with requests in a reasonable manner’.
3. Possible applicants
- Locums
- Salaried GPs
- GP Partners
- Doctors within general practice on a career break of less than 24 months who remain on the National Performers List (or are expected to have been re-admitted by the time they start as an RGP) and are registered with a licence to practice with the GMC.
Where a doctor has previously been on the Retained Doctors Scheme but is not currently on the Scheme and is otherwise eligible, they may apply to re- join the scheme.
4. Eligibility criteria for GP practices
The GP practice should offer the RGP work which enables them to maintain skills across the full spectrum of a general practitioner. The RGP should be embedded in one GP practice to enable peer support at work and continuity with patients.
Practices must be able to demonstrate they can meet the educational needs of the RGP as appropriate and that they understand the ethos of educational supervision. The designated NHS RGP Scheme Lead will assess this based on the needs of the doctor who is applying. The practice should provide a named educational supervisor who is either a GP trainer, F2 supervisor or has recently accessed a suitable training course in supervision. The precise specification is for local determination by the designated NHS RGP Scheme Lead.
Practices may employ more than one RGP where there is capacity for support and long term career opportunities with the prior approval of the designated NHS RGP Scheme Lead.
5. Funding
5.1 Professional expenses supplement
Each RGP would qualify for an annual professional expenses supplement of between £1000 and £4000 which is based on the number of sessions worked per week. It is payable to the RGP via the practice. The expenses supplement is subject to deductions for tax and national insurance contributions but is not superannuable (pensionable) by the practice.
The whole of the expenses supplement payment will be passed on by the practice to the doctor to go towards the cost of indemnity cover, professional expenses and CPD needs. The practice should not automatically make any other deductions from the RGP expenses supplement except for tax and national insurance contributions. Certain expenses may be claimed against tax by the RGP (e.g. subscriptions to medical defence organisations and membership of the BMA and GMC annual retention fee etc).
The RGP will be offered an expenses supplement payment (paid via their practice), as follows:
| Number of sessions per week | Annualised sessions* | Expenses supplement payment per annum (£) |
|---|---|---|
|
1-2 |
Fewer than 104 |
1,000 |
|
2 |
104 |
2,000 |
|
3 |
156 |
3,000 |
|
4 |
208 |
4,000 |
*annualised sessions include statutory holidays, annual leave and sessions used for CPD.
The RGP professional expenses supplement will be paid at the commencement of employment and then each year on the anniversary following a successful annual review
5.2 Support for practices
Each practice employing a RGP will be able to claim an allowance relating to the number of sessions for which their retained doctor is engaged. The practice will qualify for a payment of £76.92 per clinical session (up to a maximum of four) that the doctor is employed for. This allowance will be paid for all sessions including sick leave, annual leave, educational, maternity, paternity and adoptive leave where the RGP is being paid by the practice. Evidence of this payment will be required. The practice and RGP will continue to receive payments under the terms of the scheme as long as the RGP remains contracted to the practice and the practice continues to pay the RGP.
Costs during these absences will need to be covered by the practice. However it may be possible to claim reimbursement costs associated with covering any absences of a RGP via the GMS (General Medical Services) SFE (Statement of Financial Entitlements) for sickness, maternity, parental and adoption leave.
| Contracted sessions per week | Maximum financial support to practice per year (based on £76.92 per session) |
|---|---|
|
1 |
£3,999.84 |
|
2 |
£7,999.68 |
|
3 |
£11,999.52 |
|
4 |
£15,999.36 |
This support is to be used by the practice as an incentive to provide flexibility for the RGP and should be used towards the RGPs salary, to cover HR admin costs and to provide funding to cover any educational support required from the practice, including course fees where relevant.
Following the removal of the cap on the number sessions that can be worked per week, reimbursement will remain at up to four sessions. Those RGPs working more than four sessions would not receive any additional financial supplement and the practices they worked at would not be eligible for any additional funding. If the RGP, is working more than four sessions, annual leave and additional CPD hours are to be agreed with applicant and employer.
