Version 2, 16 May 2023
Introduction
This document provides a description of the services and details of workforce and training. A summarised illustrative patient journey is provided to understand the oral surgery clinical pathway. Sources of available information that enable local needs assessment and understanding of local current services provision are described.
A minimum clinical standard specification for the procurement of specialist oral surgery services is presented. Outcome measures that assess clinical outcomes, patient safety and patient reported outcomes (experience) are described to enable quality of services to be assessed and reviewed.
Equality and health inequalities
Promoting equality and addressing health inequalities are at the heart of NHS England’s values. Throughout the development of the policies and processes cited in this document, we have:
Given due regard to the need to eliminate discrimination, harassment and victimisation, to advance equality of opportunity and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it; and,
Given regard to the need to reduce inequalities between patients in access to, and outcomes from, healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities.
1. What is oral surgery?
1.1 Description of the speciality
Oral surgery deals with the diagnosis and management of pathology of the mouth and jaws that requires surgical intervention. It involves the treatment of children, adolescents and adults, and the management of dentally anxious and medically complex patients. Oral surgery care is provided by dental specialty oral surgeons (OS) and by medical specialty oral and maxillofacial surgeons (OMF) as the clinical competencies of these two specialties overlap.
1.2 Related specialties
The dental specialties of oral medicine, dental and maxillofacial radiology, oral and maxillofacial pathology, and oral microbiology contribute to the oral surgery patient pathway.
1.3 Description of the workforce and training
Primary care-based general dental practitioners (GDPs) are expected to undertake routine oral surgery care, such as dental extractions, as part of their general dental services contracts. More complex oral surgery care is provided by specialists in oral surgery and by oral surgery and oral and maxillofacial surgery consultants (including academics) who may work in primary care or secondary care settings[1].
Secondary care-based oral surgery consultants would not normally be found in stand-alone units; rather, they would be integrated with OMFS units with the opportunity for skillmix and multi-disciplinary team working. Postgraduate dental trainees working under consultants may also provide oral surgery care. There are currently insufficient specialists and consultants to manage the population oral surgery needs and so general dental practitioners with enhanced clinical skills and competence assured by the Managed Clinical Network (MCN) may also undertake level 2 complexity care as described below. The MCN may find the ‘Career pathways in dentistry professional framework’ published by the College of General Dentistry 2022 helpful in its description of dentists with enhanced skills and competence.
1.4 Description of the complexity levels
Patients present with a range of complexity of care needs as may be described below and as previously set out in the ‘Guide for commissioning oral surgery and oral medicine’ 2015.
It is important to note that the level of complexity may change depending upon one or more of the following factors and does not simply relate to the procedure to be undertaken or the condition to be managed:
- Complex medical modifiers, such as:
- Haematological disease such as haemophilia, von Willebrand’s Disease, and other inherited coagulation defects
- Patients on anticoagulants with unstable INRs which regularly read greater than 4 or in combination with aspirin, those who are heparinised and patients with a history of haemorrhage following tooth extractions.
- Patients on direct oral anticoagulants (DOACs) or antiplatelet medication and with a high risk of bleeding and undergoing procedures with a high risk of increased bleeding
- Poorly controlled angina or history of myocardial infarction less than 6 months prior to the referral
- Poorly controlled diabetes
- Intravenous bisphosphonate administration
- Patients with Addison’s disease requiring steroid cover
- Psychosocial modifiers, such as:
- Patients with severe learning, mental or physical disability
- Alcoholic patients
- Patient anxiety;
- Need for GA, such as:
- Particularly complex surgery
Cases should be triaged between services according to the levels of complexity, Level 1, 2 and 3. Clinicians providing oral surgery care should be competent to manage complications that may arise. Any procedure should be planned as part of a comprehensive treatment plan and consideration should be given to a multi-disciplinary approach where appropriate. The MCN will operate to assure quality of care and patient safety. The framework of complexity levels with respect to oral surgery procedures is presented in table 4.4.1 Competencies of clinicians for each of the three levels of care are described in appendix 1.
Level 1
Procedures/conditions to be performed or managed by a clinician commensurate with a level of competence as defined by the Curriculum for Dental Foundation Training or equivalent. This is the minimum that a commissioner would expect to be delivered in a primary care NHS Mandatory contract. Many dentists with experience have competencies above this.
Level 2
Procedural and/or patient complexity requiring a clinician with enhanced skills and experience who may or may not be on a specialist register. This care may require additional equipment or environment standards but can usually be provided in primary care.
Level 3a
Procedures/conditions to be performed or managed by a clinician recognised as a specialist at the GDC defined criteria and on a specialist list; OR by a consultant.
Level 3b
Complex oral surgery care to be delivered by consultants in oral surgery and oral and maxillofacial surgery who have the necessary competencies which enables them to deliver more complex care, lead MDTs, MCNs and deliver specialist training. Where OMFS consultants are not registered with the General Dental Council (GDC), they will not be eligible for performers’ list. Some OMFS consultants will be included in both the (General Medical Council) GMC and GDC specialist list; others will only be included in GMC specialist register.
Level 1 and 2 procedures are usually performed in primary care settings although some may be performed in a secondary care setting if modifying patient factors or local circumstances require this.
