Organisation objective
- Statutory item
Executive summary
Pressure has continued in emergency departments across the country, with 2.1 million attendances and 524,000 emergency admissions in August 2023. Ambulance services also faced an extremely busy month but response times for both category one and category two incidents improved on July 2023.
Continuing industrial action in the NHS has had a significant impact on patients, with almost 400,000 appointments having to be rescheduled during June, July and August 2023 as a result of strikes by junior doctors, consultants, dentists and radiographers.
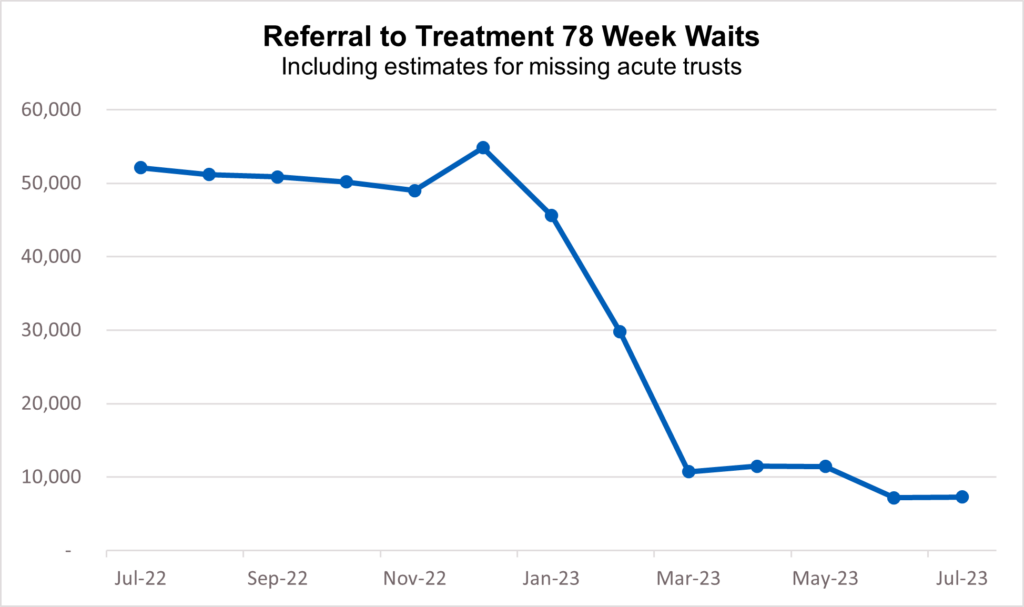
Despite disruption caused by strikes, NHS staff are working hard to reduce the longest waits for care. In August 2023, there were 7,289 waiting more than 78 weeks, down by almost 85% from a peak of 124,911 in September 2021.
The NHS continues to increase support to those outside of hospital. Urgent Community Response helps avoid hospital admissions by providing urgent care to people in their homes. ICBs now have full coverage and the latest data shows that nationally 84% of patients were seen within the 2-hour standard, with every region exceeding or meeting the 70% target in the Planning Guidance.
In diagnostics, the NHS has increased community access and overall activity levels, and in July, more than 2.2 million tests and checks were carried out. Over the past 12 months (August 2022 – July 2023) more than 25.3 million checks and scans have been carried out.
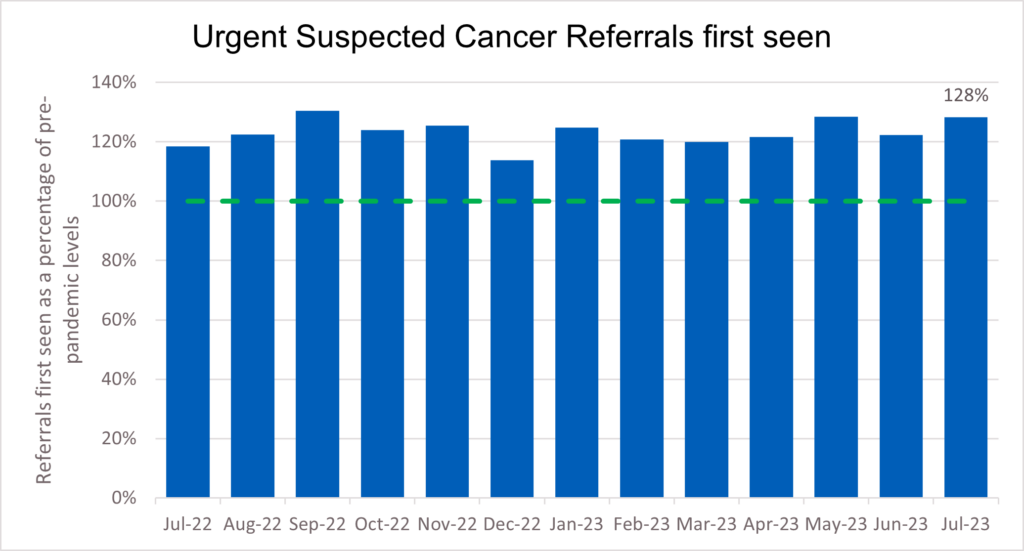
Demand for cancer services continued at record levels in July 2023, with the number of urgent suspected cancer referrals at 130% of pre-pandemic levels. Treatment is also at record levels and cancer deaths are around 10% lower in the UK compared to just 5 years ago.
Good progress continues to be made in activity levels in general practice. In July 2023, 27.8 million GP appointments took place. 43.6% of appointments in June took place on the same day that they were booked, and 68.3% were carried out face to face.
The NHS continues to expand mental health services to meet rising demand. More people than ever before now receive NHS support for their mental health, with five million patients accessing care in 2022/23, an increase of over one million in five years.
Urgent and emergency care
1. Pressure on urgent and emergency care (UEC) services continued in August.
2. There were 2,106,146 attendances in A&Es across England, an average of 67,940 per day. This means there were a total of 6,522,000 attendances in June, July and August making it the busiest summer ever (the previous high was 6,498,472 in 2019. Summer: June, July and August)..
3. Despite this demand and further periods of industrial action, NHS staff managed to maintain progress against the ambitions set out in the UEC Recovery Plan.
