Organisation objective
- Statutory item
Executive summary
1. Pressure has continued in emergency departments across the country, with 2.2 million A&E attendances, the busiest October on record, and over 547,000 emergency admissions in October 2023, the highest number since January 2020.
2. Ambulance services also faced their busiest month this year for category 1 and category 2 callouts, and answering more than 850,000 calls to 999, the highest figure in 2023 so far.
3. Continuing industrial action in the NHS has had a significant impact on patients. Since strikes began, the cumulative total of rescheduled acute inpatient and outpatient appointments exceeded one million for the first time.
4. The NHS is treating more people than before the pandemic, with 1,446,805 patients starting treatment in September, an increase of 5% from the same month last year and an increase of 2% compared with the same month in 2019. Improvements have also been made on the number of patients waiting more than a year for treatment, which is down by more than 5,500 since August 2023.
5. For the first time, the NHS has published the number of individual patients on the waiting list – 6.5 million – in addition to the total number of appointments and treatments currently on the waiting list – 7.77 million.
6. Demand for cancer services continued at record levels in September 2023, with the number of urgent suspected cancer referrals at 130% of pre-pandemic levels. Treatment is also at record levels and there has been a reduction in the 62-day cancer backlog as a result.
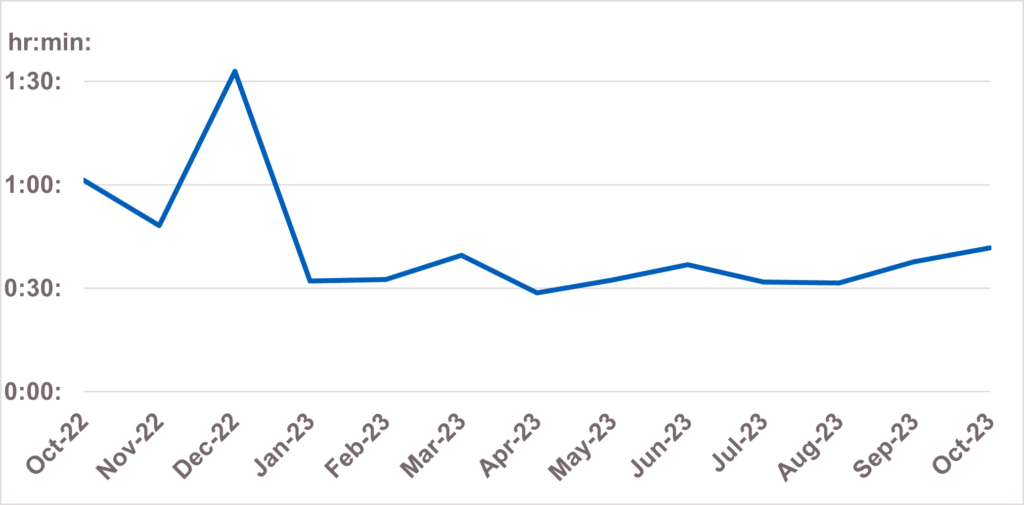
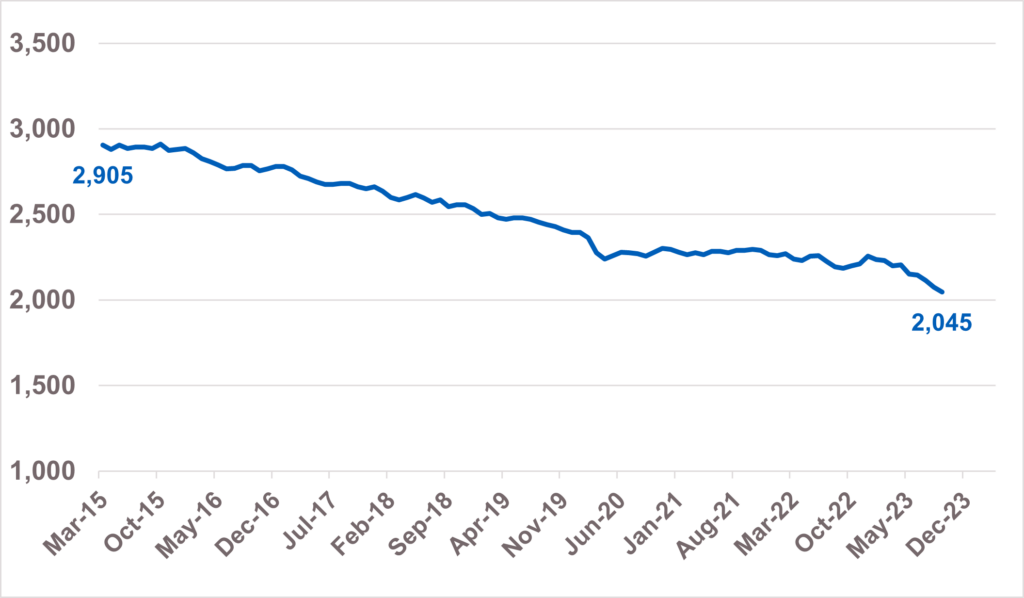
7. The NHS has made progress in reducing the number of people with a learning disability and autistic people in inpatient mental health settings. This has decreased by almost 30% since March 2015.
Urgent and emergency care
8. Three days of joint industrial action by junior doctors and consultants placed extraordinary pressure on urgent and emergency care in October. With little time to recover from the previous round of industrial action, hospital discharges slowed which inevitably impacted patient flow.
9. There were 2,219,618 attendances in A&Es across England, an average of 71,601 per day. This is an increase of 1.4% compared to October 2022 (2,188,028 people attended A&E in October 2022).
