Context
Over the past decade, there has been increasing need for mental health services to support children and young people (CYP). The pandemic resulted in a greater number of CYP presenting with mental health disorders, often with complex needs requiring care or medical stabilisation, within a paediatric or acute setting. Increasing need, coupled with winter pressures, has put a strain on systems. We need to work together to ensure CYP, and those who look after them, are supported.
The commitments outlined in the NHS Long Term Plan (LTP) make clear that achieving parity of esteem – valuing mental health equally with physical health – is a key priority, though we acknowledge there is still some way to go in meeting this challenge. For services to be delivered effectively and for patients to feel supported and staff to feel confident, we need to facilitate better integration of physical and mental health for CYP.
The NHS Long Term Plan’s Mental Health Implementation Plan has provided investment to:
- achieve 100% coverage of comprehensive crisis services to support CYP by 2023/24
- provide access to children and young people’s mental health community services for an additional 345,000 CYP aged 0-25 by 2023/24.
Most CYP with mental health needs should be supported in the community, and hospital admissions should be avoided where possible. There remain, however, instances where attendance or admission to an acute setting may be the most clinically appropriate option.
It is also recognised that when CYP are identified as requiring specialist children’s mental health care, a short admission to a paediatric ward may be appropriate whilst assessment takes place. However, due to complexities and pressures across the system, increased mental health needs, or a break down in a social care placement, some CYP may remain in an acute paediatric setting as a place of safety for longer periods than ideal.
For CYP and their families/carers, their initial contact with a service plays an important role in defining their expectations of care. Being treated with compassion and respect can have a marked impact on their experience and how they subsequently engage with services. Wherever a child first presents in crisis, this is an opportunity to positively impact their care experience.
How NHS England are responding
NHS England are committed to delivering on the LTP ambitions and have continued to expand and transform services. All-age 24/7 crisis helplines are available across the country so anyone, including CYP, can get urgent help whenever they need it. Mental health support teams continue to be rolled out in schools and colleges.
The CYP Mental Health and CYP Transformation Programme team jointly released £6m in 2022/23 to enable regions and systems to pilot and enhance integration opportunities, including testing service innovations. Iterative learning from this will underpin further work as we collectively aim to:
- Better understand how we can best provide safe, compassionate and appropriate care for patients.
- Ensure the paediatric workforce is trained and supported when caring for CYP presenting to hospital with acute mental health needs, and that the workforce understands where to get additional help, should they need it.
- Understand how systems and clinicians can work together better by reviewing pathways, identifying areas of innovation and best practice.
Royal Colleges, professional bodies, national, regional, and local system colleagues continue to support transforming pathways of care, whilst ensuring services work together to provide a holistic approach for CYP with physical health needs, mental health needs, or both.
Responding at a regional and system level
These six recommendations will facilitate systems to come together to collectively support CYP with mental health needs who present in acute paediatric settings, as well as supporting the clinical teams that manage these patients:
- Ensure that five key principles underpin joint working to support CYP with mental health needs who present in acute paediatric settings, and that a culture is fostered where we work collaboratively in providing holistic care for our CYP.
- Develop ways of working that bring system partners together across the patient journey and understand where systems are in developing joined-up pathways. This may include learning from areas doing good work to transform care across their wider footprint.
- Understand system maturity by considering ‘what good looks like’ and where the system sits along that journey.
- Ensure that specific consideration is given to managing CYP with a learning disability or autistic CYP who may present to hospital with acute mental health needs. Some systems have developed a holistic approach.
- Work together to ensure the clinical team(s) within the acute setting have the support they need to deliver high quality care. This includes ensuring access to training and education across the system.
- Testing and developing the evidence around innovative practice.
Further information and sharing good practice
For more information, support or to share good practice in your area, please do not hesitate to contact acutesetting.cypmh@nhs.net.
Element 1: Key principles
Ensure that five key principles underpin joint working to support CYP with mental health needs who present in acute and paediatric settings, and that a culture is fostered where we work collaboratively in providing holistic care for our CYP:
- Foster a culture where we work collaboratively in providing holistic care for our children and young people.
- A paediatric setting can be the right place for children and young people with mental health needs to receive care .
- The paediatric workforce should be supported by a multi-disciplinary team, both within a provider and by the wider system.
- Colleagues from health and social care systems should collaborate across acute and mental health care to avoid long waits in A&E and delayed discharge.
- High quality and safe care should be personalised for the needs of the child or young person. This would include joint escalation processes across the wider integrated care system, with reasonable adjustment made where required.