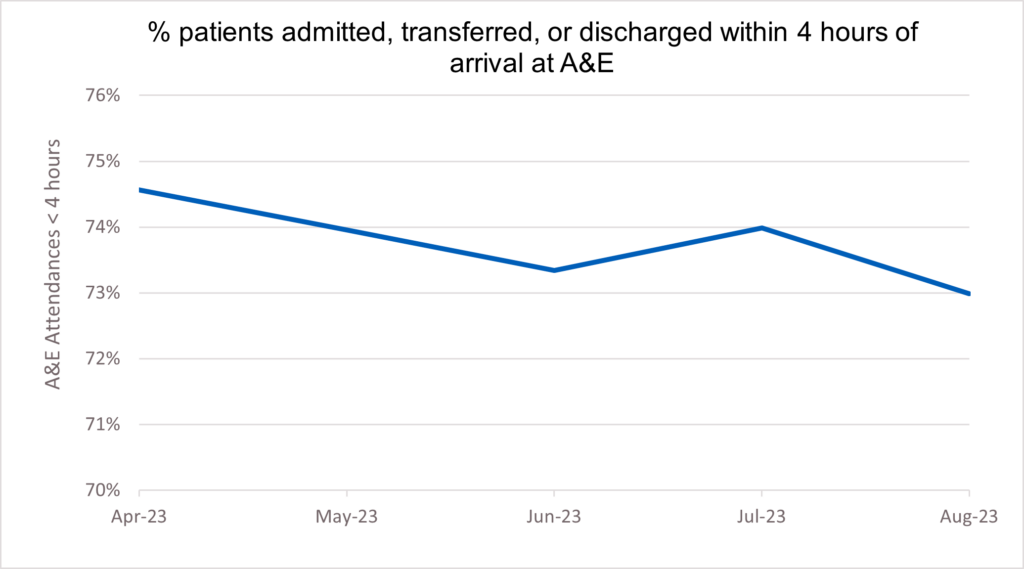
4. 73% of patients attending A&E were admitted, transferred or discharged within hours. This compares to 71.7% in August 2022.
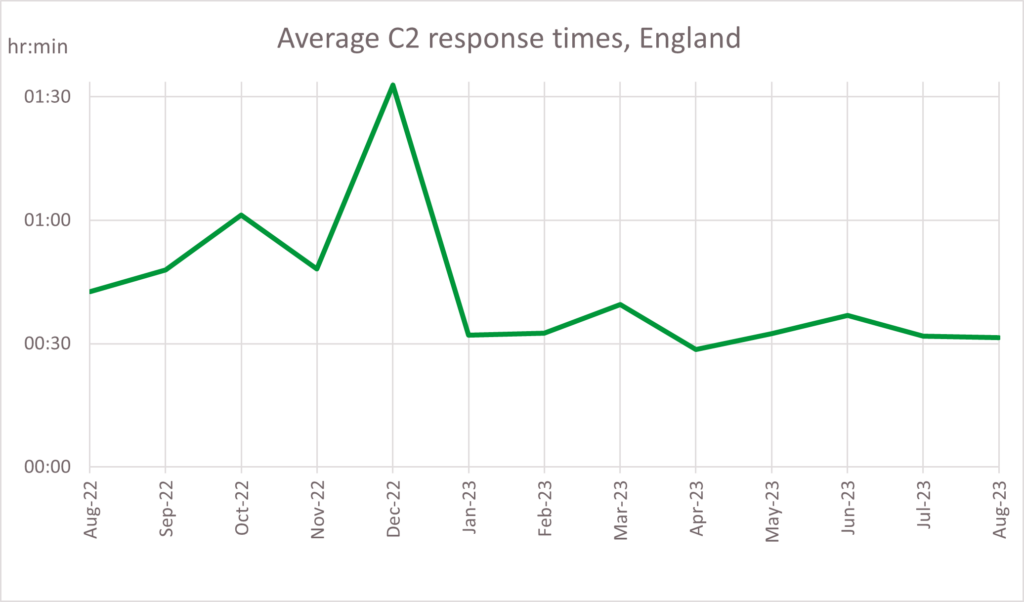
5. The average ambulance response time for a category two call was 31 minutes and 30 seconds – a faster response time of 11 minutes and 7 seconds compared to August 2022 (in August 2022, the average ambulance response time for a category two call was 42 minutes and 37 seconds) . Ambulance services answered 770,251 999 calls, 24,847 per day, and responded to 706,639 incidents.
6. An essential aim in the UEC recovery plan is to deliver an increase of 5,000 staffed and sustainable (core) beds.
7. New data published this month shows there were 98,959 general and acute beds open in August. 97.8% of these were core beds and 2.2% were escalation beds – beds that the NHS temporarily opens to cope with immediate or growing operational pressure.
8. Increasing the number of core beds is one of the ways the NHS is preparing for winter, with more than 99,000 core beds expected to be in place across the country by December 2023.
9. We are also focussed on improving in-hospital flow by reducing length of stay and bringing forward discharge processes. In August, the average number of patients who were in a hospital bed for 14 or more days decreased by over 13% since January (in January 2023, the average number of patients in a bed for 14 or more days was 50,355. In August 2023 it was 44,980 patients on average per day).
Elective recovery
10. Continuing industrial action had a significant impact on planned care in July. However, despite nine days of strikes, staffing pressures and increased demand (there were 129,833 more new RTT periods in July 2023 compared to July 2022), the NHS continued to hold delivery on reducing the longest waits for elective care.
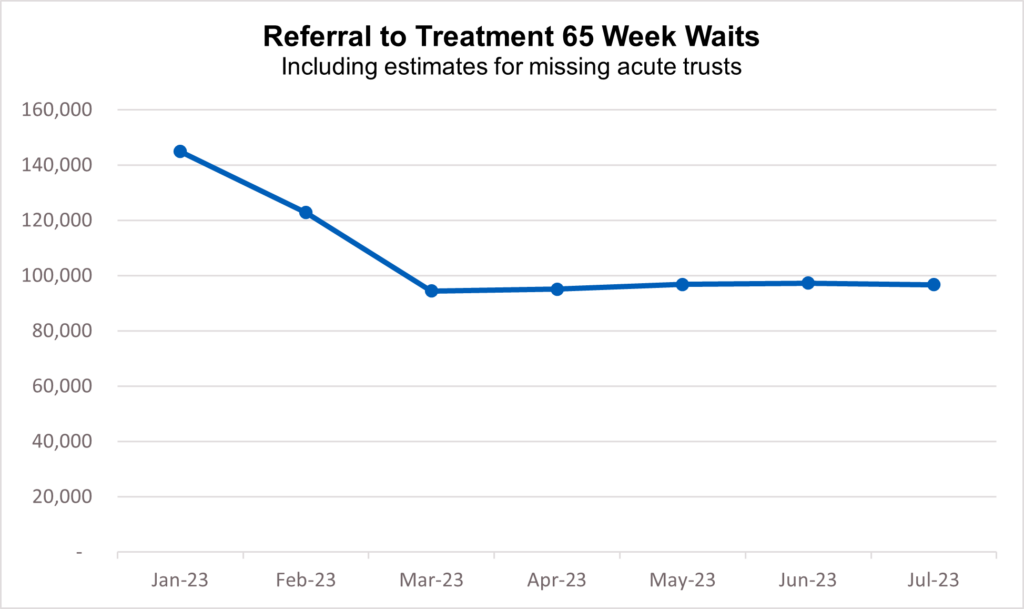
11. As of the end of July, 96,722 (1.3%) patients were waiting more than 65 weeks for treatment. This is down by 41.8% since the start of the year (166,201 patients were waiting more than 65 weeks at the end of 2022).
