1. Service background
1.1 This service specification covers initiation of oral contraception (OC), routine monitoring and ongoing supply of OC and provision of oral emergency contraception (EC) via a patient group direction (PGD).
1.2 The aim of the Pharmacy Contraception Service (PCS) is to offer greater choice from where people can access contraception services and create additional capacity in primary care and sexual health clinics (or equivalent) to support meeting the demand for more complex assessments.
1.3 This service supports the important role community pharmacy teams play in helping address health inequalities by providing wider healthcare access in their communities and signposting service users to local sexual health services in line with NICE guideline NG 102.
1.4 The service provides consistent access for women from community pharmacies across England to free OC and oral EC, removing variation in the service offer found within locally commissioned services.
1.5 The Delivery Plan for recovering access in primary care (May 2023) highlighted the ambition to expand the PCS to increase access to and convenience of contraception services in line with the previous Government’s Women’s Health Strategy for England (August 2022). The strategy flagged community pharmacy had a part to play in increasing choice in the ways people can access contraception, including EC.
2. Service objectives
2.1 The objectives of the service are:
- to provide a model for community pharmacy teams to initiate provision of OC, and to continue the provision of OC supplies initiated in primary care (including general practice and pharmacies) or sexual health clinics and equivalent
- both initiation and ongoing supply will be undertaken using PGDs to support the review and supply process
- to provide a national model for community pharmacy teams to provide free oral EC to individuals of childbearing potential to reduce the risk of pregnancy after unprotected sexual intercourse (UPSI) or where regular contraception has been compromised or used incorrectly
- oral EC supply will be undertaken using PGDs
- to establish an integrated pathway between existing services and community pharmacies that provides people with greater choice and access when considering starting or continuing their current form of OC, or when requiring EC
- to support tackling health inequalities through providing wider access to contraception services
- to support high-risk communities and vulnerable individuals by providing an integrated sexual health service to individuals from a pharmacy of their choice with no requirement to be registered with a GP
3. Requirements for service provision
3.1 Prior to provision of the service, the pharmacy contractor must:
- i. be satisfactorily complying with their obligations under Schedule 4 of the NHS (Pharmaceutical and Local Pharmaceutical Services) Regulations (Terms of Service of NHS pharmacists) in respect of the provision of Essential services and an acceptable system of clinical governance
- ii. notify NHS England that they intend to provide the service by completion of an electronic registration declaration through the NHS Business Services Authority (NHSBSA) Manage Your Service (MYS) portal
3.2 The pharmacy contractor must offer consultations for oral EC in addition to both initiation of OC and for ongoing supply of OC.
3.3 The pharmacy contractor must not:
- commence the supply of oral EC under this advanced service
- commence the delivery of the service via pharmacy technicians
prior to the commencement date for those service enhancements.
3.4 The service commencement date for those service enhancements will be announced and authorised by NHS England.
3.5 For the purposes of this specification, the following definitions will apply:
- Initiation: where a person wishes to start OC for the first time or needs to restart OC following a pill free break. A person who is being switched to an alternative pill following consultation can also be considered as an initiation.
- Ongoing supply: where a person has been supplied with OC by a primary care provider (including general practice and pharmacies), or a sexual health clinic (or equivalent) and a subsequent equivalent supply is needed. Their current supply of OC should still be in use.
3.6 The service should be provided by suitably trained and competent pharmacy staff. The responsible pharmacist must ensure that delegated tasks are being undertaken safely by competent pharmacy staff. Supply under a PGD must be undertaken by a pharmacist or pharmacy technician.
3.7 The pharmacy contractor must have a standard operating procedure (SOP) in place covering the provision of the service. The SOP must include the process for escalation of clinical and non-clinical issues identified including accessing Level 3 safeguarding advice, signposting details, record keeping, equipment maintenance and validation, and staff training.
