Organisation objective
- Statutory item
Executive summary
As we continue to measure our performance against the 2024/25 planning guidance objectives, our overall priority remains the recovery of our core services and productivity to improve patient experience and outcomes. This report provides details of performance and work being undertaken to improve those services in our wider priority operational areas.
This briefing draws on official statistics published here.
- NHS staff experienced the busiest year on record for A&E and ambulance services last year. There were a total of 2,345,934 attendances at A&E departments across England in December, bringing the total number of attendances in 2024 to 27.42 million.
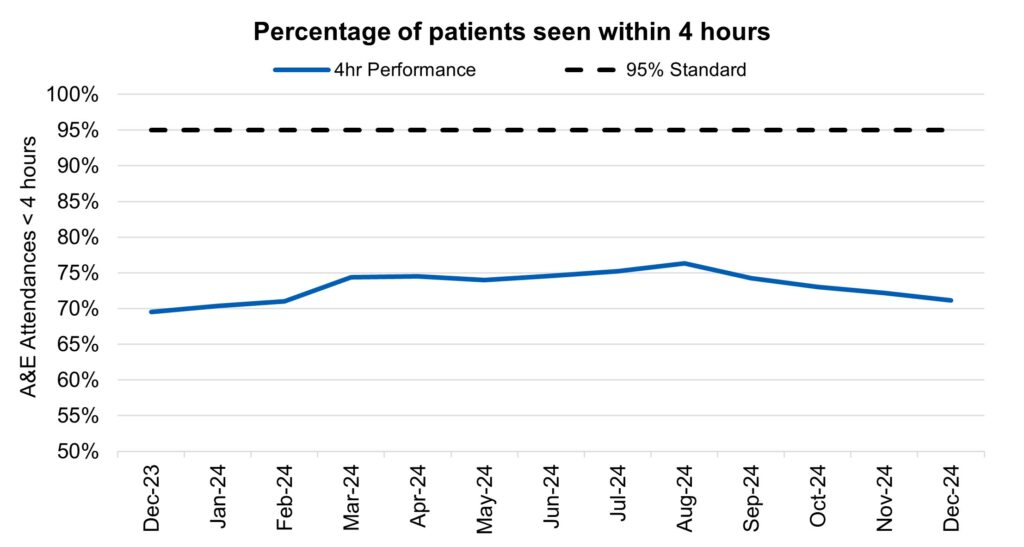
- 71.1% of patients were admitted, transferred or discharged within four hours, which is below the NHS constitutional standard of 95%. This is a deterioration from 72.1% in November, but an improvement from 69.5% in December 2023.
- Ambulance services answered 935,950 calls to 999, or 30,192 per day, an increase of 5% compared to November 2024 and 4% more than December 2023.
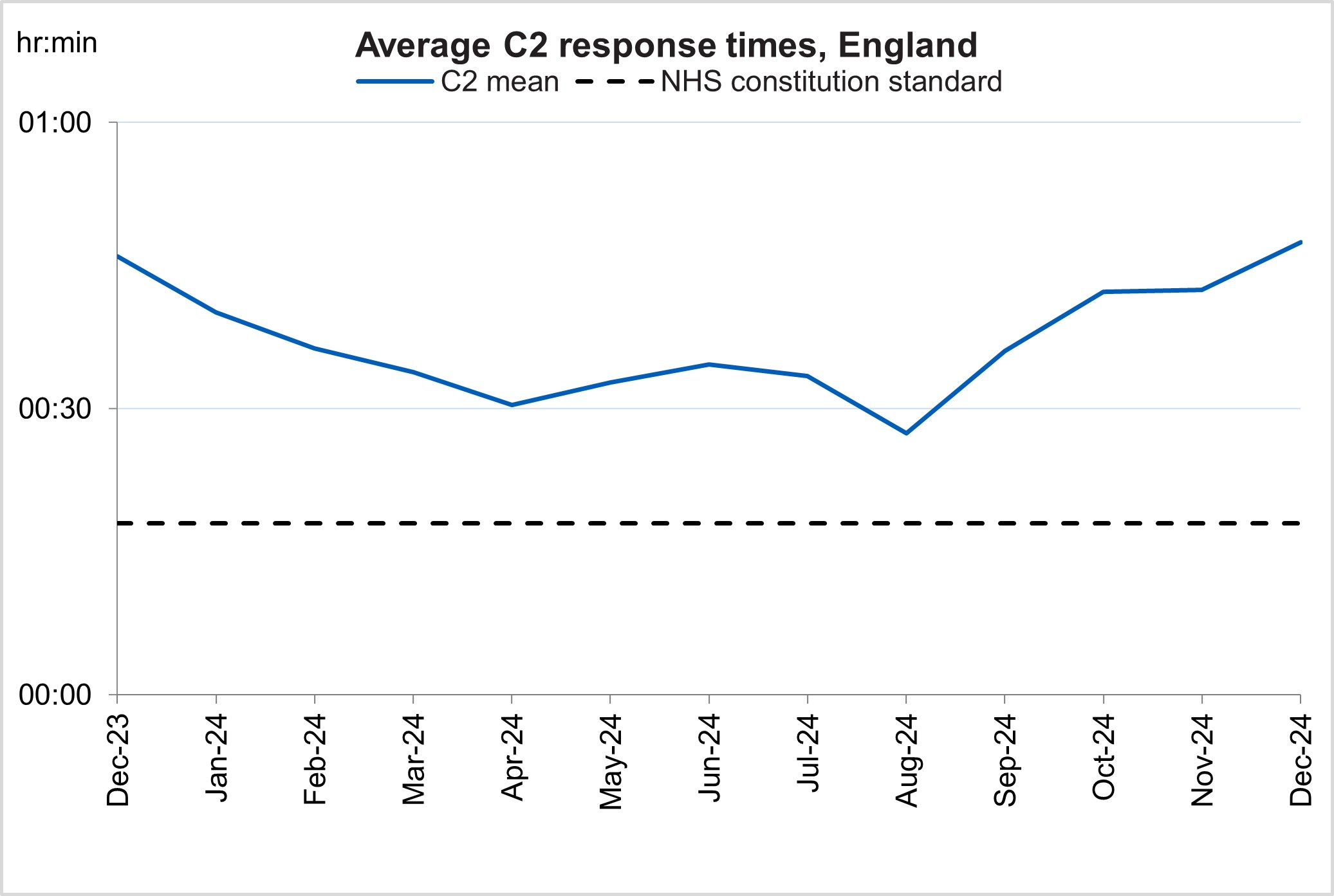
- The average ambulance response time for category 2 calls was 47 minutes and 26 seconds. This has increased from 42 minutes and 26 seconds in November 2024 and 45 minutes and 57 seconds in December 2023.
- Waits of more than 65 weeks for treatment was 16,904 at the end of November, reduced compared to 94,681 at the end of November 2023 (down 82.1%) and 20,930 in October 2024 (down 19.2%).