12. 7,289 patients were waiting more than 78 weeks for treatment. This is a reduction of 44,859 (86%) since July 2022.
13. Fewer than 280 patients were waiting more than 104 weeks for treatment. This has reduced by 77% since the start of the year (1,222 patients were waiting more than 104 weeks for treatment at the end of 2022) .
14. The NHS also carried out 2,214,141 tests and checks in July, up 7% on the same month pre-pandemic (2,064,497 diagnostic tests were carried out in July 2019). The average waiting time for diagnostic tests and procedures was 3.1 weeks.
15. Additional diagnostic capacity has been created through 111 Community Diagnostic Centres (CDCs) which have already provided millions of diagnostic tests, checks and scans.
16. CDCs are an essential focus of the elective recovery delivery plan. The aim is open 160 centres by March 2025, so patients get tested faster and more conveniently.
Cancer
17. Demand for cancer services continued at record levels in July 2023, with the number of urgent suspected cancer referrals at 130% of pre-pandemic levels. To meet high demand, treatment is also at record levels.
18. Over 335,000 people received treatment for cancer over the last year between August 2022 and July 2023 – the highest year on record, and up by more than 22,000 on the same period pre-pandemic.
19. GPs have been referring people for urgent cancer checks in record numbers since March 2021. Since then, NHS staff have seen over 970,000 more people than in the same period prior to the pandemic.
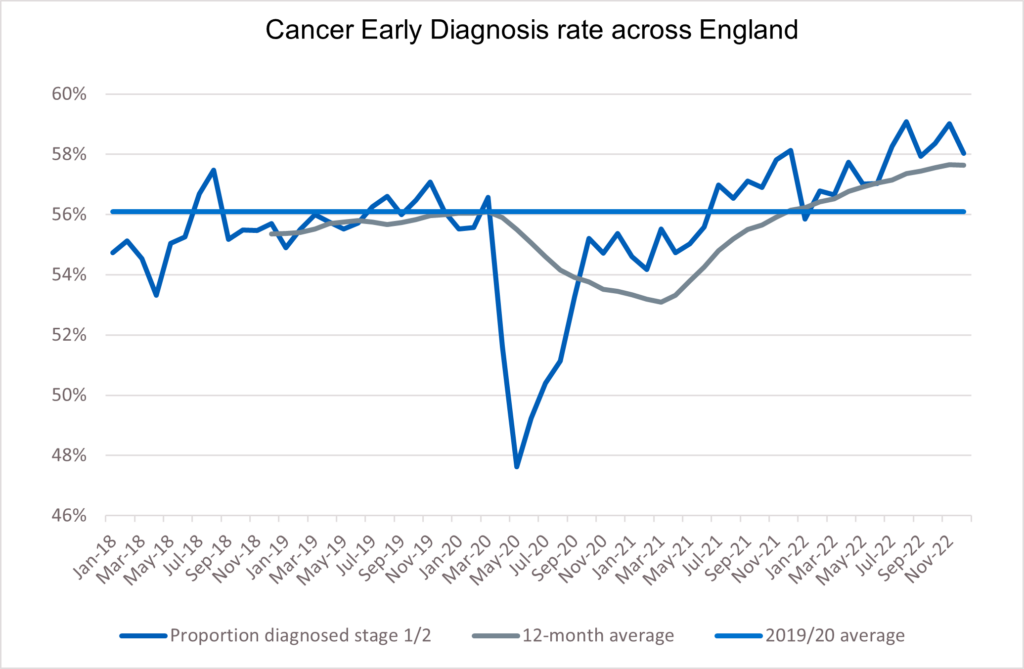
20. The increase in referrals has contributed to the NHS diagnosing more cancer at an early stage than ever before. We are diagnosing a higher proportion of cancers at an early stage now than ever before – about 2% higher than before the pandemic. Survival is also at an all-time high.
21. In 2023, the Annals of Oncology published findings showing that cancer deaths are around 10% lower in the UK compared to just 5 years ago.
22. The NHS is working hard to keep up with this increase in demand. It has been accelerating the installation of new diagnostic capacity, much of it in Community Diagnostic Centres.
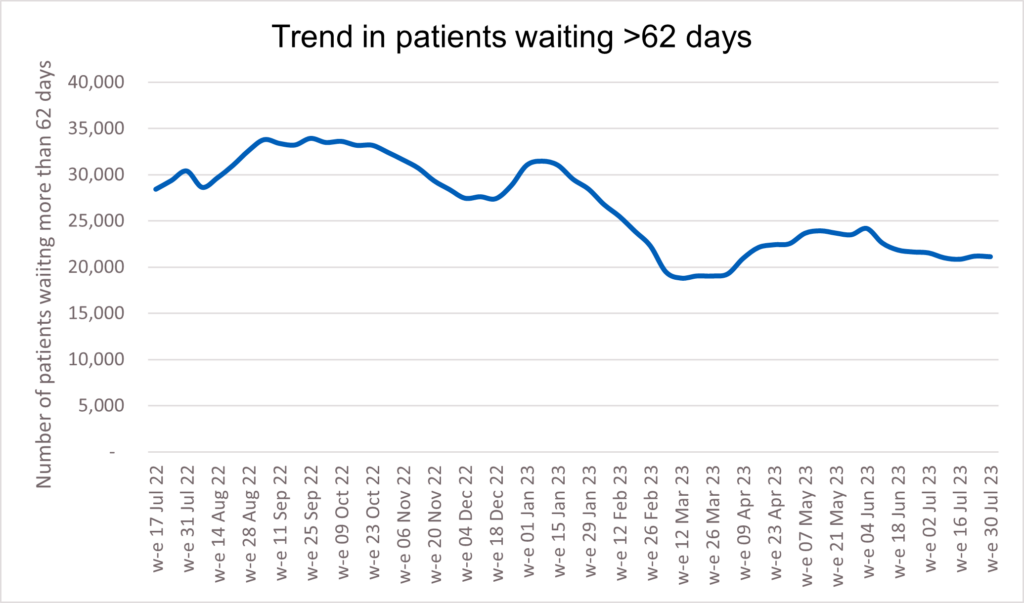
23. The backlog has already reduced by 14,000 people since its peak last summer, and despite the recent seasonal increase, NHS staff remain focused on ensuring that people who have been waiting longest or who need care most urgently are seen first.
