Organisation objective
- NHS Long Term Plan
- NHS Mandate from government
Executive summary
This paper providers an update on NHS productivity including the latest productivity estimates and the ongoing work to support productivity improvement.
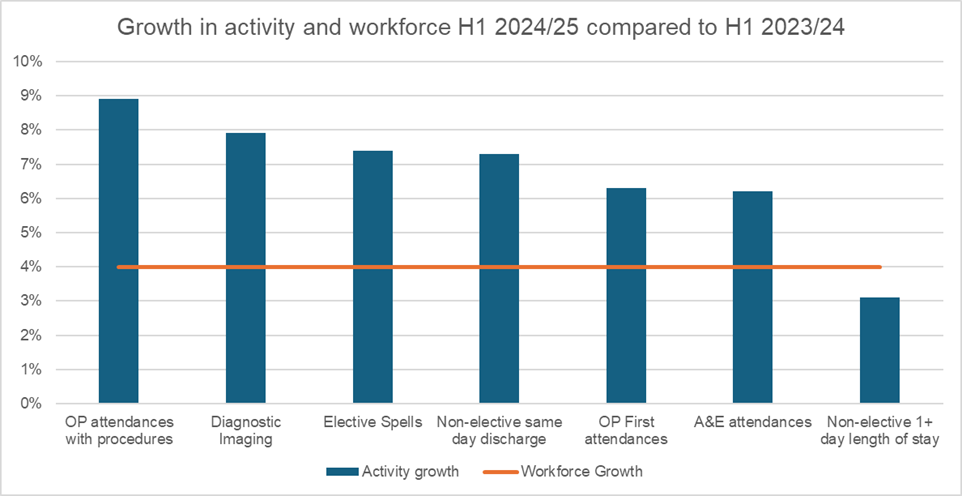
Action required
The Board are asked to note the information provided in the report.
Background
1. In the Autumn Budget, the government confirmed that the Department of Health and Social Care (DHSC) including the NHS would have a productivity target of 2% for 2025/26. Expectations for 2026/27 and beyond will be set as part of phase 2 of the Spending Review, which will conclude in Spring 2025.
2. The NHS England Public Board paper on productivity in May 2024 set out the effect of the pandemic on NHS productivity including NHS England’s estimates for the drivers of the loss of productivity observed. The paper also described the emerging plan to improve productivity.
3. Overall, NHS productivity is below pre-Covid levels, although there are positive signs that NHS productivity is continuing to recover from its low point in the height of the pandemic. The Office for National Statistics (ONS) data shows a sharp drop in productivity in 2020/21 and a sharp rebound in 2021/22, which is the latest data published. NHS England internal analysis suggests there has been steady improvement since then and the productivity gap is narrowing.
4. This paper updates the Board on the progress made in this financial year.
2024/25 acute productivity update
5. Overall, activity has grown across all points of delivery in the acute sector in the first half of 2024/25. In particular, there has been large growth in elective activity, outpatient first and outpatient procedure attendances, diagnostic imaging and same day non-elective discharges.
Table 1 – activity growth by points of delivery
|
Activity category |
Activity growth H1 2024/25 compared to H1 2023/24 |
|
Elective spells |
7.4% |
|
Outpatients o/w first attendances o/w with procedures |
5.2% 6.3% 8.9% |
|
Diagnostic imaging |
7.9% |
|
Non-electives o/w 1+ day length of stay o/w same day discharge |
4.6% 3.1% 7.3% |
|
A&E attendances |
6.2% |
Growth rates have been adjusted for differences in working days between 2023/24 and 2024/25
6. At the same time, NHS staff numbers have increased by 4.0% in the first half of 2024/25 compared to the same period in 2023/24. This includes a reduction in the number of agency staff by 33%.
Workforce FTE growth 2024/25 compared to 2023/24
|
Contract type |
Workforce FTE growth 2024/25 compared to 2023/24 |
|
Substantive |
5.0% |
|
Bank |
2.1% |
|
Agency |
-32.7% |
|
All |
4.0% |
Data from Provider Workforce Returns
7. Taken together, this means there has been an increase in labour productivity over the first half of 2024/25.
Growth in activity and workforce H1 2024/25 compared to H1 2023/24
8. Recent analysis from the Institute for Fiscal Studies has found a similar trend and also suggests a greater focus on addressing productivity, increased incentives for improving productivity, and the continued recovery from the impact of the covid pandemic have contributed to improvements.
