Foreword
This is the first annual report since the implementation on 9 September 2024 of the most significant change to the registration of deaths for many decades. It is also my last as the National Medical Examiner.
I am impressed by how smooth the transition has generally been to a statutory requirement for independent scrutiny of all deaths not investigated by a coroner; the result of months and years of preparation nationally by NHS England, the Department of Health and Social Care (DHSC) and other government departments and the Welsh Government, and locally by medical examiners, registrars and coroners, and by other partners and stakeholders.
The scope of this remarkable achievement, the additional safeguards provided, and the impact for bereaved families cannot be overstated.
I have been determined throughout my time as National Medical Examiner to ensure bereaved people were central to the new certification process – and they now are.
Preparation for few initiatives in the NHS will have been to meet a hard deadline for statutory implementation that applies to every case without exception across 2 countries.
Medical examiners and officers have delivered a step change in safeguards: since 9 September 2024 medical examiners have independently scrutinised every death in England and Wales not referred to a coroner and given bereaved people an opportunity to ask questions and raise any concerns with someone who had not provided care.
With close to 600,000 deaths annually this was a significant undertaking. Medical examiners reached the landmark of a million deaths independently examined under the non-statutory system in July 2024. They also increased the proportion of non-acute deaths that are independently scrutinised in England from 41% in the last quarter of 2023 to 58% in April to June 2024, in large part by building connections with primary and community healthcare providers.
In the months leading up to the death certification reforms, I was able to say with confidence that the NHS was ready. That confidence was in large part down to the efforts and dedication of frontline champions.
As described in this report, through 2024 medical examiners continued to strengthen the medical examiner system and deliver the benefits we anticipated, despite uncertainties along the way, particularly about the date the death certification reforms would come into force.
The feedback medical examiner offices receive remains overwhelmingly positive, as exemplified by the quotes through this report. This is testament to their enthusiasm, commitment and resilience in leading this national programme locally.
Some concerns were raised after the reforms commenced that registrations were routinely taking several weeks, but evidence does not bear this out.
Office of National Statistics (ONS) data available at the time of writing indicates the typical median time to register deaths (which includes the work of attending practitioners, register offices and in some cases coroners, and also the additional time informants now have to register deaths) has generally increased by 1 or 2 days since the additional safeguards in the new system were introduced.
In terms of variation, in English regions the mean (average) time for medical examiners to send a Medical Certificate of Cause of Death (MCCD) to registrars ranged from 3.8 to 5.2 days from date of death after the reforms commenced; and in Wales this was around 8 to 9 days.
However, I do wish to acknowledge that in a minority of areas it took longer for deaths to be registered; and the distress this may have added to bereaved families.
The reasons vary, as prompt registration of deaths depends on all stakeholders and partners working together – attending practitioners including GPs, register offices and, in some cases, coroners, as well as medical examiners.
In addition, there was an adjustment for some attending medical practitioners when medical examiners began working with them to drive up the quality of recorded causes of death.
Regional medical examiners and the lead medical examiner in Wales have been supporting those areas with the longest times to reduce avoidable delays, but reasons are often outside the control of medical examiner offices.
The medical examiner system is maturing but still in its infancy. In coming months and years it will require careful curation, support and adequate resources to protect its intended role – to give the bereaved an opportunity to raise concerns and to identify opportunities to improve care and safeguards.
This, in my opinion, means a focus nationally on digital technology to promote efficiency; maintenance of the regional escalation route and expert guidance and advice for medical examiners in England following the closure of NHS England; and locally adequate resources to ensure the resilience of this statutory function and provide appropriate services to the bereaved.
There is, of course, scope for medical examiners – in partnership with others involved in the certification and registration process – to review and improve their processes.
In Wales, a national working group reviewed processes early in 2025, and decided to consider winter planning in August and September. In England, I have encouraged medical examiners to use the (generally) quieter summer months to work with partners in the registration of deaths to review how things have gone, how together they can enhance resilience for winter 2025/26 and continue to improve the experience of bereaved people.
This depends as much on healthcare providers, attending medical practitioners, register offices and coroners as much as it does on medical examiners. It is encouraging that many medical examiner offices have started to report improved working arrangements with partners.
Considering the wider death certification reforms, I believe refinements to processes will improve the experience of the bereaved and enhance the efficiency of this public service.
For example, arrangements are needed to send crematorium medical referees reliable information about implantable medical devices and for referees to be able to raise queries with attending practitioners.
Should work restart on the digital MCCD – as hoped – this will bring efficiencies for the work of attending practitioners, medical examiners and register offices. DHSC and NHS England are continuing to evaluate how medical examiners can have easier access to patient records and, where relevant, social care records.
The quarterly updates medical examiner offices in England provide require manual counts and inputting. I hope work on a case management system will be prioritised to allow more efficient reporting and analysis of medical examiners’ findings.