Mental health
24. More people than ever before now receive NHS support for their mental health, with five million patients accessing care in 2022/23, an increase of more than one million in five years.
25. Services across the country have made great efforts to improve access and reduce waiting times against a backdrop of increased needs and complex conditions. This is particularly the case for children and young people, with one in six now facing a potential mental health problem compared to one in nine in 2017.
26. The pandemic and its aftermath have exacerbated the factors that contribute to poor mental health and demand for mental health care is at an all-time high, with bed occupancy still above 95% across NHS mental health hospitals.
27. The NHS is working hard to reduce this treatment gap and expand its mental health offer, supported by an extra £2.3bn a year. This includes expanding and transforming community services for adults and older adults with severe mental illness (SMI) such as eating disorders, schizophrenia or bipolar disorder, with the aim of offering patients access to personalised and holistic care as close to home as possible.
In June 2023, over half a million people with SMI (547,156 in total) had received an assessment and started treatment in community mental health services in the previous 12 months.
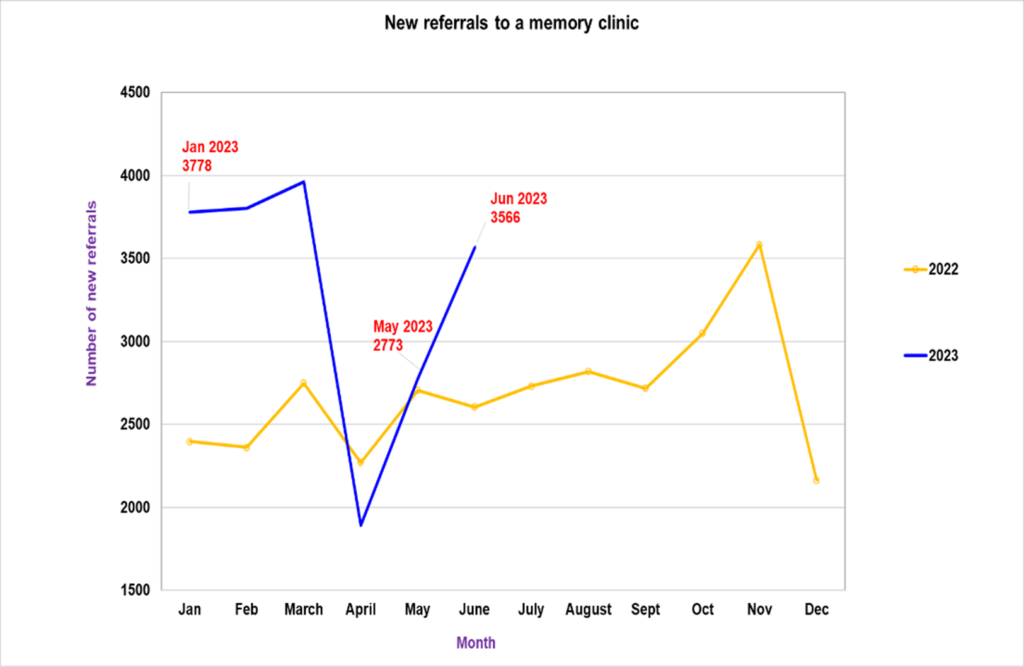
28. Improving dementia care is also a key focus of the NHS. Assessment and diagnosis begin in a memory clinic where people with symptoms and their carers can access a multi-disciplinary team for advice, information, and support.
29. In June 2023 there was a 28% increase in new referrals to memory clinics (3,566 people referred in total) as services work around the clock to clear pandemic backlogs.
30. With potential new treatments for Alzheimer’s disease on the horizon, we are stepping up and accelerating preparation for potential rollout. This includes establishing a dedicated programme team for early Alzheimer’s treatments working across the NHS in collaboration with industry partners and patient groups.
Annex: Operational performance update
Executive summary
This annex provides a more comprehensive summary of operational performance based on published data and work to restore services.
Elective Care
31. The NHS has made further progress in reducing the number of people waiting the longest for care, despite industrial action. Waits of more than 65 weeks reduced to 96,722 in July which is down 59% on the peak of 233,051 in June 2021, and down from 149,770 in July last year.
32. The latest figures also show an improvement in average waits for elective care, with the median wait for admitted treatment at 11.3 weeks in July 2023, the lowest it has been since December 2022, and the median wait for non-admitted elective care down to 8.2 weeks in July 2023.
33. As at the end of July 2023, around 1.2% (96,722) of patients had been waiting more than 65 weeks and 5.1% (389,952) over 52 weeks.
34. The majority of patients on the waiting list are outpatients, and we wrote to providers on 4th August 2023 to ask them to assure their organisation’s approach to outpatients’ productivity and transformation. The letter focused on increasing the pace in transforming outpatient services to release capacity for patients awaiting their first contact and diagnosis. It set organisations an ambition that no patient in the 65-week ‘cohort’ (patients who, if not treated by 31 March 2024, will have breached 65 weeks) is waiting for a first outpatient appointment after 31 October 2023. We also asked for a board self-certification process to be undertaken by 30th September 2023. We will work with regions and providers to monitor and support this process.
35. The GIRFT team is also working with 25 trusts to bring together clinicians and operational teams to meet the challenge of how we can collectively go ‘further and faster’ to transform our pathways. Nine specialty handbooks have been created to date to bring together clinical best practice on transformation across topics such as reducing and managing missed appointments (DNAs), remote appointments and patient initiated follow up (PIFU).