6. Obligations of the RGP, practice, educational supervisor
6.1 Obligations of the RGP
The RGP is obliged to:
- Hold full registration and a licence to practice with the General Medical Council (GMC), meet the requirements for remaining on the NHS England GP Performers List and report to NHS England any concerns that might affect their status on the National Medical Performers List.
- Maintain membership of a medical defence organisation to the level required by NHS England.
- Notify the designated NHS RGP Scheme Lead, in advance where possible, of any changes in working arrangements (e.g. additional work) and domestic circumstances that may affect participation in the scheme.
- Notify the designated NHS RGP Scheme Lead of any long spells off work (over four weeks), e.g. maternity leave or long-term sick leave.
- Submit to the designated NHS RGP Scheme Lead an annual renewal form at least one month in advance of the joining anniversary, to allow time for discussion regarding continuity of the scheme and any adjustments required.
- Make every effort to attend any events organised by the designated NHS RGP Scheme Lead expressly for RGPs.
- Meet appraisal and revalidation requirements and make their responsible officer aware of the fact that they are a RGP.
6.2 Obligations of the practice, employing organisation
The employing practice is obliged to:
- Offer adequate and appropriate induction, both on joining and after any significant break (e.g. maternity leave). This will include for example IT systems, practice procedures and protocols, referrals systems, in-house and community services, collaborative working arrangements and referral pathways, prescribing formularies, team roles, information governance, safeguarding etc.
- Nominate a clinical colleague to act as an educational supervisor, who will provide one to one support in protected time, (fortnightly or monthly as discussed and agreed with the RGP). A minimum of 2 hours a month would be recommended (additional to CPD entitlement).
- Notify the designated NHS RGP Scheme Lead and RGP’s responsible officer if appropriate and in advance of any substantial changes within the practice that may impact upon the employment and educational arrangements of the RGP.
- Work with the RGP to create a job plan suitable for the needs of the individual RGP to keep them in the profession. The job plan should include participation in team meetings during the RGPs normal working days.
- Encourage and facilitate the appropriate use of CPD time allowance.
- Record GP retainers accurately through the National Work Reporting System (Primary Care Web Tool) to facilitate national monitoring of the scheme
7. Contractual/employment issues
7.1 Contract of employment
All RGPs will be employed by the agreed practice. GMS and PMS practices should
offer terms and conditions that are no less favourable than the model salaried GP contract as determined in the GMS Contract /PMS Agreement. For APMS employers the Salaried Model Contract is considered as a benchmark.
Terms and conditions of employment are a matter of negotiation between the RGP and the practice. The BMA has developed a model retainer scheme contract which is based on the Salaried GP Model Contract but specific to the Scheme. Contract checking and advice services can be accessed by BMA members by calling 0300 123 1233 or by emailing support@bma.org.uk. General advice for non-members can be obtained by emailing info.gpc@bma.org.uk.
The RGP achieves full employment rights after 24 months with the same employer and the practice (employer) under employment law is obliged to continue the contract of employment after that time. Any changes in circumstance that may affect the employment of the RGP should be a matter of discussion between the RGP and the practice, and appropriate advice should be taken. The practice is expected to notify the designated NHS RGP Scheme Lead of any substantive changes that may affect employment of the RGP. Examples may include a practice merger, change to different premises, change of NHS England practice contract holder or contract type (e.g. following practice reprocurement).
7.2 Hours of work
The cap for the number of sessions has been removed (although reimbursement will remain for up to four sessions) therefore the RGP contracted number of sessions is to be agreed between relevant parties – a session is 4 hours 10 minutes (37.5 hrs / 9 sessions) (BMA, 2017). The number of sessions can be annualised with the expectation that the RGP works a minimum of 30 weeks out of the 52. This will include annual leave, statutory holidays and personal development time. The pattern of sessions worked will be reviewed with the RGP each year through their annual review associated with the scheme.
It is not considered good practice for an RGP to work in isolation for example on sites where they will not have access to colleagues for support and advice.
The duration of the retainer contract will be for the duration of the scheme (5 years) and reviewed annually.
