Summary
The 76-year history of the NHS has been one of progress and transformation – as society, technology and medicine change, so does our health service. But today the NHS must build momentum towards long-term solutions while managing the very real pressures on it – a legacy of the historical context set out by the Darzi Review. While headline performance is far from what any of us want to see, we know NHS staff continue to improve the services patients most value.
Our ambition is clear – to see high performing systems across the country, and we will support local leaders to transform services to secure long-term success.
We have heard loud and clear from you that our approach to oversight and performance improvement needs to be consistent and our interactions coherent. You have told us that the proposals which we consulted on in summer 2024 could be improved to be less complicated and burdensome. Taking this feedback onboard, we have developed our new assessment approach to provide more consistency and transparency on delivery scores following engagement with government, this means that segmentation will now be solely linked to delivery metrics. Discussions about performance will be led by colleagues at NHS England who are experienced in addressing delivery challenges, with a focus on offering you practical, informed evidence and guidance that is grounded in a deep understanding of the operational challenges you face.
Our assessment will be the starting point for how we work with you throughout the year and will help determine how we can support you to improve. In determining our response, to improvement we will consider the organisation’s segment score, as set out in this framework, and leadership capability. We have stated clearly what the delivery metrics are for each part of the system to ensure we have an agreed view of what good looks like and fully align with the priorities and operational planning guidance.
Improvement remains the responsibility of all boards, and all organisations are expected to have an improvement methodology in place and suitably sized improvement programme for the scale and complexities faced
The framework outlines the circumstances in which increased freedoms can be obtained and how we will consider whether an integrated care board (ICB) or provider’s performance falls below an acceptable standard and/or there are governance concerns which may lead to NHS England stepping in and using our regulatory powers to secure improvement (NHS England’s approach to the use of enforcement powers is set out further in the NHS enforcement guidance). When we do this, we will do so transparently and in a consistent way across the country.
The move to a new assessment approach means we are changing many aspects of how the system works together. We have begun this with the publication of our priorities and operational planning guidance, and we aim to have this way of working more broadly in place by the beginning of July. To do this we are committing to:
- streamline oversight: providing consistent and co-ordinated oversight to reduce duplication and prevent providers from being bombarded with conflicting instructions
- focus on performance improvement: supporting providers to achieve sustainable improvement by prioritising actionable must-dos and offering constructive challenge to drive positive outcomes
- strengthen systems and infrastructure: providing data tools and platforms that enable local analysis to drive informed decision-making, continuous improvement and effective performance management
- foster collaboration and trust: engaging with providers, ICBs and stakeholders in a way that builds trust and alignment so that shared goals are achieved in an efficient way
- embed sustainable local practices: working collaboratively on improvements that can be managed and embedded locally, minimising the reliance on external interventions or support.
Performance assessment
Roles and responsibilities
Integrated care boards (ICBs):
- responsible for achieving the 4 principal Integrated Care System (ICS) purposes: improving population health and healthcare; tackling inequalities in outcomes, experience and access; enhancing productivity and value for money; and supporting social and economic development
- statutory responsibility for arranging local services through effective strategic commissioning
- hold their partners in the ICS to account using the system levers that bind them together, such as their joint system plans, partnership agreements, joint committees and collaboratives
Providers (NHS trusts and foundation trusts):
- provide high quality and safe services as contracted
- comply with the requirements of the NHS Provider Licence, including in relation to quality governance
NHS England:
- statutory responsibility for overseeing overall delivery, performance and improvement of ICBs and providers
- conducts an ICB performance assessment each financial year* using the ICB’s segment and capability assessment
- determines the segment for each organisation
- determines how to support and drive improvement in each organisation
* NHS England is not legally required to conduct a performance assessment for providers it incorporates Care Quality Commission (CQC) findings when it assesses providers’ performance.
NHS England uses the assessment process to measure delivery against an agreed set of measures and identify where improvement is required. This determines a segment for each organisation. The appropriate response to secure improvement is then informed by the organisation’s capability assessment. The approach to capability assessment is currently being finalised and the intention is to align our approach with the CQC.
All organisations should be aiming to improve across all areas of national priority as well as support their system to deliver integrated care that meets the needs of the local population. The assessment model is built around the four principal purposes of an integrated care system (ICS) and an organisation’s delivery of sustainable improvement against the short-term priorities in the priorities and operational planning guidance.
The four purposes align with scoring domains that combine a set of high-level metrics at ICB and provider level (Table 1). Individual types of organisations (ICBs and acute, mental health, community and ambulance providers*) are measured against a range of appropriate metrics across these domains to judge their delivery of the overall NHS priorities. Guidance on the composition of the metrics is provided in Annex A. These metrics will be reviewed annually to ensure they align with any shifts in national priorities.
* Primary care providers, primary care networks (PCNs) and other non-trust providers or partnerships, such as provider collaboratives, are not allocated their own segments.
Table 1: ICS purposes and the assessment domains
| Purposes | Domains and sub-domains |
|---|---|
| Improve population health and healthcare | Operating priorities: – urgent and emergency care – elective care – cancer care – mental health care – care for those with learning disabilities or who are autistic – primary care Outcomes: – improving population health – prevention of ill health – management of long term conditions |
| Tackle inequalities in outcomes, experience and access | Quality and inequalities: – experience – safety – reducing inequality – workforce and people |
| Enhance productivity and value for money | Productivity and value for money: – finance – productivity |
The fourth purpose of an ICS – improving social and economic value – is not a domain due to its longer-term and multilateral nature; instead, it is incorporated into organisational capability ratings.