10. Despite this, the proportion of patients attending A&E who were admitted, transferred or discharged within four hours remained above last year, at 70.2% compared to 69.5% in October 2022.
11. Ambulance services answered 858,059 calls to 999, or 27,679 per day, the largest in 2023 so far. They also handled 724,362 incidents, the largest since December 2021.
12. The average response time for a category two call was 41 minutes and 40 seconds. This is 19 minutes and 39 seconds faster compared to the same month last year (the average category two response time for England excluding London was 1:01:19 in October 2022).
Average C2 response times:
13. We have also been working with systems to develop a new metric that records and measures the time between a patient’s discharge ready date and their actual date of discharge. This month, as per our commitment in the urgent and emergency (UEC) recovery plan, we have published this dataset for the first time.
14. While this data is currently in development with submissions from 53.3% of trusts meeting the required data quality and compliance, its publication signifies an important step towards a better understanding of why and where discharge delays are occurring. This intel will support collaborative action across the NHS, local government, and social care to improve discharge planning and patient flow.
15. Data shows, during September, 86.4% of patients with a hospital stay of one night or longer left hospital on their discharge ready date. Of those who stayed in hospital beyond their discharge ready date, 33.1% left hospital one day after their discharge ready date and 6.2% had an extended stay of 21 days or more.
Elective recovery
16. Industrial action continued to have a significant impact on planned care in September. Two days of joint action meant that since strikes began, the cumulative total of rescheduled acute inpatient and outpatient appointments exceeded one million for the first time.
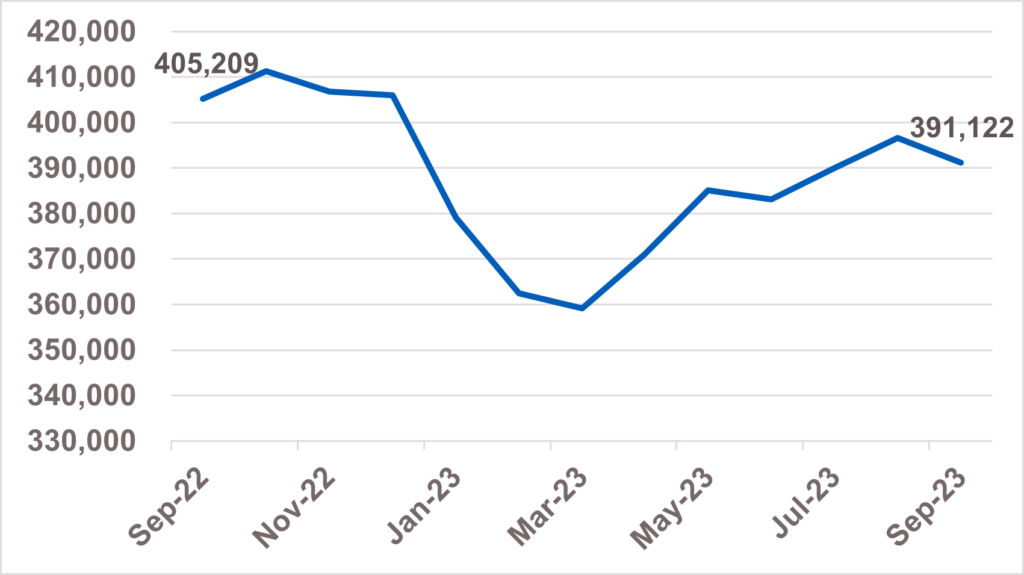
17. As of the end of September, 391,122 (5%) patients were waiting more than a year for treatment. This is down by more than 5,500 since August 2023.
Referral-to-treatment 52-week waits:
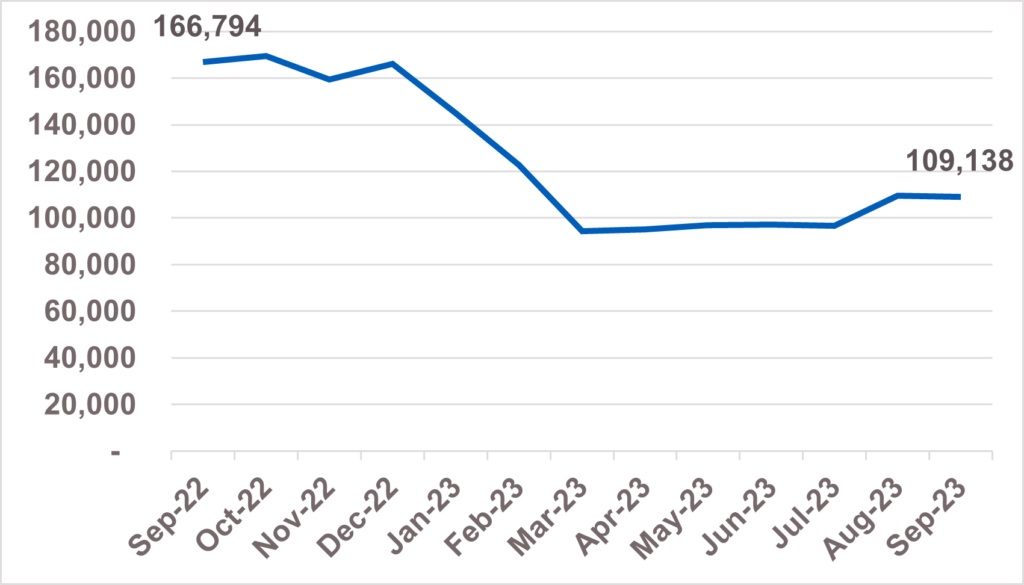
18. 109,138 (1.4%) patients were waiting more than 65 weeks for treatment. This is down by more than a third since September 2022.
