Introduction
This short guide outlines the principles behind rapid assessment and treatment (RAT), suggests practical steps to implement the approach and gives real-life examples. We also discuss the practical problems that need to be considered when implementing the model.
RAT provides early senior assessment of ambulance arrivals and may include ‘majors’ patients from alternate sources such as walk-in arrivals.
RAT is not a panacea and implementation can be difficult, particularly where there are challenges in matching capacity and demand. Senior clinicians who lead RAT teams can find the intensity of work challenging. Poor flow out of the emergency department (ED) can also present a challenge.
Its benefits include:
- patient safety and satisfaction
- improved ambulance handover times including ‘time to initial assessment’ and ‘time to treatment’ indicators
- undifferentiated patients are seen early in their journey
- early instigation of appropriate investigations
- management plans in place for prompt treatment
- early specialty referral.
- helps mitigate risk.
What is RAT?
RAT typically involves the early assessment of ‘majors’ type patients in ED, by a team led by a senior decision-maker (consultant, registrar or senior advanced clinical practitioner), with the initiation of a clinical assessment, diagnostics, treatment and/or referral to specialty teams.
The approach consciously removes ‘triage’ (as distinct from streaming) and initial junior medical assessment from the pathway. Instead, the first clinician a patient sees is one who can make an initial assessment, define a plan of care and, where appropriate, refer to an inpatient specialty team or same day emergency care (SDEC). RAT is not dependent on a single geographical location (though some departments have allocated spaces which may benefit work productivity) but instead a mindset (process), and teams then implement the first stages of the plan of care.
Aims
The aims of this approach include:
- access to earlier initial assessment
- value-adding steps in the patient journey start sooner
- utilisation of ambulance crews PCR or ePCR both pre-hospital and on arrival
- clinical resources previously tied up in initial assessment processes can be re-tasked to provide value-adding care
- unnecessary investigations and tests reduced with early senior clinician input
- subsequent junior medical assessment directed by the RAT plan of care
- patients for specialty assessment/admission identified earlier and can leave the department more quickly
- clinical risks associated with undifferentiated patients waiting for senior clinical review reduced
- senior clinicians gain an overview of patients entering the department
- time critical treatments and investigations initiated early (eg specialty care bundles including fractured NOF or CT-head where indicated in head injury)
- clinical outcomes and the patient experience improved.
Challenges
The challenges of RAT are:
- The RAT process is demanding in terms of senior clinical input. Most departments do not run RAT 24 hours a day. Experience suggests that running RAT during more limited core hours can be effective and deliver considerable benefits. However, there are good examples of nurse-delivered RAT models both out of hours and when there are senior clinician staffing constraints.
- Most systems focus RAT on ambulance patients. It is important to ensure the pathway can also meet the needs of ‘walk-ins’ who present with serious illnesses.
- Not all ambulance patients require a senior clinician review. Pathways must be flexible enough to stream patients whatever their point of entry, which may include SDECs or urgent treatment centres (UTCs).
- Bias and error of early assessment may be carried through into majors. A culture of constructive challenge to early decisions should be encouraged.
- The RAT process can be mentally demanding. This needs to be considered when planning rotas, eg some rotas have a 2 hours on, 2 hours off approach.
Process
RAT models
Several local RAT models have developed over recent years, all of which aim to provide early assessment and the start of treatment for ‘majors’ arrivals.
Typically, RAT has three potential outcomes:
- An intervention completely contained within the emergency department (ED), with discharge home/to GP.
- Referral to an inpatient specialty for assessment/admission, with or without initial investigations.
- Transfer to an alternative provider, service or facility.
An essential component of all models is ‘internal professional standards’ that define the times within which interventions take place. For example, some departments have decided that ‘time from arrival to RAT’ should not exceed 15 minutes; ‘time from RAT to decision to admit’ should not exceed 2 hours; and ‘time for imaging requests to be completed’ should not exceed 1 hour. By setting and measuring such standards, bottlenecks can be identified and performance requirements clearly understood by team leaders.
RAT teams typically consist of a senior clinician, qualified nurses, healthcare assistants and, sometimes, a dedicated porter and clerical staff.
To function effectively, RAT models depend on teamwork and clear communication. The RAT team should be resourced with all necessary equipment (eg POCT diagnostics and ECG machines) to help inform clinical decision-making and risk management.
Following assessment and initiation of treatment, patients are typically transferred to ongoing care environments such as ED areas, SDEC or assessment units.
RAT design principles
- Assemble a multidisciplinary team to design your local model of rapid assessment, including non-clinical support staff, and communicate your plans and intentions.
- Use a ‘model for improvement’ (eg PDSA) to test your ideas and plans.
- Design rotas to match capacity and demand.
- RAT should be considered a process rather than a location in which it happens. This is particularly relevant in times of high cubicle occupancy/demand.
- Introduce a standard clerking pro forma and documentation to support your model.
- Measure metrics.
- Project manage the implementation of your local model.
- Ensure rapid access to diagnostics.
- Allocate dedicated equipment to the RAT team.
- Design a system that can flex to demand; this should include in hours/out of hours.
- Introduce internal professional standards for response time to support speedy referral.