Element 2: System working
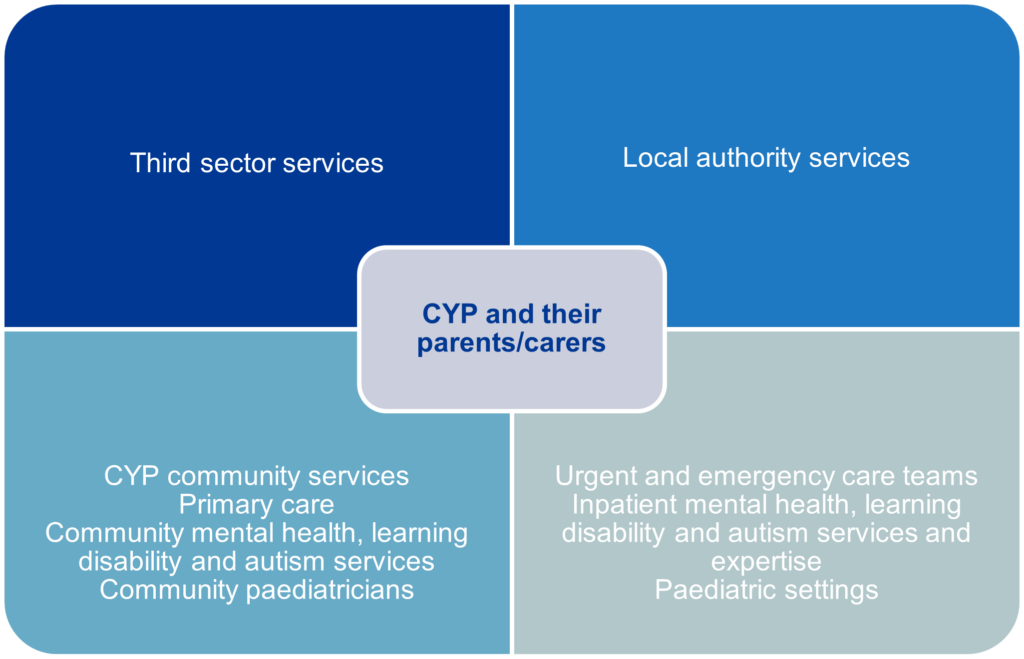
We all have a role to play in collectively supporting CYP who might present in acute environments in crisis, or with physical health needs, such as self-harm injury or refeeding. The graphic below summarises the range of services that could be involved in sharing information and supporting CYP with mental health needs, with the aim of avoiding hospital admission, where possible. The young person and their parents/carers should be involved throughout their journey.
We know that winter surge may impact paediatric bed capacity across the country and that we therefore need to work together across traditional boundaries to support systems and CYP. All paediatric settings should continue to work together to understand their ability to flex acute care capacity. This includes thinking about overall bed utility, including CYP with acute mental health needs receiving care within a paediatric setting.
Case study
Within Newham University Hospital, an average of three to six acute paediatric beds (from a total of 18-21) were being used for CYP with a variety of mental health needs. To ensure their ability to flex beds during a potential surge in 2021, they came together through joint planning, discharge discussion, and escalation and communications.
- NUH Acute, CYPMHS, social care and CCG/LA met weekly to discuss immediate issues, develop plans together and identify children requiring support to facilitate discharge.
- The Newham multi-agency collaborative met weekly to discuss and arrange a support offer for lower level “green” CAMHS referrals. From June 2021, they triaged and responded to over 100 cases.
- Monthly meetings also occurred to review system plans for CYP with learning disability or autistic CYP with the aim of developing crisis and early intervention offers.
- Daily SITREP to outline general paediatric and PICU beds availability via an app-based function is available with real time data. Thrice weekly CAMHS calls to discuss “bubbling cases” requiring tier 4 bed or other CAMHS support.
- Engagement events with young people and parent/carers on how to better respond when young people are in MH crisis.
- Development of bespoke support including care package, respite, family support to enable discharge.
- Currently developing plans for intensive support pathway, including residential “respite/step down” provision to adapt the offer of support to CYP and their families.
To find out more, please contact: Marie Trueman-Abel, Head of Commissioning & Transformation, NHS North East London, marie.trueman-abel@nhs.net
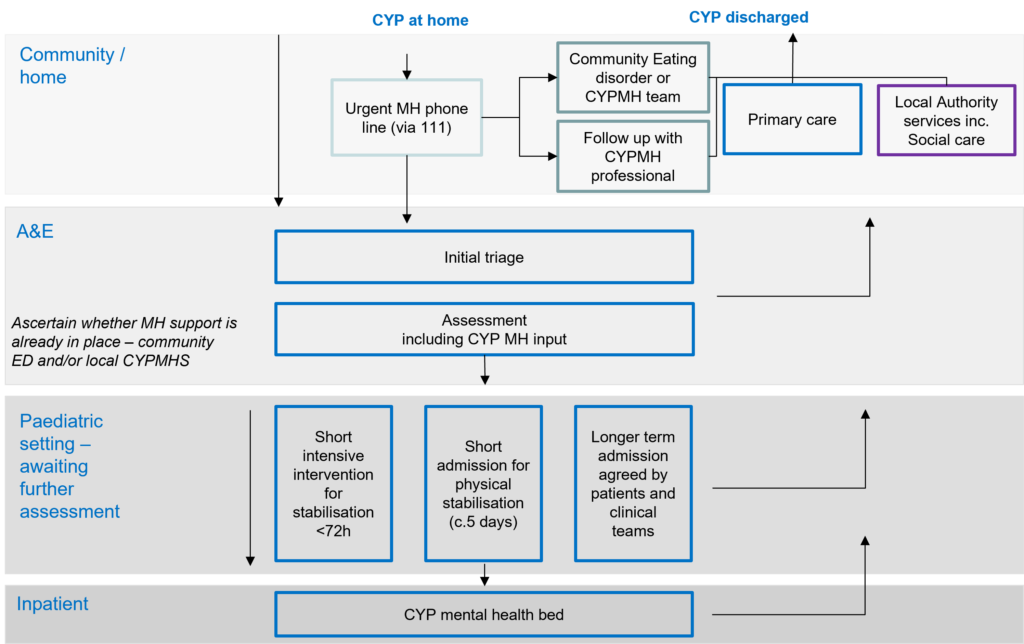
To facilitate joint working, an aspirational pathway for CYP with mental health needs in acute paediatric environments has also been developed:
Element 3: System maturity
The domains and related indicators below have been designed to support systems to gain an understanding of what good looks like for supporting CYP with MH needs within acute paediatric settings, and to aid in building an understanding of where your local system currently sits on that journey.