1.4.1 Framework of oral surgery complexity levels and procedures
N.B. Commissioners should look to the MCN for clinical advice and guidance with respect to appropriate delivery of procedures by clinicians. Appropriate remedial action plans need to be in place to enable practitioners to develop skills so they are able to deliver appropriate levels of care.
Level 1 procedures/conditions
- Extraction of erupted tooth/teeth including erupted uncomplicated third molars
- Effective management, including assessment for referral unerupted, impacted, ectopic and supernumerary teeth
- Extraction as appropriate of buried roots (whether fractured during extraction or retained root fragments),
- Understanding and assistance in the investigation, diagnosis and effective management of oral mucosal disease
- Early referral of patients (using 2-week pathway) with possible pre-malignant or malignant lesions
- Management of dental trauma including re-implantation of avulsed tooth/teeth
- Management of haemorrhage following tooth/teeth extraction
- Diagnosis and treatment of localised odontogenic infections and post-operative surgical complications with appropriate therapeutic agents
- Diagnosis and referral patients with major odontogenic infections with the appropriate degree of urgency.
- Recognition of disorders in patients with craniofacial pain including initial management of temporomandibular disorders and identification of those patients who require specialised management.
Level 2 procedures/conditions
- Surgical removal of uncomplicated third molars involving bone removal
- Surgical removal of buried roots and fractured or residual root fragments
- Management and surgical removal of uncomplicated ectopic teeth (including supernumerary teeth)
- Management and surgical exposure of teeth to include bonding of orthodontic bracket or chain Surgical endodontics
- Minor soft tissue surgery to remove apparent non-suspicious lesions with appropriate histopathological assessment and diagnosis.
Level 3 procedures/conditions
- Procedures involving soft/hard tissues where there is an increased risk of complications (such as nerve damage, displacement of fragments into the maxillary antrum and fracture of the mandible)
- Management and/or treatment of salivary gland disease
- Surgical removal of tooth/teeth/root(s) that may involve access into the maxillary antrum
- Management of temporomandibular disorders and craniofacial pain that have not responded to initial therapy
- Treatment of cysts
- Management of suspicious/non-suspicious oral lesions
- The placement of dental implants requiring complicated additional procedures such as bone grafting, sinus lifts etc.
- Treatment of complex dentoalveolar injuries
- Management of spreading infections and incision of abscesses (or abscess) requiring an extra-oral approach to drain
Depending on the complexity of the procedure, consultant-led care may be required to manage any of the above. These procedures will be delivered within a team, which may include specialist trainees, specialists and SAS grades who have appropriate ability and facilities to provide high quality care for patients.
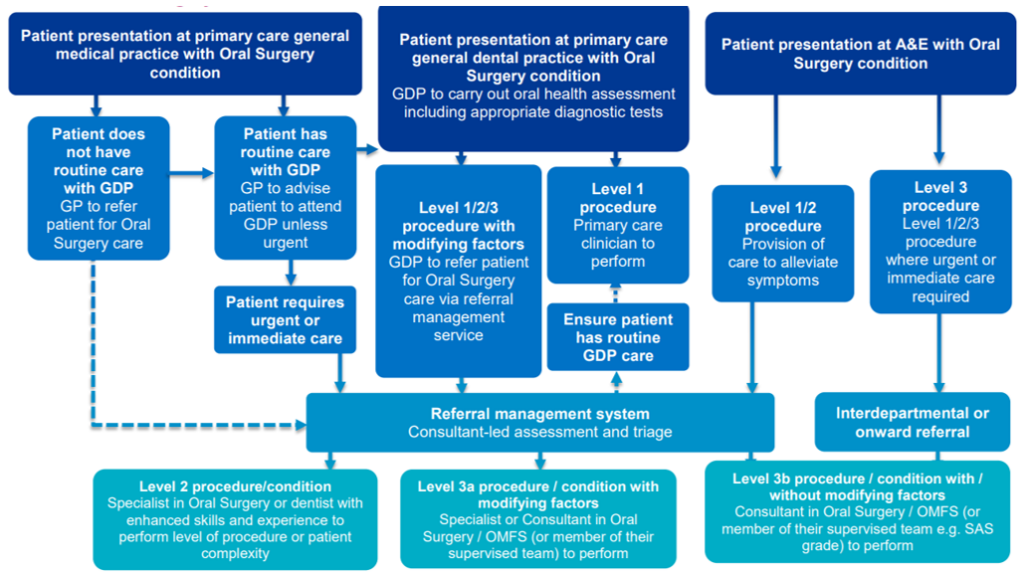
2 Summarised illustrative patient journeys
If an oral cancer is suspected or there is a suspicious head and neck mass (such as a salivary gland mass), the patient should be referred as per (2 week) cancer referral pathway wait criteria to a head and neck oncology service.
2.1 Oral surgery
3. Assessing need
3.1 Local population profile
Information regarding oral health needs assessment for all specialist dental services can be found in the NHS England publication, ‘Guide for commissioning specialist dentistry services’. Commissioners should be familiar with the sources of information available that can assist them in assessing the dental needs of the local population e.g., population number, residency, age, population growth, ethnicity, deprivation, lifestyle and prevalence of oral diseases and conditions. Given the increase in the number of people with co-morbidities, this should also be taken into account.