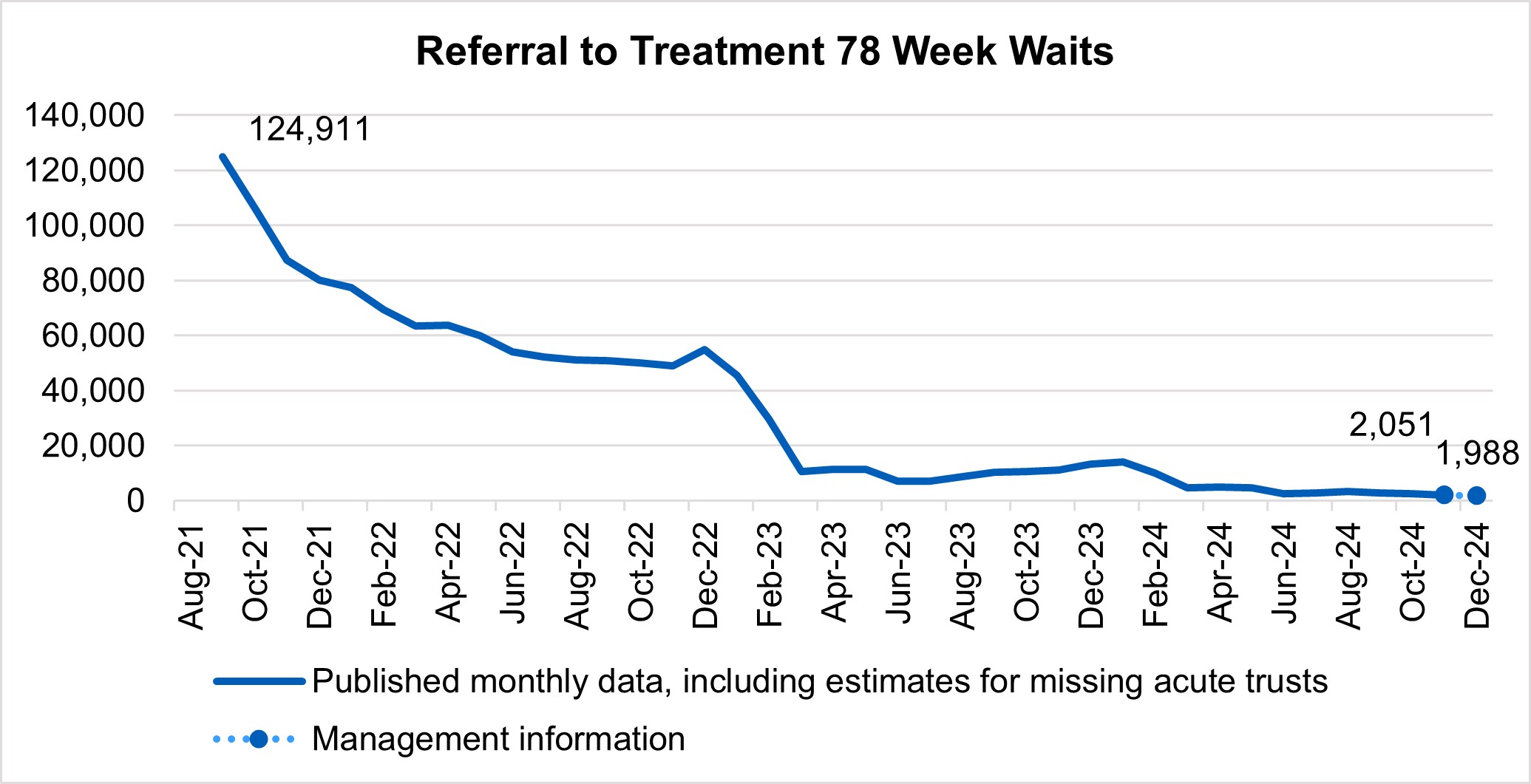
- There has been a reduction in the longest waits for care, 2,051 patients were waiting more than 78 weeks for treatment at the end of November, compared to 11,215 at the end of November 23 (down 81.7%) and 2,446 in October 2024 (down 16.1%)
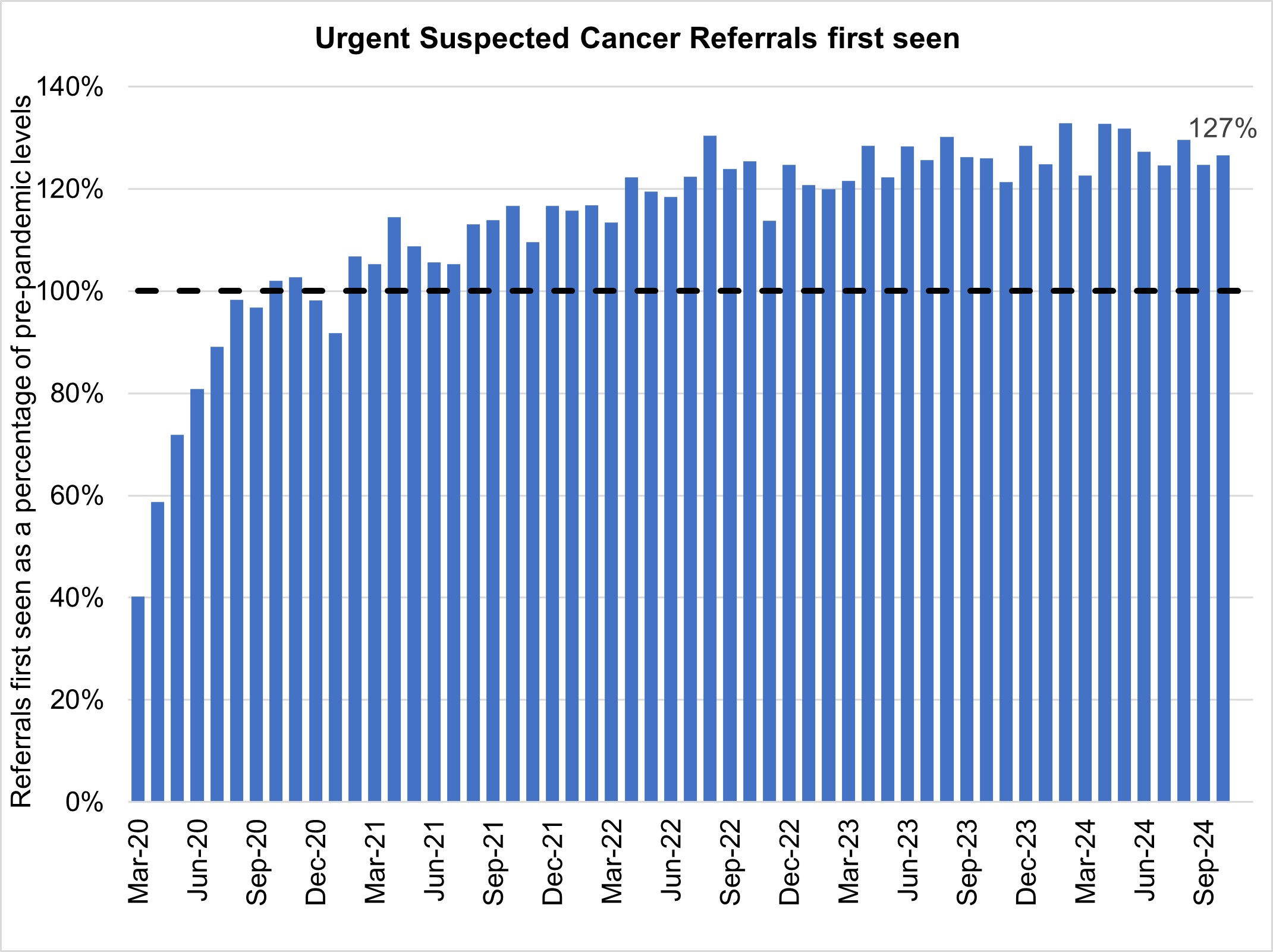
- There were 12,145 Urgent Suspected Cancer referrals per working day in November 2024. This is 27% more referrals than the NHS was seeing before the pandemic – the equivalent of 2,500 more referrals per working day – and there were 1,400 patients starting cancer treatment per working day.
- In November, performance against the 62 day Urgent Referral to First Treatment Standard, was 69.4% which was 3.9% higher than at the same point last year, and 1.2% higher than October 2024, but still well below where we want to see it. The NHS has set the ambition to improve this to 70% by March 2025, as a first step in recovering performance to the NHS constitutional standard of 85%.
Urgent and emergency care
1. Demand rose for urgent and emergency care (UEC) services in December, with an increase in winter viruses and infection prevention and control increasing pressure on flow through emergency departments.
2. There were a total of 2,345,934 attendances at A&E departments across England in December. The average daily attendances decreased to 75,675, this is 1.8% lower than November’s daily average and 7.4% higher than December 2023.