Domain: Culture
Measuring success:
- Evidence of collaboration across physical health, mental health and local authority services – including children’s social care services and primary care – who see the patient as a joint responsibility.
- Treatment and recovery are planned and delivered effectively as a wider multidisciplinary team, both pre- and post-discharge (including consideration of safeguarding principles).
Domain: Embedding innovation
Measuring success:
- Dedicated time and governance devoted to consider/agree goals and action plans.
- Evidence of discussion and collaboration between physical and mental health services.
- Sustainability planning in place.
- Service users are leading innovative practice and service development.
- Engagement with all colleagues is sought; opinions and concerns listened to and acted upon.
- CYP and families are informed, empowered and involved in decision making.
- Learning from any recent pilots relating to acute environments and mental health/learning disability and autism have been considered and implemented, if appropriate, and where resources allow.
Domain: Workforce
Measuring success:
- Highly diverse skill set appropriate to the patient group and wide range of disciplines within the MDT. Strong representation of physical health, mental health and social care roles (this can be across providers in areas in which there is collaboration between services in meeting CYPMH needs). Clear evidence that CYPMH is considered during recruitment processes at every level, also as a key part of any workforce development planning.
- CYP representatives are included as part of the recruitment process.
- Issues within the workforce are quickly responded to and there are local escalation processes if a solution cannot be found.
- Mental health training, as set out in this framework, is widely embraced for both emergency department and ward-based staff caring for patients with mental health conditions. The trust may have a paediatrician who has responsibility for mental health and physical health.
- A regular, varied training programme is embedded and encouraged as part of multi-professional CPD. Barriers to accessing training have been mitigated or removed. There is feedback documented as outcome measures from staff that give assurance the training is successful.
- Staff are trained on legal frameworks to use when providing care in the acute setting, enabling informed decision making. Advice from the trust solicitor and senior clinical and operational staff is also sought, where relevant.
Domain: Approach to system working
Measuring success:
- All partners engaged: there are regular MDT meetings which are well attended by partners and MH trained team members in acute settings/paediatricians in MH teams, etc.
- Strong shared governance arrangements are in place with good working relationships. This may be demonstrated via shared policies and SOPs, etc.
- There is a well-developed understanding of population need, including inequalities. CYP are included in planning of services and provide feedback on their care.
- Clear pre-admission meetings with partners to agree aim of admission and discharge triggers. Where pre-meeting has not taken place, eg due to unplanned admission, a post-admission meeting should take place.
Domain: Approach for escalation
Measuring success:
- Locally tailored, written CYP crisis escalation protocols are in place for ICBs aligned to acute escalation protocols.
- Clarity over when/if escalation to regional colleagues and national colleagues is clear, well communicated and understood.
- Regional and national escalation happens rarely as local protocols are robust.
- CYP are looked after in the least restrictive manner possible, in the least restrictive environment.
- Practitioners regularly assess, review and document consent, competence and/or capacity.
Element 4: Caring for CYP with a learning disability or autistic CYP
One of our recommendations is to ensure that specific consideration is given to managing and supporting CYP with a learning disability or who are autistic who may present to hospital with acute mental health needs.
Here we describe programmes of work to support systems with considering the needs of CYP with learning disabilities or autistic CYP. We also provide guidance on existing processes to support these CYP and the systems around them.
Sensory friendly environments – recommendations for sensory friendly wards
The ‘It’s Not Rocket Science’ report, compiled by the National Development Team for Inclusion and commissioned by NHS England, makes numerous recommendations on how inpatient CYPMHS sensory environments can be improved. Although this report focuses on mental health settings, the principles are useful for adaptation across acute settings:
- Create a predictable environment. Let people know what to expect, who to expect and when. Offer accurate and timely information to create more certainty and a feeling of safety.
- Involve autistic people with relevant expertise in reviewing the sensory environment, in a meaningful way. Every location is different and will have different things that need to be prioritised. Autistic people have different sensory perceptions, so it’s critical to involve people. Listen and take action. Continue to review. It is beneficial to bring in external expertise, but it’s also important to involve people using the space. Ask them what’s working and what needs to change.
- Ensure all staff have training from autistic experts and allies that understand autism and sensory needs. All staff includes the multidisciplinary team (MDT), healthcare staff, the ward team, facilities staff, educators, cooks, cleaners, and agency staff.
- Assess everyone’s sensory need on admission and consider how sensory need will be accommodated and supported in care plans. Support people to reduce problematic sensory inputs and manage these to support restraint reduction. As part of care planning, support people to do the things that help them to self-regulate, including repeated movement (“stimming”), access to hobbies and favourite possessions, quiet spaces, outdoor space, and access items such as noise cancelling headphones, caps, blankets, etc.
- Personalise risk management and decision making. Support people to have choice and control. Make decisions in relation to individuals, involving the person (and their family, as appropriate) wherever possible. Avoid blanket bans (decisions or bans that affect everyone, rather than being decided on an individual basis).