Referral-to-treatment 65-week waits:
19. 1,446,805 patients started treatment in September, an increase of 5% from the same month last year and an increase of 2% compared to September 2019. Of those, 947,400 started treatment within 18 weeks of referral. This is an increase of 0.3% from the same month last year.
20. A patient’s waiting time for elective treatment starts when they are referred to a consultant-led service in secondary care – this is known as a clock start.
21. As a patient moves through an elective pathway, they can also be referred for investigation and treatment for a different condition. In this case, a separate referral to treatment waiting time clock will start.
22. While there are 7.77 million waits for care, some of these people are waiting to be seen for more than one condition. Data published this month estimates there are 6.5 million unique patients on the elective waiting list, meaning an 83.6% ratio of unique patients to total waits.
Cancer
23. Demand for cancer services continued at record levels in September with the number of urgent suspected cancer referrals at 130% of pre-pandemic levels. To meet high demand, treatment is also at record levels and there has been a reduction in the 62- day cancer backlog as a result.
Urgent suspected cancer referrals first seen:
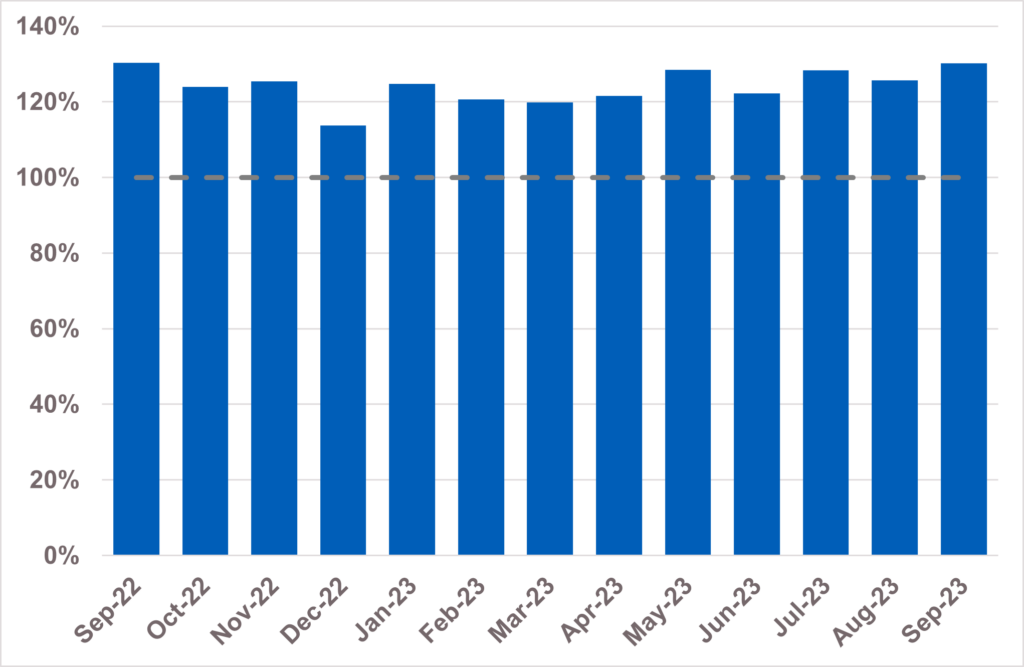
24. Over 335,000 people received treatment for cancer over the last year between October 2022 and September 2023 – the highest year on record, and up by more than 22,000 on the same period pre-pandemic. GPs have been referring people for urgent cancer checks in record numbers since March 2021. Since then, NHS staff have seen over a million more people than in the same period prior to the pandemic.
25. The increase in referrals has contributed to the NHS diagnosing more cancer at an early stage than ever before. We are diagnosing a higher proportion of cancers at an early stage now than ever before – about 2% higher than before the pandemic. Survival is also at an all-time high. In 2023, the Annals of Oncology published findings showing that cancer deaths are around 10% lower in the UK compared to just 5 years ago.
Cancer early diagnosis rate across England:
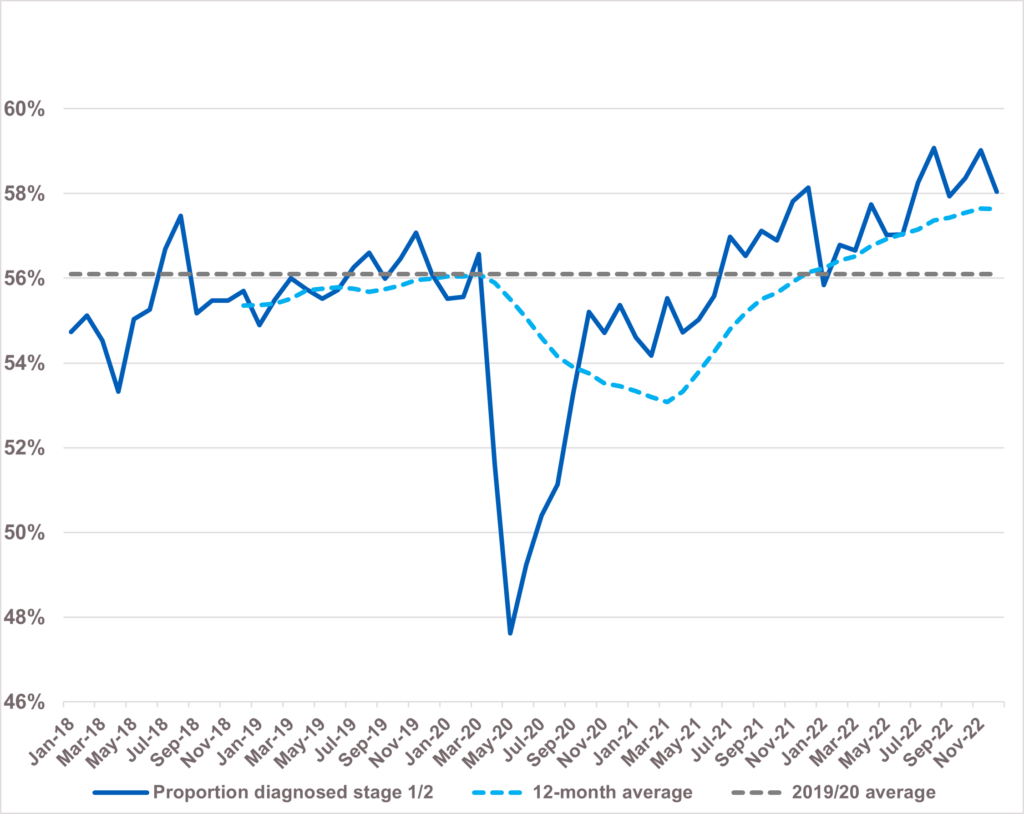
26. The NHS is working hard to keep up with this increase in demand. It has been accelerating the installation of new diagnostic capacity, much of it in Community Diagnostic Centres. The backlog has already reduced by 14,000 people since its peak last summer, and despite the recent seasonal increase, NHS staff remain focused on ensuring that people who have been waiting longest or who need care most urgently are seen first.