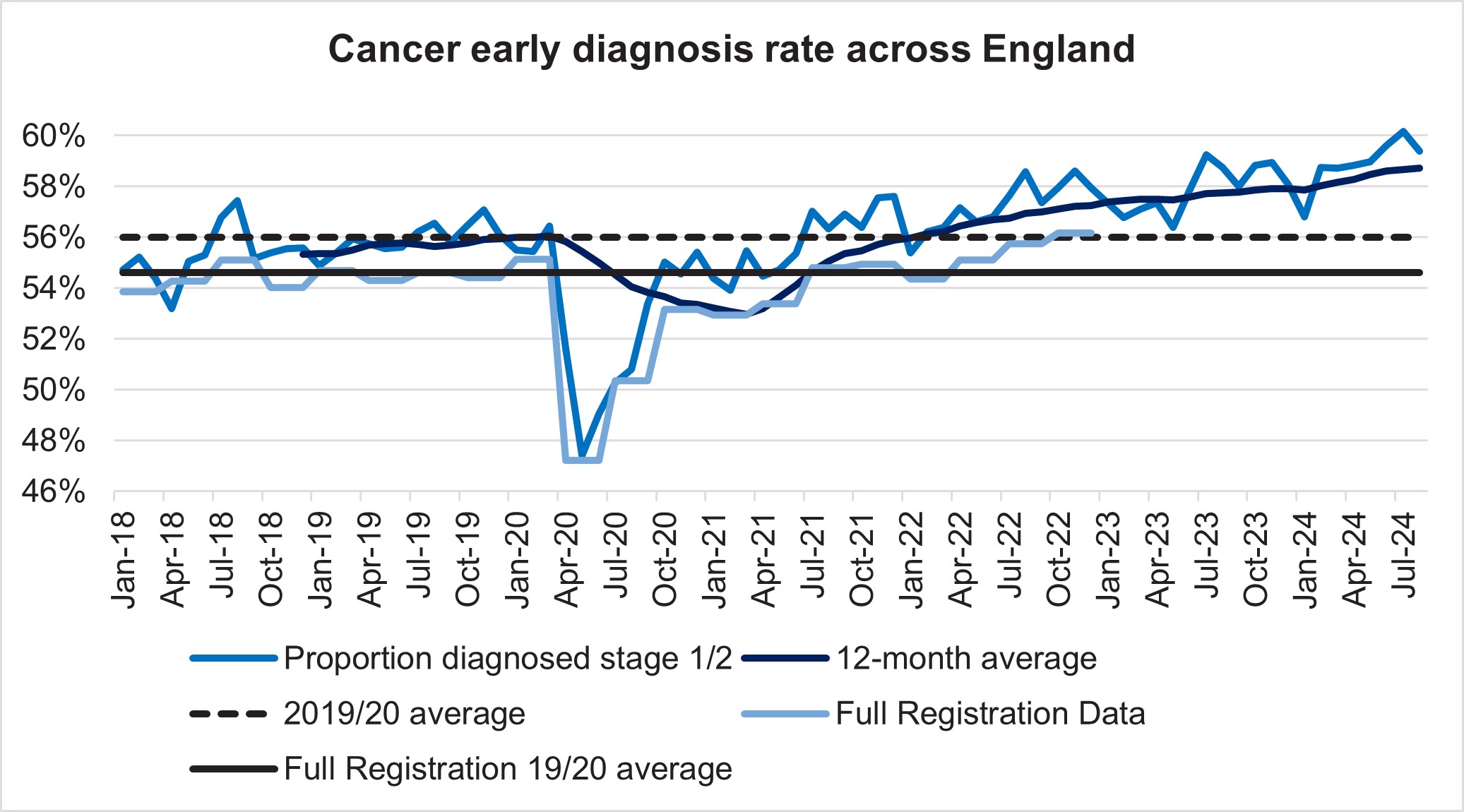
3. 7.1% of patients were admitted, transferred or discharged within four hours, which is below the NHS constitutional standard of 95%. This is a deterioration from 72.1% in November, but an improvement from 69.5% in December 2023.
4. The provisional figures published for December indicate that 12.0% of patients attending a type 1 A&E department spent 12 hours from arrival in A&E compared with 10.8% last month.
Percentage of patients seen within 4 hours
5. Ambulance services answered 935,950 calls to 999, or 30,192 per day, an increase of 5% compared to November 2024 and 4% more than December 2023. There were 388,473 incidents where a patient was conveyed to A&E or 12,531 per day, 0.5% more than in November 2024 and a 2% increase from December 2023.
6. The average ambulance response time for category 2 calls was 47 minutes and 26 seconds. This has increased from 42 minutes and 26 seconds in November 2024 and 45 minutes and 57 seconds in December 2023. This is above the 30 minute target for the year and the NHS constitutional standard of 18 minutes.
Average C2 response times, England
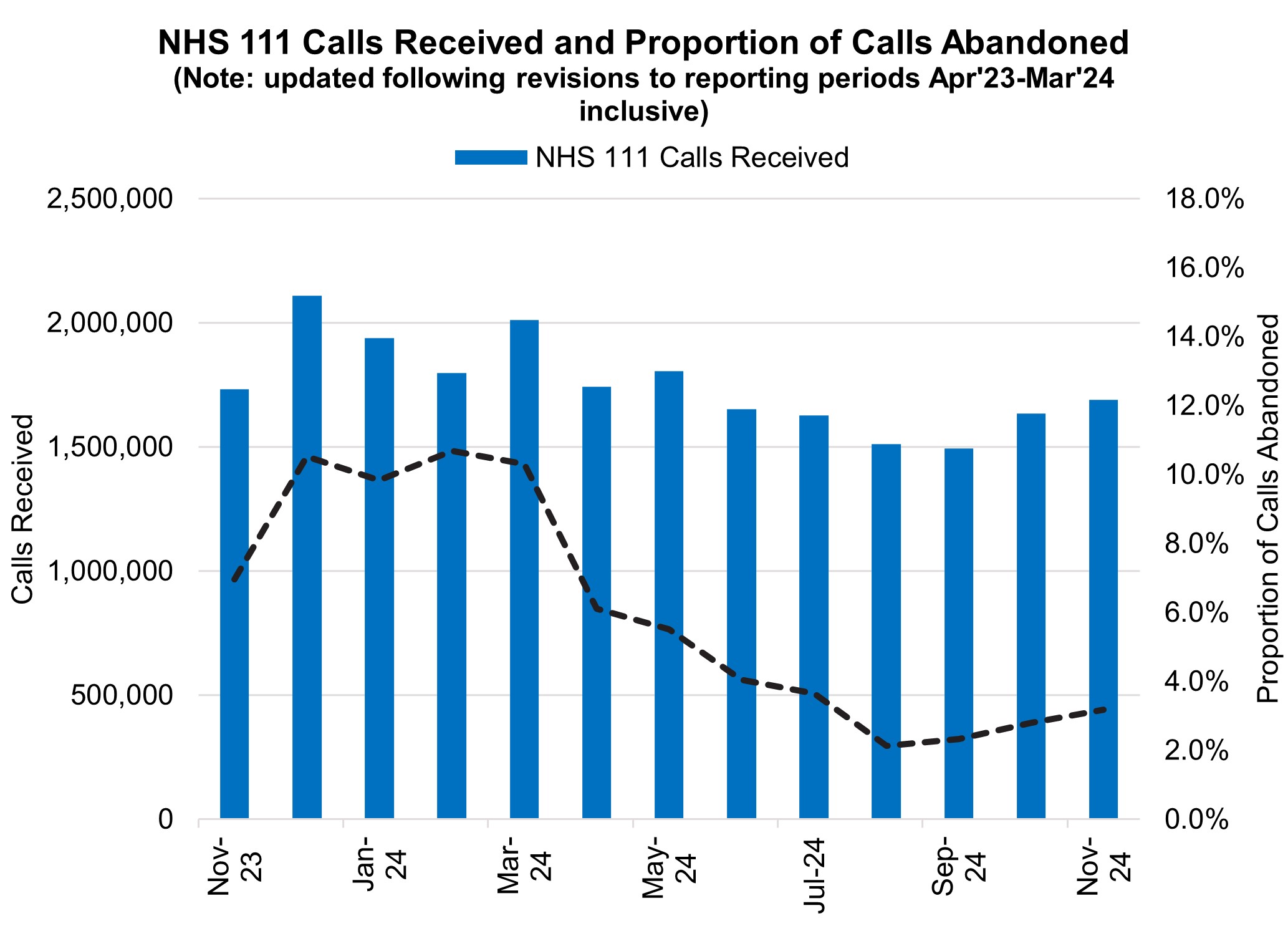
7. NHS 111 received 1.68 million calls (c. 56.3 thousand per day) in November 2024. Demand was 2.6% down year on year and 3.2% above volumes received in October 2024.
8. The proportion of calls abandoned increased 0.4% percentage points from the previous month (now at 3.2%) and the average speed to answer increased by 9 seconds to 56 seconds.
NHS 111 calls received and proportion of calls abandoned
Elective Recovery
9. As of the end of November, on the total waiting list there were 7.48 million waits for procedures and appointments and an estimated 6.28 million people waiting for care. The NHS constitution standard states that 92% of patients have a right to start consultant-led treatment within a maximum of 18 weeks from referral for non-urgent conditions.
10. There were 221,889 waits of more than 52 weeks for treatment at the end of November, compared to 355,712 at the end of November 23 (down 37.6%) and 234,885 at the end of October 24 (down 5.5%). Additional management data1 suggests there were 215,823 waits of more than 52 weeks as of the end of December.