Segmentation approach
Every ICB and provider will be allocated a segment. This indicates its level of delivery from 1 (high performing) to 4 (low performing), and informs its support or intervention needs. A diagnostic will be performed on all segment 4 organisations to identify those with the most intense support needs, these organisations will enter the recovery support programme and allocated a segment of 5. (See Table 2 for segment descriptions).
- Each organisation will receive an individual organisational delivery score derived from performance against the metrics listed in annex A. Metrics are combined into the assessment domains and consolidated into short and medium-term scores. These are then combined to make the overall score.
- For ICBs an additional system adjustment may be applied where performance against the system-level metrics (system considerations) listed in annex A, that align to system-wide delivery of major national priorities, is challenged. The system adjustment is combined with the organisational delivery score to give a picture of how the commissioning organisation is performing together with its delivery system.
Figure 1: Process for determining an ICB’s segment
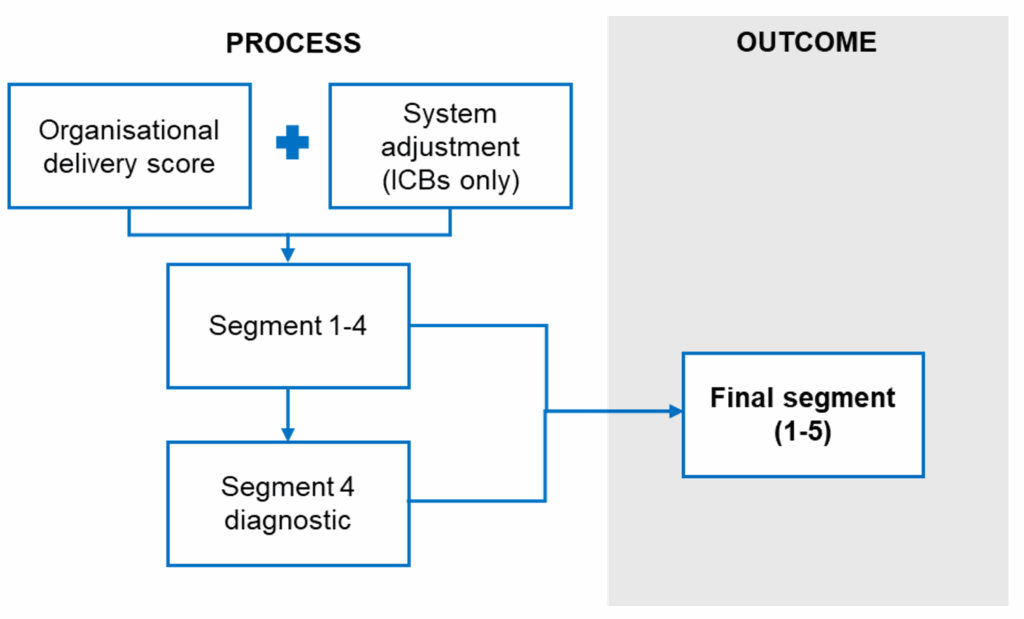
While segmentation scores for providers will be based on the organisational delivery score only and are not adjusted for system considerations, the extent to which providers are effectively collaborating and supporting system working will form part of the provider capability assessment.
The specific metrics housed under each domain are reviewed on an annual basis and are set out in annex A, further detail on the scoring approach is included in the separate methodology manual [to follow].
Each metric has an individual set of scoring rules that enable organisations to receive a score between one and four. The specific scoring regime for each metric is detailed in full in a separate technical document [to follow]. These scores are aggregated together to form domain scores which contribute to a short and a medium-term delivery score that together form the overall organisational delivery score.
As part of the scoring methodology an override will be applied relating to finance. The override will mean that organisations in deficit will have their overall segment score limited to 3.
Organisations with a segment of 4 under this framework will receive a diagnostic as set out in annex B, this will determine whether they will enter segment 5 and receive support under the Recovery Support Programme (RSP) (see annex C). For organisations currently in RSP it is expected that they will automatically transition into segment 5.
Once NHS England has approved the final segmentation decision, this is officially conveyed to the organisation and published on NHS England’s website.
Segments for all ICBs and providers are reviewed at least quarterly as part of a review meeting but may be updated at any time based on emerging information.
Segmentation response
Segmentation will inform NHS England’s performance improvement response which will also take into account our assessment of ICB and provider capability. The details of our approach to capability assessment and improvement response will be included in further guidance due to be published shortly.
Segment 4 diagnostic
All ICBs or providers in segment 4 will have a diagnostic review (see annex B) where all available data and insights will be used to assess their underlying challenges and support needs. This will lead to some organisations being considered for the Recovery Support Programme (RSP) – the most intensive support intervention (see annex C).
An organisation’s entry into the RSP is based on our consideration of the scale of the issues identified through the segmentation process and the further diagnostic review, the nature of those issues (such as care quality, financial stability and leadership) and the capacity and capability to address them. The relevant governance group will approve any decision to enter an organisation into the RSP and the organisation will be allocated a new designation of segment 5.