Learning disabilities and autism
27. The NHS has made progress in reducing the number of people with a learning disability and autistic people in inpatient mental health settings.
28. There are currently 2,045 people with a learning disability and autistic people in a mental health inpatient setting, compared to 2,905 in March 2015. This represents a decrease of almost 30% against a commitment to reduce inpatient numbers by 50% by March 2024.
Total people with a learning disability, autism or both (adults and U18s) in hospital:
29. There is a significant difference in the trend in the number of inpatients with a learning disability to the number of autistic patients. For people who have a learning disability and who do not have an autism diagnosis, there has been a 57% reduction in the number of people in hospital since March 2015.
30. For people who have a learning disability and also have an autism diagnosis, there has been a 33% reduction in the number of people in hospital since March 2015. The number of people with an autism diagnosis in hospital inpatient settings has increased significantly over the same period.
Trends for different groups of people in hospital since March 2017:
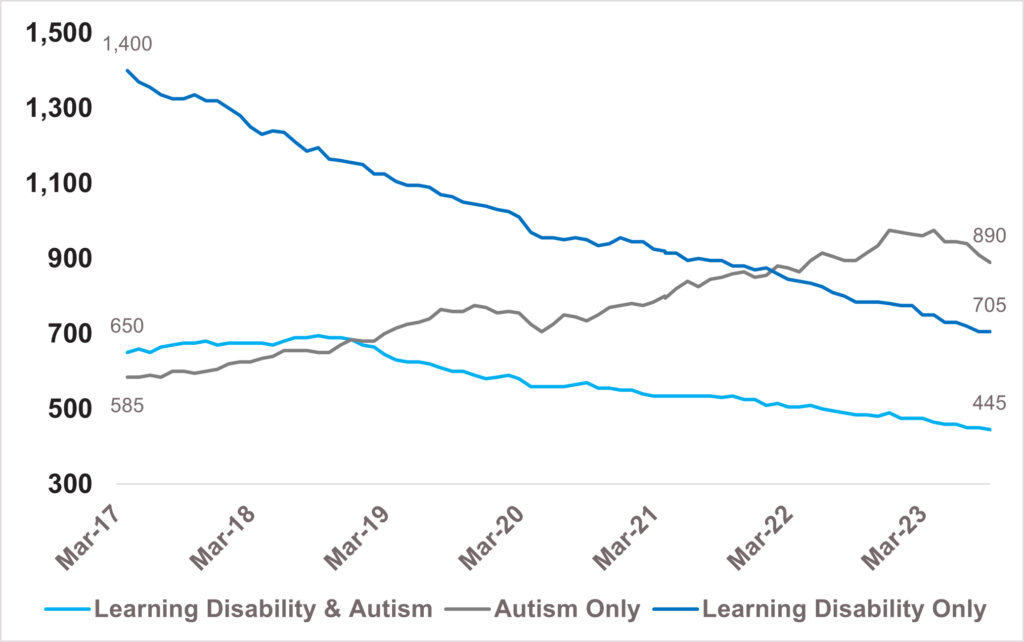
`31. There are a number of factors behind the increase in of people in mental health inpatient services with a diagnosis of autism. Both referrals to autism assessment services and the number of people who receive a diagnosis of autism are increasing rapidly, and more autistic people are being diagnosed during their stay in a mental health hospital. People who are autistic have a higher prevalence of mental ill health compared to the general population and many of these admissions may represent the most appropriate care for people who need mental health care in hospital.
32. The NHS is committed to ensuring that autistic people in mental health settings receive the right care and support.
Annex: Operational performance update
Agenda item: 4.1 (Public session)
Report by: N/A
Paper type: For information
7 December 2023
Executive summary
This annex provides a more comprehensive summary of operational performance based on published data and work to restore services.
Elective care
1. Despite ongoing pressures and industrial action in September, including joint action by both Consultants and Junior Doctors, progress continues to be made.
2. There has been further progress in reducing the number of people waiting the longest for care, despite industrial action. Waits of more than 65 weeks reduced to 109,138 in September. This is down by 53% on the peak of 233,051 in June 2021, and down by 35% from 166,794 in September last year.
3. The latest figures show the median wait for admitted treatment in September 2023 was 11.8 weeks, against the a median wait of 12.6 weeks in September 2022.