36. GIRFT have published the Closing the Gap guidance – high impact actions and supporting case studies and resources to help with recovering Children’s elective surgery.
37. As at the end of July 2023, the overall waiting list was 7.68 million.
UEC (including Discharge)
38. The UEC Recovery Plan was published in January 2023 with two clear ambitions: The first, for ambulances to get to patients quicker: with the ambition to improve ambulance response times for Category 2 incidents to 30 minutes on average over 2023/24, with further improvement in 2024/25 towards pre-pandemic levels. The second, for patients to be seen more quickly in emergency departments: with the ambition to improve to 76% of patients being admitted, transferred or discharged within four hours by March 2024, with further improvement in 2024/25.
39. The pressures on the iUEC pathway remain high and services continue to work hard to respond to these challenges and to mitigate the impacts of industrial action. Despite this, the national position against the two main targets remains ahead of the same period last year.
40. This has been the busiest summer on record for emergency departments, with overall attendances for June, July and August at 6,522,000, a 2.4% increase from summer 2022. The summer also saw the second highest recorded number of emergency admissions at 1,582,864, a 6.8% increase from summer 2022. Despite this, flow through emergency departments remains better than last year, with 73% of patients being admitted, transferred, or discharged within four hours in August 2023 compared to under 72% in August 2022.
41. Ambulance response times for the most critical patients have improved, despite an increase in the number of ambulance incidents per day. In August, responses to category 2 incidents were on average 31 minutes and 30 seconds, a reduction of over 11 minutes compared to the same month last year. The total number of incidents in August 2023 was 22,795 per day on average, up 5.3% from last August.
42. We are also focussed on improving in-hospital flow by reducing length of stay and bringing forward discharge processes. In August, the average number of patients who were in a hospital bed for 14 or more days decreased by over 13% since January. Development of a new metric that better measures discharge delays is ongoing.
43. A key aim in the UEC recovery plan is to increase capacity, including an increase of 5,000 staffed and sustainable (core) beds, so that more than 99,000 core beds are open across the country over winter. There were 98,959 general and acute beds open in August, an increase from last year, 97.8% of which were core beds. Additionally, between January and September this year, 145 new virtual wards have been mobilised, with 9,885 virtual ward ‘beds’ available in August. This is very close to the 10,000 ambition for September, although we continue to work with local providers to increase occupancy. Key programme guidance has been updated and new guidance published including on procurement of technology and in vitro point of care diagnostics. Upcoming guidance will support new pathways including heart failure and children and young people.
44. Modules for our universal improvement offer, including Same Day Emergency Care (SDEC), care transfer hubs and intermediate care planning, will be rolled out over autumn 2023. Our intermediate care rehabilitation and reablement framework was published in September 2023, to help ensure high quality step-down care. Building on the work of discharge frontrunners this best practice guidance focusses on a number of recommended actions that systems should consider in partnership with their intermediate care services.
Diagnostics
45. 2.21 million of the 15 key diagnostic tests were performed in July 2023, 12% more than in July 2022. The percentage of patients waiting less than six weeks for a diagnostic test decreased slightly, from 74.8% in June 2023 to 74.5% in July.
46. The 115 permanent and three temporary operational CDC sites have delivered 5.14m tests since the first CDC was launched (as at 03/09/23) and 1.48m tests in-year – 8% ahead of activity plan in 23/24 to date.
Cancer
47. As at w/e 30 July 2023 there were 21,118 patients waiting longer than 62 days following an urgent suspected cancer referral, for either exclusion of cancer or for cancer treatment to start. This represents an expected seasonal increase in comparison to the April 2023 position but remains 9,256 lower than the same point last year.
48. Performance against the 75% Faster Diagnosis standard improved to 74.1% in July 2023, up from 73.5% in June 2023, and 71.3% in May 2023. This demonstrates that progress continues to be made against the ambitions set for 2023/24, despite ongoing capacity reductions related to Industrial Action.
49. We saw performance against the 62-day urgent suspected cancer referral to first treatment standard increase to 62.6% in July 2023, up from 59.2% in June 2023. Performance was 0.6 percentage points higher than in July 2022, which is the first year-on-year increase in performance seen since March 2018, other than where this was driven by the drop in referrals seen at the start of the pandemic.
50. The level of demand for cancer services remained high in July 2023, with the number of urgent suspected cancer referrals at 128% of pre-pandemic levels. The NHS has increased the levels of first treatments provided in response which are higher than the same point last year and 7% above pre-pandemic levels.
51. Notable progress is being made against transformation initiatives, with 2,396 lung cancers diagnosed through the Targeted Lung Health Checks programme to date, 74.7% of these at stage one or two, and a total of 1,052,083 invites sent out. The national referral trajectory for Non-Specific Symptom pathways is currently being exceeded, with referrals reaching over 5,000 a month for the first time, reflecting 96% population coverage, and over 100,000 patients being seen to date.
52. Our BRCA programme, which offers genetic testing of those at risk of carrying the mutation, has sent out 3,735 saliva packs so far of which 2,336 have been returned. 1,108 results have been communicated to patients and 24 BRCA carriers have been identified. The Community Liver Health Checks pilot has delivered 20,286 fibroscans and 2,197 people have been identified at risk of liver cancer, with 1,663 people referred into liver surveillance.
53. The NHS continues to run a rolling programme of campaigns and partnerships that raise awareness of a range of cancer symptoms and encourage people to come forward. These campaigns aim to reach people from more deprived communities, in whom we see higher cancer incidence, as well as those more likely to experience health inequalities, such as Black and South Asian people. In August we launched a partnership with Morrisons to include cancer messaging on their own-brand underwear products, and a campaign to tackle the fear-related barriers to timely help-seeking was launched in September. This will be supplemented by a campaign on persistent coughs to support diagnosis of lung cancer.
Primary Care and Community Health Services
54. The Primary Care Access Recovery Plan (PCARP) was launched in May 2023. Supported by investment, the plan responds to feedback and outlines measures that will make a difference now to patients and staff, supporting primary care teams to improve and recover access in general practice. A programme of work is in place focusing on the following four areas:
- Empowering patients to manage their own health including using the NHS App, self-referral pathways and through more services offered from community pharmacy.
- Implementing Modern General Practice Access to tackle the 8am rush, provide rapid assessment and response, and avoid asking patients to ring back another day to book an appointment.