- Swap alarms for ‘silent’ alarms. This will significantly reduce noise and escalation on the ward and reduce the frequency of distress caused by alarms for those with auditory sensitivity. Staff need to be alerted rather than alarmed; silent alarms will ensure alerts happen without causing distress to other people.
- Reduce noise and echo. Ensure there is quiet space and outdoor space that people can access at any time. Soft furnishings, gently closing doors, carpet, sound absorbing panels and acoustic vinyl can all help. Consider background noise too (including roads, heating and cooling systems, extractor fans, voices, TVs/radio, chatting etc). Ensure there is a quiet space and outdoor spaces people can access at any time. Support time out from noisy or otherwise overloading environments as needed.
- Change all fluorescent lighting for alternatives. Ideally halogen, but high-quality LED bulbs, with diffused lights are better than fluorescent. Lights should be quiet – not buzzing or flickering.
- Consider the impact of smells. This includes smells from people, food, cleaning products, and laundry products. Neutralise smells wherever possible (closing doors, using unscented products, supporting people to ‘mask’ smells with preferred scents, or to use preferred products).
- Consider the impact of touch and texture. Hypo and hyper sensitivities might mean that people may be more or less sensitive to physical contact. This needs consideration in relation to potential physical restraint (best avoided), food, shower/bath/personal care and textures of materials including bedding, furniture, clothes and towels.
Two pilots (see annex 1) have been commissioned to develop sensory friendly environments, within acute paediatrics. Learning will be extracted and shared in future iterations of the framework.
Hospital passports
A hospital passport provides important information about a patient with a learning disability, including personal details, the type of medication they are taking, and any pre-existing health conditions.
The passport also includes information about how a person communicates and their likes and dislikes, which can be very important when they are first admitted to hospital.
This can include any communication aids, and how they can be used, so health staff can communicate clearly. They can also show how the person expresses things such as happiness, sadness, pain and discomfort.
Hospital passports allow health staff to understand the needs of the individual and help them make the necessary reasonable adjustments to the care and treatment they provide.
Examples of these can be found on the landing page of our related e-learning platform – co-developed with Health Education England – under ‘Featured co-produced resources’.
Dynamic Support systems
Building the Right Support and the NHS Long Term Plan (LTP) set out what autistic children, young people, and adults and people with a learning disability should expect when they need care and support in the community. This includes specific intervention and support for their mental health needs and for times of crisis or difficulty.
Dynamic support registers (DSRs) and care, (education) and treatment reviews (C(E)TRs) are central to the NHS LTP ambitions of: reducing the number of children and adults in inpatient services; avoiding inappropriate admissions; and developing responsive, person-centred services in the community. DSRs play a key role in helping health and social care and other partner organisations in local areas to identify their population of children, young people and adults with a learning disability, autism or both and to ensure they are included in commissioning plans, financial plans, service delivery and development. Most importantly, dynamic support exists to identify people whose health and care needs are increasing, or where there are complexities in how systems meet individuals’ needs. These people may require a multi-agency response to be able to receive care, education and treatment in their local community, or as close to home as possible wherever possible, avoiding hospital admission.
Care (education) and treatment reviews
For children and young people with a diagnosis of a learning disability or who are autistic, and who are at risk of admission, or who are admitted to a mental health or learning disability hospital, the use of care (education) and treatment reviews is an essential person-centred process. It aims to ensure system partners are working with individuals and families to provide the right care, education, and treatment that, wherever possible, avoids the need for an admission to a specialist mental health or learning disability hospital. Where an admission is essential, it provides the opportunity to review and ensure care and treatment is effective and discharge as soon as possible is supported.
C(E)TRs bring together those responsible for commissioning and procuring services. This includes: the responsible health commissioner from the provider collaborative or integrated care system; consultants; responsible clinicians; nurses; social workers; therapists; education commissioners and providers; and other health, education and social care professionals with independent clinical opinion; and the lived experience of people and families from diverse communities with learning disabilities or autism.
The aim of the C(E)TR is to bring a person-centred and individualised approach to ensuring that the care (education) and treatment and differing support needs of the person and their families are met, and that barriers to progress and / or discharge are challenged and overcome.
The Learning Disability and Autism programme are developing joint national DSR and C(E)TR guidance which is due for publication in Autumn 2022.
Keyworking
The NHS LTP includes a commitment that ‘by 2023/24 children and young people with a learning disability and/or who are autistic with the most complex needs will have a designated keyworker’, initially for those CYP who are identified as at risk of admission on the DSR or who are inpatients. Keyworking is our programme response to this LTP commitment.
Keyworkers work with young people, families and services to avoid unnecessary admissions to hospital and to facilitate timely discharge with the right support in place.
Keyworking is not a single defined role, but a service delivering the keyworking functions. This may be hosted by a health, local authority or third sector organisation shaped to fit well into the local system.
Young people and their families are allocated a keyworker via the Dynamic Support Register. Keyworkers work with the young person and their family to make sure they are fully involved in their plans; are listened to and informed; plans are personalised; and they have the support they need at the right time, in a co-ordinated way. Keyworkers work across local services and organisations to facilitate the integration of support and the implementation of care Education and treatment review recommendations.
More information regarding the development and roll out of keyworking is available on the NHS England website.