The ONS predicts number of deaths will increase over the next decade due to changing demographics: in England alone by 10% from 2023/24 to 2033/34.
Efficiencies may release capacity to meet some of the extra workload, but NHS bodies are likely to need to consider increasing staffing for medical offices to continue to fulfil their statutory obligations in a timely manner.
The new National Medical Examiner will need to better understand the difference medical examiners are making in terms of probity, patient safety incidents and inadequate care. They may also be helped in this by the DHSC commissioned independent review of the impact of the death certification reforms.
The role of medical examiners and officers, the resources available to medical examiner offices and assurance about their independence should continue to be kept under review and protected.
I am confident that I am leaving the medical examiner system in safe hands, and my successor will provide the vision, clarity and ambition to build on the outstanding successes already delivered and ensure bereaved people continue to benefit from the insight and support provided by medical examiners and officers.
Dr Alan Fletcher, National Medical Examiner
Introduction
The National Medical Examiner is required to produce a report for the Secretary of State and Welsh Ministers under the National Medical Examiner (Additional Functions) Regulations 2024, setting out how the National Medical Examiner and medical examiners have exercised their functions and the way in which attending medical practitioners have exercised their functions under the Medical Certificate of Cause of Death Regulations 2024.
This is the first National Medical Examiner’s report since the government introduced the death certification reforms on 9 September 2024. It explores the final steps in their implementation and the experience in the initial months following this.
These reforms represent the first significant change to death certification policy and process in many decades and it is notable that their implementation has been smooth and without significant disruption in most areas. Over half a million deaths have now been successfully registered since the reforms were implemented; the overwhelming majority without incident or concern about the process.
Every non-coronial death now receives independent scrutiny by doctors not involved in the deceased’s care and bereaved people are given the opportunity to ask questions and express their concerns.
At national level, close working between government departments, the Welsh Government, and NHS England provided the basis for this success. The support of the Royal College of Pathologists has also been pivotal.
Locally, medical examiners and officers in England and Wales worked closely with NHS staff, registrars, coroners and other partners including crematorium staff and funeral directors.
Local challenges did emerge in a few areas, but these have now largely been overcome as a result of local partners working together with the interests of bereaved people uppermost in their efforts.
Preparations for the death certification reforms
At the start of 2024 the timing for implementation of the death certification reforms was still uncertain, but from the governments’ draft regulations, published in December 2023, we knew this was potentially from April 2024 and that we needed to continue to prepare.
Earlier dates had been postponed to ensure legislation and regulations were in place and robust. It was in April 2024 that Parliament approved 9 September 2024 as the commencement date, and this was confirmed by the new government in July 2024.
Extension of medical examiner scrutiny to deaths in wider healthcare settings and the community continued during the remainder of the non-statutory phase.
The estimated proportion of scrutinised non-acute deaths in England increased from 41% in October to December 2023 to 58% in April to June 2024 and to around 70% in July to September 2024 (figures may not be directly comparable to previous quarters as data collection changed to reflect the statutory arrangements and in the final 3 weeks all deaths were scrutinised).
NHS Wales Shared Services Partnership (NWSSP) estimates that about 70% of all deaths were being scrutinised in Wales in the weeks immediately before 9 September 2024.
These statistics may underplay the readiness of NHS systems for the transition. Many GP practices, while not yet referring all cases, had engaged with medical examiner offices and by referring a sample of cases had tested and established effective processes.
In early 2024, reports from medical examiner offices in England suggested more than one third of GP practices were regularly referring deaths to medical examiners. Of the remainder, nearly 30% had engaged with medical examiners or tested referral processes. NWSSP reports that around 25% of GP practices were referring some deaths with all practices having engaged with medical examiners at some level before September 2024.
However, some GP practices chose not to engage with medical examiner offices until the new process was imminent and consequently had to learn or establish processes after 9 September 2024. Unfortunately, this did contribute in a minority of areas to delays for bereaved people in registering deaths.
Support for medical examiner offices and other stakeholders
In preparation for the death certification reforms, the National Medical Examiner’s office and Lead Medical Examiner Officer for Wales developed guidance, tools and resources for medical examiner offices and the medical community:
- National Medical Examiner’s guidance for England and Wales, issued under the National Medical Examiner (Additional Functions) Regulations 2024
- Publication in July 2024 helped medical examiners and officers get ready for the reforms.
- The guidance provides a flowchart summarising the new processes for registering deaths , which was developed in co-operation with the DHSC, Welsh Government and other government departments, along with other major stakeholders.
- Guidance also set out the training requirements existing and new medical examiners needed to fulfil.
- An operational readiness checklist; available to medical examiner offices in July 2024.
- 4 new e-learning modules were published setting out the legal changes introduced by the death certification reforms.
- Podcasts describing how medical examiners and GPs could work together for the benefit of bereaved people and frontline NHS staff and how the regulations would work.