The number of sessions the RGP is contracted to work on the scheme may be changed following the submission of a revised suitable job plan which is subject to approval of the designated NHS RGP Scheme Lead and NHS England’s local Director of Commissioning Operations (DCO) (or nominated deputy either within NHS England or delegated ICB).
7.3 Duration of the scheme
RGPs can be on the scheme for a period of up to five years.
7.4 Extended absence and scheme extensions
The RGP, in discussion with the designated NHS RGP Scheme Lead and subject to agreement by the NHS England’s DCO (or nominated deputy either within NHS England or delegated ICB), can extend their time on the scheme in the following circumstances.
- To replace time off the scheme relating to maternity, parental, adoption or sick leave.
- Under special circumstances e.g. where a RGP has had to change practices due to relocation or due to break down in placement and support and would not have enough time left on the scheme to acquire employment rights in a fresh post.
In these circumstances an extension of up to 24 months would be deemed appropriate.
The RGP continues to be a member of the scheme whilst on maternity, parental leave and sick leave. RGPs are strongly advised to make use of “Keeping in Touch” (KIT) days where they are available. If a RGPs annual renewal falls whilst they are on paid parental leave, they can choose to send a renewal application or defer until they return to work.
The practice and RGP will continue to receive payments under the terms of the scheme as long as the RGP remains contracted to the practice and the practice continues to pay the RGP.
The scheme extension form should be used for extensions in relation to maternity, parental, adoption, sick leave or special circumstances only.
8. Annual review of RGPs and their placements
RGPs will be required to undergo an annual review with the designated NHS RGP Scheme Lead; this will allow careful consideration of their needs and whether they are being met by the practice, requirements for future months and whether they should remain on the scheme.
9. Job plan
All GPs should have a job plan. In regards to the National GP Retention Scheme the job plan is a working schedule which ensures that the RGP post delivers its aims, including provision for CPD and the requirements of the contract of employment are met by the employer and RGP. Please refer to the BMA’s guidance on job planning which is available on the BMA website.
Example job plans are included in annex 2. Principles of a good job plan include:
Job plans should be developed collaboratively between the employer and RGP. They should be revised only by mutual agreement as a minimum 8-12 weeks after joining the scheme, annually and when any major changes are suggested by either party.
Scheduling in the job plan should include:
- Clinical duties: appointments, visits, dealing with telephone queries from patients or other health care professionals.
- Administrative / paperwork whether arising directly from this caseload (referrals, investigations, results) and indirectly (reports, medicals, etc.).
- Meetings (whether informal or formal) essential to the delivery of team based care, discussing clinical practice standards; support significant event audit (SEA) etc. Where these occur on an ad hoc basis, adjustments to clinical workload may be required.
- Personal continuing professional development (CPD) time – see CPD section.
- Time for supervision.
- Specific specialist roles in the practice: e.g. medical student teaching, QoF area of responsibility, other special interests, e.g. dermatology, women’s/sexual health, minor surgery.
Workload should:
- Be defined in amount (number of patients) and type (clinical, paperwork, team meetings), with provisions for fluctuations in exceptional circumstances such as returning after career break.
- Reflect RGP abilities.
- Realistically match contracted hours as defined in the contract of employment.
- Be balanced, recognising both clinical and non-clinical work. It is recommended that the ratio of direct clinical care to indirect clinical care should be no more than region of 3:1 (excluding meetings) in accordance with BMA safe working guidance.
The job plan will set out clear arrangements around how and when extra-contractual duties (where agreed) will be recognised and when time in lieu will be taken (e.g. monthly or added to annual leave). This is especially relevant where there are significant fluctuations in workload and hours of the RGP if they are helping to cover another doctors’ absence (e.g. sickness or maternity leave).
RGPs on this scheme are able to work extended hours to support seven day access to primary care where appropriate and where this suits their personal circumstances. However, this must take place within the agreed pattern of work/work plan.