Learning disability liaison nurses
The ‘All-England Plan for Learning Disability Nursing’ by NHS England and Health Education England (2020) highlighted the important role of liaison learning disability nurses in the acute setting. Colleagues in this role provide ‘additional support before, during and at the point of discharge for people with learning disabilities and their family, and education and support for health professionals in acute care’. (Brown, M (2020). Learning disability liaison nurses: the provision of compassionate, person-centred care for people with learning disabilities accessing acute hospital care. Nursing Standard. 35, 10, 90-94).
They work to support the needs of people with a learning disability and/or autistic people, family carers and staff to ensure equitable access to healthcare. There are large education, co-ordination and listening elements to the role to ensure that reasonable adjustments are person-centred and conveyed to those who can implement these.
Element 5: Access to training and education
We recognise that the paediatric workforce may require additional training to ensure they have the skills to support CYP with acute mental health needs requiring treatment within a paediatric setting. (When we refer to the paediatric workforce, we mean wider health and care professionals that may include nursing; allied health professionals; paediatricians; psychologists; and health care assistants, etc). Providers should consider the implementation of a range of training and education to support their teams, which may include:
- short e-learning training and educational videos
- in person training days
- simulation training
- peer and multidisciplinary team (MDT) shadowing
- MDT support.
In Summer 2022, we launched a co-created single digital platform in partnership with HEE and e-Learning for Health (eLfH) to host peer-reviewed resources and training modules to support staff. Resources on the platform aim to improve the skills and confidence of the workforce to safely care for children who have mental health needs, including those with additional needs, such as a learning disability or autistic children, in an acute paediatric setting. There are also over 400 other e-learning programmes hosted by HEE for health and social care staff on the wider website. The platform continues to be enhanced through feedback and further engagement.
Quick reference guide to mental health and learning disability and autism training and education which may be relevant to those in acute settings
This platform hosts peer-reviewed resources and training modules to support staff. Resources on the platform aim to improve the skills and confidence of the workforce to safely care for children who have mental health needs – including those with additional needs, such as a learning disability or autism – in an acute paediatric setting. There are also over 400 other e-learning programmes hosted by HEE for health and social care staff on the wider website.
Training: Healthy Teen Minds
Face-to-face CYPMH distress training for acute staff now going virtual, funded by HEE. One hour online compassionate training for all staff free online on their website.
Crisis tools
Hear directly from young people who have experienced mental health crisis, and learn how to better support them in a tough moment. These resources aim to build an individual’s confidence to have effective conversations and provide personalised support to a young person in a mental crisis. Also includes specific learning guides co-designed and delivered by young Black men.
HEE has commissioned Healthy Teen Minds to develop a resource to support those working with young people in crisis to develop confidence in providing the best care for young people from LGBTQ+ communities. This will be available on the Crisis Tools website in March 2023.
We Can Talk
Co-designed and co-delivered project working with over 50 acute and MH hospitals to train more than 4,000 staff to transform the experience of young people and hospital staff around managing children and young people with mental health needs. Particularly aimed at supporting those from acute settings working with young people in crisis.
Training: Medical emergencies in eating disorders
The Royal College of Psychiatrists (RCPsych) has launched new guidance for all frontline staff on how to respond to medical emergencies in eating disorders. This replaces the Junior management of really sick patients with anorexia nervosa guidance and will enable paediatricians and child health professionals to identify children and young people with eating disorders needing urgent care earlier.
Training: MindEd
A free educational resource covering numerous topics regarding CYP, adults and older people’s mental health.
Training: MindEd hub for professionals, MindEd For Families
Recently launched ‘Tips for children and young people’s feeding and eating disorders’ aimed at professionals working across health and care settings. The five tops tips include:
- what to be aware of
- what to look out for
- what medical investigations
- what to do
- feeding development and issues in infants aged 0-2 years
Training: Oliver McGowan mandatory training in learning disability and autism
Seeks to ensure staff working in health and social care receive learning disability and autism training, at the right level for their role. They will have a better understanding of people’s needs, resulting in better services and improved health and wellbeing outcomes.
Training: Paediatric critical care in practice e-learning eating disorder module
Mental health module on eating disorders via an e-learning platform.
Training: Youth mental health first aid
Two-day course offering delegates the skills to be mental health first aiders and a deeper understanding of what mental health is and what factors can affect wellbeing. The course teaches practical skills to spot the signs of mental illness and confers the confidence to step in and support a person who needs assistance.
Training BEAT Beyond the Symptoms
Beyond the Symptoms runs over either one daylong or two half-day online sessions. The sessions are CPD-accredited interactive training, which allow staff to practice key skills for supporting patients with eating disorders under the guidance of clinicians who are experienced in the field, and give staff the opportunity to reflect on their own work.
Element 6: Innovative practice
NHSE CYP Mental Health and CYP Transformation Programme Teams jointly released £6m in 2022/23 to enable systems to enhance integration opportunities and test service innovations suggested by our programme’s Task and Finish Group. This included developing a CYP mental health/physical health clinical lead role, in line with recommendations from The Royal Collage of Paediatrics and Child Health and the National Confidential Enquiry into Patient Outcome and Death.
The information below summarises service and workforce innovations being tested. We plan for learning to be gathered during 2022/23 and shared in an updated version of this framework. Case studies have also been shared in annex 2 to highlight work already happening across the system.