Referral to treatment 52 week waits
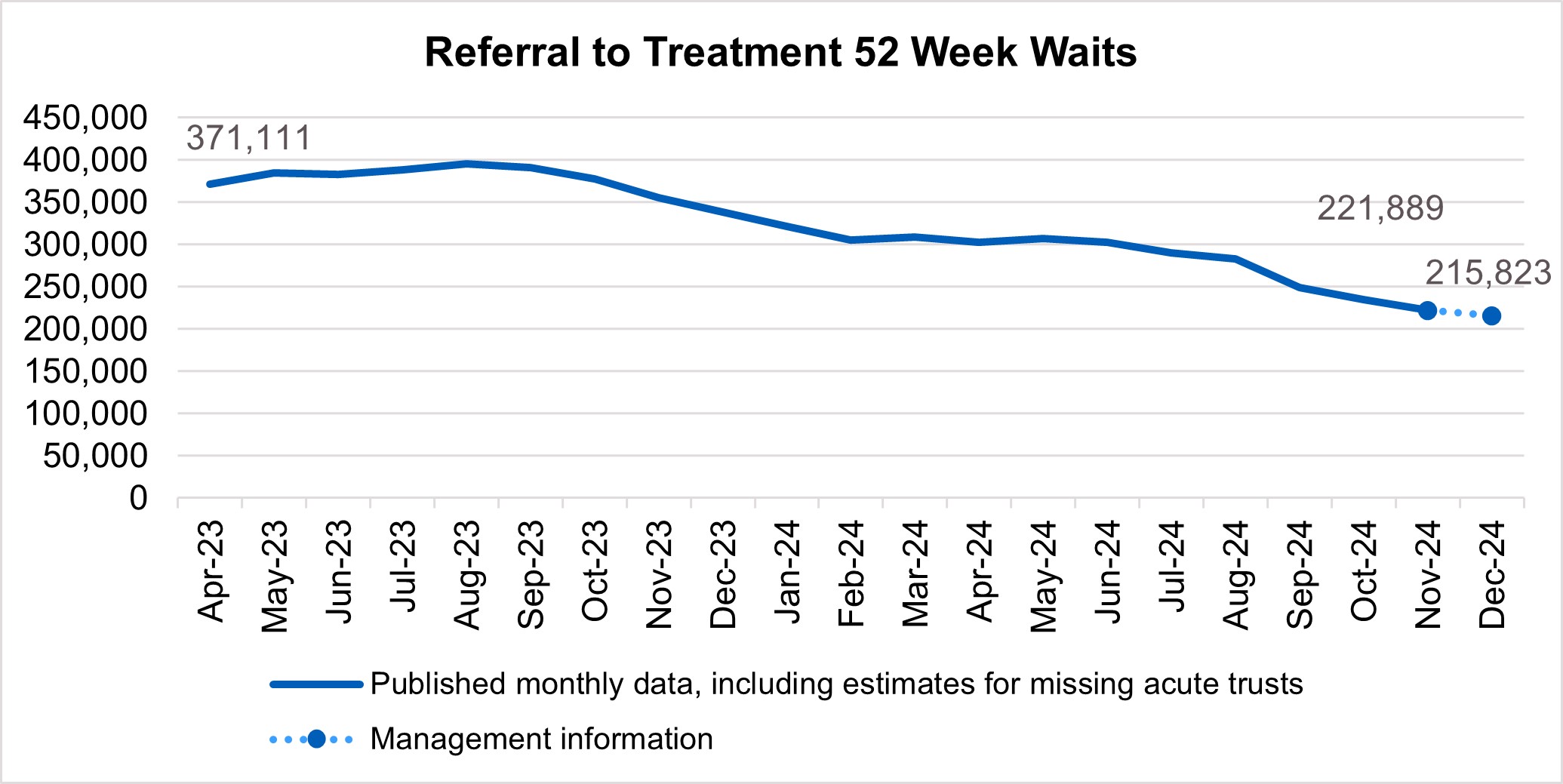
11. Waits of more than 65 weeks for treatment was 16,904 at the end of November, reduced compared to 94,681 at the end of November 2023 (down 82.1%) and 20,930 in October 2024 (down 19.2%). Additional management data1 suggests there were 16,890 waits of more than 65 weeks for treatment as of the end of December.
Referral to treatment 65 week waits
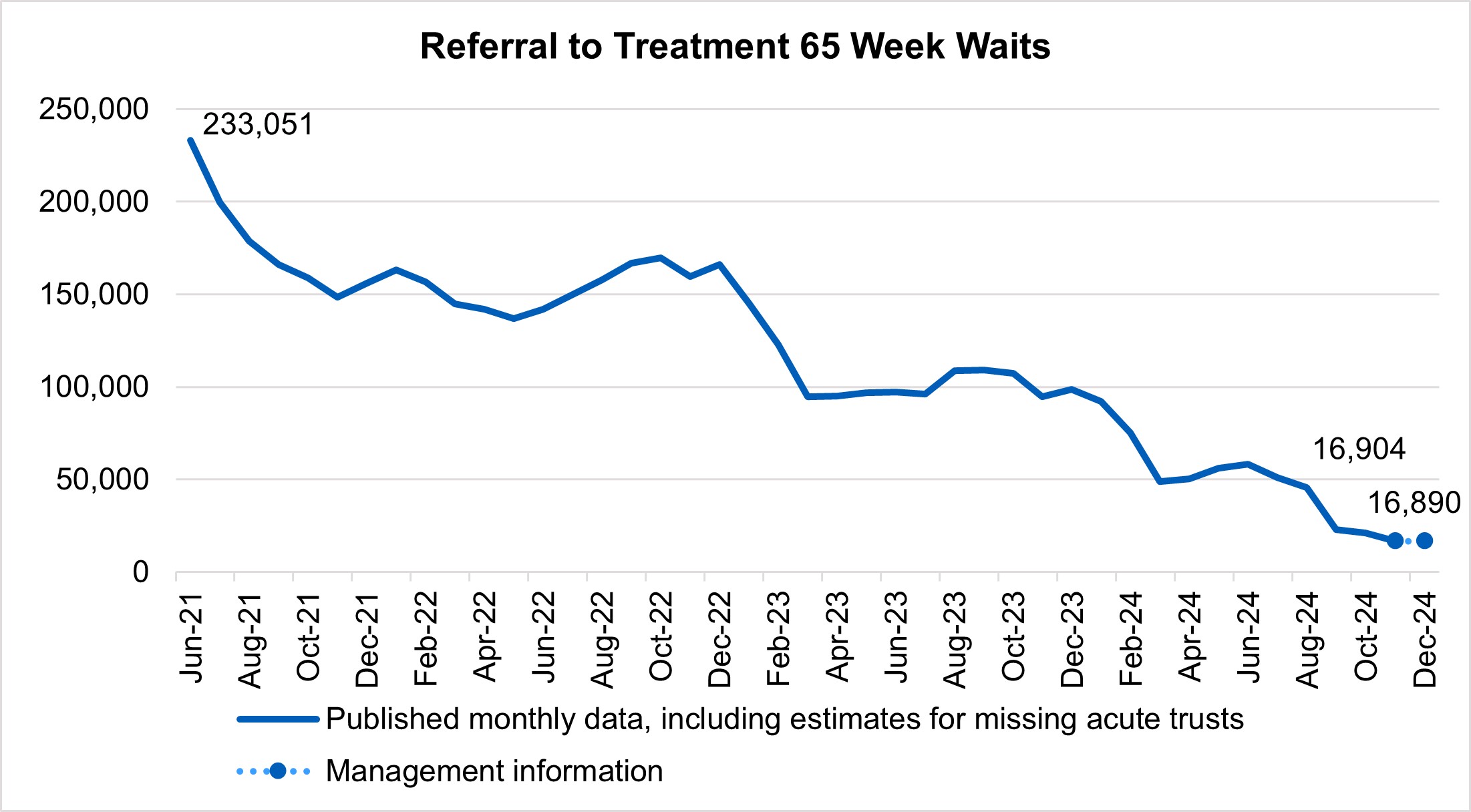
12. There has been a reduction in the longest waits for care, 2,051 patients were waiting more than 78 weeks for treatment at the end of November, compared to 11,215 at the end of November 23 (down 81.7%) and 2,446 in October 2024 (down 16.1%). Additional management data* suggests there were 1,988 waits of more than 78 weeks for treatment as of the end of December.