- These received over 8,000 visits and were in part intended to help overcome hesitancy among some GP practices to engage with the programme ahead of the introduction of the statutory reforms.
- How-to guide from the Lead Medical Examiner Officer for Wales for adding digital signatures to PDF files (to make scanning and sending paper MCCDs more efficient).
The National Medical Examiner provided medical examiner offices with fortnightly updates, informing them of new tools and encouraging their further engagement with GP practices and other healthcare providers. NHS England bulletins and letters from the Deputy CMO in Wales were used to increase awareness of the forthcoming changes.
The National Medical Examiner’s office continued to build on wider resources available to medical examiners. For example, the Royal College of Pathologists published 4 further good practice papers for medical examiners on topical matters in 2024:
- palliative and end of life care
- maternal deaths
- deaths after delays in care and treatment
- supporting bereaved people
Work on 5 more started in 2024 and these have since been published:
- inherited cardiovascular conditions
- sepsis
- sickle cell disease
- deaths of children and neonates (update to existing paper)
- organ and tissue donation (update to existing paper)
Implementation of the death certification reforms
Despite the steady extension of medical examiner scrutiny to a greater proportion of deaths in the run up to 9 September 2024, the requirement after this date for all non-coronial deaths to be reviewed represented a significant step up in activity for medical examiner offices in England and Wales, from 92,543 deaths scrutinised in January to March 2024 to 132,994 in October to December 2024.
The death certification reforms are often described only in terms of the start of the statutory medical examiner system, yet they impact on the work of many others including attending practitioners, register offices, coroners and crematorium medical referees.
In the initial weeks following implementation, DHSC co-ordinated work across responsible government departments to address undue variation in application of the new requirements.
The General Register Office provided clarifying guidance to register offices, and the National Medical Examiner and Chief Coroner issued a joint statement to achieve greater consistency in interactions between coroners and medical examiners.
Welsh Government convened a Strategic Oversight Board of all stakeholders to work through implementation issues.
Time to complete medical certificates of cause of death
Despite the scale of the changes, implementation went smoothly in most areas, without widespread and systemic problems. ONS data indicates there was not a substantial increase in the time to register deaths, despite the additional safeguards introduced.
In those areas that did face initial challenges, these have largely been resolved by local agencies and stakeholders working together in the interests of bereaved people.
As medical examiners are obliged by law to make the enquiries they consider necessary and ensure the bereaved have the opportunity to ask questions and raise concerns, it is not possible to set a time limit for completion of enquiries. Some cases take longer than others for various reasons.
The National Medical Examiner’s guidance states, “Delays in all parts of the death certification process must be kept to a minimum, including the work of medical examiners, but medical examiners must devote adequate time to each case to maintain the integrity of independent scrutiny.”
It is crucial that the additional safeguards and benefits which the medical examiner system was designed to deliver are maintained.
Nevertheless, any delay, particularly if avoidable, in the ability to register a death can add to the distress felt by the recently bereaved. The National Medical Examiner’s office, DHSC and Welsh Government have closely monitored the time taken to register deaths following introduction of the reforms, to identify variation and support those areas with the longest times. As noted previously, this depends on the work of all partners, not just medical examiners.
In most areas arrangements are working well and those that initially experienced challenges have seen improvements.
For the period October to December 2024, the reported median time from death to MCCD completion was 5 days or less for nearly three-quarters of medical examiner offices in England (73%); and 3 days or less for over a third (36%). NWSSP report the median time in Wales was 8 days.
Figures reported for the subsequent quarter were generally similar. The average (mean) time in the 7 regions in England from death to sending MCCDs to register offices ranged from 4 to 5.5 days for the last quarter of 2024, with this variation in part explained by the higher demand for urgent scrutiny in some areas (around 11% of deaths in the London region). The equivalent variation between health board areas in Wales was just under 2 days.
Informants must now register the death within 5 days of MCCD completion (not from the date of death) and arrange an appointment with local authority registrars to complete this.
ONS data shows the typical (median) time from death to registration, reflecting all parts of the certification and registration process for deaths certified by a doctor, was 7 to 8 days in England at the end of quarter 4 2024/25, and 12 to 14 days in Wales.
Where the time taken has increased, many complex factors were involved. In Wales, medical examiner offices are not located in hospitals, and NWSSP believes this contributes to longer times for registering deaths in hospital settings. The Welsh Government convened an oversight group to identify causes of delays and mitigating actions, which have largely been implemented.
Some healthcare providers, including certain GP practices, have struggled to provide medical examiner offices with MCCD and patient records in a timely manner.
In Wales, NWSSP reports that in October to December 2024, medical examiners waited a median of 3 days for deaths to be referred to them.
Similarly in England, more than 50 medical examiner offices reported typically waiting 2 days. In many cases further work was also required, to formulate a satisfactory cause of death or to facilitate access to required patient records.