3.8 Where a pharmacy technician is to deliver the service using a PGD, the pharmacy contractor must have an SOP in place to include the process of how the responsible pharmacist will supervise associated activities connected to the supply of medicines, such as labelling. The SOP should define the roles and responsibilities of the responsible pharmacist and pharmacy technician to meet legal requirements and to enable a supply of medicine to be made autonomously by the pharmacy technician under the PGD, with appropriate supervision.
3.9 The pharmacy contractor must ensure that all pharmacy staff involved in the provision of the service, are familiar with and adhere to the SOPs. The SOPs should be reviewed regularly, including following any significant incident or change to the service.
3.10 Pharmacists and pharmacy technicians delivering the service must have completed one of the recommended Safeguarding level 3 training materials (see 5.3) OR have direct access to professional advice from someone who can advise on Safeguarding at Level 3.
3.11 All consultations should be verbal (face-to-face or remote) and must be provided from the pharmacy premises. Distance selling premises pharmacies (DSPs) are not permitted to provide face-to-face consultations with patients present at the pharmacy premises.
3.12 All consultations must be directly with the person accessing the service, and for whom the medication is for.
3.13 Pharmacies (with the exception of DSPs) must have a consultation room that will be used for the provision of the service which meets the requirements of the terms of service. There must be IT equipment accessible within the consultation room to allow contemporaneous records of the consultations provided as part of this service to be made within the NHS-assured IT system. Where a face-to-face consultation is the preferred access model for the person, these consultations must be delivered from the consultation room at the pharmacy.
3.14 Remote consultations are also permitted to be used to provide the service where assessed as clinically appropriate by the pharmacist or pharmacy technician. When undertaking remote consultations, the contractor must ensure that there are arrangements in place at the pharmacy which enable staff to communicate confidentially with the person receiving the service by telephone or another live audio link or a live video link. NHS Guidance to support community pharmacy teams can help to plan for this.
Equipment
3.15 Where blood pressure measurements (see 4.24 are performed within the pharmacy (not DSPs), the pharmacy contractor must use equipment that is validated by the British and Irish Hypertension Society (BIHS), as recommended by NICE, to measure a person’s blood pressure. To access the BIHS Approved Monitor List visit Validated BP Monitors: Clinical, Policy, and Procurement Guidance.
3.16 Where weight and height measurements are taken within the pharmacy (not DSPs), the pharmacy contractor must have appropriate equipment to measure a person’s weight and height. The NHS website provides an online BMI calculator.
3.17 In accordance with 3.11, where a DSP pharmacy is providing a remote consultation and requires an individual’s blood pressure, height and weight, these measurements cannot be performed in the DSP pharmacy. As combined oral contraceptive supplies will require the person’s blood pressure and BMI, and in some cases, certain requests for oral EC supplies may require consideration of weight or BMI, this information can be self-reported by the person requesting the service in line with 4.24.
3.18 An NHS-assured IT system which meets the minimum digital requirements of the service (as specified within the Community Pharmacy Clinical Services Standard and including an application programming interface (API) to facilitate transfer of data into the NHSBSA MYS portal) must be used by contractors. When choosing an IT supplier, contractors should refer to the NHS CPCS IT Buyers Guide.
4. Service description
4.1 The pharmacy contractor must ensure the service is accessible, appropriate, and sensitive to the needs of all service users. No eligible person shall be excluded or experience particular difficulty in accessing and effectively using this service due to their race, gender, disability, sexual orientation, religion or belief, gender reassignment, marriage or civil partnership status, pregnancy or maternity, or age.
4.2 People will access the service by one of the following routes:
- Identified as clinically suitable by the community pharmacist or pharmacy technician and accept the offer of the service.
- Self-refer to a community pharmacy.
- Signposted by their general practice.
- Signposted from a sexual health clinic (or equivalent).
- Signposted from other NHS service providers; for example, urgent treatment centres or NHS 111.