- Build capacity to deliver more appointments from more staff than ever before and add flexibility to the types of staff recruited and how they are deployed.
- Reducing the workload across the interface between primary and secondary care, and the burden of medical evidence requests so practices have more time to meet the clinical needs of their patients.
55. The number of appointments taking place in General Practice continues to increase. In the 12 months leading to July 2023, 352.6 million appointments took place, including 10 million for COVID-19 vaccinations. Adjusting for working days, this is 15.6% higher than the number of appointments carried out in the 12 months to March 2019.
56. On 16 August 2023 NHS England published General Medical Services (GMS), Personal Medical Services (PMS) and Alternative Provider Medical Services (APMS) contract variations alongside updated GMS, PMS and APMS contracts. The contract variations and updated contracts incorporate the 2023/24 GP Contract changes announced by NHS England in March 2023.
57. Workforce data shows that as of 31 July 2023 there were 35,897 FTE doctors working in general practice in England. This is an additional 4% compared to the baseline of 31 March 2019 and reflects the continued increase in GP training places, although the number of fully qualified GPs has reduced by 4.6% over the same period. The NHS Long Term Workforce Plan sets out plans for a further 50% increase to GP training places to build the future workforce.
58. The primary care workforce continued to expand with, as of 30 June 2023, 31,370 additional direct patient care staff recruited into general practice. This led to the March 2024 target of an additional 26,000 direct patient care staff being recruited being achieved a year early. More than 4,000 care navigators registered for training.
59. In August 2023, 92% of contracted dental activity was delivered across England compared to 85% in July showing a steady increase month on month (80% in June, 77% in May and 56% in April).
60. The Community Pharmacy Independent Prescribing Pathfinder Programme was launched in August with a letter going to ICB Chief Executives asking them to establish pharmacy sites. The programme is expected to run up to 12 months in the first instance depending on the outcome of evaluation. Findings and recommendations were published from the TARGET “treating your infection” leaflet which formed part of the Pharmacy Quality Scheme (PQS) in 2022/23, to improve community pharmacy integration with multi-disciplinary teams and support consistent messages on appropriate use of antibiotics. Further information is available here.
61. Urgent community response (UCR) services provide assessment, treatment and support for adults who are experiencing a health or social care crisis which puts them at risk of hospital admission in the next 24 hours. UCR is available in every ICB, and is delivered 8am-8pm, 7 days a week at a minimum. Our latest data from May 2023 shows that over 39,000 referrals were responded to by UCR services, which is more than double the activity recorded in May 2023. All UCR services aim to achieve a national threshold of 70% of activity being seen within two hours of referral. This target was achieved ahead of the December 2022 deadline, with data from May showing 84% of people being seen within two hours of referral.
62. Against an LTP commitment of 900,000 people being referred to a social prescribing service, there are currently 3,475 social prescribing link workers employed by a PCN/GP practice. Since April 2019, they have seen approx. 2.3 million patients. Currently 92% of PCNs have access to a social prescribing link worker, which means more patients than ever now have access to this service. We are also on track to meet the LTP commitment of 200,000 people having received a personal health budget by 23/34, which includes some one-off personal health budgets that facilitate hospital discharge. Overall, 7.8 million individuals have now benefitted from a personalised care intervention.
Mental Health
63. The LTP, building on the Five Year Forward View, set out a 10-year plan to address a significant treatment gap in mental health services, with deliverables and ringfenced funding up to 2023/24. Progress has been strong, in the context of service disruption due to the pandemic, and the consequent increase in prevalence and acuity. The NHS continues to expand and transform mental health services at pace, meeting several commitments including:
- 6-week and 18-week standards for referral to treatment and the 50% recovery rate for NHS Talking Therapies;
- the Early Intervention in Psychosis waiting time standard of 60%;
- creation of Mental Health Support Teams (MHSTs) in schools with accelerated delivery – while no MHSTs existed in 2016, they now provide prevention and early intervention for 35% of pupils and learners in schools and colleges in England;
- roll-out of 24/7 crisis lines ahead of schedule to provide a much needed service to patients experiencing a crisis, with lines receiving c. 200,000 calls a month.
64. A winter planning letter was issued to ICBs and providers in July 2023, setting out the key steps needed across all parts of the system to meet anticipated challenges. Mental health will be a key part of winter planning efforts; particularly as the Urgent and Emergency Care Adult Mental Health pathway continues to experience high bed occupancy at 95.9% as of 12th September 2023, and length of stay continued to rise to an average of 49.5 days nationally by July 2023. Flow challenges are having an impact on services’ ability to provide care to patients close to their home and families, with Out of Area Placements increasing from 415 to 435 between March and April 2023.
65. As of May 2023, 697,305 Children and Young People (CYP) (0-17s) accessed support against a target of 768,609. Performance has decreased when compared to the previous month (701,839 in April 2023). CYP Eating Disorders pathways continue to be pressured, with 61.6% of urgent cases starting treatment within one week and 67.1% of routine cases starting treatment within four weeks as at May 2023.
66. In Q4 2022/23, NHS Talking Therapies services delivered access for 320,254 people, a similar level to the previous quarter. 50,979 women accessed a specialist community perinatal mental health service or a maternal mental health service in the 12 months to May 2023; access is increasing however performance remains behind trajectory. Across all challenged areas, we are working closely with teams to determine how best to mitigate key risks, address delivery challenges and offer support.
67. Work continues to reduce health inequalities in mental health services. The Patient and Carers Race Equality Framework, which was co-produced and is the first framework of its kind, will support trusts to address inequalities and improve access, experience, and outcomes for people from ethnic minorities and marginalised communities. The final version is expected to be published in the coming months. Physical health checks for people with Severe Mental Illness support tackling health inequalities and premature mortality. In the 12 months to June 2023 the NHS provided a physical health check to 273,858 people with severe mental illness.
68. Significant progress has been made in expanding workforce as part of the LTP; by March 2023 the mental health workforce had increased by 33,600 since March 2016 (equivalent to 31% growth compared to 25% growth in rest of the NHS). Workforce expansion remains a priority, as does addressing significantly high vacancy rates, particularly in mental health nursing. NHS England continue to work with regions and systems to identify and implement high impact initiatives to improve retention and to increase supply.