Although a session is defined as 4 hours and 10 minutes, periods of duty do not need to be exact multiples of this. For example a contract for 16 hours 40 minutes can be divided into 2 x 6 hours days and a day of 4 hours and 40 minutes if this suits both parties and delivers the educational supervision and CPD component of the post.
Breaks should be granted within worked hours in keeping with the European working time directive. Start and finish times should consider the RGPs situation and caring responsibilities if appropriate.
The RGP is expected to complete medical reports that are part of GMS contractual obligations. However, the RGP is not normally expected to complete medical reports for private purposes, unless there is an agreement between the RGP and the practice for additional remuneration or time within the job plan.
On call commitment where applicable should be specified: e.g. 12 half days a year and no more onerous than the RGPs pro-rata share of the clinical complement of the practice. So if there are 40 clinical sessions worked by doctors in the practice and the RGP works 4 they should do no more than 1/10 of the on call over the year.
10. Educational aspects
10.1 Induction
All RGPs, irrespective of length of service, must complete an appropriate induction programme specific to their role and the practice in which they will be based. This will include for example IT systems, practice procedures and protocols, referral systems, in house and community services and referrals pathways, prescribing formularies, team roles, collaborative working arrangements, information governance, safeguarding etc.
The practice will be required to offer the RGP experience of a sufficiently wide range of general practice experience to ensure that they retain their skills. This will be mutually agreed and stated within the job plan, which will include hours of work, duties, time set aside for CPD and necessary attendance at meetings.
10.2 Continuing Professional Development (CPD)
RGPs have a wide range of experience and it is important that CPD opportunities are tailored to individual need. The RGP is entitled to the pro rata full time equivalent of CPD as set out within the salaried model contract.
CPD is based on:
- The needs of the individual, as established at their appraisal.
- Discussion with the designated NHS RGP Scheme Lead.
- Discussion with the practice supervisor.
This is underpinned by a robust job plan and reviewed annually by the designated NHS RGP Scheme Lead.
There should be an appropriate balance of CPD sessions spent in the practice (such as in house educational meetings, SEA and prescribing meetings, quality improvement activities) and activities outside the practice (such as learning groups, e-learning, self-directed learning, talks, courses and locality protected learning events). Some RGPs may value the opportunity to develop leadership skills as part of their CPD.
CPD activities may fall outside the RGPs contracted time. For example, if an RGP only works on Monday, it is highly likely that they may find the course they wish to access occur on Tuesday, Wednesday Thursday or Friday. The CPD time can then be taken on an “in lieu” basis on a mutually agreed date.
In line with the standard contract there are no specific contributions to CPD apart from the professional expenses supplement and financial support for practices.
The practice will:
- Invite the RGP as appropriate to practice based events, including practice meetings, in-house training, away-days and significant event meetings, in protected time, using the CPD allowance as appropriate and agreed, with reference to learning needs as established at the RGPs appraisal.
- Ensure that the workload of the doctor takes into account that this is a supported post.
- Monitor sessions worked to ensure that these do not exceed those agreed in the job plan, recognising that sessions worked may be annualised.
- Ensure that all members of the practice are aware of these requirements.
Development and educational input will vary according to the circumstances of the RGP and the practice in which they are working. The RGP will meet their educational supervisor annually to review the job plan and ensure CPD arrangements are in place to meet their annual Personal Development Plan (PDP) as agreed with their appraiser.
If the RGP has concerns around the organisation and times for their CPD, they should contact their designated NHS RGP Scheme Lead.
10.3 Supervision
The scheme includes a requirement for protected time for supervision by the educational supervisor. The educational supervisor will provide one to one support in protected time, (fortnightly or monthly as discussed and agreed with the RGP). A minimum of 2 hrs a month would be recommended (additional to CPD entitlement).
The aim of the supervision is to provide individual support for the doctor, help facilitate their integration into the practice, ensure that their professional development needs are supported and avoid professional isolation. This support should be tailored to the individual needs of the RGP.
11. Existing retainees
RGPs who have been accepted on to the Retained Doctor Scheme 2016 (where the application form has been approved by the NHS England DCO (or nominated deputy either within NHS England or delegated ICB) but who are not in post before 31 March 2017 will be accepted onto the National GP Retention scheme without the need to re-apply.