4. Illustrative journey of a patient (elective oral surgery care)
Primary care dental teams and medical colleagues should understand how to navigate the oral surgery patient pathway and benefit from the use of a referral management system. Appropriate use of PREMS and PROMS and quality indicators would provide data with respect to the quality of service provision, clinical effectiveness and patient experience delivered by providers. These data could be used for benchmarking and annual review of services. Many matrices are described below and Commissioner in collaboration with the MCN may wish to use their agreed priority items.
Level 1 care dentist
Oral surgery procedures should only be undertaken in those situations where they will clearly contribute to the oral health of the patient.
In all situations the clinical advantages and long-term benefits of oral surgery procedures to the patient should justify such treatment and outweigh any detrimental effects.
The clinician should ensure that the cooperation, motivation, aspirations, and general health of the patient are consistent with the provision of oral surgery.
Prior to the provision of oral surgery, a comprehensive oral health assessment should be undertaken; the information collected and the risks identified should be reviewed before oral surgery procedures are undertaken.
The information gathered and reviewed in the oral health assessment should be used to reach a consensus as to whether it is in the patient’s best interests to provide an oral surgery procedure or to make a referral to another clinician.
Level 1 complexity are oral surgery procedures or conditions to be performed or managed by a dentist commensurate with the level of competence as defined by the curriculum for dental foundation training, or its equivalent. The level of complexity may, however, change from level 1 to level 2 or level 3 depending on one or more modifying factors, for example:
- Level of anxiety: medical history social factors:
- Other complications
| Dentist referral | Standards | Metrics |
|---|---|---|
| Dentist makes referral and ensures that the consistent required data set is complete. Dentist ensures all relevant medical history detail is provided. Dentist ensures that all workup and readable radiographs are available as per agreed oral surgery referral guidelines. Dentist ensures that information regarding the referral and triage processes is appropriately explained to patient Referrals from other health professionals, with the exception of suspected head and neck cancers must have primary dental care assessment. | Level 2 and 3 procedures communicated to referrers and OS providers. Agreed OS referral guidance, including required data set, communicated to referrers and Oral Surgery providers. Consistent and accurate data set with respect to referrer details. Appropriate radiographs to support diagnosis; ideally these should be digital images sent electronically. Documentation of incidences when patient compliance prevented diagnostic radiographs. Consistent and accurate data set with respect to patient demographics and contact details. Specific relevant medical history communicated to Oral Surgery provider. Patient appropriately informed and aware of the Oral Surgery procedure that is required and the reasons why it is required. Patient anxiety assessed. Indicator of Sedation Need (IOSN) completed if sedation is considered necessary. ASA (American Society of Anesthesiologists) physical classification of the patient is assessed: I, II, III or IV I – A normal healthy patient II – A patient with mild systemic disease III – A patient with severe systemic disease IV – A patient with severe systemic disease that is a constant threat to life Dentist referring within 2 working days of the decision to refer being made. | Number (%) of referrals received that have complete referrer details. Number (%) of referrals received that have complete patient demographic and contact details. Number (%) of referrals that have specific relevant medical history. Number (%) of patients aware of the Oral Surgery procedure they require and why. Number (%) of patients confirming receipt of information with respect to: procedure; choice appropriate to needs and level of complexity; and Oral Surgery provider details. Number (%) of patients assessed with respect to level of dental anxiety. Number (%) of patients requiring sedation who have a completed IOSN. |
| Triage decision making with respect to complexity and setting | Standards | Metrics | Enablers |
|---|---|---|---|
| Every patient identified by a unique reference number (URN) to enable tracking of referral e.g. NHS number, dental registration number or other URN. Consultant-led decision making within 4 working days of receipt of referral. When triage decision unclear (Level 2 or Level 3, escalate) patient may be required to attend an assessment clinic to determine appropriate care provision. | Specialist triage decision made within 4 working days of receipt of referral. Relevant medical history details included with triage decision. Any other information e.g. wheelchair user Accuracy of diagnostics assessed and reported upon. All referrals received have appropriate readable radiographs and work up. Primary care dentists who refer Level 1 procedures contacted to ascertain their reasons for referral and any requirements for remedial training | Number (%) of referrals where specialist triage decision is made within 4 working days from receipt of referral. Number (%) of referrals that are deemed at triage to have appropriate Oral Surgery procedural level and setting request. Number (%) of incidents of unplanned difficulties reported. Number (%) of referrals received that have readable radiographs and work up as set out in referral/ procedure guidelines OR that reported patient compliance issues that prevented accurate diagnostic radiographs from being taken. Number (%) of referrals received that require patient assessment and onward referral to specialist Level 2 or 3 service in a secondary care setting due to surgical difficulty not recognised by referrer, complex medical condition or other. | Electronic access to referrals available within 4 days. Referral and triage decision can be tracked electronically by both referrer and patient. Specialist triage decision making Incorporated into specialist (consultant) job plan. Referrers have access to high quality digital DPT radiography facilities and can use these appropriately to assist in timely diagnosis, referral and treatment. Access to, and funding for, Head and Neck EQA compliant diagnostic service in a CPA/ISO1519 accredited laboratory |
| Assessment: decision made to treat | Standards | Metrics |
|---|---|---|