4.3 When a person attends the pharmacy to collect an NHS repeat prescription for OC, the service can be highlighted to them to consider for future supplies. The service must not be offered at that time as an alternative to dispensing the person’s NHS prescription.
4.4 When a person attends the pharmacy or makes contact for other services, e.g. to access a supply of oral EC, the service can be highlighted to them for both the opportunity to access free oral EC, but also to consider their ongoing contraception requirements.
4.5 Individuals can identify which pharmacies are participating in the service via uk Find a Pharmacy. Health professionals can access this information via NHS Service Finder. Pharmacy contractors must keep their profile manager status up to date as this will ensure Find a Pharmacy and Service Finder are accurate.
4.6 A member of the pharmacy team will agree with a signposted person, the date and time of their consultation.
4.7 The pharmacy must respond to anybody requesting a supply of oral EC or OC as soon as is reasonably possible, having particular regard to the need for timely provision of emergency contraception after UPSI, or where regular contraception has been compromised or used incorrectly. Following discussion, if the pharmacy is unable to offer a consultation within the time needed to meet the person’s emergency contraception or contraception need, they should be signposted to an alternative pharmacy or other service provider for a consultation.
Inclusion criteria
4.8 To be eligible to access this service a person must:
- Be an individual of childbearing potential seeking a supply of oral EC only following confirmation of UPSI or where regular contraception has been compromised or used incorrectly OR
- Be an individual seeking to be initiated on an OC, or seeking to obtain a further supply of their ongoing OC for contraceptive purposes:
- Combined Oral Contraceptive (COC) –
- from menarche up to and including 49 years of age; or
- Progestogen Only Pill (POP) –
- Norethisterone, Levonorgestrel and Desogestrel – from menarche up to and including 54 years.
- Drospirenone only – from menarche up to and including 49 years.
- Combined Oral Contraceptive (COC) –
Exclusion criteria
4.9 A person will not be eligible for this service if:
- they are considered clinically unsuitable, or are excluded for supply of oral EC or OC according to the relevant PGD protocols, including, but not limited to:
- individuals under 16 years of age and assessed as not competent using Fraser Guidelines
- individuals 16 years of age and over and assessed as lacking capacity to consent
4.10 The service exclusions also include all advance supplies of oral EC.
Consultation
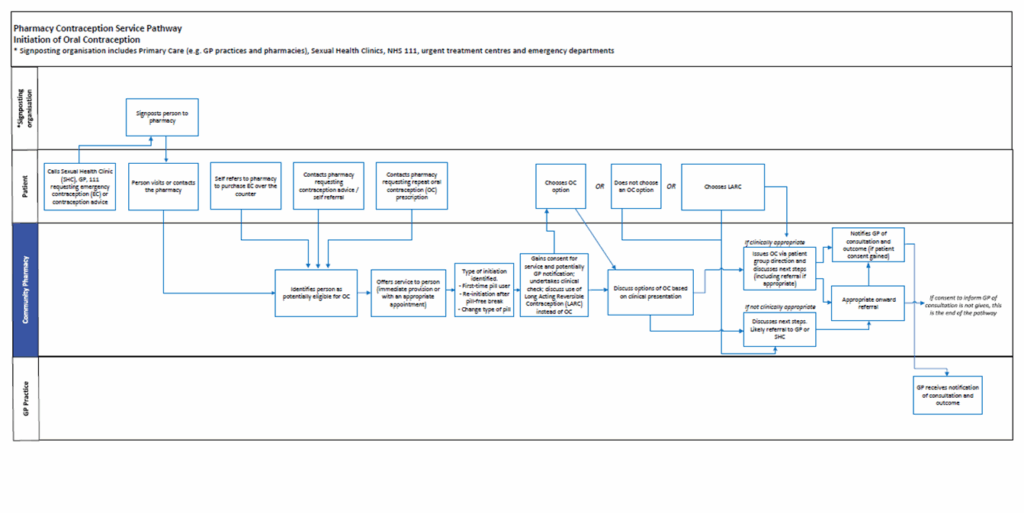
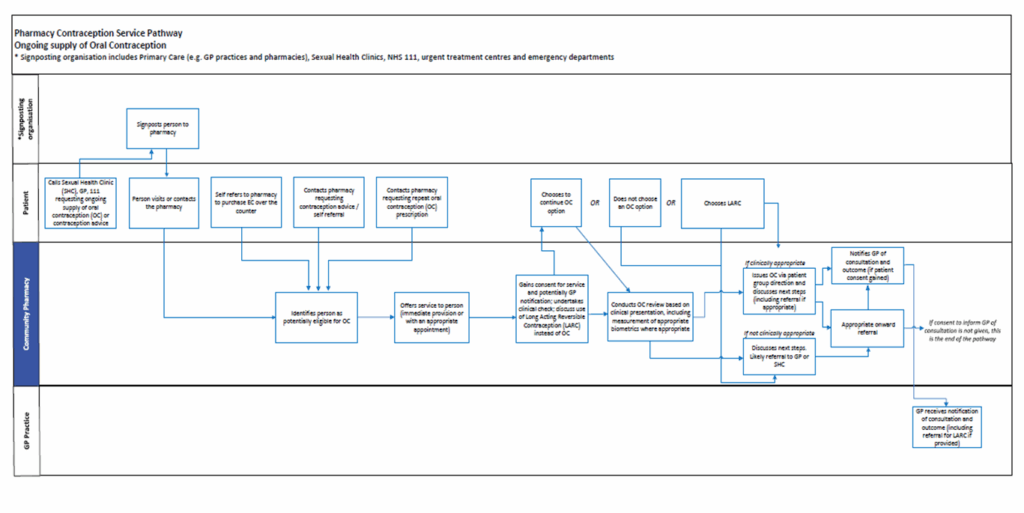
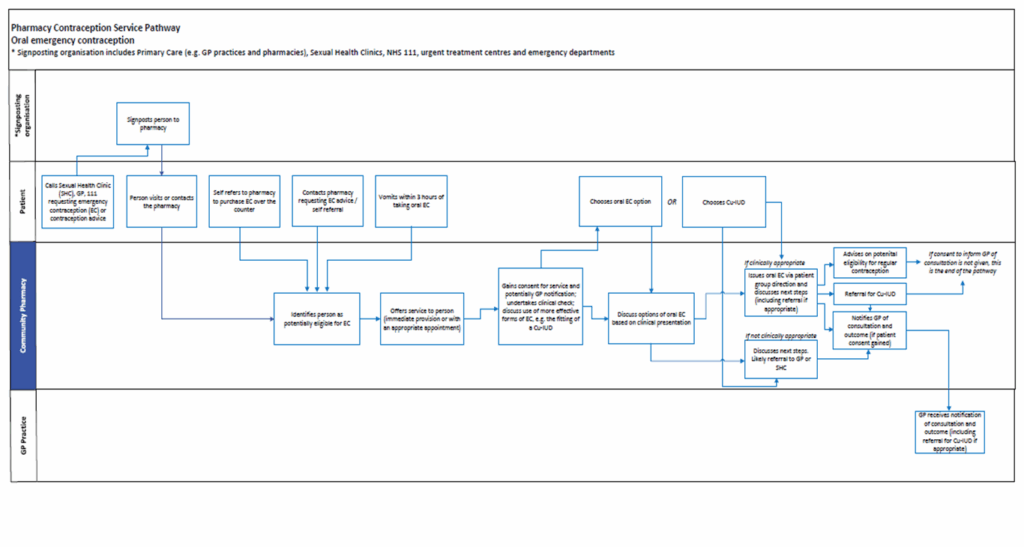
4.11 Please refer to Annex A for flow diagrams describing the service.
4.12 Verbal consent to receive the service must be sought from the person and recorded in the pharmacy’s clinical record for the service.