4. NHS England wrote to providers on 8 November to provide clarity on the funding and actions the NHS has been asked by Government to take to manage the financial and performance pressures created by industrial action. The letter asked systems to complete a rapid two-week exercise to agree actions required to deliver the priorities of protecting patient safety and prioritising emergency performance and capacity, while protecting urgent care, high priority elective and cancer care for the remainder of the financial year – alongside financial balance.
5. The Further Faster GIRFT programme is continuing with a second cohort of providers onboarded. It focuses on supporting Outpatient transformation in high-volume low complexity specialties, delivering rapid clinical transformation. Learning from cohort one is being shared with cohort two trusts through speciality level work and handbooks to help share best practice from cohort one trusts.
6. As at the end of September 2023, the overall waiting list was 7.77 million. UEC (including Discharge)
7. The UEC Recovery Plan was published in January 2023.
8. Four days of joint industrial action by junior doctors and consultants across September and October placed additional pressure on urgent and emergency care, with 10 months in total of industrial action. With little time to recover from the previous round of industrial action, hospital discharges slowed which inevitably impacted patient flow. The UEC system also continues to face increasing demand. These factors combined have led to higher bed occupancy rates and flow challenges through hospitals causing longer waiting times in emergency departments. There were 2,219,618 attendances in A&Es across England (October 2023) (an increase of 1.4% compared to October 2022) and an 8.0% increase in total emergency admissions over the same period. Ambulance services answered 858,059 999 calls in October 2023 (the highest in 2023 so far). They also handled 724,362 incidents – the highest since December 2021.
9. Despite this, A&E performance was recorded at 70.2%, and Category 2 Ambulance response times were 41 minutes and 40 seconds. This is an improvement on last year in both cases, with Cat2 response times almost 20 minutes faster.
10. There is a focused effort on managing risks within the system. One example of this is working with systems who have long ambulance handover delays, which in turn impacts ambulance Cat2 response times, meaning that there is a high risk in the community with those who are waiting for an ambulance. We have seen early positive signs in two organizations who have implemented new processes to manage this and are working with others to implement improvements.
11. We have met our ambition to scale up capacity to more than 10,000 virtual ward beds with 10,421 beds available as of September to help patients get hospital-level care at home safely and in familiar surroundings.
12. In November we have also published a new Discharge Ready Date metric which measures the actual delay for discharges, as committed in the UEC Recovery Plan. This will support ongoing work to reduced delays to discharge and improve flow. While this is experimental data, in September it suggests that of those who identified as staying in hospital beyond their discharge ready date, 33% left hospital one day after their discharge ready date, and while 6% had an extended stay of 21 days or more.
Diagnostics
13. 2.2 million of the 15 key diagnostic tests were performed in September 2023 9% more than in September 2022. The percentage of patients waiting less than six weeks for a diagnostic test improved slightly, from 72.5% in August 2023 to 73.7% in September. The rise in activity was driven by a growth both in elective planned activity and in unscheduled (urgent and emergency) activity.
14. The 135 operational Community Diagnostic Centre sites have delivered 5.81m tests since the first CDC was launched and 2.18m tests in-year – 8% ahead of activity plan.
Cancer
15. As at w/e 1 October 2023, there were 24,920 patients waiting longer than 62 days following an urgent suspected cancer referral, for either exclusion of cancer or for cancer treatment to start. This represents an expected seasonal increase in comparison to the April 2023 position but remains 8,590 lower than the same point last year.
16. The 28-Day Faster Diagnosis Standard (FDS) means patients with suspected cancer who are referred for urgent cancer checks should be diagnosed or have cancer ruled out within 28 days. Performance against the FDS was 69.7% in September 2023, compared to 71.6% in August 2023. The drop in performance reflects expected seasonal patterns during August and September, as well as the impact of industrial action. Despite this, FDS performance in September 2023 was still 2.7% points higher than at the same point last year, and we are maintaining our focus on delivery of the 75% target by March 2024.
17. We saw performance against the 62-day urgent suspected cancer referral to first treatment standard decrease to 59.3% in September 2023, from 62.8% in August 2023. Although performance against this standard also regularly drops in September due to seasonal factors, we know that industrial action disproportionately impacts the treatment end of cancer pathways, and particularly challenges performance against the 62-day standard.
18. The level of demand for cancer services remained high in September 2023 with the number of urgent suspected cancer referrals at around 130% of pre-pandemic levels. The NHS has increased the levels of first treatments provided in response which are 7% above pre-pandemic levels. Referrals on non-specific symptoms pathways for patients presenting with vague symptoms who may have cancer continue to exceed targets, with 5,531 referrals in September 2023. This is an increase of 15% from the previous month.
19. Progress continues to be made against our transformation initiatives. Since its inception in April 2019, the Targeted Lung Health Check (TLHC) programme has discovered 2,705 lung cancers, 74% at stage one or two, with nearly 1.2m people invited for a lung check. All Cancer Alliances now have TLHC services in operation.
20. The National Cancer Programme has prioritised rolling out Targeted Lung Health Checks (TLHCs) in areas of highest deprivation first which is already having a positive impact on health inequalities. People in the most deprived quintile are now more likely to be diagnosed with lung cancer at an early stage (one or two) than those in the least deprived quintile. In the 12 months to June 2023 more than a third of people living in the most deprived quintile who were diagnosed with lung cancer were diagnosed at stage one or two (36.3%), up from 29.3% in the 12 months to December 2019. Those diagnosed with lung cancer at stage one are 11 times more likely to survive for five years or more compared to those diagnosed at stage four.
21. Our Community Liver Health Checks project has built on the success of the Hepatitis C Elimination programme, to offer fibroscans to people at high risk of cirrhosis and advanced fibrosis (and therefore liver cancer) and refer them into 6-monthly liver ultrasound surveillance. To date, 31,301 fibroscans have been delivered, finding 3,105 people at risk of liver cancer and 2,536 people have already been referred into liver surveillance.