- Place of sanctuary
To provide a safe space alternative to a health-based place of safety for CYP whilst health and social assessments can be undertaken. - Liaison team
By skill sharing within the paediatric and mental health workforce, improving early support for CYP with physical health or mental health needs. - CYPMH Decision Unit
Triaging CYP with mental health needs away from the A&E environment to support de-escalation and assessment. - CYP mental health/physical health lead role
Ensuring there is designated time within each paediatric unit to champion the change needed to support the paediatric workforce in caring for these CYP, as well as linking in across the system.
1. Diversion: Place of sanctuary
Function
- To provide a safe space alternative to a health-based Place of Safety for CYP whilst health and social care assessments can be undertaken.
- May provide immediate support for CYP in crisis whilst awaiting mental health assessments, alongside health and social care assessments.
- May be used as a setting for de-escalation or where there may be a safeguarding concern but CYP do not meet statutory thresholds.
Benefits
- Supports strong relationships with local authority funded social services.
- Diversion from traditional paediatric admission, so could reduce admission numbers.
- Improved patient experience as an alternative to traditional A&E.
Key available evidence
- This is a relatively new concept with published literature focuses mainly on ‘health-based places of safety’ (HBPOS).
- Has been applied in several regions across England.
- Ealing has adopted an intensive community intervention programme for CYP with learning disability and autism.
Published case studies
- Cambridgeshire & Peterborough Mental Health Crisis First Response Service & Sanctuaries
- The CYP Haven – Guildford – Surrey & Borders Partnership NHS Foundation Trust
Dependencies and potential challenges
- The setting may vary and requires further exploration.
- Service model clarity would be key to differentiate between HBPOS and Place of Sanctuary.
- Local integration with interdependent services would be key.
Assessment: Paediatric Mental Health Liaison team (or similar)
Function
- A paediatric mental health liaison team would look to offer 24/7 access to CYP who present in acute care and require immediate support.
- These teams would support the paediatric workforce to respond to the mental needs of CYP in acute settings and may also offer brief interventions while CYP are on a paediatric ward.
- A dedicated comprehensive paediatric mental health liaison team would be multi-disciplinary but where this isn’t possible hybrid models have been seen as effective, for example upskilling adult liaison teams to also support CYP over 16.
Benefits
- Improved integration and culture between mental health and physical health services.
- Potential diversion from inpatient mental health admission.
- CYP and families receive timely response and support.
- With improved integration and relationships, paediatric workforce (ie paediatrician or nurse specialist) may also undertake shifts within an inpatient mental health setting to upskill staff around physical health management (ie wound care), potentially preventing admissions to acute settings
Published case studies
- Brighton: up to 18 years old
- King’s College, London (SLAM): all ages
- Tower Hamlets: 24/7, over 16 (under 16 out-of-hours)
- Sheffield: over 16 years old
- North Staffordshire Combined Healthcare NHS Trust
Key available evidence
- Several peer-reviewed case studies show promise in reducing admissions and waiting times to access appropriate care.
- Established body of research suggesting liaison mental health services are cost effective and generate savings. Mainly related, however, to reduction in the length of stay of older adults admitted to general hospital wards, many of whom have significant mental health needs linked to dementia, depression or anxiety (Wood and Wand, 2014).
Dependencies and potential challenges
- Further testing and research would need to be done to explore options for hybrid models, where fully funded comprehensive paediatric mental health liaison team are not feasible due to demand or resources.
- Workforce models vary dramatically.
- Culture shift required, which could be supported by local service level agreements.
- As part of the commitments in the Long Term Plan, by 2023/24 CYP crisis services should be comprehensive and this includes Function 3: Crisis assessment and brief response within the emergency department and in community settings, with CYP offered brief interventions 24/7. Paediatric mental health liaison teams could fall into this category and local systems should be considering how a comprehensive paediatric mental health liaison team would fit within their local crisis response model.
Assessment: CYPMH Decision Unit
Function
- Triaging CYP with mental health needs away from the A&E environment in a dedicated space.
- Providing an assessment area/ward within acute hospitals that provides a calming atmosphere away from A&E for the assessment, and potentially the development of treatment plans for CYP with mental health needs. Resourced with staff who are skilled in CYPMH.
Benefits
- Potential reduction in traditional paediatric admissions.
- Environment supports de-escalation.
- Improved patient experience.
- Opportunity to work with MH team to develop/review care package.
Key available evidence
- A recent national survey of psychiatric decision units in England identified six in existence, all of varying configuration; further research into their efficacy is required.
- The Lotus Assessment Suite in SW London and St George’s is currently enrolled in a formal evaluation process; results are expected within the next year (purportedly the first evaluation of psychiatric decision units in England).
- No studies were identified that explicitly investigated the impact on CYP.
Published case studies
Dependencies and potential challenges
- Consideration needed as to where these might fit in the care pathway.
- Concern they may not be suitable environments if multiple CYP wait there for extensive periods.
- CYPMH Decision Units require estate which isn’t always available in acute hospitals.
- Workforce; training and availability could impact on the ability to roll these out.
CYP mental health / physical health lead role
- As recommended by RCPCH, we propose ensuring there is designated time within each paediatric unit to champion the change needed to support the paediatric workforce in caring for these CYP, as well as linking in across the system.
- This role is not intended to provide a greater share of the clinical care for CYP with mental health needs, rather it aims to empower colleagues to feel competent and supported.