Tables 2: Segment descriptions
Segment 1
| Description | How NHS England support | How NHS England drives improvement | How NHS England intervenes |
|---|---|---|---|
| The organisation is consistently high-performing across domains, delivering against plans. It has a track record of successful delivery. | No specific support or intervention needs are identified. Expected to set up own support plans. | The organisation works alongside NHS England to develop best practices and improvement initiatives in areas that it excels in. | The use of our enforcement powers is not usually expected for organisations in this segment due to their lack of intervention or support needs but if necessary enforcement action can still be taken. |
Segment 2
| Description | How NHS England support | How NHS England drives improvement | How NHS England intervenes |
|---|---|---|---|
| The organisation has good performance across domains. Specific issues exist with plans in place that have the support of system partners | The organisation can diagnose and clearly explain its support needs, which is predominantly supplied locally. Our support on specific issues is provided where appropriate. | The organisation works with us to support the development of best practices in areas it shows high performance in. Targeted support is aimed at improving specific pathways where issues have been identified. | Due to the relatively high-performing nature of the organisation and its level of maturity, the use of enforcement powers is not common but may be used where specific issues call for this approach |
Segment 3
| Description | How NHS England support | How NHS England drives improvement | How NHS England intervenes |
|---|---|---|---|
| The organisation and/or wider system are off-track in a range of areas. | Support needs are between NHS England and the organisation (for providers this also includes its relevant ICB) and delivered through local support offers, defined national support programmes and bespoke regional interventions | The organisation receives increased scrutiny targeted at delivering improvement in challenged performance areas. | NHS England may apply interventions and/or require the organisation to take action in specific areas of poor performance. This may involve use of enforcement action, particularly where performance concerns continue. |
Segment 4
| Description | How NHS England support | How NHS England drives improvement | How NHS England intervenes |
|---|---|---|---|
| The organisation is significantly off-track in a range of areas. Application of the diagnostic did not identify a need to enter the Recovery Support Programme (RSP). | NHS England will consider the organisation’s challenges and support needs to inform the appropriate support or intervention. Support needs are prioritised through local support offers, defined national support programmes and bespoke regional interventions. | The organisation receives significant scrutiny targeted at delivering improvement in the most challenged performance areas. Recovery KPIs and trajectories are agreed and proactively monitored | NHS England may apply interventions and/or require the organisation to take broad actions or address specific concerns related to diagnosed issues. This may involve the use of enforcement action, particularly to secure improvement or where improvement is insufficient. |
Segment 5
| Description | How NHS England support | How NHS England drives improvement | How NHS England intervenes |
|---|---|---|---|
| Following a diagnostic, the organisation’s entry into the RSP is considered necessary to address serious failures of patient safety, quality, finance, leadership and/or governance. | NHS England appoint an improvement director to intensively support the organisation to meet improvement goals. The programme supports the ICB or provider in undertaking a full diagnostic to identify support needs and develop a full recovery plan in collaboration with system partners and agree transition criteria | The organisation is subject to the highest level of NHS England scrutiny and performance management to meet agreed transition criteria demonstrating sustainable levels of improvement to leave the programme | Alongside entry into the RSP, enforcement action may also be agreed through the relevant executive governance group if deemed necessary. Transition out of segment 5 requires transition criteria to be met |
Publication of data
To support transparency, NHS England will publish a new interactive scorecard later this year with organisations’ delivery scores and final segmentation along with benchmarking data and ICB and provider capability ratings. This data will be updated quarterly.
Emerging information and capability assessments
As part of the assessment process, insights will be gathered across the assessment domains. This mix of quantitative data and qualitative information will be collected annually, in-year or by exception.
Qualitative information may be derived from:
- ICBs and providers as part of routine interactions, for example around emerging financial risks or clinical quality risks in line with the National Quality Board guidance on risk response and escalation
- reports from other regulators such as the CQC, including ICS assessments and internal and external audit reports
- third-party information, for example, from 360-degree feedback, peer reviews, complaints or formal publications/assessments
Alongside, NHS England will work with regulators including the CQC, Health and Care Professions Council, General Medical Council (GMC) and Nursing and Midwifery Council (NMC) through the national and regional Joint Strategic Oversight Group (JSOG). This group provides a space for regulators to share intelligence and develop aligned approaches to support organisations.
This information is assessed as part of the separate capability assessment process and subsequent capability rating. Guidance on this process is under development and will be published in due course as part of our wider improvement approach, and the results will be used by NHS England alongside segmentation scores to direct our performance improvement activities to the organisations who have poor performance and lack the capability to improve without support.
Critical to the assessment approach is identifying emerging issues and concerns early so they can be addressed before they have a material impact or performance deteriorates further. Organisations should not wait for the assessment process to acknowledge performance, finance or quality concerns, ICBs, and providers through ICBs*, should promptly escalate all issues that are significantly affecting these areas to their NHS England regional team.
* The ICB to which the provider is allocated is the same as that for financial control purposes as set out in the NHS Data Service Directory. For ambulance services, ICBs should follow the guidance on the commissioning of ambulance services.
Oversight of delegated commissioning
Where NHS England has delegated responsibility to ICBs for commissioning services – certain specialised services and all primary care services (primary medical care, dentistry, pharmacy and ophthalmic services) – and the handling of associated complaints, NHS England remain accountable for these services. NHS England will hold ICBs to account for the performance of these services in their system through delegation agreements.
Oversight of delegated functions will form part of NHS England’s wider oversight of ICBs. In particular, NHS England will use the ICB capability assessment process to judge whether delegated commissioning activities and associated complaints handling are being carried out appropriately. This may involve monitoring additional data in relation to delegated services in-year.
Incentives and consequences
NHS England is committed to supporting providers and ICBs to drive improvement and deliver high quality care for all.
The ambition is to see high performing systems across the country and to embed earned autonomy and incentives into the operating framework. There has already been progress with fewer national priorities in the planning guidance to increase local flexibility in decision making.
Moving forward, NHS England will work closely with highly capable organisations, who are high scoring in both their segment and their capability rating, and draw on their expertise to shape and drive national policy and to test new models of care. NHS England will also introduce greater incentives for performance in 2025/26.
To incentivise revenue performance, the 2025/26 capital planning guidance proposes that high-performing providers and ICBs, who are demonstrating effective governance, strong financial management and operational resilience, will receive some freedoms and flexibility, including a partial release of revenue surpluses for capital expenditure. As set out in the Elective Reform Plan, NHS England also intends to introduce capital incentives for improvements in elective performance.