| Referral and triage decision Patient receives information in an appropriate format regarding oral surgery procedure and provider setting. | Patient informed of triage decision within one week of triage decision or earlier as part of the referral management system Referring dentist and patient informed when referrals have been assessed and require onward referral to Level 2 or 3 service in a secondary care setting due to surgical difficulty not recognised by referrer, complex medical condition or other. Appointment offered to patient within 4 weeks of triage decision or assessment. | Number (%) of referrals received that are assessed and need to be onward referred to specialist Level 2 or 3 service in a secondary care setting due to surgical difficulty not recognised by referrer, complex medical condition or other. Number (%) of triaged referrals that are appointed within 4 weeks for assessment and linked oral surgery treatment appointment made. Number (%) of appointments that are cancelled/postponed by patients. |
| Patient attends for oral surgery assessment (primary or secondary dental care setting) | Standards | Metrics |
|---|---|---|
| Patient has received appropriate information regarding the oral surgery assessment appointment Patient has choice of appointment time. Patient has all necessary maps and information about setting. When required, a responsible adult accompanies the patient to assist their understanding so they are able to give valid informed consent. Patient has information with respect to appropriate self-care after oral surgery procedure has been completed. | All criteria specified i.e. competence and qualification of operator and DCP. Record of CPD and evidence informed and based on professional consensus on treatment practices. Specialist formal appraisal and peer review; twice annual supervision visits and review format agreed. DPT radiography available on site and access to Cone Beam CT imaging available. Drugs and equipment available as recommended by RC UK. Unimpeded ambulance access to building and surgery (DDA compliant). Consent process aligned to current secondary care process. Chair-side IT available. All records completed using key diagnostic words and procedure codes to agreed toolkit. Tariff consistent with agreed NHS CB pricing | Number (%) of patients who have received appropriate information from referring practitioner re: proposed oral surgery procedure and choice of providers. Number (%) of cancellations by provider. Number (%) of DNAs/ cancellations by patient. Number (%) of records completed using key diagnostic words and procedure codes to agreed toolkit. |
| Delivery of oral surgery procedure (primary or secondary dental care setting) | Standards | Metrics |
|---|---|---|
| Patient has received sufficient information about procedure to enable them to provide informed consent. If secondary care setting is required, patient is aware why this is necessary Where sedation is required, a responsible adult accompanies the patient. Patient has information with respect to appropriate selfcare after oral surgery procedure has been completed. Named consultant takes responsibility of biopsied tissue that is sent to pathology services for reporting. Arrangements made for timely reporting of biopsy results to patient. | All criteria specified i.e. competence and qualification of operator and DCP. Record of CPD and evidence informed and based on professional consensus on treatment practices. Specialist formal appraisal and peer review and twice annual supervision visits and review format agreed. Environment and equipment available e.g. for oral surgery, meets specified standards i.e. sterile water supply, single use water line and surgical hand piece available. DPT radiography available on site and access to Cone Beam CT imaging available. Suitable magnification for endodontic Oral Surgery. Service setting needs to meet decontamination best practice HTM 0105. Drugs and equipment available as recommended by RC UK. Sedation equipment and environment meets SAAD checklist. Local Head and Neck EQA compliant pathology services and safe transfer system in place – gold standard. Unimpeded ambulance access to building and surgery (DDA compliant) Consent process aligned to current secondary care process Chair-side IT available. Responsiveness to an admitted patient’s personal needs. Control of pain, nausea or vomiting. All records completed using key diagnostic words and procedure codes to agreed toolkit. Tariff consistent with agreed NHS CB pricing | Number (%) of cancellations by provider. Number (%) of DNAs/cancellations by patient. Number (%) of cases where triage decision was different to care provided Number (%) of unplanned difficulty. Number (%) of adverse incidents e.g. extraction of wrong tooth; nerve injury; Re-admission/admission. Theatre and day case admission environment and process. Number (%) of records completed using key diagnostic words and procedure codes to agreed toolkit Number (%) of cases reported by Head and Neck EQA pathologist and in accredited laboratories |
| Discharge and follow up | Standards | Metrics |
|---|---|---|
| Patient is provided with all necessary discharge information in an appropriate format, including: Information on advised selfcare and who to contact following procedure should there be a problem; What to expect during the recovery period; and Information about postoperative ‘home check’. | Patient-friendly information available in a number of formats including information on what to expect post-surgery and who to contact and what to do if problems occur after discharge. Patient comfortable on discharge and prescribed pain relief where appropriate. Appropriate patients contacted for 24 hour ‘home check’ (using skill mix) e.g. telephone call, online, email survey or text messaging (maximum 2 contact attempts) to ask patient if they are experiencing any of the following: Persistent bleeding; Nerve injury; Unmanaged pain. If yes to any of the above or a Level 3 procedure has been carried out, patient contacted again (2nd ‘home check’) within 1 week of oral surgery procedure. If patient has not returned to normal function, review arranged. Adverse events and complications recorded and reported using Datix e.g. Patient collapse; Wrong site surgery; Damage to adjacent tissues; Jaw fracture; Displacement of tooth/root fragment; Chemical, thermal or mechanical damage e.g. to lip. | Number (%) of treatments completed where discharge information sent to referrer. Number of cases when the patient had to return or seek advice due to unexpected adverse event following care i.e. infection; post-op bleeding; pain, numbness/nerve injury etc. PROMs collected through ‘home check’ and other surveys. Routinely reported PROMs are described in section 13.3 of this Commissioning Guide Number (%) of patients who do not respond to 1st and 2nd ‘home check’ contact telephone calls. |
5. Reporting measures
Oral surgery patient reported experience
5.1 Patient reported outcome measures (PROMs)
The use of appropriate PROMs is essential for measuring the four key areas (access, communication, value for money and clinical care). The measures should be patient focused and consider potential inequalities throughout the patient journey. PROMs can be collected following treatment through ‘home check’ telephone calls and other surveys. However, providers should consider users’ different communication needs and alternative ways in which they can provide feedback.