Primary care and Community Health Services
22. The Primary Care Access Recovery Plan (PCARP) was launched in May 2023. The plan responds to feedback from patients and outlines measures that will make a difference to patients and staff now, supporting primary care teams to improve and recover access in general practice. A programme of work is in place focusing on the following four areas:
i. Empowering patients to manage their own health including using the NHS App, using self-referral pathways and through accessing more services offered from community pharmacy.
ii. Implementing Modern General Practice Access to tackle the 8am rush, provide rapid assessment and response and avoid asking patients to ring back another day to book an appointment.
iii. Building capacity to deliver more appointments from more staff than ever before and adding flexibility to the types of staff recruited and how they are deployed.
iv. Reducing the workload across the interface between primary and secondary care, and the burden of medical evidence requests so practices have more time to meet the clinical needs of their patients.
23. The number of appointments taking place in General Practice continues to increase. In the 12 months to September 2023, 356.7 million appointments took place, including 9.7 million for COVID-19 vaccinations delivered by general practice. Adjusting for working days, this is 17% higher than the number of appointments carried out at the start of the Long Term Plan in the 12 months to March 2019.
24. The Department of Health and Social Care (DHSC) and NHS England have begun the period of consultation with the BMA General Practitioners Committee (GPC England) on changes to the GP Contract in 2024/25.
25. Workforce data shows that as of 30 September 2023 there were 37,419 FTE doctors working in general practice in England. This is an additional 8.4% compared to the baseline of 31 March 2019 and reflects the continued increase in GP training places, although the number of fully qualified GPs has reduced by 4.2% over the same period. The NHS Long Term Workforce Plan sets out plans to further increase GP training and we are developing a streamlined retention offer for qualified GPs.
26. Monthly contracted dental activity has fluctuated across the year. In October 2023, 83% of contracted dental activity was delivered across England.
27. We continue to make progress towards launch of Pharmacy First. For example, as of 10 November 2023, the NHS Lateral Flow Device (LFD) Tests Supply Service became available for patients who are potentially eligible for COVID-19 treatments to collect free of charge from one of 4,415 participating pharmacies who had registered to provide the service.
Mental health
28. The NHS continues to deliver at pace against public commitments as set out in the Long Term Plan (LTP) despite significant challenges including increased demand and prevalence. A number of mental health commitments continue to be met including:
- The Talking Therapies RTT targets of 75% within 6 weeks and 95% within 18 weeks, with performance in August 2023 of 89% and 98% respectively.
- The Early Intervention in Psychosis (EIP) waiting time standard of 60%, with performance in August 2023 reaching 69.2%.
- Access to Community Mental Health Services, which continues to increase. 546,875 people received 2+ contacts in the 12 months to July 2023, an 8.5% increase since the same period the previous year, and above the expected level of 5%.
- There are now 37 established sites for specialist mental health provision for rough sleepers, exceeding the LTP ambition of 20 sites by 2023/24.
29. There has been year-on-year improvement for access to Individual Placement and Support (IPS) services. For the year to date to September 2023, 20,000 people had accessed IPS services, a 28% increase from the September 2022 position.
30. There are currently 12 gambling clinics in operation and a further three clinics will be opening during Q3 2023/24, bringing the total to the LTP ambition of 15 by the end of March 2024.
31. In Q2 2023/24, 280,000 physical health checks were delivered to people living with severe mental illness (SMI). Physical health checks are an important metric with which to measure the reduction of health inequalities in mental health given the higher mortality rate among people with SMI.
32. In November 2023 NHS England published data on the median and longest waits in adults and children and young people (CYP) for community mental health, learning disabilities and autism services for the first time. Alongside prioritising publishing and managing these long waits we will be working with providers to improve data quality of the returns.
33. There continues to be extremely high demand for services, as well as capacity issues, with a number of areas remaining significantly challenged as a result:
- The UEC pathway continues to experience pressure. There continue to be challenges with flow through the system, meaning that Out of Area Placements (OAPs) remain high. In August 2023, 435 new inappropriate OAPs were started, although this represents a decrease of 3% since July 2023. Discharge challenges remain significant, and local organisations are working with partners in social care to resolve where possible. NHS England have prepared and circulated a Winter Resource Pack to regions which will assist with planning this winter, which includes good practice across the mental health pathway and dedicated sections on CYP, and Learning Disability and Autism.
- CYP Eating Disorders pathways continue to be pressured, with 71.1% of CYP starting urgent treatment within one week in the three months to August 2023, an increase from 67.5% in July 2023. 73.2% started routine treatment within four weeks in August 2023, an increase from 71.1% in the previous month.
- The number of patients accessing NHS Talking Therapy services for the first time in August 2023 is 107,361.
- 51,716 women accessed a specialist community perinatal mental health service or a maternal mental health service in the 12 months to August 2023. Access is increasing with a 9.5% increase compared to the same period last year.
34. Across all challenged areas, NHS England is working closely with regions and systems to determine how best to mitigate key risks, address delivery challenges and offer support. As the initial 5-year part of the 10-year LTP comes to an end, work is underway to create a vision that will unite the sector behind future priorities for further transformation over the next 5–10 years.
35. Progress has been made in expanding the workforce, which is the biggest risk to delivery and transformation. Between March 2016 and June 2023, the mental health workforce increased by 35,508 WTE – equating to 32% growth, compared to 25% growth in the rest of the NHS. Workforce expansion remains a priority, as does addressing high vacancy rates, particularly in mental health nursing which is experiencing vacancy rates of around 19%. NHS England continues to work with regions and systems to identify and implement high-impact initiatives to improve retention and to increase supply.