4.13 If the person provides consent to share the outcome of the consultation with their general practice, information relating to the consultation will be shared with the person’s general practice. However, if the person does not consent to sharing information with their general practice or they are not registered with a general practice, the consultation can still proceed, and a notification to the practice will not need to be sent.
4.14 A person providing consent to share outcomes with their general practice should be made aware that other health professionals who have access to the GP record may also see the information supplied. Any person wishing to mark this information as confidential and not for onward sharing can do so via their GP.
4.15 The person must be advised of the following information sharing that will take place:
- The sharing of information about the service with NHS England as part of service monitoring and evaluation.
- The sharing of information about the service with the NHSBSA and NHS England for the purpose of contract management and as part of post-payment verification (PPV).
4.16 The clinical appropriateness of a supply of oral EC or OC will be determined by the pharmacist or pharmacy technician, as part of a consultation with the person, following the guidelines in the PGDs.
4.17 With the person’s consent, their GP record (for example, via GP Connect Access Record), national care record, or an alternative clinical record for the person, should be checked by the pharmacist or pharmacy technician unless there are exceptional circumstances preventing this.
4.18 During the consultation, if the pharmacist or pharmacy technician is concerned about a potential safeguarding issue, then appropriate action should be taken, where necessary, in line with local safeguarding processes. Any actions must be documented in the clinical record.
4.19 Either party may request or offer a chaperone to be present during the consultation. Details of the chaperone should be documented in the clinical record.
4.20 Oral EC consultations must include a conversation with the person regarding more effective forms of emergency contraception; for example, the fitting of a Cu-IUD.
4.21 OC consultations must include a conversation with the person regarding alternative and more effective forms of contraception; for example, Long-acting reversible contraception.
4.22 Irrespective of the outcome of the consultation, it may be appropriate to also signpost the person accessing the service to another healthcare provider. In some cases, a person may require urgent escalation to another healthcare setting.
4.23 Where appropriate, consultations should provide additional support and advice, including advice on the avoidance of pregnancy and sexually transmitted infections (STIs) through safer sex and condom use. This may include highlighting other locally commissioned pharmacy services (such as C-card and other condoms distribution schemes or chlamydia testing) that the pharmacy is able to offer, or signposting to other services that provide long-term contraceptive methods and diagnosis and management of STIs.
4.24 For COC, a supply will require BMI and a blood pressure measurement to be taken in line with NICE guideline 136. For a supply of oral EC, in some circumstances, there may be a need to confirm a person’s BMI or for a measurement of their weight to be taken. A person accessing the service may also offer their own weight, height and blood pressure measurements. Any self-reported measurements that the pharmacist or pharmacy technician has deemed clinically suitable, will need to be recorded as such.
Outcomes and next steps
4.25 If the assessment criteria are met, supply of oral EC or an OC can be made.
4.26 A single dose of oral EC should be made for all oral EC consultations. This should be 1 tablet unless the person meets criteria outlined in the PGD that allow for an alternative regimen.
4.27 If a person is sick within 3 hours of the initial dose of oral EC being taken, a further supply of oral EC can be made by the pharmacist or pharmacy technician. This should be recorded as a separate consultation (and will be paid for accordingly), however, the reason for the second supply should be noted in the clinical record.
4.28 On initiation, the quantity of OC supplied should not exceed 3 months.
4.29 Following initiation, ongoing supplies of an OC should be for a minimum of 6 month’s supply, unless there are clinical reasons not to. Such reasons should be documented in the clinical record. Supplies can be made of up to 12 months duration and the duration of supply should be considered in line with the College of Sexual and Reproductive Healthcare (CoSRH) guidance. Restricting the length of supply could result in unwanted discontinuation of the method and an increased risk of pregnancy for the person.