PROMs should include core data that are collected consistently at a national level; and may additionally include data collected at local levels. Triangulation with other sources of information should be possible in order to validate data. There should be evidence to demonstrate that PROMs data are representative of the patient groups treated and not just those who can easily provide feedback. Generic PROMs regarding the effectiveness of care (using simple questions around function and oral health) are included in the ‘Guide for Commissioning Specialist Dentistry Services’.
Oral surgery services should report how they have evaluated, responded to, and acted upon PROMs feedback. Then they should demonstrate how services are being developed to improve patient experience as a result of these data.
5.2.1 Routinely-reported Oral Surgery PROMs
Routinely-reported (core) data should include specialty-specific (not procedure specific) PROMs. These are detailed in Table 5.2.2 below.
5.2.2 Table – Core PROMS for oral surgery
| Question | Response | Details |
|---|---|---|
| Did you need to seek advice or assistance hours/ days after the procedure? | Yes/No/Unsure | List for data recorder (not shared with the patient unless clarification or prompts needed) Interested in: Uncontrolled bleeding (%) Inadequate pain relief that needed further medication (e.g. dry socket? Typically 5% of cases) Infection that needed further treatment (%) Damage to other teeth/fillings (%) Nerve injury altered sensation (Typically 1% of cases) fifth or trigeminal TMD |
| Have you had to have additional surgery subsequent to this treatment? | Yes/No/Unsure | If yes, what is the problem? Fractures jaw Unintentional root retention Bone infection Nerve injury (1%) fifth or trigeminal |
| Time taken to achieve restoration of normal activities or appearance | Yes/No/Unsure | Days Weeks Months |
5.3 Measures (PREMs)
Generic patient reported experience measures (PREMs) are included in the ‘Guide for Commissioning Specialist Dentistry Services’. Table 5.3.1 presents PREMs for oral surgery patients.
5.3.1 Table – Oral surgery PREMs
| Question | Patient response to be recorded |
|---|---|
| Did the clinical team (clinician) involve you in your treatment decision in terms that you understand? | Agree/disagree/not sure |
| Did you receive information about the risks/ benefits in terms that you can understand before the operation? | Agree/disagree/not sure |
| Was your pain managed well during the procedure? | Agree/disagree/not sure |
| Was your anxiety managed well during the procedure? | Agree/disagree/not sure |
| Did you receive information, in a format that you could understand, about care after the operation and a contact number to call for help? | Agree/disagree/not sure |
| Were you given the opportunity to ask questions? | Agree/disagree/not sure |
| Did a member of staff tell you about medication side effects to watch out for when you went home? | Agree/disagree/not sure |
6. Clinical outcome measures
6.1 Clinical outcomes
Reference to CQC inspection reports and CQC outcomes could be used as evidence that appropriate processes and protocols are in place but do not look at clinical quality per se.
Publication of key outcome measures for dentistry and Oral Surgery in accordance with MyNHS (February 2015).[2]
6.2 Minimum standard data collection and reporting
Standard data collection and reporting should reflect the main objectives of the quality framework for dentistry [3] and national commissioning intentions[4] i.e. the implementation of patient pathways that include consistent:
6.3 Clinical quality outcomes
Table 6.4 outlines specific quality outcomes that are recommended for oral surgery.
Table 6.4 Clinical quality outcomes for oral surgery
| Quality outcome | Details |
|---|---|
| Clinical codes | In order to measure quality and effectiveness, these should include: Diagnosis Treatment Outcomes |
| Clinical effectiveness | Diagnosis OPCS-4 codes Treatment ICD codes Outcomes ICD codes Reported patient safety events Could include: Consent Patient info Pain management Anxiety management Patient information Morbidity PROMS Patient safety (QOF, CQUIN, CQC, MHRA) Compliance with guidelines: Patient information Antibiotic prescribing NICE indications for M3Ms Endodontic surgery Dry socket Basic suggestion – Have you required further corrective surgery? Retreatment surgery or medication or admission Mortality Professional standards e.g. GDC, RCS |
| Quality standards | Quality and Outcomes Framework (QOF)[5]] |
| Patient experience | Specialty-specific (NOT procedure-specific) PREMs & PROMs |
| Safety | Medication and Healthcare products regulatory agency (MHRA) reported adverse drug reactions using the Yellow Card Scheme(any drug related serious event see below)82 Medical history checked. Appropriate drug prescription83 NPSA/ NRLS84 85 Wrong site surgery Wrong implant Retained foreign object Overdose of midazolam STEIS Commissioning for Quality and Innovation (CQUIN)[6] NHS Trusts report quarterly on: The proportion of patients with harm from a fall in care The proportion of patients with a VTE risk assessment % The proportion of patient with appropriate VTE prophylaxis % The proportion of patients being treated clinically for a new VTE% Overall The proportion of patients with ‘harm free’ care% Care Quality commission (CQC)[7] Collates data on reported serious events and governance and PROMs & PREMs. Serious events must be reported to the CQC within 21 days by provider or registered manager[8] if: Is fatal Is life-threatening- the patient is was in the view of the investigator, at immediate risk of death from the adverse event as it occurred Results in an UNPLANNED in-patient hospitalisation, or prolongs an existing hospitalisation Is significantly or permanently disabling Is a congenital anomaly or birth defect Iv antibiotics Serious harm to patients or death are events that require obligatory reporting to CQC and commissioning body. |
6.5 Primary care oral surgery provider minimum data set
The following is an example minimum dataset currently used by a primary care specialist oral surgery provider.