NHS England will work with ICBs and trusts to agree the appropriate response to a particular segmentation. This will take into account their capability rating and consider enhanced oversight arrangements, and targeted support intervention.
Where NHS England has specific concerns about an organisation, the actions it may consider taking to address the situation include:
- significant concerns about an organisation’s ability to deliver a specific improvement or recovery plan on its own: NHS England may consider requiring it to take on the necessary expertise to do so – for example, diagnosing the issues and/or addressing them
- significant concerns about leadership at a provider or ICB: NHS England may consider taking steps to remove/replace executive or non-executive board members
- significant concerns about an ICB’s ability to carry out certain functions: NHS England may consider directing specific remedial action, carrying out these functions on behalf of the ICB or transferring responsibility for them to another ICB.
Enforcement
NHS England’s oversight of ICBs and providers may involve the use of regulatory powers to take enforcement action, in line with the NHS enforcement guidance, against a provider if there is a suspected or actual breach of its licence or against an ICB if it is failing or at risk of failing to meet its duties.
NHS England has a range of statutory powers to address serious issues at ICBs and providers. Where assessment and monitoring highlight concerns with performance, and after further enquiries or investigation, NHS England may use its powers as set out in the NHS enforcement guidance to address the issue, according to the level of concern. Use of these enforcement powers is not appropriate for organisations in segment 1 and should they be deemed necessary; segmentation would be reviewed at the same time.
Where organisations are found to be persistently underperforming in relation to a statutory function or their obligations under their provider licence NHS England may use powers including:
- ICB undertakings – where NHS England has reasonable grounds to suspect failure to discharge a function, the ICB can offer to take specific corrective actions to address identified issues and ensure compliance with its statutory responsibilities. NHS England may agree undertakings to secure progress where ICBs are capable of resolving performance issues themselves.
- Provider undertakings – can be used where NHS England has reasonable grounds to suspect that a provider has failed to meet the conditions of its provider licence. NHS England may agree undertakings to secure progress where providers are capable of resolving performance issues themselves.
- Discretionary requirements – can be imposed to require the remedy of a breach of a provider’s licence where NHS England is satisfied that a breach has occurred. NHS England may consider imposing discretionary requirements to ensure that progress is made and where NHS England does not have confidence the provider is taking sufficient action to resolve performance issues.
Where there is evidence of significant or persistent failure to perform statutory functions properly NHS England has powers of direction over ICBs. Those taken may include:
- requiring the organisation to take specific actions to address failures or resolve issues
- directing the organisation to cease certain functions and transferring responsibility for them to another party
- directing leadership changes: terminating the appointment of the chief executive, or requiring the removal or replacement of other senior executives or board members* where leadership or governance failures are identified as contributing to a failure to perform functions properly.
* NHS England also has the power to remove ICB chairs.
NHS England has powers in relation to NHS trusts, which may be used in appropriate cases to effect executive leadership change, and the power to remove chairs and non-executive directors. For NHS foundation trusts, NHS England can also impose additional licence conditions relating to governance or quality issues, breach of which may then lead to leadership change.
NHS England may consider using our powers of direction or additional licence conditions in more serious cases of governance failure.
More information can be found in the NHS enforcement guidance, including how NHS England chooses which powers to use and when, the factors to consider when enacting them and how to ensure consistency in approach.
Annex A: Delivery metrics
Delivery segments are determined by routinely considering a range of metrics at organisational level connected to shared NHS priorities.
This document sets out the headline delivery metrics that underpin the segmentation scores for each organisation. These scores taken together, translate to a provisional oversight segment, designed to guide discussions between NHS England and organisations to reach a final segmentation judgement.
These high-level metrics are aligned to the 4 core purposes of an ICS as set out in Table 1 and are designed to reflect both short-term operational priorities and medium-term strategic transformation goals. While they indicate areas of potential challenge, they should not be used in isolation, all parties should consider a broader range of measures, including those detailed in the Insightful Board frameworks, to provide a comprehensive view of performance and improvement needs when undertaking oversight activity.
Table 3: 2025/26 operating priorities
These metrics relate to the national objectives set out in the priorities and operational planning guidance for 2025/26 and other commitments relating to the NHS Constitution.
Elective care
| Metric | Organisations to which the metric relates |
|---|---|
| Annual change in the size of the waiting list | Integrated care boards |
| Percentage of patients treated within 18 weeks | Acute trusts |
| Percentage of patients waiting over one year | Acute trusts |
| Estimated time it would take to clear the waiting list if no new patients were added | Acute trusts |
| Percentage of all cancers diagnosed that are diagnosed at stage 1 or 2 | Integrated care boards |
| Percentage of urgent referrals to receive a definitive diagnosis within 4 weeks | Acute trusts |
| Percentage of patients treated for cancer within 62 days of referral | Acute trusts |
Cancer care
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of all cancers diagnosed that are diagnosed at stage 1 or 2 | Integrated care boards |
| Percentage of urgent referrals to receive a definitive diagnosis within 4 weeks | Acute trusts |
| Percentage of patients treated for cancer within 62 days of referral | Acute trusts |
Urgent and emergency care
| Metric | Organisations to which the metric relates |
|---|---|
| Number of bed days per 100,000 head of population | Integrated care boards |
| Percentage of emergency department attendances admitted, transferred or discharged within four hours | Acute trusts |
| Percentage of emergency department attendances spending over 12 hours in the department | Acute trusts |
| Average Category Two ambulance response time | Ambulance trusts |
People with a learning disability or who are autistic
| Metric | Organisations to which the metric relates |
|---|---|
| Change in the number of inpatients who are autistic or have a learning disability | Integrated care boards |
Mental health care
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of adult inpatients discharged with a length of stay exceeding 60 days | Mental health trusts |
| Number of mental health bed days per 100,000 head of population | Integrated care boards |
Primary care
| Metric | Organisations to which the metric relates |
|---|---|
| Growth in the number of emergency dental appointments provided | Integrated care boards |
| Percentage of patients who describe their experience of their GP as good | Integrated care boards |
Table 4: Finance and productivity metrics
These metrics will be used to judge organisational financial delivery.