* Management information for the latest month is taken from the Waiting List Minimum Dataset (WLMDS). Figures include data up to week ending 29 Dec 24. WLMDS data is subject to less validation than the published monthly figures. All acute trusts submitted data for week ending 29 Dec 24.
Referral to treatment 78 week waits
13. At the end of November, on the diagnostic waiting list there were 1.61 million waits, of which 321,773 had waited 6 weeks or more. The percentage of 6 week waits was 19.9%, down from 23.3% in November 2023. Progress is being made towards the interim recovery target of not more than 5% of the waiting list over 6 weeks and an increased percentage of diagnostic activity is supplied by Community Diagnostic Centres.
Cancer
14. Levels of Urgent Suspected Cancer referrals have remained at high levels, with 12,145 referrals per working day in November 2024. This is 27% more referrals than the NHS was seeing before the pandemic – the equivalent of 2,500 more referrals per working day.
15. Treatment activity was also at a record high level with 1,400 patients starting cancer treatment per working day, 12% above pre-pandemic levels.
Urgent suspected cancer referrals first seen
16. The increase in referrals has also contributed to increases in early diagnosis, which are now about 2 percentage points higher than before the pandemic. Cancer survival also continues to improve. In 2023, the Annals of Oncology published findings showing that cancer deaths are around 10% lower in the UK compared to five years ago.
Cancer early diagnosis rate across England
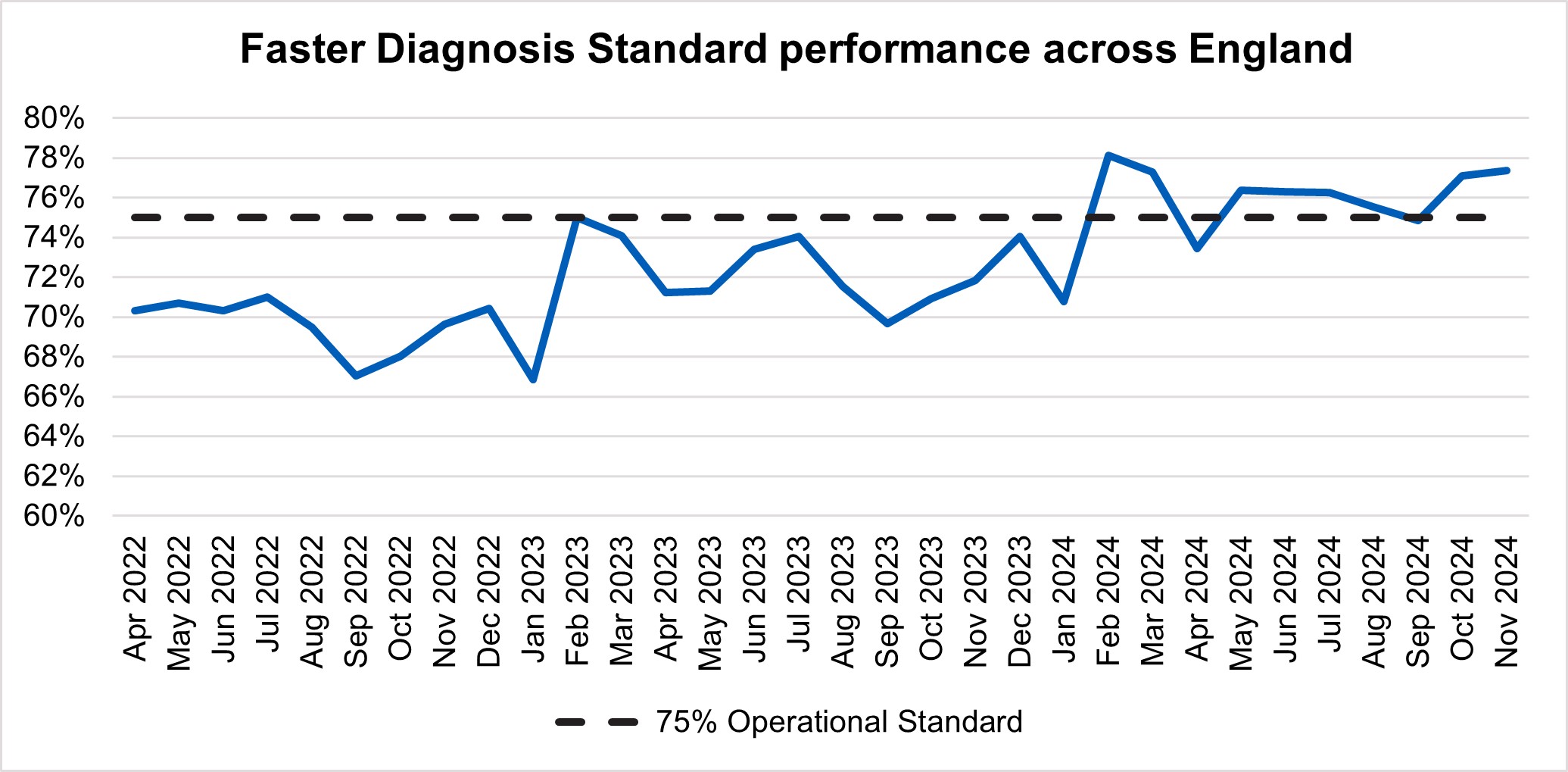
17. The NHS is working hard to keep up with this increase in demand. It has been accelerating the installation of new diagnostic capacity, much of it in Community Diagnostic Centres. Performance against the 28 day faster diagnosis standard in November was 77.4%, which is above the NHS constitutional standard of 75% represents a 5.6% improvement compared to the same point last year and 0.3% improvement on October 2024.
Faster diagnosis standard performance across England
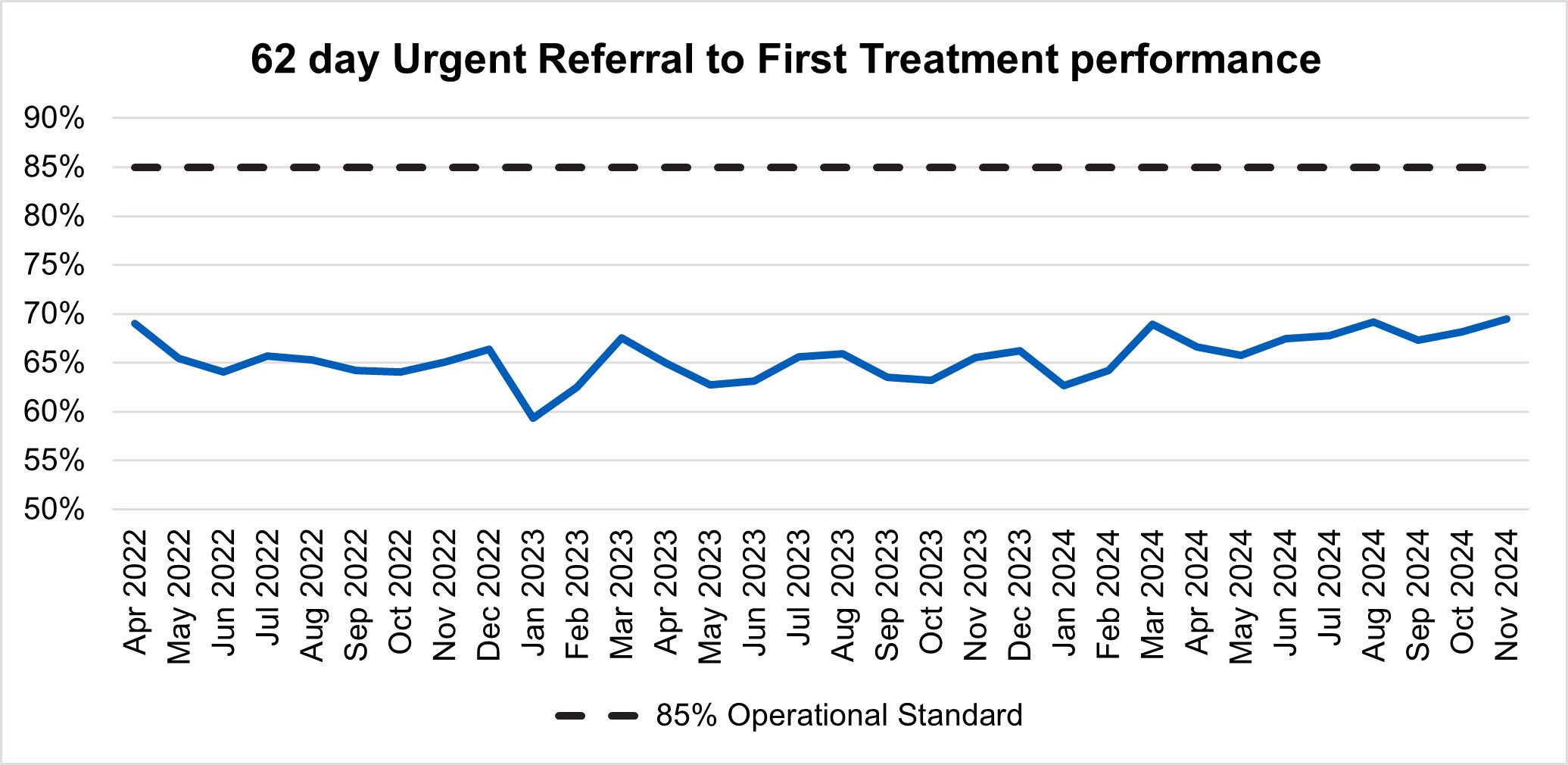
18. In November, performance against the 62 day Urgent Referral to First Treatment Standard, was 69.4% which was 3.9% higher than at the same point last year, and 1.2% higher than October 2024, but still well below where we want to see it. The NHS has set the ambition to improve this to 70% by March 2025, as a first step in recovering performance to the NHS constitutional standard of 85%.