6.6 Diagnosis and procedure
- NHS Number
- Unique patient reference number
- Performer name
- Provider practice
- Name of referring dentist
- Date referral received by practice
- Date of appointment given
- Length of time from referral to appointment
- Appointment attendance (attended/failed)
- Pre-operative assessment appointment details
- Details of procedure performed
- Procedure date
- Follow-up visit details
- Total number of visits to complete the treatment
- Details of discharge letter sent to referring practitioner
- Oral Surgery-related adverse events
- Oral Surgery complication details, if any
- Treatment provided for oral surgery complication
- Final outcome of treatment
- Biopsy result
- Appropriateness of referral for the service
- Payment validity details
6.7 Outcomes of appointment
- Attended
- Not suitable for primary care oral surgery service
- Operative procedure not required
- Patient cancelled
- Patient did not attend
- Unable to contact patient despite repeated attempts
6.8 Clinical outcome
- Bleeding
- Dry socket
- Generalised pain
- Infection
- None
- Oro-antral communication
- Possible nerve injury
- Swelling
6.9 Treatment provided for complication
- Debridement of bone
- Intraoral Incision and drainage of abscess.
- Packing of tooth socket
- Prescription of oral antibiotics
- Surgical arrest of bleeding from tooth socket
- Suture of gingiva
6.10 Outcomes of treatment
- Discharged – no treatment provided
- Discharged – treatment completed
- For follow up
- Referral to secondary care: Further management of current treatment
- Referral to secondary care: As a new consultation
- To see referring GDP for further discussion/management
7. Value and impact
7.1 Value for money
Assessing value for money will need to take account of local oral health needs assessments and service capacity.
Consider
- Access to oral surgery services and barriers to care.
- Efficiency and effective measures
- access, waiting times, provision of urgent care / freedom from pain
- some data could be collected using PROMs
- Safety
- Quality of life questionnaires
Appendix 1- competency framework
Competency framework for oral surgery practitioners
N.B. The professional qualifications and training requirements listed in this table apply to individuals who are currently undertaking training or who wish to undertake training in the future. Existing practitioners and providers may not necessarily have followed the recently established training pathways, and may not hold any or all of these qualifications, but have demonstrated clinical excellence in oral surgery for many years. These practitioners should not currently be excluded from consideration of provision within the commissioning process.
There are currently insufficient specialists and consultants to manage the population oral surgery needs and so general dental practitioners with enhanced clinical skills and competence assured by the Managed Clinical Network (MCN) in line with the published Accreditation of Performers of Level 2 Complexity Care may also undertake Level 2 complexity care as described below. The MCN may also find the ‘Career Pathways in Dentistry Professional Framework’ published by the College of General Dentistry 2022 helpful in its description of dentists with enhanced skills and competence.
| Assurance criteria | Primary care dentist (non specialist) | Dentist with enhanced skills and competence | Specialist in oral surgery | Consultant in oral surgery |
|---|---|---|---|---|
| Experience | Registered as a dentist with the GDC. | GDC-registered primary care dentist with enhanced skills and competence in oral surgery | Must be on GDC oral surgery specialist list. | Must be on GDC oral surgery specialist list. |
| Qualifications | No additional qualifications necessary. | Additional experience, enhanced skills and competence assured by MCN | Must be on GDC oral surgery specialist list. | Must be on GDC oral surgery specialist list. |
| Training in oral surgery | No specific training in Oral Surgery. | No specific training in Oral Surgery. Evidence of experience, enhanced skills and competence | Must be on GDC oral surgery specialist list. | Must be on GDC oral surgery specialist list. |