Financial balance
| Metric | Organisations to which the metric relates |
|---|---|
| Planned surplus/deficit | Integrated care boards and all trusts |
| Variance year-to-date to financial plan | Integrated care boards and all trusts |
| Level of confidence in delivery of financial plan | Integrated care boards and all trusts |
Productivity
| Metric | Organisations to which the metric relates |
|---|---|
| Rate of productivity | Integrated care boards and acute trusts |
| Comparative difference in costs | All non-acute trusts |
Table 5: Public health and patient outcome metrics
These metrics relate to longer term priorities such as patient outcomes, prevention and inequality as well as cultural and experience measures.
Outcomes
| Metric | Organisations to which the metric relates |
|---|---|
| Average number of years people live in healthy life | Integrated care boards |
| Deaths as a result of venous thromboembolism related events within 90 days of hospital discharge | Integrated care boards |
| Percentage of deaths with three or more emergency admissions in the last 90 days of life | Integrated care boards |
| Percentage of patients over the age of 65 in their own home 91 days after being discharged from hospital (to be confirmed) | Integrated care boards |
| Percentage of patients admitted as an emergency within 30 days of discharge | Acute and community trusts |
| Summary Hospital Level Mortality Indicator | Acute trusts |
| Average number of days between planned and actual discharge date | Integrated care boards and acute trusts |
| Percentage of patients who do not meet the criteria to reside | Community trusts |
| Percentage of ambulance incidents which do not result in a hospital conveyance | Ambulance trusts |
| Percentage of talking therapies patients achieving reliable recovery | Mental health trusts |
| Percentage of eligible children to receive two doses of the MMR vaccine by age 5 | Integrated care boards |
Prevention of ill health
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of eligible patients to receive cervical screening | Integrated care boards |
| Percentage of eligible patients to receive breast screening | Integrated care boards |
| Percentage of eligible patients to receive bowel screening | Integrated care boards |
| Percentage of pregnant women supported to quit smoking | Integrated care boards |
| Percentage of inpatients referred to stop smoking services | Acute and mental health trusts |
| Percentage of patients supported by obesity programmes | Integrated care boards |
| Percentage of patients at risk of cardiovascular disease treated with lipid lowering therapies | Integrated care boards |
| Percentage of patient-facing staff to receive a flu vaccination | All trust types |
| Percentage of people waiting over six weeks for a diagnostic procedure or test | Acute trusts |
Managing long term conditions
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of hypertension patients treated to target | Integrated care boards |
| Percentage of diabetes patients to receive all eight care processes | Integrated care boards |
Table 6: Quality and inequalities metrics
Patient safety
| Metric | Organisations to which the metric relates |
|---|---|
| NHS staff survey raising concerns sub-score | Integrated care boards and all trusts |
| CQC safe inspection score | All trusts |
| Rate of inpatients to suffer a new hip fracture (to be confirmed) | Acute trusts |
| Rate of inpatients to suffer a new pressure ulcer | Acute trusts |
| Rates of MRSA, C-Difficile and E-Coli | Acute trusts |
| Percentage of children prescribed antibiotics in primary care | Integrated care boards |
| Number of neonatal deaths and stillbirths per 1,000 total births | Integrated care boards |
Patient experience
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of patients able to see their preferred primary care professional | Integrated care boards |
| Percentage of standard Continuing Healthcare referrals complete within 28 days | Integrated care boards |
| CQC inpatient survey satisfaction rate | Acute trusts |
| National maternity survey “looking after you” sub score | Acute trusts |
| Rate of restrictive intervention use | Mental health trusts |
| Percentage of patients waiting over 52 weeks for community services | Community trusts |
| Annual change in the number of diagnostic tests booked directly by GPs per 100,000 people | Integrated care boards |
| Percentage of patients referred to crisis care teams to receive face to face contact within 24 hours | Mental health trusts |
| Change in the number of people accessing community mental health services with serious mental illness | Mental health trusts |
| Number of mental health patients spending over 12 hours in A&E | Acute trusts |
| Percentage of people with suspected autism awaiting contact for over 13 weeks | Community trusts |
Workforce and people
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of NHS Trust staff to leave in the last 12 months | Integrated care boards and all trusts |
| Percentage of GPs to leave in the last 12 months | Integrated care boards |
| Sickness absence rate | Integrated care boards and all trusts |
| NHS staff survey engagement theme score | Integrated care boards and all trusts |
| National Education and Training Survey satisfaction rate | All trusts |
| NHS staff survey we are always learning sub score | Integrated care boards |
Reducing inequality
| Metric | Organisations to which the metric relates |
|---|---|
| Deprivation and ethnicity gap in pre-term births | Integrated care boards |
| Deprivation gap in early cancer diagnosis | Integrated care boards |
| Deprivation gap in myocardial infarction and stroke admissions | Integrated care boards |
| Percentage of patients with serious mental illness to receive an annual healthcheck | Integrated care boards |
| Percentage of patients on GP learning disability registers to receive an annual healthcheck | Integrated care boards |
| Percentage of over 65s attending emergency departments to be admitted | Acute trusts |
| Percentage of under 18s attending emergency departments to be admitted | Acute trusts |
| Rate of annual growth in under 18s elective activity | Acute trusts |
| Number of adults over the age of 65 with a length of stay beyond 90 days at discharge | Mental health trusts |
| Annual change in the number of children and young people accessing NHS funded mental health services | Mental health trusts |
Table 7: System considerations for ICB segmentation
These metrics relate to tests applied at a whole system level for ICBs.