12. The role of the designated NHS RGP Scheme Lead
The RGPs application and proposed job plan will be reviewed by the designated NHS RGP Scheme Lead to ensure that the education and development elements are appropriate for the individual and meet the individual doctor’s skills, work-life balance requirements and career objectives. The designated NHS RGP Scheme Lead will ensure the practice has the capacity to meet the obligations of the scheme throughout its duration.
The designated NHS RGP Scheme Lead will support the RGP to ensure that they are able to keep up to date with CPD and education. They will ensure that the RGP has an annual review to make sure that the practice is fulfilling its obligations and meeting the needs of the RGP and as well as the RGPs suitability to continue on the scheme.
13. Management of the scheme
The designated NHS (previously HEE) RGP Scheme Lead will manage the scheme including the review of applications and job plans of potential RGPs, monitoring educational aspects, maintaining a database of RGPs and practices and developing a support network for RGPs within their region. RGP application records will be retained by the NHS local team for audit purposes for six years. The retention period will be triggered by the RGP leaving the scheme, the six year retention will begin from the end of the relevant financial year (Information Governance Alliance, 2016).
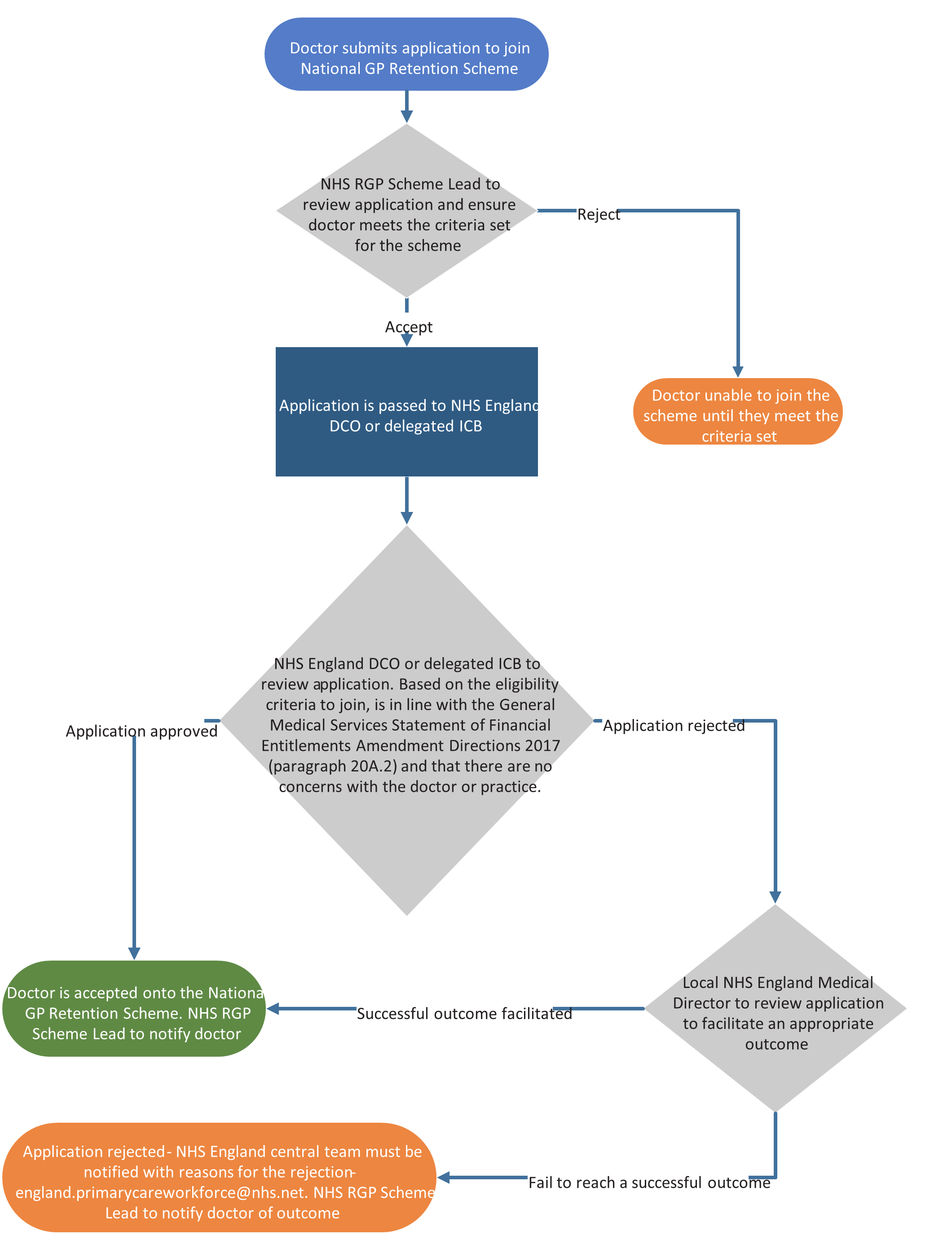
In terms of approval of RGPs applications and payment:
- Designated NHS England RGP Scheme Lead process RGP applications (using the standard application form) and pass eligible applications with their recommendation to their NHS England local office – NHS England DCO (or nominated deputy either within NHS England or delegated ICB).
- NHS England DCO (or nominated deputy either within NHS England or delegated ICB) makes the final decision whether the doctor can join the scheme. This is based on the eligibility criteria to join the scheme, is in line with the General Medical Services Statement of Financial Entitlements Amendment Directions 2017 (paragraph 20A.2) and that there are no concerns with the doctor or practice. Where the ICB is delegated, a discussion between the NHS England DCO (or Medical Director) is recommended when considering the application. For successful applications the designated NHS RGP Scheme Lead is to be notified who will then notify the doctor and practice. If an application is rejected please see section 15.
- NHS England local office finance team (or equivalent within the ICB) notifies Primary Care Support (PCS) England of the practice that will be hosting the retained doctor.