Learning disabilities and autism
36. There remain health inequalities for people with a learning disability. Data gathered via the LeDeR programme and other sources evidence that 49% of the deaths of people with a learning disability in 2021 were avoidable, compared to 22% in the general population. In addition, the median age of death for people with a learning disability was 61 compared to 82 in the general population. Inequalities are even starker for people from ethnic minority groups with the average life expectancy for people with a learning disability from an ethnic minority being 34, compared to 62 years for people from non-ethnic minority groups.
37. An action plan is being developed in response to the NHS Race and Health Observatory report on health inequalities for people with a learning disability from ethnic minority communities, with a further range of actions being taken to reduce health inequalities. These include the learning disability Annual Health Check programme, with performance at August 2023 showing an improvement on the same reporting period last year. Consequently, we are on track to meet our LTP commitment that by March 2024, at least 75% of people aged 14 and over on the GP learning disability register will receive an Annual Health Check. Work is also focussing on the supporting health actions plans that accompany a health check, and on increasing the size of GP learning disability registers. In addition, a specific health check for autistic people has been created and is currently being piloted in four NHS regions.
38. Work continues to improve primary and secondary prevention of long-term conditions for people with a learning disability and autistic people. This includes increasing access to COVID and flu vaccinations, introducing pneumococcal vaccinations, supporting initiatives across obesity, diabetes, CVD and respiratory programmes, and increasing levels of cancer screening.
39. The number of people with a learning disability and autistic people in a mental health inpatient setting has reduced by 30% since March 2015, to 1,842 adults and 205 under 18s as at September 2023. Since March 2015 there have been significant reductions in inpatient numbers for people with a learning disability, and for people with a learning disability who are also autistic. However, the number of people with an autism diagnosis (with no learning disability) in hospital inpatient settings has increased significantly over the same period.
40. There has been a 46% increase in referrals for people waiting for an autism assessment between June 2022 and June 2023, with demand outstripping supply by 4,000 referrals per month. The Oliver McGowan ‘train the trainer’ autism training for mental health care providers has now been rolled out for residential special schools and youth justice settings.
Prevention and long term conditions
41. Thrombectomy and thrombolysis activity continues to track towards trajectory, with increased adherence to the National Optimal Stroke Imaging Pathway (with 92% of units introducing AI decision support), video triage for rapid diagnosis, publication of a GMC thrombectomy credential, and funding for additional equipment and QI initiatives to increase thrombolysis rates. Implementation of the National Integrated Community Stroke Service (ICSS) model is being directed by the Stroke Quality Improvement in Rehabilitation (Squire) programme.
42. Latest published data from the National Respiratory Audit Programme shows 58% of the patients who had initial assessment in August 2023 and enrolled for PR, completed a discharge assessment. This figure has remained relatively stable over the past four years.
43. Over 1.3 million referrals have been made into the NHS Diabetes Prevention Programme to date. A recent independent evaluation looking at programme completers found that they reduce their risk of developing type-2 diabetes by 37%, and the programme in general resulted in a 7% reduction in population-level incidence in areas where the programme was delivered between 2016 – 2018. When looking at people referred to the programme, the latest independent research published in February 2023 demonstrated a 20% reduction in incidence in those at risk of type 2 diabetes that are referred into the programme compared to those not referred.
44. The NHS Type 2 Diabetes Path to Remission Programme is currently available in 70% of the country (30 ICSs). To date over 14,600 referrals have been made. Early data indicates participants each lose 7.2kg (over one stone) on average after one month, and 13.4kg (over two stone) after three months. This is in line with the outcomes seen in the trials where participants were able to improve their diabetes control, reduce diabetes-related medication and, in around 50% of cases put their type 2 diabetes into remission.
45. The 2023/24 operational planning guidance highlights hypertension and lipid management as key targets for improvement. Two new QOF indicators for cholesterol have been introduced in 2023/24. In June 2023, 60.3% of people with a high-risk score were being treated with lipid lowering therapy meaning the 2023/24 Operational Priorities and Planning Guidance target has been met. Recently published QOF data indicates that in 2022/23 6.2 million patients with hypertension were managed to NICE targets. This is 175,000 more than pre-pandemic in 2019/20. Up to June 2023, 66.7% of the hypertension patients in England are managed to target. This is over 7 percentage points improvement compared to June 2022, although there is variation across the ICBs. 23/24 planning guidance goal is 77%.
46. A key ambition of the LTP is reduced death from heart attacks. Timely emergency treatment following a heart attack is important to improve clinical outcomes. From 14 August to 30 September 23 the NHS ran a public NHS heart attack campaign aimed at helping the public recognise the symptoms and call 999 sooner. Revised standards of performance have been agreed to support improving the emergency management of the most serious type of heart attacks, to improve clinical outcomes and will be monitored through the national heart attack audit. Cardiac rehabilitation is a NICE recommended intervention which can save lives, improve quality of life and reduce hospital readmissions. In 2023/24 targeted funding has been allocated to systems to support improved provision of cardiac rehabilitation for all suitable patients following heart attack and patients newly diagnosed with heart failure. Evaluation of the funded schemes is ongoing.
Screening and vaccinations
47. All NHS screening programmes have removed backlogs caused by the pandemic including breast screening. Funding has been provided to increase the number of advanced breast screening practitioners being trained.
48. The NHS bowel cancer screening programme continues to exceed the 65% uptake target with age extension to 58-year-olds and 56-year-olds rolled out as planned since 2021/22 and the roll out to 54-year olds having commenced as planned from April 2023. A marketing campaign to promote the return of bowel screening FIT kit (home testing) samples was run in February and March 2023 and successfully increased uptake. There will be an additional campaign in London later in 2023.