9. Combining these estimates of activity growth with overall expenditure by acute trusts on pay and non-pay items in the same time period shows that overall acute productivity has improved by 1.8% in H1 2024/25 compared to the same period last year. The acute sector has delivered 5.7% more activity (weighted for cost) than in the same period last year, whilst real terms costs have increased by 3.9%. This means this year so far we are continuing the c.2% productivity improvement seen between 2022/23 and 2023/24.
10. This increase in acute productivity has been delivered through a number of improvements, such as:
- an increase in the proportion of elective procedures with a same day discharge – from 83.5% in 2023/24 to 84.2% in 2024/25
- continued reductions in agency spending. Spend has reduced from £3.5 billion in 2022/23 (4.5% of total pay) to £3.0 billion in 2023/24 (3.7% of total pay), and is currently at £1.2 billion for H1 2024/25. This has included targeting the use of expensive off-framework providers, which has reduced from £7 million a month in July 2023 to £1 million a month in August 2024 (0.6% of total agency shifts)
- a reduction in the average length of stay of non-elective admissions by 2.3%
Non-acute productivity
11. In the non-acute sectors including mental health, primary care, community services, data quality issues have to date prevented more timely measurement of productivity. In recent years, ONS has begun to incorporate community and mental health patient level costing data into overall NHS productivity calculations. However, there is still significant variation in the quality of data in these sectors. In addition, the lack of granularity in data constrains the ability to capture value of activity accurately, in particular in primary care.
12. NHS England has been developing productivity measurement in all non-acute sectors, with the aim to start testing initial outputs with providers and systems in the coming months. The productivity data reporting, alongside benchmarking of a wider set of metrics, will enable trusts and systems to start identifying areas of opportunities.
13. There are further challenges to capture the value of preventative care, eg when unnecessary admissions are avoided, or when care is moved into a different setting. Further work is needed to incorporate such shifts into productivity measurement
Ongoing work to improve productivity
14. Despite the improvement to date, relative to the pre-pandemic position, productivity has not yet recovered to the level it was in 2019/20. There continues to be impact from Covid (see Public Board paper on productivity in May), including permanent Covid-associated costs in the NHS baseline such as enhanced infection prevention and control measures, increasing acuity and dependency of patients in hospital settings, constrained social care capacity, and persistently higher sickness and absence among NHS staff.
15. In addition, industrial action taking place over June and July 2024 is estimated to have reduced productivity by around 0.5% in comparison to 2019/20, with the NHS incurring additional cost to cover shifts, and foregoing some elective activity on strike days.
16. To continue recovering NHS productivity, there are further opportunities to drive operational and clinical excellence, workforce efficiency and reduce waste by spending every pound well.
17. To support NHS providers to realise these opportunities, since May 2024 we have launched a national Clinical and Operational Excellence programme through NHS IMPACT which:
a. Published clinical and operational improvement guides, co-developed with NHS staff, covering:
- improving flow through emergency care (reducing avoidable admissions and optimising admitted care)
- generating greater value for patients from theatres, elective surgery and perioperative care
- generating greater value for patients from outpatient services
- medical job planning as a key enabler to improved productivity
b. Published 3 new analytics compartments on Model Health System, focused on UEC flow, theatres and outpatients, covering a range of process, outcomes and quality metrics which providers can use to track progress against implementation of the ‘change ideas’ set out in the guides.
c. Established 16 learning improvement networks across the regions to support the delivery of best practice care.
18. To ensure the workforce is deployed effectively, the focus will include:
a. A continued effort to minimise agency spend:
- agency limits this year intended to reduce spending further to 3.2% of total pay, which systems are currently on course to exceed, forecasting to bring it down to £2.2 billion
- further action is being taken to strengthen agency rules and to explore restrictions to agency use for entry level roles (Agenda for Change bands 2 and 3) and with staff who have recently left the NHS to work back on an agency contract
b. A consultant job planning project has been launched, led by the national medical director for secondary care and all 7 regional medical directors. National and regional improvement support is currently being established to support and skill up local clinical and operational leaders, in addition to the national guidance and toolkits already published. The objectives of the work are to:
- achieve 95% job plans signed-off at Board level by April every year
- improve quality and levels of Attainment for medical consultant e-job planning
- improve consistency of job plans to align with service demand with reduced variation and increased fairness
- fully deliver approved job plans and only incur premium costs when core capacity is fully utilised.
c. National retention programme which supports and helps organisations and systems to improve staff experience and achieve tangible improvements in staff retention. In August 2024, the all staff (excluding medics) leaver rate was at 6.96%, below the Long Term Workforce Plan target range for 2023/24 and below the stretch scenario for 2024/25, helping to support workforce productivity improvements.