There were also temporary increases in registration times at the Christmas/New Year and Easter periods. The increase over winter has been a feature of registrations for many years. Cross-government co-ordination of action across all components of the registration system would be required to fully avoid such issues in future.
Local authority register offices would need to provide more appointments on bank holidays and weekends, and consider whether the number of appointments available through the year is adjusted adequately to reflect the higher number of deaths in the winter.
Similarly, coroners’ offices and attending practitioners would need to be available to reduce the time taken processing CN1A cases.
In the NHS, the time taken to by attending practitioners to complete MCCDs will be affected by winter pressures and the priority given to treating those who are unwell or in hospital. Mortuary staffing over public holidays may also not accommodate the release of bodies on bank holidays and weekends.
Medical examiner offices are well placed to help co-ordinate local arrangements, but they do not oversee other parts of the system and have no authority to compel them to work in different ways. Medical examiner offices have been asked to plan ahead for winter 2025/26, maximising medical examiner and officer capacity over this period.
“We noticed a surge in deaths in an ITU…it appears that most were inappropriate admissions to ITU with an expected poor outcome. Admissions criteria have been re-emphasised to the team.”
(Medical examiner office)
Some reports of difficulties in local death management processes were unrelated to the death certification reforms, such as the bereaved not being able to view the deceased before burial or cremation and bodies not being released to families or funeral directors.
The death certification reforms include no new directions on such matters. Public mortuaries have differing rules about viewing bodies, and the coroner may restrict access to or release of the body.
Both these examples pre-date introduction of the death certification reforms. Medical examiners have no oversight or authority over mortuaries and cannot influence coroners’ discharge of their independent judicial role.
More recent submissions from medical examiner offices report improved working arrangements with other parts of the death management system such as GP practices, register offices and coroners. Most issues were local and resolved through constructive dialogue in the interests of bereaved people.
A final observation is that in the longer term, the proposed digital MCCD has great potential to reduce the time taken in certifying deaths.
Impact in 2024
Summary
Medical examiners independently scrutinised over 403,696 deaths in 2024; 381,603 in England and 22,093 in Wales. When implementation of the medical examiner system started on a non-statutory basis in 2020, there were a number of expected benefits.
Medical examiners support local learning and improvement by detecting and referring concerns to established clinical governance processes, and protect the public with greater safeguards, identifying poor practice and deterring criminal activity.
Since 9 September 2024, medical examiners in England have referred 7 to 8% of deaths in acute trusts for case record review or equivalent, and 5 to 6% of all deaths for some form of clinical governance review.
Of the deaths referred for case record review at host NHS trusts in England, 2,873 were deaths of people with a learning disability or severe mental illness. In addition, 1,922 patient safety incidents in England were notified by medical examiner offices as a result of scrutiny.
Under the slightly different governance processes in Wales, NWSSP report that 29% of acute hospital deaths and 16% of non-acute hospital deaths were referred to care providers for further learning. The categories for referral in Wales were realigned to Healthcare Quality Standards.
Medical examiners have also identified a small number of matters that have been referred to coroners and ultimately reported to the police.
A medical examiner office identified a cluster of infected implants, this was escalated to the clinical lead for orthopaedics to investigate, and also dealt with via the Learning from Deaths (LfD) team.
Clearer information governance freedoms for medical examiners to share information could improve cross-system learning. The National Medical Examiner’s guidance notes “Medical examiner offices should facilitate learning where possible but will need to take information governance requirements including confidentiality into account.”
Taking the example of people who die of natural causes but have (at some point) been patients of mental health providers; these trusts often do not learn that their former patients have died or the circumstances, information that could be used to improve care for current and future patients.
It has been noted that medical examiners would facilitate greater transparency for bereaved families and give them more opportunities to raise concerns. In England and Wales medical examiners and officers are giving the bereaved this opportunity in all cases.
Medical examiners are also expected to improve the quality and accuracy of the cause of death recorded in medical certificates (MCCDs) and make referrals to coroners more consistent and appropriate. Deaths reported to coroners fell by 10% in 2024 compared to 2023 and are expected to fall further (explored later in this report).
Current reporting systems do not allow accurate assessment of the proportion of MCCDs for which causes of death are amended after medical examiner scrutiny. Anecdotally, the proportion may be as high as 40% for MCCDs in some healthcare settings.
In due course it should be possible for the ONS to estimate the impact of medical examiner scrutiny on MCCD accuracy through evaluation of registration data. The proposed digital MCCD may provide a reliable mechanism for reporting the proportion of MCCDs for which causes of death are amended.
Experience of bereaved people
“One office has been trialling a text information service which sends a message to the NOK [next of kin] to acknowledge the death and to inform them that the ME office will be in touch.
“They report that this is working well, feedback has been positive so far, and believe this may have helped to decrease phone call enquiries from relatives.”