- Consider implementing rapid assessment into assessment units.
Metrics
The following measures are examples of recommendations from the ECIST team:
- Improvement in mean ambulance to hospital handover performance (national QI: ambulance handover <15, >15, >30 and >60 minutes). Note: The practice of returning a patient to the ambulance after RAT would not deliver this change and would not be recommended.
- Reduction in time from arrival to treatment (national QI: median time to clinician from time into ED <60 minutes).
- Reduction in time from arrival to referral to an inpatient team. The NHS England Opel 1 escalation card defines this to be within 30 minutes.
- Where indicated:
- reduction in time from arrival to analgesia (RCEM standards on pain)
- reduction in time from arrival to first-line antibiotic (sepsis)
- reduction in time from arrival to investigation (pathology and/or imaging).
- Measure length of stay pre a RAT process and post implementation.
- Length of stay in the department for admitted patients.
- Length of stay in the department for non-admitted patients.
All the above are time driven but you can also look at and measure human factors such as team dynamics, staff survey and patient satisfaction.
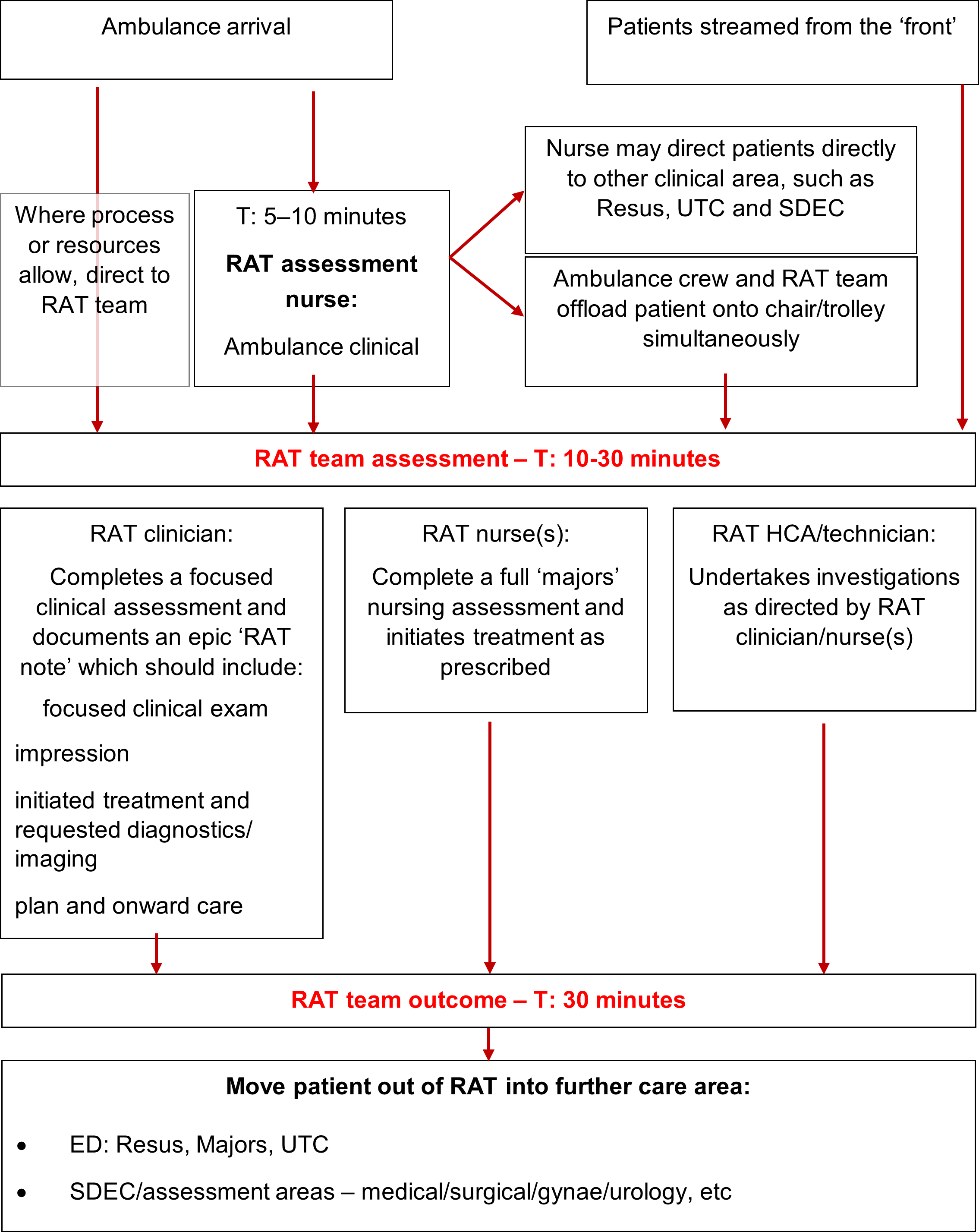
Example RAT process with indicative times
The above figure shows the process from when someone is directed to the RAT team to them moving out of RAT into further care. It sets out indicative times within which interventions take place including T: 10-30 minutes for a RAT team assessment and T: 30 minutes for a RAT team outcome.
Publication reference: PRN00958