62 day urgent referral to first treatment performance
Primary Care and Community Health Services
19. In 2024/25 we are aiming to make it easier for people to access community and primary care services, particularly general practice and dentistry. We also are improving patient experience through expanding capacity, ensuring people can see a clinician when they need to and increasing use of the NHS App, on information access, routine services such as repeat prescriptions, and booking appointments.
20. As at the end of November 2024, there have been 378.4 million GP appointments in the previous 12 months. This includes COVID-19 vaccinations and Primary Care Network appointments an increase of 0.4% from the previous month and up 22.6% versus end of March 2019/2020.
21. In November 2024, 50% (748,600 per working day) of all practice appointments took place on the same day or day after booking which is a decrease of 0.6 percentage points from November 2023 (722,900), but up 4.9 percentage points from October 2024 (754,300).
22. Just over eight out of out of 10 practice appointments (80.7%) took place within 14 days of booking).
23. Latest publication of Health Insight Survey published 9 January 2025, reported
- 40.0% of the respondents tried to contact their GP practice in the last 28 days. Of these respondents, 77.8% were able to make contact on the same day and of these, 71.0% found it easy to contact their GP practice and 72.7% had a good overall experience with their GP practice.
- 8% of respondents reported having an NHS dentist, compared to 12.0% who reported having no dentist
24. In November 2024, 1,055,712 referrals were waiting for a first treatment from a community health service. From this, the largest waiting lists were for adult musculoskeletal service (340,901), children and young people’s community paediatric service (132,195) and adult podiatry and podiatric surgery (112,239). The community services with the largest percentage of people waiting over 52 weeks in November 2024 were children and young people’s community paediatric services (28% waiting over 52 weeks), adult weight management and obesity services (14%), and children and young people’s therapy interventions: occupational therapy (9%).
Mental Health
25. Work continues with the mental health programme priorities to expand, transform and improve access to care in order to meet significantly increased demand, particularly among children and young people.
26. Access to community mental health services (CMH) is steadily increasing with 640,437 people receiving two or more contacts as of November 2024, a 9% increase compared to 587,099 in November 2023. Newly published CMH metrics further includes the percentage of people receiving meaningful help within four weeks of referral for both Adult CMH and CYP services.
27. The number of people who have completed an NHS Talking Therapies course of treatment in 2024/25 is 455,592 in the year to date as of November 2024 compared to 455,382 in November 2023. In November 2024, 47.6% of those have achieved reliable recovery, with 67.4% achieving reliable improvement.
28. Access to Individual Placement and Support (IPS) services is an evidence-based approach to help people with mental health issues find and keep paid jobs. In the financial year to November 2024, 40,797 people have accessed this service compared to 27,755 in November 2023, an increase of 47%. To further increase access, NHS England is working with IPS Grow (a voluntary, community and social enterprise organisation supporting delivery of IPS) to share learning from five pilot sites aiming to increase referrals from primary care, as well as increase recruitment and retention of staff in the IPS workforce.
29. Improving inpatient flow is a top priority in 2025/26. NHS England continues to work on supporting systems to improve flow and reduce out of area placements, focusing on key issues including data and good practice. Challenged systems are being additionally supported through joint working with the Getting It Right First Time (GIRFT) programme.
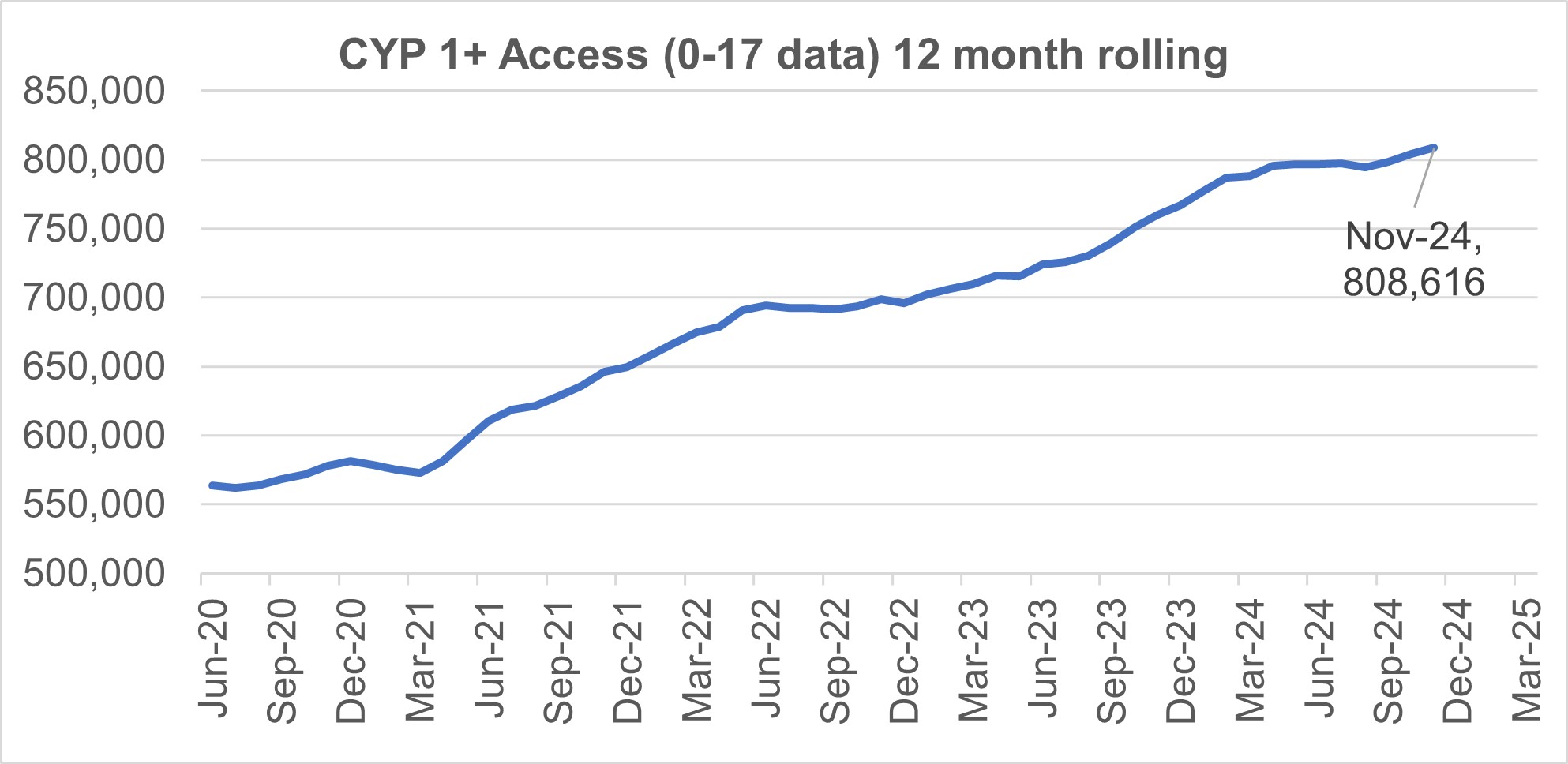
30. As of November 2024, 808,616 CYP aged 0–17 received support (1+ contacts) from an NHS-funded service.
CYP 1+ access (0-17) 12 month rolling
31. CYP eating disorder (ED) pathways continue to be challenged. As of November 2024, 79.9% of routine CYP ED referrals were seen within four weeks, and 83.3% of urgent referrals were seen within one week, an improvement on October 2024 data which showed 77.3% and 81.2% respectively. NHS England continues to work with providers to improve the quality and completeness of data submissions which aims to support improved reporting of performance against the 95% access and wait standard.