| Teaching and education | Undergraduate teaching in oral surgery. May have attended relevant postgraduate oral surgery courses. | Evidence of attendance at relevant postgraduate oral surgery courses. Evidence of experience, enhanced skills and competence. | Supervision of higher training in oral surgery and provision of mentorship for dentists with enhanced skills and competence who provide primary care oral surgery services. Involvement in undergraduate &/or postgraduate training desirable. | Leading higher training in oral surgery and provision of mentorship for dentists with enhanced skills and competence who provide primary care oral surgery services. Involvement in undergraduate &/or postgraduate training desirable |
| Referral base | Providers must provide level 1 care. | Providers will accept level 2 care referrals as defined by the terms of the oral surgery care pathway. It is not expected that level 1 care will be provided. | Providers will accept level 2 referrals as defined by the terms of the oral surgery care pathway | Providers will accept level 3 referrals as defined by the terms of the oral surgery care pathway |
| Clinical expertise | Clinical experience limited for patients with oral surgery needs. May undertake shared care with specialist or dentists with enhanced skills and competence. Ability to recognise when the help and advice of a specialist or dentist with enhanced skills and competence is required. | Ability to carry out a range of clinical activity for patients with moderate needs. Ability to recognise when help and advice of a specialist is required. Membership of Managed Clinical Network (MCN) | Acceptance of a wide range of clinical cases for patients with complex needs. Taking a lead role for developing a local infrastructure for the delivery of oral surgery. Participation in Managed Clinical Network. | Acceptance of a wide range of clinical cases for patients with complex needs. Taking a lead role for developing a local infrastructure for the delivery of oral surgery, including service development and workforce planning. Participation and supervisory role in Managed Clinical Network |
| Continuing professional development | May attend relevant oral surgery courses as part of CPD cycle (GDC requirement. | Ability to carry out a range of clinical activity for patients with moderate needs. Ability to recognise when help and advice of a specialist is required. Membership of Managed Clinical Network (MCN) | Co-ordination, provision and participation in CPD in oral surgery. | Acceptance of a wide range of clinical cases for patients with complex needs. Taking a lead role for developing a local infrastructure for the delivery of oral surgery, including service development and workforce planning. Participation and supervisory role in Managed Clinical Network |
| Setting and facilities | Primary care setting. Compliance with CQC, DDA and HTM 01-05. Appropriate oral surgery equipment to meet current quality and patient safety standards. | Primary care setting. Compliance with CQC, DDA and HTM 01-05 at best practice level. Appropriate oral surgery equipment to meet current quality and patient safety standards. Provision of care as per specific contract. | Clinical experience and training enables provision of care in a variety of clinical settings, including primary and secondary care. Appropriate oral surgery equipment to reflect complexity of procedures delivered, which meets current quality and patient safety standards. | Clinical experience and training enables provision of care in a variety of clinical settings including primary and secondary care. Appropriate oral surgery equipment to reflect complexity of procedures delivered which meet current quality and patient safety standards. |
| Dental team and multidisciplinary teams | Works with dental team and may not have any training in oral surgery. | Dental team trained both formally and informally in oral surgery, appropriate to contracted activity, to include sedation, BLS/PLS etc. | Dental team trained both formally and informally in oral surgery appropriate to contracted activity to include sedation, ILS/PLS etc. | Dental team trained both formally and informally in oral surgery to include sedation, ILS/PLS etc. Part of MDT. |
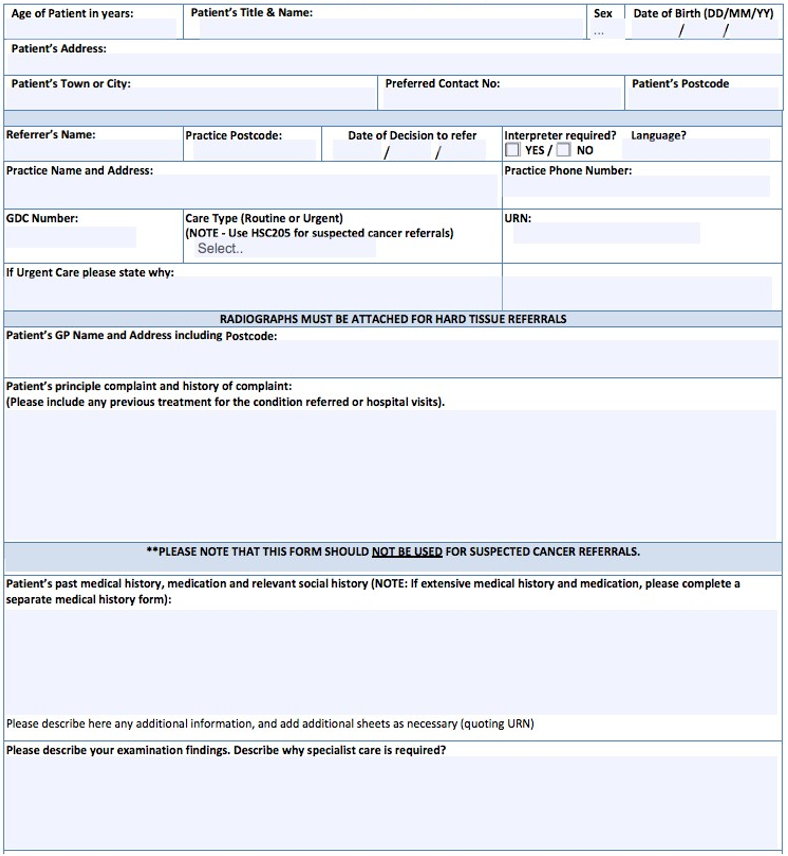
Appendix 2 – referral form
Specialist dental services referral form example
Appendix 3 – coding
Coding used by secondary care oral surgery/OMFS departments
Descriptions of clinical standards for Primary Care/OMFS units are presented in the following lists APP3.1 – APP3.4.
Electronic versions of the National Clinical Coding Standards ICD-10 4th Edition reference book and the National Clinical Coding Standards OPCS-4 reference book, for use from 1 April 2015, are available from the Health and Social Care Information Centre Technology Reference data Update Distribution site93.
