Accessible image text
Laxatives are always first line management of acute or chronic constipation in children. Do not use diet and fluids alone as treatment.
Chronic constipation
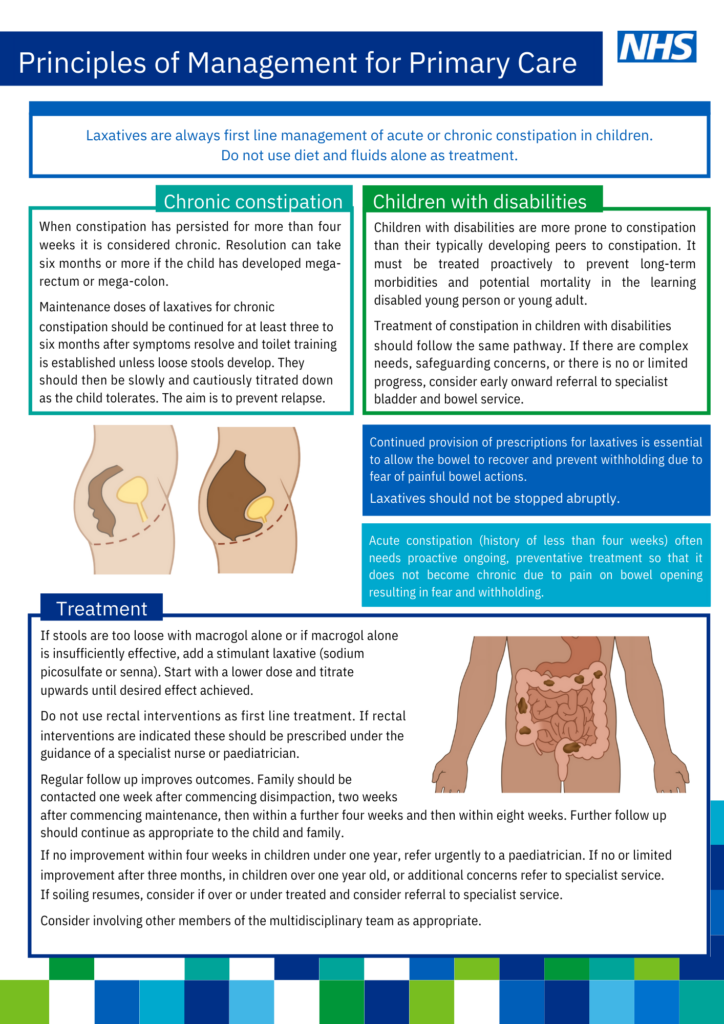
When constipation has persisted for more than four weeks it is considered chronic. Resolution can take six months or more if the child has developed megarectum or mega-colon. Maintenance doses of laxatives for chronic constipation should be continued for at least three to six months after symptoms resolve and toilet training is established unless loose stools develop. They should then be slowly and cautiously titrated down as the child tolerates. The aim is to prevent relapse.
Children with disabilities
Children with disabilities are more prone to constipation than their typically developing peers to constipation. It must be treated proactively to prevent long-term morbidities and potential mortality in the learning disabled young person or young adult. Treatment of constipation in children with disabilities should follow the same pathway. If there are complex needs, safeguarding concerns, or there is no or limited progress, consider early onward referral to specialist bladder and bowel service.
Note
Continued provision of prescriptions for laxatives is essential to allow the bowel to recover and prevent withholding due to fear of painful bowel actions. Laxatives should not be stopped abruptly.
Acute constipation (history of less than four weeks) often needs proactive ongoing, preventative treatment so that it does not become chronic due to pain on bowel opening resulting in fear and withholding.
Treatment
If stools are too loose with macrogol alone or if macrogol alone is insufficiently effective, add a stimulant laxative (sodium picosulfate or senna). Start with a lower dose and titrate upwards until desired effect achieved.
Do not use rectal interventions as first line treatment. If rectal interventions are indicated these should be prescribed under the guidance of a specialist nurse or paediatrician.
Regular follow up improves outcomes. Family should be contacted one week after commencing disimpaction, two weeks after commencing maintenance, then within a further four weeks and then within eight weeks. Further follow up should continue as appropriate to the child and family.
If no improvement within four weeks in children under one year, refer urgently to a paediatrician. If no or limited improvement after three months, in children over one year old, or additional concerns refer to specialist service.
If soiling resumes, consider if over or under treated and consider referral to specialist service.
Consider involving other members of the multidisciplinary team as appropriate.