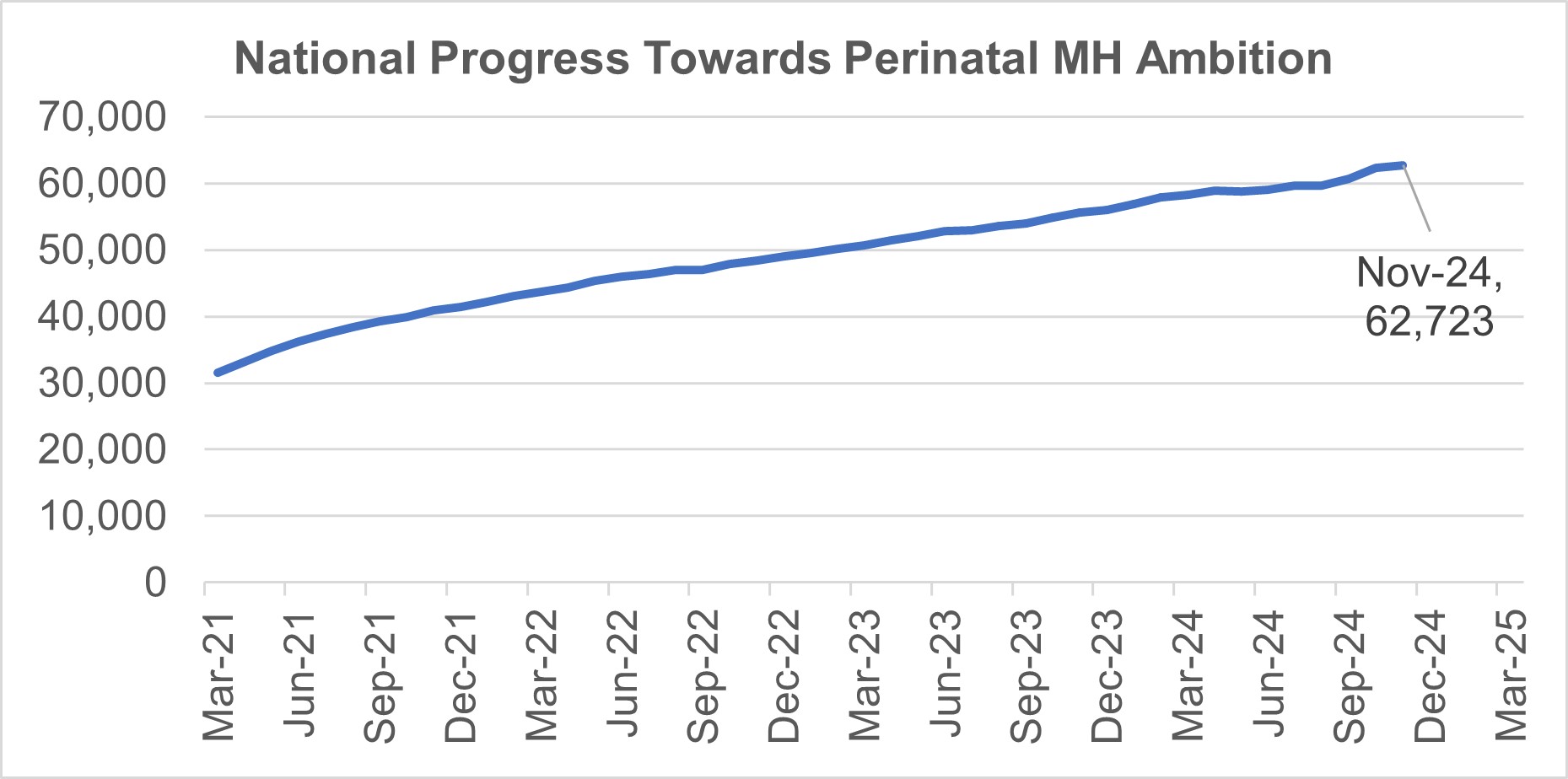
32. Access to specialist perinatal mental health (PMH) and maternal mental health services (MMHS) has seen steady growth since March 2021. In the 12 months to November 2024, 62,723 women accessed these services which is an increase of 12.9% from 55,561 in the 12 months to November 2023. Best practice on data quality and overcoming delivery challenges continues to be shared in order drive up access.
National progress towards perinatal MH ambition
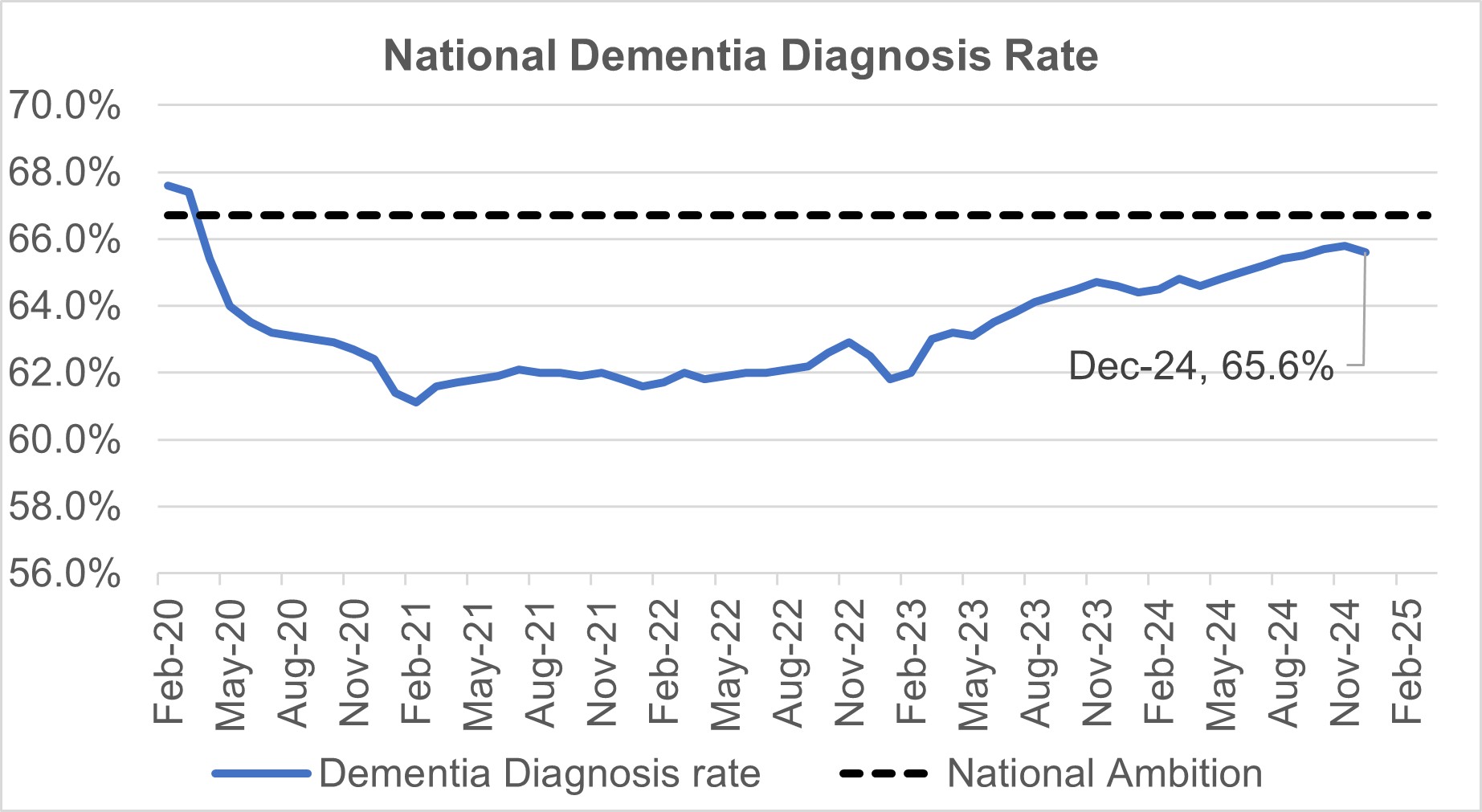
33. The dementia diagnosis rate (DDR) has continued to steadily improve since January 2023. For December 2024 the DDR is 65.6% compared to 64.6% in December 2023. The number of people with a recorded dementia diagnosis has reached 498,000. NHSE England sponsored 14 sites to pilot the DiADeM (Diagnosing Advanced Dementia Mandate) protocol, supporting configuration of alternative pathways for dementia diagnosis via care home settings. All pilots were completed at the end of May 2024, and it is anticipated that learning will be shared by end of Q4 2024/25.