| National priority | Test |
|---|---|
| Urgent and emergency care | Is the system in tier one of the National Urgent and Emergency Care support programme? |
| Elective care | Has the system been in the lowest quartile for 18 week performance for each month of the last quarter? |
| Cancer care | Has the system been in the lowest quartile for 62 day performance for each month of the last quarter? |
| Primary care | Is the system in the lowest quartile for overall general practice patient satisfaction? |
| Mental health | Is the system in the highest quartile for the proportion of bed days that were out of area bed days? |
| Finance | Is the system projecting an annual deficit of over 2% or a deficit below 2% that is over 1% off plan? |
Annex B: Segment 4 diagnostic
The core purpose of the diagnostic is to drive faster recovery. The diagnostic will build on existing evidence to identify the root cause of failure. This will be used to recommend priorities for the integrated improvement plan and determine the necessary trajectories for success, ensuring that any intervention is impact-driven and sustainable. Beyond highlighting the underlying root cause of poor performance, the output of the diagnostic will recommend whether entering RSP and making a targeted investment will meaningfully improve outcome/results within a shorter time.
In instances where the capacity to run the diagnostic is limited, the diagnostic process will be targeted towards organisations which score highest in assessment, ensuring that diagnostic resource is directed toward the areas of greatest need. However, all organisations will receive a diagnostic after entry into segment 4 over a period of time.
The diagnostic assessment will determine the underlying drivers of the issues and will build on existing evidence to:
- analyse the root cause(s) of the problem(s) that must be addressed across quality, safety, finance and performance. This includes consideration of the scale of the issues identified at an organisation, the nature, spread, and duration of those issues, as well as the organisation’s capacity and capability to address them
- comprehensively review all existing regulatory and enforcement action making recommendations on new or changes to existing enforcement action
- assess whether further evaluation of the organisation’s leadership capability or governance should be commissioned
Where the diagnostic recommends that RSP entry is not appropriate and that the board has the capacity or capability to deliver the requisite improvements without the additional support of RSP, the relevant governance group will confirm a final segment of 4. These organisations will not enter RSP. However, they will still be mandated to have an improvement plan, and NHS England will deploy support through the wide range of approaches that are on offer, as agreed by our relevant governance group, to assure timely recovery.
Figure 2 summarises the processes and steps that will be taken as part of the diagnostic. Table 8 outlines our principles for conducting the diagnostic.
Figure 2: RSP diagnostic process and steps
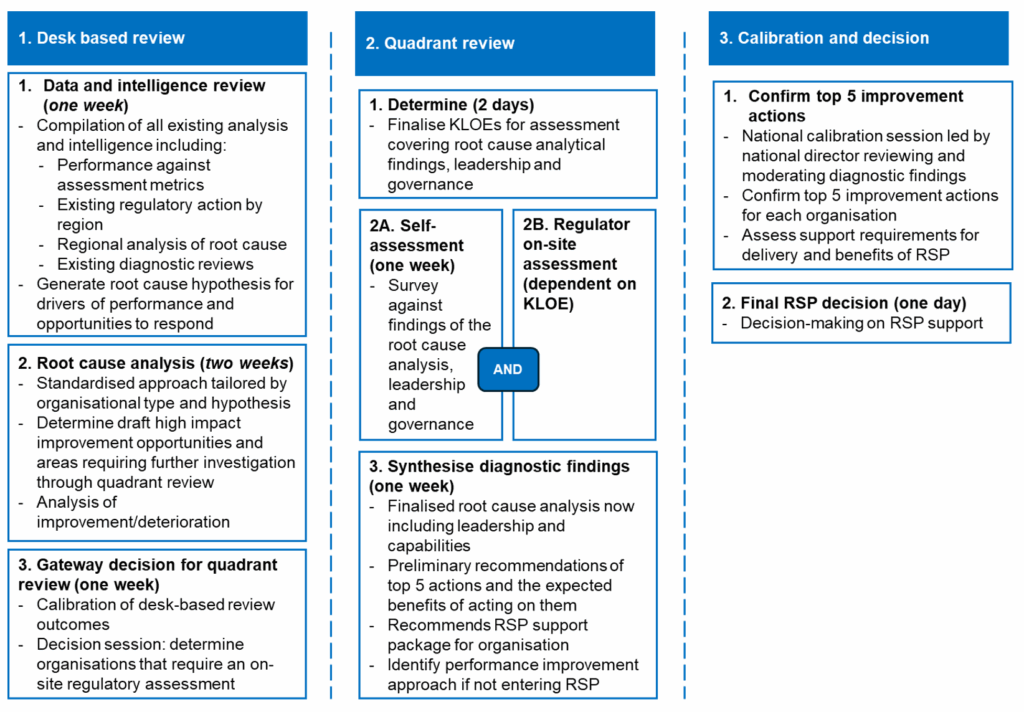
Where our evidence-based diagnostic concludes that entry into RSP and making a targeted investment would meaningfully improve outcomes/results within a shorter time, a joint recommendation is made by the regional director and the national director for recovery support to the appropriate NHS England governance meeting. Consistency in the recommendations will be ensured by a calibration session led by the national director of RSP, reviewing and moderating the diagnostic findings. NHS England through its appropriate governance arrangements considers and takes the decision whether to approve the recommendation. Once we have decided to enter an organisation into the RSP, this is communicated to the organisation by the executive and published on NHS England’s website. The segment of this organisation is also deteriorated to 5.