69. In response to the central government drive to increase policing productivity, NHS England worked with the Home Office, DHSC, and the National Police Chiefs’ Council to develop a National Partnership Agreement (NPA) committing to reduce the inappropriate involvement of police in mental health-related incidents. The NPA was published on 26th July 2023 and NHS England are developing supporting health-facing guidance, to be published in Q3 2023/24.
Learning Disabilities and Autism
70. The NHS Long Term Plan (LTP) set an ambition that by 2023/24, at least 75% of people aged 14 and over on the GP learning disability register will receive an Annual Health Check (AHC). This target was achieved by the end of 2022/23; a year earlier than planned. AHC performance continues to be a priority for GPs practices and performance in Q1 2023/24 is on a par with performance in the same quarter last year.
71. There is a focus on maintaining support to GP practices and Primary Care Networks. The main emphasis of this work will be on increasing the number of people on a GP learning disability register (GPLDR), improving access to the GPLDR and improving access to and the quality of health action plans.
72. AHCs are particularly important as we start the Autumn/Winter 2023 COVID and Flu Vaccination Campaign, as evidence indicates that people with a learning disability are disproportionately adversely impacted by COVID. The National Clinical Director is leading work with regional colleagues looking at people who do not have a formal diagnosis of learning disability but could be included within GPLDR and receive an AHC, thus improving their health and reducing their health inequalities.
73. The number of people with a learning disability and autistic people in a mental health inpatient setting has reduced by 30%, since March 2015. As at July 2023, there were 1,845 adults and 200 under 18s in a mental health inpatient setting. However, there has been a significant increase in the number of autistic people (with no learning disability) in a mental health hospital. Our focus remains on supporting local areas to develop community services as alternatives to mental health inpatient care; to deliver Care (Education) and Treatment Reviews and Dynamic Support Registers to prevent hospital admission and on delivery of keyworkers for children and young people at risk of admission or in a mental health hospital.
74. In June 2023 there were 143,119 patients with a currently open referral for autism – a 27% increase in children and young people and a 42% increase in adults – equating to an overall 46% increase compared to June 2022. As at June 2023 there were 118,223 patients with a currently open referral for ‘suspected autism’ that has been open for at least 13 weeks, this is a 49% increase compared to the June 2022 position.
75. Work continues to support the delivery of Oliver McGowan Mandatory Training on Learning Disability and Autism for the health and social care workforce. Since November 2022, there have been over 2.5 million launches of the e-learning components of training for people who require general awareness (Tier 1) or people who may need to provide care and support (Tier 2). For the same period, there have been over 700,000 e-learning courses completed. Follow up sessions, led by autistic trainers and trainers with a learning disability are also underway. These sessions are being delivered by ICBs with support from NHS England.
76. A new Care (Education) Treatment Reviews and Dynamic Support Registers policy was implemented from May 2023. This offers support to systems with implementation across external stakeholder groups, including promoting the importance of these reviews and registers and their role in supporting a focus on reducing in lengths of stay, reviewing out of area placements and supporting timely discharge.
Prevention and Long Term Conditions
77. Recently published QOF data indicates that in 2022/23 6.2 million patients with hypertension were managed to NICE targets. This is 175,000 more than in 2019/20. 68.6% of patients with hypertension were treated to NICE targets in 2022/23, an increase of 8.2 percentage points compared with 2021/22 and is close to the pre-pandemic baseline of 70%. The NHS Priorities and Operational Planning Guidance has set a target of 77% in 2023/24. The CVDPREVENT audit has published a new regional and insights dashboard which allows anyone to view data from national to practice level, including peer comparisons and detailed breakdowns by health inequalities markers.
78. The latest phase of NHS England’s ‘Help Us, Help You’ campaign has launched with a focus on heart attack. The aim of this phase is to raise awareness of the symptoms of a heart attack and encourage anyone experiencing one to call 999. The campaign runs from 14 August to 1 October 2023. A revised framework has been published to support clinicians and commissioners to improve the design and provision of palliative and end of life care services for heart failure patients.
79. Thrombectomy and thrombolysis activity continues to track towards trajectory, with increased adherence to the National Optimal Stroke Imaging Pathway (with 90% of units introducing AI decision support), video triage for rapid diagnosis, publication of a GMC thrombectomy credential, funding for additional equipment and QI initiatives to increase thrombolysis rates. Implementation of the National Integrated Community Stroke Service (ICSS) model is being directed by the Stroke Quality Improvement in Rehabilitation (Squire) programme with 61.8% of patients transferred from hospital to home-based stroke rehabilitation to drive recovery.
80. Latest published QOF data for 23/24 shows the number of people offered a referral to pulmonary rehabilitation, an exercise and education programme for people with moderate to severe breathlessness, has returned to pre-pandemic levels; a 6.2% increase from 21/22.
81. Over 1.3 million referrals have been made into the NHS Diabetes Prevention Programme to date. A recent independent evaluation looking at programme completers found that they reduce their risk of developing type-2 diabetes by 37%, and the programme in general resulted in a 7% reduction in population-level incidence in areas where the programme was delivered between 2016 – 2018. When looking at people referred to the programme, the latest independent research published in February 2023 demonstrated a 20% reduction in incidence in those at risk of type 2 diabetes that are referred into the programme compared to those not referred.
82. The NHS Type 2 Diabetes Path to Remission Programme is currently available in 70% of the country (30 ICSs) and will expand to full national coverage by the end of 2023/24. To date almost 12,500 referrals have been made. Early data indicates participants each lose 7.2kg (over one stone) on average after one month, and 13.4kg (over two stone) after three months. This is in line with the outcomes seen in the trials where participants were able to improve their diabetes control, reduce diabetes-related medication and, in around 50% of cases put their type 2 diabetes into remission.
83. The 2023/24 operational planning guidance highlights improvement in hypertension and lipid management as key targets for improvement. Two new QOF indicators for cholesterol have been introduced in 2023/24. In December 2022 58.6% of people with a high-risk score were being treated with lipid lowering therapy, this is a 3.1 percentage point increase since September 2021. The number of patients submitting their home BP readings as part of the BP@Home programme (1.6 million people in 12 months to Jan 2023) and having checks in community pharmacy (over 750,000 people in 12 months to Dec 2022) continue to increase month on month.