National dementia diagnosis rate
34. NHS England has committed to developing reporting against the nationally-held data and information set out in the Patient and Carer Race Equality Framework (PCREF) for 2024/25.
Learning Disabilities and Autism
35. There continues to be a steady reduction in the number of adults with a learning disability and/or who are autistic in a mental health inpatient setting. Provisional data for December 2024 shows there were 1,835 adult inpatients, a reduction of approximately 8% from the inpatient population as of March 2024.
36. As of December 2024, provisional data shows there were 210 inpatients under the age of 18 with a learning disability and/or who are autistic. Since March 2017 there has been a decrease in ‘under 18’ inpatients with a learning disability and/or who are autistic.
37. There has been an increase in the number of people receiving an annual health check compared to the same period last year. Up to November 2024, 44.9% of people on GP learning disability registers received a check, compared to 39.5% between April and November 2023. We remain on trajectory to achieve the 75% annual health check target by March 2025.
Proportion of people aged 14+ with a learning disability on the GP register receiving annual health check
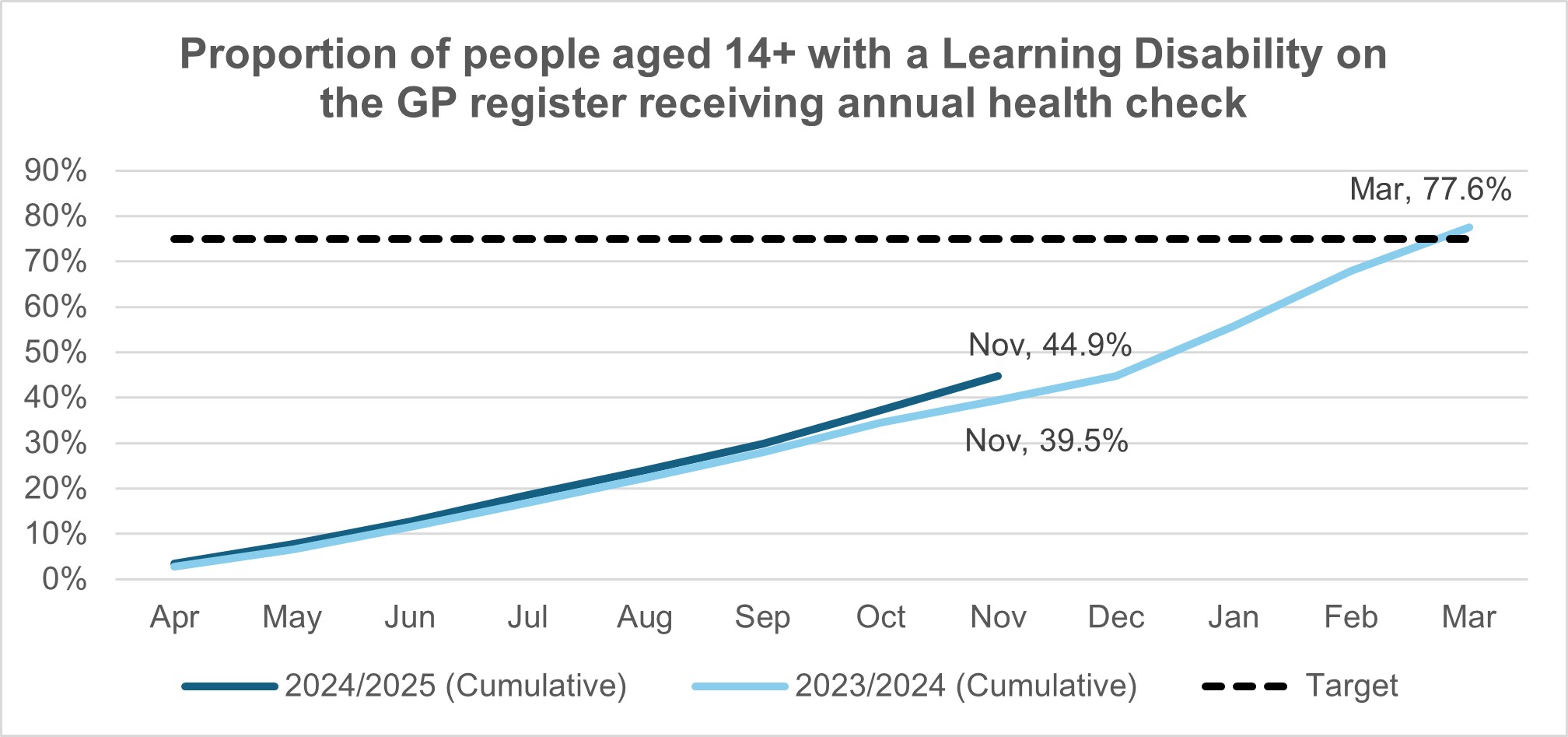
38. As of November 2024, there were 336,321 people aged 14 and over on GP learning disability registers, representing a decrease of 10,942 (3%) compared to the position in November 2023.
Prevention and Long Term Conditions
39. A total of 10 dental and eight optometry sites have been selected to take part in the pilots to test the effectiveness of Blood Pressure checks in wider primary care settings and funding has been transferred to systems. A community of practice group has been set up to support successful sites to share experiences and good practice As of December 2024, 12 sites have gone live, we are expecting a further three sites to have gone live in January. The pilots will run until summer 2025 and the evaluation partner (South West Health Innovation Network) will report on their findings by Autumn 2025.
40. From 2016 to 2023, around 1.3 million referrals have been made into the Healthier You NHS Diabetes Prevention Programme, with the programme to set to achieve or exceed the ambition of 160,000 new participants benefitting from the programme in 2024/25.
41. National review of 26 mechanical thrombectomy (MT) sites with National Medical Director Steve Powis has been completed supporting the ambition to increase access. Follow up visits to select Mechanical Thrombectomy sites are being arranged with Prof. Powis throughout Q4/Q1.
42. To support the improvement in the time it takes for patients to be transferred from non-heart attack centres to heart attack centres a national review of inter-hospital transfers for patients following a heart attack has resulted in the ambulance service prioritisation of these transfers in line with that of a Category 2 dispatch. The national guidance for inter-facility transfers has been updated to reflect this amendment for cardiac patients. Impact of this initiative is being monitored.
Recovery Support Programme
43. The Recovery Support Programme (RSP) provides national mandated intensive support to trusts and ICBs in NHS Oversight Framework segment 4 that have complex, deep-seated concerns around leadership, governance, finance, patient safety, quality, or performance. There are currently 20 trusts and 3 ICBs in the RSP. Since the launch of the programme in 2021, a total of 12 organisations have successfully exited the programme after meeting the agreed exit criteria in their improvement plan.
Genomics
44. The NHS continues to provide and develop the NHS Genomic Medicine Service (GMS), delivering over 809,000 genomic reports in 2023/24.
45. The NHS GMS has now sequenced over 126,000 Whole Genome Equivalents since the inception of the Whole Genome Sequencing (WGS) service in November 2021.
46. As a result of increased growth in testing in the NHS GMS, compliance with turnaround times has been impacted. Minimising backlogs and the time taken to deliver a genomic test is a key priority for NHS England and the NHS Genomic Laboratory Hubs (GLHs). NHS England continues to monitor the backlogs as part of the NHS GLH assurance framework, and those NHS GLHs with a backlog have submitted a backlog recovery plan to NHS England which is reviewed and monitored closely in contract monitoring meetings. A number of NHS GLHs do not have a backlog.
Publication reference: Public Board paper (BM/25/02(Pu)