This diagnostic process cannot rely on a binary algorithm because the decision to enter RSP and invest in an organisation must be based on a holistic assessment rather than a simplistic pass/fail threshold. Assessment will be used as the primary driver of prioritisation, identifying the most underperforming organisations. However, beyond just highlighting poor performance, the diagnostic will evaluate whether entering RSP and making a targeted investment will meaningfully improve outcome/results. The core purpose of the diagnostic is to establish prioritisation for the improvement plan and determine the necessary trajectories for success, ensuring that any intervention is impact-driven and sustainable. The decision to pull an organisation into RSP will be a joint recommendation from the regional director and national director for RSP to NHS England’s Board, ensuring alignment across regional and national leadership before any escalation occurs.
Table 8: Principles of conducting the diagnostic
| Principle | Description |
|---|---|
| Bespoke and non-duplicative | The diagnostic process is a tailored offer, ensuring previously completed work is not repeated. NHS England will not ask the same questions that have already been addressed multiple times. |
| Building on existing evidence | If repeat themes have emerged in historical reviews, these will be accepted as valid and replay them as evidence rather than re-examining them unnecessarily. Where there isn’t strong evidence, short, focused follow-ups will be conducted with RSP teams and the regional teams to verify findings efficiently. |
| Automation and future integration | Over time, the diagnostic process will be automated within the NHS Federated Data Platform wherever possible, reducing manual efforts and increasing efficiency. |
| Tailored approach based on RSP status | The diagnostic approach will differ based on whether the organisation is already in RSP or is a new potential entrant to the framework. |
| Independent, continuous diagnostic capability | The diagnostic will be conducted by NHS England’s national recovery support team. External organisations may also be commissioned by the team for support as required. |
| Fully evidenced and objective reports | The diagnostic report will be evidence-based, ensuring decisions are rooted in data rather than subjective opinions about individuals. |
| An integrated plan which addresses all domains and the underlying causes | The diagnostic will integrate each of the domains of quality, safety, operations and finance. The decision to pull an organisation into RSP will be a joint recommendation from the regional director (RD) and national director for RSP (NDRSP) to NHS England’s Board, ensuring alignment across regional and national leadership before any escalation occurs. |
| Prioritisation based on performance | The diagnostic process will prioritise the worst performers according to the scoring in the assessment process together with regional insight, ensuring that resources are directed toward the areas of greatest need. |
Annex C: Recovery Support Programme
The RSP supports boards to drive sustainable recovery in the most challenged NHS organisations, where there are profound, structural/complex issues and major failures of quality, governance, leadership, finance, or operations, to recover safe, good-quality care in a timely manner. RSP works in partnership with each region and with other regulators. RSP is mandated for all segment 5 trusts; the NHS boards are required to cooperate with RSP in an open manner and to notify promptly RSP of anything relating to the organisation which will impact on delivery of recovery.
Entry to the RSP will be determined by a diagnostic carried out for all providers and ICBs in segment 4, as previously described. The diagnostic report will be evidence-based, ensuring recommendations to enter segment 5 and the RSP are rooted in data. NHS England will communicate its decision that an organisation is mandated to enter RSP to the NHS organisation and to the public. On entry to RSP, the board of the segment 5 organisation is required to meet with the board of NHS England.
RSP will drive sustainable recovery by:
- maintaining the NHS board’s accountability for effective delivery
- mandating an integrated improvement plan based on the underlying causes of failure, which may include leadership, operational, or cultural factors
- taking a holistic, integrated improvement approach across quality and safety, finance, and operational performance
- supplying efficient and co-ordinated expert support, including drawing down from the entirety of the support offer across NHS England
- providing oversight and intervention with leveraging a consistent and proportionate regulatory approach
Figure 3: RSP entry and monitoring process
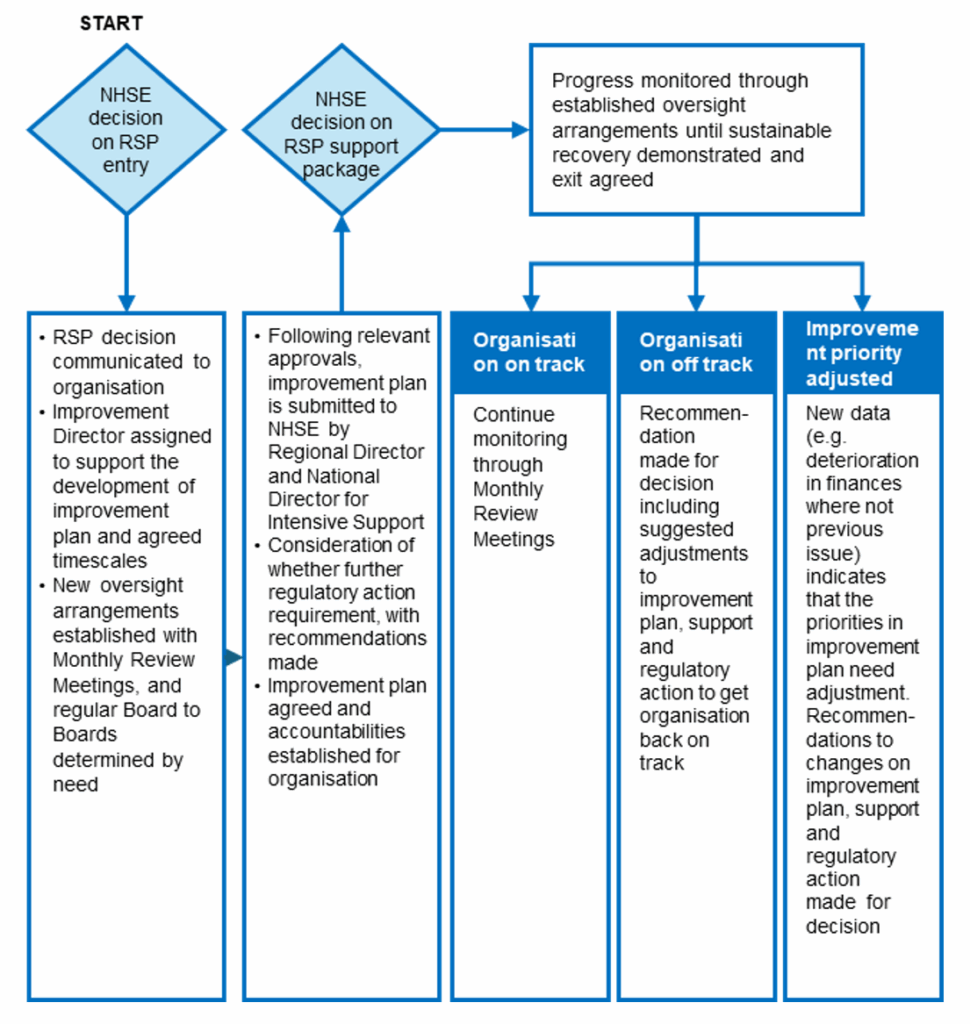
The flow diagram above summarises the steps and monitoring arrangements in place following the decision to enter an organisation in RSP; through our relevant governance processes, NHS England will:
- establish new monitoring and oversight arrangements, including:
- monthly oversight meetings led by the regional director, alongside a representative from the RSP team (ND or deputy)