Regional medical examiner
The death certification reforms put bereaved people at the centre of the process for registering deaths. For every death in England and Wales, the bereaved now have the opportunity to ask questions or raise concerns with someone who did not provide care to the deceased.
Medical examiner offices report near universal coverage: for over 95% of the 381,603 deaths scrutinised by medical examiners in England in 2024 there was an interaction with bereaved people (97% in October to December 2024).
Some bereaved people will understandably decline the offer and are free to do so as participation is voluntary, and some individuals die without identifying their next of kin.
In Wales, if there is no interaction with the bereaved person, NWSSP contact others, either a professional or an informal associate of the next of kin, such as a friend or neighbour.
Feedback and complaints
Feedback from bereaved people to medical examiner offices remains overwhelmingly positive, noting the compassion shown by medical examiners and officers and the comfort and reassurance they provide.
“We were notified [of a death] just before 8pm and had completed full scrutiny and countersigned the MCCD and sent it to the register office by 10.40pm.”
(Medical examiner office)
Some medical examiner offices survey bereaved people – sensitively and with understanding that many will not wish to participate.
However, the National Medical Examiner’s good practice paper 12 published by the Royal College of Pathologists asks medical examiner offices to consider feedback. One office reported that of 53 responses to its survey, 90% felt the interaction with the medical examiner office was helpful and 94% that causes of death had been explained in a clear way.
Medical examiner offices in England are now required to report the number of complaints they receive about their service to the National Medical Examiner’s office.
For the first full quarter (October to December 2024) only 102 ‘complaints’ were received in England (0.08% of deaths scrutinised) and this number consists of both minor concerns and formal complaints as the reporting threshold is low.
Complaints are for local response and resolution and the National Medical Examiner’s office does not have access to individual records, limiting the opportunities for analysis of what complaints relate to.
It was only possible to determine whether the complaint related to the medical examiner office or some other element in the death certification and registration system in around half the reports, but nearly three-quarters of these related to matters outside medical examiner office control, particularly delays arising from waiting for attending practitioners to complete MCCDs or coroners to determine whether they have a duty to investigate a death.
In Wales there were 16 complaints in 2024. Of these, 5 related to delays related to scrutiny or service, and 4 to delays that were outside the medical examiners’ control. Others related to various concerns including coroners declining to investigate, information documented in medical records taken into account by the medical examiner and other diverse matters.
The collaboration between medical examiners, bereavement services, Imams and mortuary staff has been nothing short of remarkable…Feedback from the Muslim community and funeral directors has been overwhelmingly positive.
(Funeral/bereavement service CEO)
Urgent scrutiny
In some cases urgent scrutiny is required. The National Medical Examiner’s good practice paper on urgent release of bodies (2021) makes clear that medical examiner offices must ensure their ways of working reflect the needs of local communities.
In many cases there is no barrier to releasing a body before the MCCD is completed. However, mortuaries each make their own interpretation of their duties regarding the care and dignity of the deceased and must comply with relevant requirements published by the Human Tissue Authority.
“Without the help we received from medical examiner offices like yours, brain donations would not be possible and research into neurodegenerative conditions would be slower.” (organ donation team)
Medical examiner offices that face high demand for urgent scrutiny may need to extend their opening hours beyond the normal working days, while ad hoc arrangements may be a more efficient use of resources for those that do not.
At December 2024, 73 medical examiner offices in England reported they operated extended hours of working, such as weekday evenings or weekends.
In Wales, each hub office is open on public holidays (except Christmas Day) and has a medical examiner and officer available at weekends.
“I do my work in a predominantly Jewish area and look after a Jewish care home in addition to my GP work.
“As an orthodox Jewish GP in this area, I was very hesitant about what the new service and legislation would mean for both myself as a GP as well as my community.
“I have had numerous interactions with the service in the past months and each time I am astounded by how wonderful it is.”
(GP)
Medical examiner offices in England reported they achieved the requested time in 7,447 cases (88%) in 2024.
Data from October to December 2024 provided the first opportunity to evaluate the reasons why a minority of requests for urgent scrutiny were not fulfilled. These were largely beyond the control of the medical examiner office:
- In 5.6% because cases had potential concerns or complexities – for example, requiring coroner notification.
- In 3.7% because the attending practitioner was unavailable to complete the MCCD.
- In 2% because medical examiners were waiting for attending practitioners to provide patient records.
- Other reasons accounted for less than 1%.
NWSSP reported no cases in Wales where they were unable to achieve scrutiny in the time requested. The proposed digital MCCD could potentially reduce delays and improve the data available for analysis of causes when urgent scrutiny cannot be achieved.
Notifications to coroners
Medical examiners reported notifying 35,359 deaths (9.3%) in England and 4,926 deaths (22.3%) in Wales to coroners after scrutiny.