- We are establishing a ‘learning collaborative’ for colleagues in these roles to provide a space for peer support and gathering of learning.
The role
- A children and young people’s mental/physical health lead role established in each provider that admits paediatric patients (1 PA per week will be allocated to clinical leads).
Eligibility
- Any senior clinician who can admit CYP to a paediatric ward and holds clinical responsibility for paediatric inpatients/outpatients.
- Likely a paediatrician / senior paediatric nurse / senior paediatric AHP.
Function
The role will have four key functions:
- to build team confidence and morale across the department
- encourage uptake of training
- facilitate joint working across mental health and physical health trusts and clinical colleagues
- provide leadership and link into trust governance structures.
Annex 1: Sensory friendly pilots
Commissioned pilots
In 2021, NHSE has commissioned two pilot sites to develop sensory friendly acute paediatric environments. These projects are due for completion in 2022.
One of the projects in Alder Hey, North West England aimed to:
- Support clinical and non-clinical staff working within Alder Hey to understand children and young peoples’ sensory needs.
- Map the journeys children, young people and families/carers often take using ‘walk throughs’, for example through the main hospital atrium, to outpatient settings or to wards.
- Improve the experience for children, young people and families/carers through every part of their journey.
- Improve how children and young peoples’ needs are supported through person-centred pathways and a more flexible environment.
Phase 1 of the project, “the listening phase”, saw the project team ask children and young people, families and carers and staff their views to help make Alder Hey hospital a better place to be for children and young people with sensory processing challenges and sensory impairment.
The pilot phase sees key staff coming together to contribute to the planning and delivery of solutions in response to the listening phase. Work will include:
- Adaptations to the environment and procurement of possible equipment.
- Live training for staff, including: outpatients, emergency department, learning disability and autism champions, play specialists and others.
- An offer of an e-learning module to all staff.
- An animation voiced by children and young people from Alder Hey youth forum and developed by NDTi to bring to life the experience of sensory challenges in the hospital setting.
This pilot is due for completion and evaluation in Autumn 22. We plan to refresh our framework to incorporate this learning in 2023/24.
Annex 2: Innovation case studies
Crisis and Enhanced Treatment Team pilot
Lincolnshire Partnership NHS Foundation Trust and East Midlands Provider Collaborative created a joint crisis and enhanced treatment team to prevent CYP hospital admissions. The impact of the pilot has seen a 68% reduction in all bed type admissions.
What was the issue?
- Inpatient beds had been closed at the trust. The aim was to operate a community service rather than an inpatient one.
- The aim was to provide an intense enhanced treatment package as an alternative to inpatient CAMHS, with the goal to keep children and young people (CYP) out of hospital
- If CYP were admitted to hospital, the aim was to ensure they were discharged quickly. There was already a substantive CAMHS crisis team in post.
What was the solution?
- Developed an ‘enhanced’ team to work alongside the current crisis team, to prevent hospital admissions.
- CYP at risk of admission provided with extra support from the MDT, including nursing, OT, clinical leads (band 7 nurses) and social worker.
- Specialised care plan for all CYP – crisis services are limited to 6 sessions, but enhanced treatment is not time limited. All CYP are RAG rated, red – daily contact, amber – 2-3 times a week, and green – ready to move into community CAMHS or discharge.
- If CYP are admitted to hospital, the combined team put in a package of care to repatriate the young person back into the community from the moment they are admitted into hospital. This also includes continued support for family and links with inpatient colleagues to enable quick and safe discharge.
Challenges
- Developing new ways of working, including virtual platforms, was challenging, alongside managing the merger of two teams.
- The pandemic meant that some team members had not met in person and caused some issues developing the new team, as well as impacting on staff wellbeing.
- Ensuring both teams merged digitally was challenging. Families fed back that they felt they were being referred internally and “swapping” teams but the intention was to prevent this.
- Issues initially obtaining enough psychiatric cover for both teams and ensuring out-of-hours cover.
Impact
- Admissions in 2020 to general adolescent units (GAU) have seen a 76% reduction to an average of less than 1 per month, compared to an average of 4 per month in 2018-19.
- In the 11 months since the introduction, there has been a 68% reduction in admissions to all bed types to an average of 1.6 per month.
- Monthly meetings with ICB (integrated care board) around inpatient length of stay and actions to discharge CYP reduced as a result of lower admissions.
- Decline in the median length of stay in GAU beds. There were concerns that not having an inpatient unit may increase the median length of stay for young people with less control in managing discharge. Average length of stay was 62 days (Jan 20 -Sep 20) compared to 167 in (Apr 18-Dec 19).
- Successful links made with paediatric services to develop joint care plans for CYP admitted to paediatric wards
Lessons learnt
- Ensure patients and families provide feedback to enhance services.
- Offer regular clinical supervision.
- Ensure care plans for children and young people are communicated effectively with families.
- Ensuring the now merged team is viewed both internally and externally as one team.
Find out more
Caroline Sanders, Service Manager Lincolnshire CAMHS: carolinesanders@nhs.net
Paediatric Psychosocial Service (PPS)
Royal Manchester Children’s Hospital created a Paediatric Psychosocial Service (PPS) to provide mental health support for CYP with physical health conditions. The service has been well received by patients and the Trust. The service continues to see high referrals and low DNA rates.
What was the issue?
- There was a need to provide psychological and mental health support for children with complex, long-standing and sometimes life-limiting physical health conditions.