- regular board-to-board meetings with each NHS organisation in RSP, chaired by an NHS England non-executive director (frequency determined by need)
- take proportionate regulatory action on entry. All interventions while an organisation is in RSP may be supported or implemented, as using formal statutory enforcement action as outlined. NHS England will continue to review enforcement action while an organisation is in RSP, making any changes as necessary. Organisations may also be subject to an evaluation of the organisation’s leadership capability, culture and governance conducted at our discretion
- appoint an improvement director, who works in partnership with the region. They will support and assure a single integrated improvement plan, based on the underlying causes of failure, which is likely to include leadership, governance and organisational cultural factors
- agree the integrated improvement plan to deliver sustainable recovery within an appropriate timescale. It remains the responsibility of the NHS board to remedy all failures and to agree an integrated improvement plan with RSP, working in partnership with the region and, when appropriate, other regulators. The integrated improvement plan and trajectories, signed off by the regional director and national director for intensive support, serve as the guiding framework for progress
- agree the package of improvement support that will be provided to the organisation based on the integrated improvement plan. This may include support from its NHS system, NHS England or, where appropriate, external third parties. The support package will be agreed and formalised through a memorandum of understanding between the RSP team and the board of the segment 5 organisation. Where RSP support is provided by NHS England, it will draw down from the entirety of the support that NHS England has on offer across NHS England. NHS England’s relevant governance group will ensure the co-ordination of support and that it is focused to best support delivery on the Integrated improvement plan
- in some instances, based on the outcomes of the diagnostic, there may be recommendations that the ICB and/or the wider NHS system should be in the RSP alongside the provider that is being supported. This is likely to be in cases where there is evidence the provider is being serially challenged and/or other NHS system partners in the ICS need to be involved to implement the requisite solutions as determined by the diagnostic.
Progress will be monitored through the established oversight and monitoring arrangements. While in RSP, NHS England will continue to review enforcement action and make any changes as appropriate:
- if an organisation is on-track with delivery of their integrated improvement plan, monitoring will continue through the regular monthly oversight meetings
- if an organisation is off-track with delivery of their integrated improvement plan, RSP and the region will make recommendations to NHS to mitigate non-compliance with the improvement trajectory, which may include further regulatory action
- if additional significant areas of concern are identified, RSP and the region may recommend to the relevant NHS England governance group that the integrated improvement plan is amended accordingly. Further regulatory action may also be considered.
Organisations will remain in the RSP until such time as there is evidence that the organisation is able to implement and embed improvements and sustain the improvements made. Recognising the scale and severity of the issues which have resulted in organisations entering RSP, often requiring significant improvement to governance and culture, it is anticipated that the organisations would typically remain in the programme for approximately 2 years.
When sustainable improvement can be evidenced, the quality and performance committee will consider whether the organisation is ready to exit from RSP. In taking this decision, NHS England will consider delivery against its improvement plan and whether this recovery can be sustained.
If NHS England is satisfied with the organisation’s delivery against the improvement plan and the sustainability of its recovery, it will approve exit from RSP. NHS England will inform the organisation of our decision to approve exit once NHS England has completed the formal decision-making processes. NHS England will then share the decision publicly on our website.
On exit from RSP, any remaining enforcement action will be reviewed; it may be the case that even though exiting RSP, the trust may still have support needs and/or action required to remedy any outstanding licence breach which continues to be addressed by such action.
However, if sufficient recovery progress has not been evidenced to enable exit from RSP within 2 years, this will trigger a new review and diagnostic to be conducted. The NHS England relevant governance group will consider the outcomes of this diagnostic, agree the new improvement plan, and consider further regulatory actions that will ensure that the organisation complies with delivery of the requisite improvements.
Publication reference: PRN01347