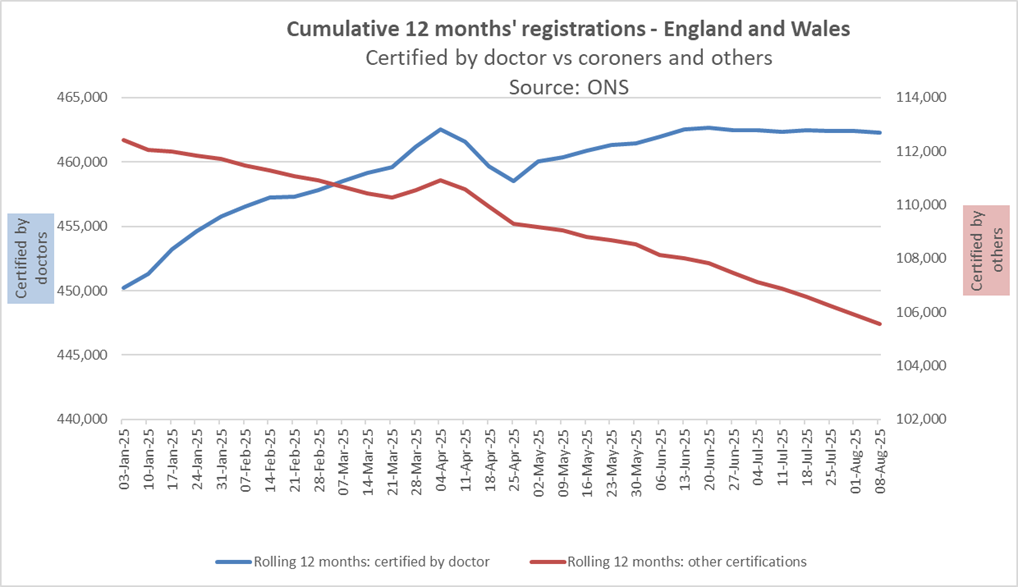
The introduction of medical examiners has significantly reduced the number of deaths notified to coroners in England and Wales, with a shift from certification of deaths by coroners to certification by doctors. ONS data indicates that deaths certified by doctors are typically registered much more quickly than those certified by coroners.
Although the death certification reforms were only in force for the final third of 2024, the Ministry of Justice reported a 10% reduction in deaths reported to coroners in in England and Wales in 2024 compared to 2023 (source: Coroners statistics 2024). We expect the number will fall even more sharply in 2025, the first full year under the new arrangements.
As a proportion of the number of deaths registered, those referred to coroners has also declined: from 36% in 2022 to 31% in 2024 and with a further decline expected in 2025. This represents a reduction in unproductive referrals and unnecessary bureaucracy that often delayed registration and caused distress to the bereaved.
The proportion of deaths reported to coroners for which no inquest is held has also fallen steadily; from 81% in 2020 to less than 75% in 2024. Many factors may have influenced this trend, but one will be the role medical examiners have played since 2020 in ensuring more consistent notifications to coroners and avoiding unnecessary referrals.
Figure 1: Deaths reported where no inquest occurred
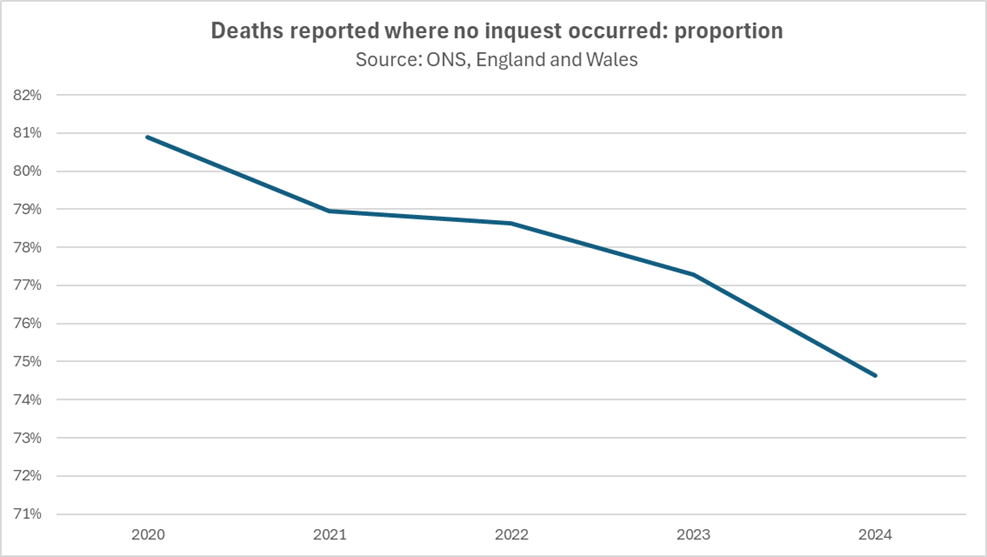
Of course, some deaths will continue to be reported directly to coroners without medical examiner involvement. Similarly, there will continue to be some deaths reported to coroners where no inquest occurs; for example, in a proportion of deaths which doctors must report under Notification of Deaths Regulations 2019, coroners decide their duty to investigate is not invoked.