84. In December 2022, the England Heart Failure (HF) readmissions average was 20.3%, an improvement on the 2021/22 baseline of 21.2%. Reducing admissions is a focus of the cardiac programme in collaboration with projects including HF virtual wards and Managing HF@ home which have demonstrated reductions in readmissions and mortality. All 15 cardiac networks have submitted plans to reduce 30-day non elective readmissions, improve community diagnosis and management of people with heart failure and to improve access to cardiac rehabilitation.
85. Thrombectomy and thrombolysis activity continue to improve. Identifying patients to benefit from this treatment requires access to immediate brain scans, and the National Optimal Stroke Imaging Pathway incorporates the use of Artificial Intelligence (AI) to support rapid decision making – 88% of England’s stroke units now have access to AI (up from 5% in 2019). Stroke rehabilitation is a key part of the stroke care pathway. The national model for an Integrated Community Stroke Service with provision of both Early Supported Discharge and needs-led community stroke rehabilitation has been adopted by 49% of services, with patient access rising to 61% in 2023/24 and a target of 75% in 2027/28.
Screening and vaccinations
86. All NHS screening programmes have removed backlogs caused by the pandemic including breast screening. Funding has been provided to increase the number of advanced breast screening practitioners being trained.
87. The NHS bowel cancer screening programme continues to exceed the 65% uptake target with age extension to 58-year-olds and 56-year-olds rolled out as planned since 2021/22 and the roll out to 54-year olds having commenced as planned from April 2023. A marketing campaign to promote the return of bowel screening FIT kit (home testing) samples was run in February and March 2023 and successfully increased uptake. There will be an additional campaign in London later in 2023.
88. Uptake for the NHS diabetic eye screening programme continues to meet the efficiency standard. Uptake of initial ultrasound screens in the Abdominal Aortic Aneurysm screening programme is exceeding the achievable standard. The three NHS antenatal and three NHS new-born screening programmes continue to achieve continuous coverage levels close to 100%.
89. The Sickle Cell and Thalassaemia programme is participating in a national initiative to improve lifetime care for people suffering from sickle cell and thalassaemia disease.
90. The use of a new vaccine and an increase in eligible cohorts for the Shingles Immunisation Programme is well underway with delivery from September 2023.
91. A change in HPV schedule for adolescent boys and girls primarily administered in schools is underway with delivery from September 2023 which means eligible adolescents will only require one dose of the vaccine to be fully protected.
92. NHS London is offering polio vaccinations to those children who missed the opportunity to be vaccinated previously in response to the detection of polio in the sewage system in the city. MMR vaccine is also being offered to this cohort, with a nationwide MMR catch up campaign being delivered during 23/24 to address the fact that England has lost its measles elimination status.
93. Changes to the targeted neonatal BCG vaccination programme following the introduction of a new neonatal screening programme in 2020 are being monitored closely in order to improve uptake amongst at risk babies.
94. The 2023/24 children’s flu vaccine programme has started and plans for the seasonal flu and COVID-19 vaccination programmes have been accelerated to September in line government guidance. The revised plans include working at speed to prioritise vaccinations for those most at risk including care home residents and people that are housebound ensuring as many eligible people as possible are vaccinated by the end of October. This will build on the NHS achieving its second highest total of people vaccinated for flu in the season just gone, with 21.2 million people taking up the offer of a vaccination and as of 31 March 2023. In addition, more than 17 million COVID-19 jabs were delivered last winter with more than 149 million COVID-19 vaccinations since the programme started.
Children and Young People
95. Having already exceeded the commitment to treat 1,000 children a year for severe complications related to their obesity by the end of 2022/23, latest figures show that over 2,500 patients have begun treatment since the first clinic was launched. Work is now underway to further expand the number of clinics and their reach in 2023/24.
96. Work continues to implement the recommendations set out in the national urgent and emergency care recovery plan, including the roll-out of the inpatient paediatric early warning score (PEWS) chart; the continued expansion of the paediatric NHS111 clinical assessment service, including the onboarding of Advanced Clinical Practitioners; and the development of virtual wards for children and young people, expanding from July 2023 to cover every region of England. Updated national guidance will be published shortly setting out key considerations and principles around developing age-appropriate virtual wards for children and young people, based on learning from existing sites.
97. A national elective recovery campaign took place between June and September 2023 with a focus on children and young people to examine and take action on key clinical and operational challenges to address backlogs in paediatric elective care, with over 1,100 attendees from provider, system and regional teams joining events.
Genomics
98. The NHS continues to provide the NHS Genomic Medicine Service (NHS GMS) through a network made up of seven NHS Genomic Laboratory Hubs. There are seven NHS GMS Alliances working together to support clinical leadership and embedding of genomic medicine in end-to-end pathways; and clinical genomic services that diagnose and manage complex rare and inherited disease.
99. Throughout August we have continued to see an increase in access to genomic services. In line with the NHS Long Term Plan, there has been a growth in the number of patients accessing the whole genome sequencing service, in addition to the rapid whole genome sequencing service launched in October 2022 for acutely unwell babies and children. There has also been an increase in the number of extensive genomic tests offered to patients diagnosed with cancer.
100. September also saw the final in a series of workshops looking to ratify pathways and turnaround times for solid cancers across the NHS Genomic Medicine Service, as well as the approval of 8 business cases from NHS GMS Alliances for forming NHS Genomic Networks of Excellence. The NHS Genomic Networks of Excellence, announced in the NHS Genomics strategy, will play a key role in bringing together the NHS GMS, National Institute for Health and Care Research, Biomedical Research Centres, Academic Health Science Networks and other partners across industry and academia to accelerate genomic research. This will support the generation of evidence and models of adoption for new technology and testing, and clinical and laboratory practice, for example rapid whole genome sequencing, in defined areas of strategic importance.
Recovery Support Programme
101. The Recovery Support Programme (RSP), provides national mandated intensive support to trusts and ICBs in NHS Oversight Framework segment 4 and who have complex, deep-seated concerns around leadership, governance, finance, patient safety, quality or performance.
102. Since the last update in July 2023, one trust, The Hillingdon Hospitals NHS Foundation Trust, has exited from the RSP. The Programme now has 22 trusts (seven legacy special measures) and five ICBs.
103. 26 RSP Review Meetings chaired by Sir Andrew Morris, with National Executives in attendance, have been held between March 2021 and August 2023 to stress test the trusts improvement plans, review progress against their exit criteria, acknowledge improvements made following exit and escalate where there has been national or regional concern about lack of progress. There are a further two meetings planned for the remainder of Q2 23/24, and eleven meetings planned for Q3 23/24.