- Payment authorisation – local finance team (NHS England or ICB) complete/approve retainer form and send to PCS England. Retainer to be funded through the Primary Medical Care Allocation. Payment provisions to GP practices are contained within the General Medical Services Statement of Financial Entitlements Amendment Directions 2017, paragraph 20A.2.
- PCS England sends a claim form to the practice hosting the retained doctor and then processes claims when received. Approval is sought from the relevant NHS England Contract Manager (or ICB equivalent) to enable PCS England to make payment to the practice directly.
The standard application/annual review form is to be used as part of the application and annual review process.
The end of scheme form is to be completed by the RGP and designated NHS RGP Scheme Lead on the RGPs last day of the scheme.
Following the merger of HEE and NHS England, data previously held by HEE will be shared with NHS England for the purpose of approving applications and monitoring the effectiveness on the scheme. Regular reporting of the progress of applications through the scheme will be undertaken and regional and local colleagues are expected to encourage practices to record GP retainers accurately through the National Workforce Reporting System (Primary Care Web Tool) to facilitate national monitoring.
14. Unsuccessful applications
When an application is rejected the rationale for the decision is to be stated on the application form. Before the decision is communicated back to the doctor the local NHS England Medical Director is to review the application to facilitate an appropriate outcome.
Where a successful outcome cannot be achieved and the application rejected, the NHS England central team must be notified by emailing the application form and a summary of the reasons for the application being rejected to england.primarycareworkforce@nhs.net.
The final decision can then be communicated back to the doctor via the designated NHS RGP Scheme Lead.
15. Flow chart of the approval process for RGPs
Annex 1 – Local Office Contacts
Details of the local offices are available via the NHS England website – contact your local scheme office.
Annex 2 – Example job plans
The following two example job plans can also be found in the PDF version of this document.
Example 1
To include the number of appointments and appointment type
Job plan:
RGP with young dependents preferring to work school hours working 4 sessions (16 hours 40mins) per week.