A minority of coroners may also instruct doctors to notify them of classes of deaths over and above those specified in these regulations.
In Wales, the medical examiner service works with 7 coroner areas. The rate of referral is influenced by local population demographics (for example, prevalence of industrial disease) and different hospital settings. Some coroners also have varying approaches to individual circumstances.
Some of the benefits and improved efficiency in the new system are difficult to measure or describe succinctly. It is therefore welcome that there appears to be a shift in the number of deaths being registered by coroners, with more being certified by doctors.
This adjustment will take time to work through and for the impact to be fully visible, as deaths certified by coroners take longer to be registered, and some deaths notified to coroners before 9 September take time to complete the process.
ONS data indicates the times taken for deaths certified by doctors to be registered are typically much shorter than those certified by coroners, and over time an increasing proportion of deaths are being certified by doctors.
Figure 2: Cumulative 12 months’ registrations – England and Wales
“In separate incidents, serious concerns were raised by the bereaved about 2 deaths (one in the community and one in an acute trust). These were discussed with the coroner and subsequently reported to the police.
“A medical examiner office was instrumental in raising concerns about 2 care homes, with one review leading to a police investigation.”
(Regional medical examiner)
Medical Certificates of Cause of Death
DHSC previously commissioned work to introduce a digital MCCD to support the new process. However, technical challenges could not be surmounted before September 2024 and the death certification reforms were implemented with a paper MCCD still to be used.
DHSC ensured that all healthcare providers had adequate supplies of the new MCCD in advance of 9 September 2024. This was a significant undertaking and challenge but was accomplished successfully by officials.
The continued reliance on a paper form required the development of processes to transfer MCCDs securely between healthcare providers and medical examiner offices, and the agreement of arrangements for amending MCCDs when required.
Medical examiners and officers led this work locally and agreed processes with register offices, coroners, healthcare providers and other partners.
After initial problems in some areas after 9 September 2024, further guidance was issued to register offices, coroners and medical examiners.
An effective digital MCCD, when and if it can be introduced, will make the entire registration process significantly more efficient.
Sharing patient records between healthcare providers
Attending practitioners must provide medical examiners with relevant patient records along with the MCCD, and medical examiners are required to make the enquiries they consider necessary.
All medical examiner offices have developed their own arrangements for the receipt of or access to patient records, reflecting the IT systems and processes used locally.
These arrangements are working adequately but the increased use of electronic records and improved digital connectivity across the NHS are needed to make it easier for attending practitioners to share patient records with medical examiners.
In 2025, it became apparent that medical examiners in England can only access some parts of shared care records – the social care records – if the attending practitioner first reviews them and then shares them with the medical examiner, potentially hindering efficient and effective scrutiny in some cases.
Addressing this obstacle may require a change to regulations.
Without change, medical examiners are constrained in making enquiries and there is potential for matters of concern to come to light after medical examiners have completed their scrutiny, risking avoidable additional distress to bereaved people and complaints.
Removal of implantable medical devices
MCCD guidance notes that any hazardous medical device must be removed from a body before it is released for cremation or burial, and the attending medical practitioner is responsible for identifying whether such devices are present and have been removed.
The Royal College of Pathologists published a good practice paper in June 2025 to underline that responsibilities for identifying hazardous implantable devices lie with attending practitioners, and described the processes now that the Cremation 4 form has been discontinued.
However current arrangements have proved less than ideal in some cases and require further work by national and local partners.
Crematorium medical referees and funeral directors can find it hard to identify and contact the attending practitioner responsible for the information provided. In many cases they turn to medical examiners and officers who do not have this responsibility, may not have access to required records, and face additional unforeseen workload as a result.
Local partners should work constructively to ensure their processes are as effective as possible, and medical examiners are supporting these local discussions, but DHSC, Welsh Government, NHS England, the General Register Office and the Ministry of Justice may need to further consider the national framework.
Workforce and training
Medical examiners and officers are employed by NHS trusts in England and by NHS Wales Shared Services Partnership in Wales. Medical examiners’ terms of appointment were provided to the NHS bodies employing them in advance of the changes on 9 September 2024.
DHSC’s 2018 impact assessment assumed that 1 full time equivalent (FTE) medical examiner and 3 FTE medical examiner officers would be required for every 3,000 deaths, though some adjustment is required for viable working arrangements in individual circumstances.
For 2024/25, NHS England assessed the requirement was 182.1 FTE medical examiners and 527.8 FTE medical examiner officers in England.