APP3.1 Diagnostic codes (these do not currently conform to NICE guidelines)
Diagnosis
- Periapical abscess
- Dental caries
- Pericoronitis (no code)
- Periodontal disease
Radicular Cyst - Odontogenic cyst
- Resorption M2M or M3M
- In line of fracture
- For orthognathic or ablative surgery
- Retained root
APP3.2 Treatment codes
Treatment
Procedure not carried out because of patient’s decision for other and unspecified reasons (Use code for failed appointment)
- Intraoral examination
- Unspecified examination of the mouth
- Intraoral radiology film
Other diagnostic imaging of mouth - Creation of impression for dental prosthesis e.g. bite guard
- Simple extraction of tooth
- Surgical extraction of third molar(s)
- Surgical extraction of other teeth
- Surgical removal of wisdom tooth
- Surgical removal of tooth
- Surgical removal of retained root of tooth
- Extraction of multiple teeth
- Apicectomy of tooth
- Surgical exposure of tooth
- Insertion ortho appliance
- Coronectomy
- Biopsy of lesion on tongue
- Full dental clearance
- Extraction single tooth
- Enucleation cyst
- Excision lesion from jaw
- Fraenectomy
- Packing socket of tooth
- Arrest haemorrhage
- Debridement of socket
- Biopsy gingivae
- Biopsy tongue
- Biopsy palate
- Biopsy lip
- Biopsy lesion of mouth
- Operation maxillary antrum
- Drainage of abscess of alveolus
- Suture of mouth
- Removal suture from mouth
- Fitting of dental prosthesis bite guard
- Minor mouth or throat procedure
- Intermediate mouth or throat procedures
- Oral surgery
- Oral and maxillofacial surgery
- Local anaesthetic
- Oral sedation
- Inhalation sedation
- IV sedation
- Outpatient general anaesthetic
- Inpatient anaesthetic
- Steroids
- Antibiotics
- Other
APP3.3 Clinical outcome codes (ICDN code)
Clinical outcome
- Dry socket
- Trigeminal nerve injury
- Altered sensation/numbness/pain
- Use for implant insertion damaging inferior alveolar nerve
- Numbness of tongue or lip
- Paraesthesia of tongue or lip
- Pain in joint (TMJ)
- Infection of bone /joint
- Osteomyelitis
- Cellulitis
- Oro-antral fistula / chronic sinusitis
- Fracture mandible
- Tuberosity fracture
- OAC
- Fracture of tooth
- Retained root
- Dislocation of tooth: luxation, extrusion or avulsion
- Unintentional cut during surgical e.g. tongue/cheek laceration
- Bleeding from socket
- Retreatment <21 (CQC) <30 days (CQUIN)
- Surgical reoperation medical
Current coding deficiencies that require addressing:
No codes for acute or chronic pericoronitis;
No ability to differentiate if caries is in the tooth itself or adjacent teeth;
No codes for local spreading infection;
No code for high risk of development of caries /damage in adjacent tooth;
No codes for LA, Sedation, GA or additional operative medication;
No code for coronectomy.
APP4.4 Co-morbidity codes used in oral surgery departments in secondary care
Co-morbidity
- Smoker
- Blindness
- Ischaemic heart disease
- Cardiac arrhythmia
- Prosthetic heart valve
- Cardiac failure
- Congenital Cardiac Malformation. This code refers to the cardiac chambers and connections. If this is for ASD or PFO Q21.9 would be more appropriate. Please confirm.
- Cerebrovascular disease
- Hypertension
- COPD / COAD
- Asthma
- Chronic renal disease
- If with increased BP/failure
- If with increased BP/no failure
- Chronic liver disease
- Transplanted (any) organ
- Pre-transplant/chemo/bisphosphonate assessment
- Epilepsy
- Parkinson’s disease
- Movement disorder
- MS
- Dementia
- Dental phobia
- Mental health problems
- Learning disabilities
- Diabetes type 1
- Diabetes type 2
- HIV disease – symptomatic HIV disease – asymptomatic
- Hepatitis B
- Hepatitis C
- Other infectious disease
- Bleeding disorders, Coagulopathy
- Long term anticoagulant therapy
- Sickle cell disease
- Bisphosphonate therapy
- Cancer current disease.
- History of malignant disease
- Alcohol dependence
- Cannabis dependence
- Cocaine dependence
- Heroin/methadone dependence
- Drug dependence (combination)
- Endocrine disorder
- Disease of digestive system
- Autoimmune disease
- Congenital malformation of skull/face bones
- Arthritis, unspecified
References
[1] Kendall N. Improving access to Oral Surgery services in primary care. Primary Dental Care 2009; 16(4): 137-142.
[2] MyNHS (February 2015). greater transparency for better health and care MyNHS planning 2015-2017 Available at gov.uk Accessed February 2015
[3] Dental Quality and Outcomes Framework 2011. Available at gov.uk. Accessed February 2015.
[4] NHS Commissioning Board. Securing Excellence in Commissioning NHS Dental Services February 2013. Accessed February 2015
[5] Health and Social Care Information Centre. Quality and Outcomes Framework. Available at: http://www.hscic.gov.uk/qof Accessed February 2015 82
MHRA Vigilance, safety alerts and guidance . Accessed February 2015
83 – SCDEP Drug Prescribing For Dentistry Second Edition, published August 2011 Latest Update – September 2014. Accessed February 2015
84 – NHS Commissioning Board Special Health Authority Patient Safety (National Patient Safety Agency) Accessed February 2015
85 – National Patient Safety Agency National Reporting and Learning System Accessed February 2015
[6] CQUIN pct portal
[7] Care Quality Commission. Dentistry. Accessed February 2015
[8] Care Quality Commission. Notifications. Accessed February 2015