49. Uptake for the NHS diabetic eye screening programme continues to meet the efficiency standard. Uptake of initial ultrasound screens in the Abdominal Aortic Aneurysm screening programme is exceeding the achievable standard.
50. In October, the Diabetic Eye Screening programme commences moving participants assessed as low risk to biannual screening. This complies with a recommendation of the United Kingdom National Screening Committee and reduces the need for participants to attend unnecessary appointments.
51. The three NHS antenatal and three NHS new-born screening programmes continue to achieve continuous coverage levels close to 100%.
52. The Sickle Cell and Thalassaemia programme is participating in a national initiative to improve lifetime care for people suffering from sickle cell and thalassaemia disease.
53. The use of a new vaccine and an increase in eligible cohorts for the Shingles Immunisation Programme is well underway with delivery having commenced from September 2023.
54. A change in HPV schedule for adolescent boys and girls primarily administered in schools is underway with delivery from September 2023 which means eligible adolescents will only require one dose of the vaccine to be fully protected.
55. There is a focus on increasing the MMR vaccine as part of a catch-up campaign being delivered during 2023/24 to address the fact that England has lost its measles elimination status.
56. Changes to the targeted neonatal BCG vaccination programme following the introduction of a new neonatal screening programme in 2020 are being monitored closely to improve uptake amongst at risk babies.
57. The 2023/24 delivery for the seasonal flu and COVID-19 vaccinations programmes were accelerated to September in line with government guidance. The 2023/24 flu immunisation programme made its fastest ever start with improvements in uptake across cohorts and for those most at risk. Improvements in uptake have been seen in cohorts, notably including care homes, 2-3 year olds and over 65s. This will build on the NHS achieving its second highest total of people vaccinated for flu in the 2022/23 season, where 21.2 million people took up the offer of a vaccination as of 31 March 2023.
Children and young people
58. The national inpatient paediatric early warning system (PEWS) was published in November 2023. The standardised chart, committed to in the UEC Recovery Plan, used to spot and manage deterioration in children, will now be implemented in paediatric in-patient settings. Implementation is being closely aligned with the work on Martha’s Rule led by the Patient Safety Commissioner.
59. The national bundle of care for children and young people with epilepsy was published in October 2023. This sets out the key standards around the care and delivery of epilepsy services and focusses on variation in care, mental health and wellbeing, tertiary care and epilepsy surgery, and transition from paediatric to adult services. Recommendations for ICBs to support the implementation of key standards have also been developed.
60. Work continues to implement the remaining recommendations set out in the UEC Recovery Plan, including the continued expansion of the paediatric NHS111 clinical assessment service, the onboarding of Advanced Clinical Practitioners, and the development of virtual wards for children and young people.
61. The NHS continues to exceeded its previous commitment to treat 1,000 children a year for severe complications related to their obesity by the end of March 2023. Latest figures show that over 2,500 patients began treatment since the first clinic was launched. Work continues to further expand the number of clinics and their reach during the remainder of 2023/24.
Genomics
62. The NHS continues to provide the NHS Genomic Medicine Service (NHS GMS) through a consolidated laboratory network made up of seven NHS Genomic Laboratory Hubs. There are seven NHS GMS Alliances working together to support clinical leadership and embedding of genomic medicine in end-to-end pathways; and clinical genomic services that diagnose and manage complex rare and inherited disease.
63. Throughout October and November, we have continued to see an increase in access to genomic services. In line with the NHS Long Term Plan, there has been a growth in the number of patients accessing the whole genome sequencing service, in addition to the rapid whole genome sequencing service launched in October 2022 for acutely unwell babies and children. There has also been an increase in the number of extensive genomic tests offered to patients diagnosed with cancer.
64. NHS England are continuing to support the Generation Study, which is delivered by Genomics England and supported by the NHS GMS. Colleagues from Genomics England and NHS England have been working with clinicians to discuss the genes or conditions to be included in the programme and map downstream care pathways. The initial list of genes and conditions was published in October 2023 to enable public consultation on inclusion into the research study.
65. October also saw the establishment of the 8 approved NHS Genomic Networks of Excellence, which will start to deliver work packages by early 2024. The NHS Genomic Networks of Excellence, announced in the NHS Genomics strategy, will play a key role in bringing together the NHS GMS, National Institute for Health and Care Research, Biomedical Research Centres, Academic Health Science Networks and other partners across industry and academia to accelerate genomic research. This will support the generation of evidence and models of adoption for new technology and testing, and clinical and laboratory practice, for example rapid whole genome sequencing, in defined areas of strategic importance.
Recovery Support Programme
66. The Recovery Support Programme (RSP), provides national mandated intensive support to trusts and ICBs in NHS Oversight Framework segment 4 and who have complex, deep-seated concerns around leadership, governance, finance, patient safety, quality and/or performance.
67. The Programme now has 19 trusts (six legacy special measures) and 4 ICBs enrolled. Since the last update in October 2023, there have been no new entries and two Trusts and one ICB have met the criteria to exit the RSP as set out below:
- On Tuesday 17 October, it was agreed by the Quality Performance Committee (QPC) that the University Hospitals of Morecambe Bay NHS Foundation Trust (UHMBT) has successfully met its exit criteria and should transition into segment 3 of the NHS Oversight Framework.
- On Tuesday 14 November, it was agreed by the QPC that the Liverpool University Hospitals NHS Foundation Trust (LUFT) and Lincolnshire ICB have both successfully met their exit criteria and should transition into segment 3 of the NHS Oversight Framework, which will be arranged in the coming weeks.