At 31 December 2024, medical examiner offices in England reported that 185.5 full-time equivalent (FTE) medical examiners and 508.3 FTE medical examiner officers were in post. In Wales there were 13 FTE medical examiners and 39.5 FTE medical examiner officers.
The provisional number of deaths reported by ONS for 2024 and number of deaths scrutinised by medical offices in 2024 are generally in line with expectations.
However, around the time of transition to the new processes, a few offices in England found themselves with more deaths to review than anticipated.
In some areas coroners required that medical examiners review all deaths before referral, which is not in keeping with the intention of the death certification reforms or guidance from the National Medical Examiner or the Chief Coroner.
Regional medical examiners have explored solutions with offices in England experiencing higher activity, including re-allocating healthcare providers between offices to achieve more balanced activity levels, and discussed resources with NHS trusts, ICBs and NHS regions. This matter will be kept under review.
The supply and focus of medical examiner officers should also be monitored. The workforce, while still fledgling, is maturing and naturally some turnover is occurring. Individual offices do at times have vacancies and some report these can be challenging to recruit to as with a limited supply pipeline they have few applicants.
Some medical examiner offices have been asked to merge with other functions, particularly bereavement teams. While the pursuit of efficiencies is understandable given the pressures on NHS services, the National Medical Examiner’s guidance notes that merged roles are problematic.
NHS trusts and ICBs must maintain adequate medical examiner officer resource and that changes do not compromise independence and satisfy information governance requirements.
Through 2024 the Royal College of Pathologists continued to provide training days for medical examiners and medical examiner officers.
A further 376 senior doctors were trained as medical examiners during 2024, bringing the total for England and Wales to 2,466, and 796 staff have been trained as medical examiner officers.
The Royal College of Pathologists has been increasing opportunities for continuing professional development and launched a forum for the profession.
It should be recognised that this dedicated workforce is still in its infancy. The winter was challenging for morale, particularly where stakeholders or commentators attributed issues to medical examiner offices which were beyond their control.
Support must be maintained to enable medical examiners and officers to deliver the objectives for which they were appointed.
Inquiries
The Thirlwall Inquiry into the deaths of babies at Countess of Chester Hospital asked the National Medical Examiner to provide a witness statement and to appear as a witness.
These tragic deaths occurred before implementation of the medical examiner system on a non-statutory basis commenced in 2020, and long before the death certification reforms were implemented in 2024.
However, the hearing provided an opportunity to consider the arrangements which commenced in 2024, the tools available for medical examiners, and what difference medical examiners could make if similar distressing events were to emerge elsewhere.
A refresh of the Royal College of Pathologists’ good practice paper on deaths of children and neonates had commenced earlier in 2024 to reflect the death certification reforms, and in parallel work began on a new e-learning module for medical examiners on the same topic.
The updated good practice paper was published in February 2025, and the e-learning module is likely to be released around the time this report is published.
In 2025 the Lampard Inquiry also asked the National Medical Examiner to provide a witness statement, which is being finalised at time of drafting this report.
Funding for medical examiner offices
The cost of employing medical examiners and officers is met from NHS budgets in England and DHSC’s departmental budget for Wales. Overall their work benefits the public purse by reducing deaths reported to coroners (funded by local authorities).
NHS England introduced a new funding mechanism for English medical examiner offices for 2024/25. The formula to calculate the funding for each office factored in the anticipated number of deaths for each office (NHS England assessment), corresponding staffing requirement (DHSC impact assessment), and likely demand for urgent scrutiny and cover for weekends and bank holidays.
The full amount was distributed through ICBs’ Service Development Funds (SDF) on the basis that it should be made available to trusts and medical examiner offices through contractual arrangements.
For 2025/26, NHS England has de-ringfenced many elements of ICBs’ SDF, including the work of medical examiners, but finance technical guidance states that “ICBs and NHS trusts (unless the NHS trust has agreed otherwise with the National Medical Examiner) are required to provide resources for an appropriately staffed and resourced medical examiner office, as required within the standard NHS contract.”
Generally, this is working satisfactorily, though national and regional teams have received some requests for support to secure resources.
NHS trusts and ICBs must adequately resource medical examiner offices to ensure they can deliver their statutory function to the standard bereaved people deserve.
Conclusion
In closing, 2024 proved a very significant year as proposals dating back to the Shipman inquiry were finally implemented.
It is encouraging that feedback to medical examiner offices continues overwhelmingly to be positive, and that many medical examiner offices report improving working arrangements with partners in the death certification and registration system. This demonstrates the value of local stakeholders working together constructively in the interests of bereaved people.
However, not all areas saw consistent improvements and there is more to do. Improvements depend on local partners such as attending practitioners, coroners and register offices as well as medical examiners.
In England, ICBs and NHS trusts, and in Wales, health boards, also have their role to play in ensuring the statutory services for which they are accountable are adequately supported.
Publication reference: PRN01922