4.30 Where a person is initiated on an OC, pharmacists and pharmacy technicians should use their professional discretion as to the appropriate choice of product, from those included in the PGD. To help protect NHS resources, wherever practicable, pharmacy contractors should supply the best value product to meet the clinical need of the patient. Local formularies/restrictions should also be referred to and followed accordingly. Please refer to your local integrated care board (ICB) formulary for further information.
4.31 Ongoing supplies should be made in line with the person’s previous supply, e.g. in the instance that a branded product has been supplied for clinical reasons, such as an allergy to product constituents, the ongoing supply should be made from an equivalent brand/generic equivalent of OC that follows any medicines formulary requirements of the local ICB.
4.32 If an NHS medicine is to be supplied following a consultation, it is expected that the supply will be made with reasonable promptness. The time period to supply must take into account the clinical need of the individual, for example, a supply of oral EC should be made as soon as possible to allow the individual to take the medication within the defined timeframes of clinical efficacy of the oral EC. DSP pharmacies providing the service should make necessary arrangements for a prompt delivery of the item, at no cost to the individual.
4.33 If a supply of oral EC or an OC is not deemed clinically appropriate, the pharmacist or pharmacy technician should explain why this is the case to the person, document this in the clinical record and refer them to their general practice or sexual health clinic (or equivalent).
4.34 The pharmacy is required to report any patient safety incidents in line with the Clinical Governance Approved Particulars for Pharmacies.
5. Clinical skills and knowledge
Competency requirements
5.1 Before commencement of the service, the pharmacy contractor must ensure that pharmacists, pharmacy technicians and pharmacy staff providing the service are competent to do so in line with the specific skills and knowledge in paragraph 5.3 and with the relevant PGDs. This may involve completion of training.
Competency evidence
5.2 The pharmacy contractor must keep documentary evidence that pharmacy staff involved in the provision of the service are competent and remain up to date with regards to the specific skills and knowledge that are appropriate to their role, and to the aspects of the service they are delivering.
Recommended training modules
5.3 To deliver this service, the pharmacist or pharmacy technician should have evidence of competence in the clinical skills and knowledge required to deliver all aspects of the service they provide. The appropriate clinical skills and knowledge are covered in the following training modules on the Centre for Pharmacy Postgraduate Education (CPPE) or the NHS England e-learning for healthcare (elfh) websites:
Packages that are highly recommended are indicated by an asterisk *
Safeguarding (see 3.7)
- Safeguarding Level 3 – Safeguarding Children and Adults Level 3 for Community Pharmacists – video on elfh
OR - Safeguarding Level 3 Learning for Healthcare Safeguarding Children and Young People (SGC) – Safeguarding Children Level 3
Emergency Contraception
- *CPPE Emergency contraception e-learning including emergency contraception e-assessment
Ongoing supply
- *CPPE Contraception e-learning including contraception e-assessment
or the following 4 subsections of
*Module 3 – Contraceptive Choices of the CoSRH Sexual and Reproductive Health e-learning (e-SRH) on elfh:- 03_01: Mechanism of action, effectiveness and UKMEC
- 03_02: Choosing contraceptive methods
- 03_03: Combined hormonal contraception
- 03_04: Progestogen only methods (oral and injectable)
- *CPPE Sexual health in pharmacies e- learning and e-assessment
or the following four subsections of
*Module 9 – STIs of the CoSRH e-SRH on elfh:- 09_01: Epidemiology and transmission of STIs;
- 09_02: Sexually transmitted infection (STI) testing
- 09_03: STI management
- 09_04: Partner notification
and one subsection in the
*External Resources module of the Sexual Health (PWP) e-learning on elfh:
-
- FSRH – Contraception counselling eLearning.