- The previous service had been developed in a piecemeal fashion over several years and required a refresh.
- Prior to this, the psychological and mental health needs of children with a physical health condition often went unmet, as they did not meet referral criteria for local child and adolescent mental health services (CAMHS).
- The service aim and aspiration was to integrate mental health care into physical health teams.
What was the solution?
- Setting up a multidisciplinary team to include psychology, psychiatry, psychotherapy and other CAMHS professionals (eg occupational therapists, nurses). These clinicians developed links to specific paediatric specialties/conditions which helped build relationships and develop specialist knowledge.
- Staffing included: consultant clinical psychologist (head of service, clinical psychologists, child and adolescent psychiatrists, psychological therapists, psychotherapists, and administrative staff, alongside assistant psychologists, plus clinical psychology and psychiatry trainees.
- Ensure team was based in the acute setting (both in- and out-patients), and that cover was flexible across Monday to Friday, with out of hours support linked into the all-age liaison mental health service.
- The wider skill mix meant families and CYP could be offered a wide range of individual therapeutic approaches and highly specialised neuropsychological assessments.
Challenges
- The pandemic brought challenges: as a result of the changes in NHS financial management, the second phase of the development could not be progressed which left gaps in provision. Service accommodation was also lost, leaving pressures on both office and clinical space.
- Being based within CAMHS but working into the acute hospital means documenting in both mental health and acute hospital IT systems and therefore duplication for both clinical and admin staff.
- Recruitment to expanding the PPS further has proven more challenging in the current climate.
Impact
- The service has grown by more than 60% and been well received by patients, families, paediatric colleagues and the hospital’s senior leadership team.
- Patients and staff have reported that being reviewed by a member of the team during multidisciplinary clinics has been helpful as often families did not know about available resources.
- In 2021, the service completed 11,363 contacts across the whole year, this is 157 contacts more than capacity predicted.
- The service’s DNA rate was consistently low across the whole of the year, averaging at 4.4% for new appointments (10.3%: 2019-2020) and 5.7% for follow up appointments (7.3%: 2019-2020).
- The number of breaches of internal waiting time targets was also low. The total number of breaches – for both referral to first attended contact and for referral to second attended contact – was 37. This was similar to 2019-2020’s number of 36, despite an almost doubling of the number of appointments offered.
Lessons learnt
- As the team were employed by the acute trust and sat within the wider CAMHS Clinical Service Unit, this helped with integration and in breaking down organisational barriers.
- Ensuring good links with local CAMHS, meant that CYP who may require input from more than one service would have a seamless journey.
Find out more
Sarah Gaskell, Head of Paediatric Psychosocial Service at Royal Manchester Children’s Hospital: sarah.gaskell@mft.nhs.uk
CYP Learning Disabilities: Intensive Therapeutic and Short Breaks Service (ITSBS)
Funded by Ealing Local Authority, a multi-agency Intensive Therapeutic and Short Breaks Service (ITSBS) was created to prevent unnecessary residential care or inpatient admissions and enable CYP with LD to remain in their family/local community. Positive feedback and outcomes have been received around the service.
What was the issue?
- There is a need to provide intensive community support to young people with learning disabilities or autistic young people, who are at risk of inpatient admission or residential care/home breakdown
- Evidence continues to show autistic CYP and those with intellectual disabilities continue to be inappropriately admitted to mental health hospitals.
What was the solution?
- Create a collaboration between CAMHS-LD clinical psychology, social care and short breaks services for CYP with disabilities. This took the form of a multi-agency collaboration based within Ealing services for children with additional needs (ESCAN).
- Aim of the collaboration would be to provide intensive clinical psychology and social care input to the young person, family and frontline workers, including additional/intensive short breaks as needed.
- Current model is additional short breaks in the home (hours vary) for as long as required.
- All CYP would have an allocated social worker in the Ealing children with disabilities team; referrals into the service would need to be made by social worker or CAMHS-LD clinician.
- All CYP referred have a diagnosis of LD or ASD and are presenting with significant mental health needs or challenging behaviour at home and in other settings.
Challenges
- Weaning some people off intensive support/being supportive, while not empowering parents/carers.
- Finding good carers; having to work with multiple care agencies.
- Workload: managing crises, risk, and a large network.
- Meeting the needs of all family members and the network.
- Carer turnover and school placement breakdown.
Impact
- The service has been well received by other agencies, CYP and their families, with positive feedback on the multi-agency approach.
- Cost effective alternative to residential care: of the 43 CYP offered ITSBS, only five are in residential placements (Oct 2008 – March 2019).
- Good outcomes for many young people and families.
- Connection to a CAMHS-LD team for support, training, sharing out the work, training/recruitment, and for step up/step down model.
Lessons learnt
- Local infrastructure will determine how effective any intensive support service is, as well as how you are best to design/structure it. Any intensive services needs to be well linked to existing CAMHS and social care teams and pathways.
- Having a multi-agency working approach ensures links with key people who can make decisions/influence support.
Find out more
Dr Catherine Sholl, Autism and Intellectual Disabilities Intensive Intervention Team (AID-IIT), SLAM NHS Foundation Trust: Catherine.sholl@slam.nhs.uk
Dr Caroline Barber, Ealing Child & Adolescent Mental Health Service for Learning Disabilities (CAMHS-LD), West London NHS Trust: caroline.barber1@nhs.net