19. NHS continue to invest in technology-enabled transformation and are making good progress.
- The NHS App is estimated to have achieved benefits equivalent to £249 million in financial year 2023/24, including freeing up 2 million hours of staff time and 890,000 hours of GP time. Patient engagement portals rollout has continued at pace, preventing up to 1.59 million did not attends so far, helping to maximise capacity. The ‘Ping and Book’ service was launched to invite women to attend a breast screening appointment in November, marking a significant modernisation of those services while delivering a better user experience at lower cost by using digital communication channels. We continued to invest in enabling infrastructure, supporting almost 6,000 sites to upgrade their internet connectivity this year.
- Over the remainder of this year progress will be made a few key areas including further roll-out of the Federated Data Platform (FDP). The target of onboarding 71 trusts has already been achieved, with those utilising the FDP seeing on average an 11% decrease in their waiting lists. We continue to make progress in digitising providers, and will achieve 92% of secondary care trusts having an EPR by March. We are also forecasting to achieve the 80% adoption target for digital social care records, driving substantial time savings and reducing pressure on the NHS.
- While future investment will be subject to further discussion, NHS England is assessing opportunities to make the best use of new technologies and are supporting the NHS at large to innovate through the health innovation networks. A recent example was from Great Ormond Street Hospital where they trialled the use of artificial intelligence to automate the process of drafting notes and composing letters, enabling clinicians to spend more time engaging with patients directly. While further work is required, technology like this has the potential to yield significant productivity and experiential improvements.
20. To increase the value of every pound spent, progress has been made in:
a. Medicines efficiencies through price savings and switches to biosimilars which have saved £171 million year to date July 2024. Work on the pipeline opportunities available for biosimilars up to 2028 which could realise over £0.5 billion in savings.
b. Leveraging procurement and commercial savings through NHS Supply Chain via price reductions and increased uptake from NHS trusts (with an aim to release up to £100 million of savings in 2024/25); broader commercial efficiency opportunities such as the national energy framework along with a mobile audit which is due to deliver £14 million savings this year.
21. 2 key enablers for generating productivity improvement have also been progressing:
a. Improving productivity measurement and reporting
- NHS England is also working with the ONS and the University of York to develop our measure of in-year NHS productivity, to ensure it captures the fullest and broadest range of activities and service improvements
- progress has been made in producing in-year productivity measurement in non-acute sectors for the first time
- benchmarking data of a wider set of productivity and efficiency metrics is published on Model Health System, currently for acute providers with non-acute providers under development. These are intended to enable providers and systems to identify opportunities by comparing with peers, and track trends over time
b. Supporting frontline clinical and operational staff to drive productivity. Through the Operational and Clinical Excellence Programme as well as professional networks and engagement channels (eg NHS Providers, Healthcare Financial Management Association), to increase awareness about the benefits, generate and spread local good practice. Further work is underway to use creative and engaging methods to reach, involve and connect with clinical and operational staff to share and implement best practice.
Next Steps
- The remainder of financial year 2024/25 and financial year 2025/26 will see an increased effort on fully embracing the opportunities listed above in all NHS sectors. This means an enhanced effort to recover productivity and a clear drive in understanding and improving productivity in all non-acute sectors.
- Through the planning process, a greater emphasis will be placed on rigorous assessment of productivity and efficiency opportunities, to enable providers and systems to live within the financial envelope set by government, while delivering better value for patients.
- It is important to emphasise that to enable sustainable improvement in productivity beyond next year, boosting investment in technology and infrastructure is essential. These will be further developed as part of the multi-year spending review in the Spring.
Publication reference: Public Board paper (BM/24/42(Pu)