To be completed jointly by RGP, Educational Supervisor and Practice Manager. Refer to job planning guidance in RGP handbook.
How many weekly sessions will the post comprise of (1-4): 4
| Post details | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
|---|---|---|---|---|---|---|---|
| Practice site (should normally only be one) | Chesterfield | Chesterfield | Chesterfield | N/A | N/A | Chesterfield | N/A |
| Start time | 9.30 | 8.00 | 9.30 | N/A | N/A | 8.30 | N/A |
| Finish time | 13.30 | 15.00 | 15.10 | N/A | N/A | 12.30 | N/A |
| AM surgery: Number of appointments, time of first and last appointment | Appointments from 9.30-13.30 (2 catch up slots) | Appointments from 8.00-13.00 (2 catch up slots) | Appointments from 9.30-15.10 (2 catch up slots) | N/A | N/A | Appointments from 8.40-12.30 (2 catch up slots) | N/A |
| PM surgery: Number of appointments, time of first and last appointment | N/A | None | 8.00 from 13.30 14.50 | N/A | N/A | – | N/A |
| Visits | – | Up to 2 | – | N/A | N/A | 2 | N/A |
| Time for admin | 90 minutes | 1 hour 50 | 90 minutes | N/A | N/A | 90 minutes | N/A |
| Meetings – title, start and finish times | – | Clinical meeting 13.00–14.30 | – | N/A | N/A | – | N/A |
| Mentoring time slot | – | 14.30 -15.00 | – | N/A | N/A | – | N/A |
| Hours worked this day | 4 hours | 7 hours | 5hr 40mins | N/A | N/A | 4 hours | N/A |
| Comments: Ad hoc adjustments to allow for non weekly meetings or time in lieu for late finishes/extended hours | When extra visiting doctor is needed morning appointments reduced. When working Saturday extended hours this will be instead of Monday | When on call 8.0013.00 no booked slots and duty system applies | – | N/A | N/A | 8 Saturdays a year, instead of Mondays | N/A |
On call duties – using contracted time as RGP in the practice
| Start and finish time, day of week | Frequency (number per year) | If extends normal day length, arrangements for time in lieu |
|---|---|---|
| Wed 8.00 – 13.00 | 8 times a year – reflects pro-rata share of clinical team | Yes by 1 ½ hours. Time in lieu = 12 hours added to annual leave |
| CPD Activity | In house education meetings: describe frequency, duration and purpose | Formal courses or protected learning events occurring on contracted retainer days | Practice development work where aligned to PDP goals and NHS appraisal | Time out of practice for self directed learning or time in lieu for CPD carried out outside of contract time where aligned to NHS appraisal PDP goals | Total |
|---|---|---|---|---|---|
| Details | Monthly 1hour, education including prescribing and SEAS | – | Safeguarding, or palliative care, QOF area, etc. | – | |
| Hours / year | Up to 42 potentially in Tuesday meeting | 5 hours attending GP update course 5.40 attending safeguarding update day Time outs 2 on Tuesday = 2x90mins from 13.00 2 on Wednesday = 2x 2hr10mins Total : 16 hours | 4 hours leading on safeguarding area | 19 | 81 |
| Sessions / year approx. | 10 | 4 | 1 | 5 | 20 |
To be completed by the Educational Supervisor:
| How will you support the RGP in carrying out practice development work? (e.g. IT training, admin support, etc) | Planned protected time will be given without clinical work to allow handover from previous lead, updating of protocols systems, meeting with health visitor. |
| What are the arrangements for booking CPD time at the practice for all the above categories? | Request made via Educational Supervisor, preferably 8 weeks notice. Every effort will be made to accommodate and we ask that time in lieu is taken where possible when others are not absent. |
Example 2
Job plan:
RGP is senior GP with management role working 2 sessions (8 hours 20mins) per week.
To be completed jointly by RGP, Educational Supervisor and Practice Manager. Refer to job planning guidance in RGP handbook.