Initiation
- The following subsections of Module 2 of CoSRH e-SRH on elfh:
- 02_01 Health history and risk assessment
- 02_02 Confidentiality, chaperones, and consent
- The following subsection of Module 3 of the CoSRH e-SRH on elfh:
- * 03_07 Barrier contraceptives
- The following subsections of Module 5 of the CoSRH e-SRH on elfh:
- 05_01 Managing bleeding problems in women using contraceptives
- 05_02 Managing contraceptive side-effects
- 05_03 Managing side-effects and complications of IUD and IUS
Other training to support clinical practice:
- CPPE Documenting in patient clinical records e-learning
- CPPE Remote consultation skills e-learning
- PGD e-learning on elfh
- CPPE Pharmacy technicians: using patient group directions in practice
- CPPE consultation skills for pharmacy practice: taking a person-centred approach and e-assessment
5.4 Pharmacists and pharmacy technicians must be familiar with at least one online shared decision-making contraception consultation tool. These tools can be used to support the pharmacist or pharmacy technician and should be shared with people to support their decision making. Examples are:
6. Data and information management
6.1 The pharmacy contractor must maintain appropriate clinical records within the NHS assured IT system to ensure effective ongoing service delivery. Further information on the data that is collected and retained in the contractor’s clinical record as part of service delivery, including where this data is shared with other organisations, can be accessed via the following links.
- Information shared with a GP following consultation Summary of GP Connect service – NHS England Digital
- Information shared with NHS Business Services Authority to support pharmacists being paid and to monitor the service they provide MYS – Pharmacy – NHSBSA
- Information that is additionally collected and stored in the pharmacy’s patient clinical record is outlined in the NHS Pharmacy Contraception Service Patient Group Directions (PGDs)
6.2 The pharmacy contractor must adhere to defined standards of record keeping ensuring that the clinical record is made on the same day that it occurs unless exceptional circumstances apply. Where the NHS-assured IT system is unavailable due to exceptional circumstances beyond the control of the pharmacy contractor, then the clinical record must be added to the system as soon as possible after it becomes available again. If the problem persists for a period greater than 3 working days, then the contractor must notify the local commissioner of the issue.
6.3 Where the individual consents, the pharmacy contractor will ensure that a notification of the provision of the service is sent to the individual’s general practice on the day of provision or on the following working day. This will be sent as a structured message in real-time by the approved clinical services IT system.
6.4 If the structured message system is not available or fails, the pharmacy contractor must ensure a copy of the consultation is sent or emailed (via NHSmail) to the individual’s registered general practice.
6.5 The data which is submitted to the MYS portal via the API will be used by the NHSBSA for payment and PPV purposes. Some of this data, which has been anonymised, will be shared with NHS England for service evaluation and research purposes.
6.6 Records of service delivery relating to consultations where claims have been made via the NHSBSA’s MYS portal should be retained at the pharmacy premises and be available for PPV purposes for 3 years.
6.7 All relevant records must be managed in line with the Records Management Code of Practice for Health and Social Care. As part of this requirement, pharmacy contractors should ensure that clinical records for the service are retained for the appropriate period. This retention period may be beyond the specified period for PPV purposes and should be in line both the requirements for the record type and if the record relates to a child.
7. Payment arrangements
7.1 Data to populate a payment claim for this service will automatically be added to the MYS portal using the API between the approved service IT system and the NHSBSA. Contractors will need to submit the claim within the MYS portal, as part of the normal month end claims process.
7.2 Pharmacy contractors providing this service will be paid according to arrangements set out within the Drug Tariff.
7.3 Reimbursement will be paid on the condition that the pharmacy has provided the service in accordance with the service specification.
7.4 If the pharmacy contractor is commissioned to deliver any related services, e.g. the Advanced Hypertension Case-Finding Service (incorporating BP clinic measurement), the contractor may not claim twice for the same activity.
7.5 The product price for the oral EC or OC supplied will be reimbursed in accordance with the Drug Tariff determination. Any purchase margin by pharmacies relating to medicines supplied as part of this service would be included in the calculation of allowed purchase margin that forms a part of agreed NHS pharmacy funding.
7.6 Where a price concession has been granted for specific strengths of a product, this concession will apply to those specific strengths of products supplied as part of this service. Concessions will only apply to the month in which they are granted according to the usual Drug Tariff arrangements.