How many weekly sessions will the post comprise of (1-4): 2
| Post details | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
|---|---|---|---|---|---|---|---|
| Practice site (should normally only be one) | Abbots | N/A | N/A | Abbots | N/A | N/A | N/A |
| Start time | 17.30 | N/A | N/A | 7.30 | N/A | N/A | N/A |
| Finish time | 20.00 | N/A | N/A | 13.20 | N/A | N/A | N/A |
| AM surgery: Number of appointments, time of first and last appointment | N/A | N/A | N/A | 7.30-10.20 10.20-10.50 mentoring. 10.50–13.20 appointments and admin. (2 catch up slots) | N/A | N/A | N/A |
| PM surgery: Number of appointments, time of first and last appointment | 17.30-20.00 appointments (1 catch up slot) followed by admin | N/A | N/A | – | N/A | N/A | N/A |
| Visits | – | N/A | N/A | 1 visit | N/A | N/A | N/A |
| Time for admin | – | N/A | N/A | – | N/A | N/A | N/A |
| Meetings – title, start and finish times | None | N/A | N/A | Monthly team meeting 8.00-9.00 | N/A | N/A | N/A |
| Mentoring time slot | – | N/A | N/A | 10.20-10.50 | N/A | N/A | N/A |
| Hours worked this day | 2h 30 | N/A | N/A | 5 hr 50 | N/A | N/A | N/A |
| Comments: Ad hoc adjustments to allow for non weekly meetings or time in lieu for late finishes/extended hours | – | N/A | N/A | When on call 8.0013.00 in which case no booked slots and duty system applies. When monthly meeting 8.00-9.00 then surgery appointments cancelled during meeting time. | N/A | N/A | N/A |
On call duties – using contracted time as RGP in the practice
| Start and finish time, day of week | Frequency (number per year) | If extends normal day length, arrangements for time in lieu |
|---|---|---|
| Thursday 8.00-13.00 | 4 times a year reflects pro-rata share of clinical team | No |
| CPD activity | In house education meetings: describe frequency, duration and purpose | Formal courses or protected learning events occurring on contracted retainer days | Practice development work where aligned to PDP goals and NHS appraisal | Time out of practice for self directed learning or time in lieu for CPD carried out outside of contract time where aligned to NHS appraisal PDP goals | Total |
|---|---|---|---|---|---|
| Details | e.g. monthly 1hour, education including prescribing and SEAS | n/a | (e.g. safeguarding, or palliative care, QOF area, etc.) | n/a | n/a |
| Hours / year | Monthly 8-9am =10 hours | Time out events occur outside of contacted hours Practice education meetings occur outside of contacted hours on Tuesdays Possibly GP update event if occurs Thursday. Total: 7 hours | 4 hours leading on QoF/ prescribing | 20 hours To take 20 hours back from clinic time in lieu of attending educational meetings on a Tuesday. Will attend practice education meetings on Tuesdays when outside role permits | 41 |
| Sessions / year approx. | 2.5 | 1.5 | 1 | 5 | 10 |
To be completed by the Educational Supervisor:
| How will you support the RGP in carrying out practice development work? (e.g. IT training, admin support, etc) | Planned time will be arranged with practice pharmacist and individually to progress prescribing lead area. |
| What are the arrangements for booking CPD time at the practice for all the above categories? | Will be emailed routinely to be made aware of schedule of practice education meetings and have an opportunity to influence the programme. Will have protected time to attend monthly meeting 8.00-9.00 unless RGP does not find this useful and appraisal/review time would be better spent on other activities. Time out of practice for courses or for time in lieu of courses/self-directed learning will be booked via our rota manager Lesley. We ask for as much notice as possible and will endeavour to ensure requests are met whenever feasible. Authorisation will be confirmed within 7 days unless there is a more urgent request. |
Equality and health inequalities statement
Promoting equality and addressing health inequalities are at the heart of NHS England’s values. Throughout the development of the policies and processes cited in this document, we have:
- Given due regard to the need to eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it; and
- Given regard to the need to reduce inequalities between patients in access to, and outcomes from healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities.
Publication reference: PRN00578