7.7 Prescription charges do not apply to products supplied in the provision of this service and a patient declaration is not required.
7.8 Claims for payment should be submitted within one month of, and no later than three months from the claim period for the chargeable activity provided. Claims which relate to work completed more than three months after the claim period in question, will not be paid unless the submission of a claim was delayed by IT issues outside the pharmacy contractor’s control (such as issues with the NHS approved API system used by the pharmacy contractor or with the MYS portal). Such claims will be accepted outside the usual grace period within twelve months of the date by which the claim should have been submitted. This is subject to the NHSBSA receiving evidence of the IT issue, and only if investigation finds that the evidence demonstrates that the IT issue was outside the control of the pharmacy contractor, and it delayed the claim submission.
8. Withdrawal from the service
8.1 If the pharmacy contractor wishes to stop providing the service, they must notify the Commissioner that they are no longer going to provide the service via the MYS portal, giving 30 days’ notice prior to the cessation of the service. Contractors may be asked for a reason as to why they wish to stop providing the service.
8.2 If the pharmacy contractor de-registers from the service they will be unable to re-register for a period of four months from the date of de-registration.
8.3 If the pharmacy contractor de-registers from the service or ceases trading within 30 days of registration, they will not qualify for the £400 set up fee. In this event, if the £400 fee has already been paid to the contractor, this money will be claimed back subject to contractor agreement.
9. Monitoring and post payment verification
Monitoring
9.1 In addition to meeting the Essential services requirements, the pharmacy contractor shall ensure the pharmacy has the following and that these are available for inspection should the local NHS England or Integrated Care System (ICS) Primary Care Commissioning team undertake a site visit:
- A working and appropriately calibrated blood pressure monitor and equipment to measure height and weight (not DSPs) (see section 3.15).
- Sexual health promotional media or evidence of an ability to signpost.
- A suitable quantity of oral EC or OC products to enable efficient and direct supply to the person attending and ensure continuation of supply.
Post payment verification
9.2 NHS England has a duty to be assured that where contractors make claims for payment for set up fees or activity in services, that they meet all the specified requirements of the service. NHS England will work with the NHSBSA Provider Assurance Team to undertake PPV checks on claims made.
9.3 Reasonable additional evidence related to service delivery may be requested directly from contractors. The verification checks include comparing the information provided by contractors in their claims against datasets and evidence sources that are available to the NHSBSA Provider Assurance Team.
9.4 It is the contractor’s responsibility to be able to provide any reasonable additional evidence related to service delivery to eligible patients in accordance with the service specification and PGDs when requested by the NHSBSA for PPV.
9.5 In cases where contractors have been requested to provide evidence and it is not available or does not demonstrate that the service activity was delivered in accordance with the service specification and PGDs, and so these claims cannot be verified, the contractors will be informed. Where claims cannot be verified and the contractor does not agree to the recovery of the associated payments, the case may be referred to the Pharmaceutical Services Regulations Committee (PRSC) to decide whether an overpayment has been made.
9.6 In such cases, where the PSRC decides that an overpayment has been made, and will need to be recovered, contractors will be contacted by the NHSBSA and notified of the overpayment recovery process.
9.7 Any overpayment recovery would not prejudice any action that the NHS may also seek to take under the performance related sanctions and market exit powers within The National Health Service (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013.
9.8 Accurate record keeping of service delivery to eligible patients in accordance with the service specification and PGDs is an essential part of the service provision. The necessary records for reimbursement must be kept for a period of three years to demonstrate service delivery in accordance with the service specification, and to assist with post-payment assurance activities. These records must be provided by a contractor when requested by the NHSBSA Provider Assurance Team.
Annex A: Service pathways
Initiation of oral contraception
Ongoing supply of oral contraception
Supply of oral emergency contraception
Publication reference: PRN02207_i

