Summary
Clinical decision support (CDS) systems are digital tools that can support clinicians to make more equitable, evidence-based decisions. They can be used across care settings, specialties and pathways to improve healthcare delivery and reduce errors.
Transformation of healthcare services with CDS requires consideration of several critical success factors – encapsulated by the six Is: inclusive, intelligent, interpretable, integrated, impactful, interoperable. Furthermore, there are five core principles for CDS design: providing the right information, to the right person, in the right format, through the right channel, at the right time. Local teams can maximise their likelihood of successful CDS implementation through early consideration of key elements including strategic alignment, addressing workforce issues, barrier identification and ensuring interoperability.
This guide sets the vision for CDS uptake across the NHS in England, highlighting its potential to improve the quality of care, outcomes and safety. It assimilates salient points from the literature and shares best practices to guide digital and clinical leaders at local and regional level on the implementation of CDS. Critically, it focuses on the role of CDS in improving clinical safety and designing problem-orientated solutions that achieve intended benefits. It suggests key actions that digital and clinical leaders should take as a part of their digital transformation plans, including developing multidisciplinary teams, engaging the workforce and avoiding unintended consequences.
Introduction
Clinical practice is increasingly complex with a growing body of evidence-based guidelines. Clinical decision support (CDS) systems promote best practice by supporting clinicians with the right information at the time of decision-making. They have been shown to enhance the quality of decision-making, reduce errors and unwarranted variation, as well as support shared decision-making (Kwan et al, 2020). CDS systems can also be applied across different care settings using a combination of clinical tools, technologies, information resources and guidance (Greenes, 2011).
CDS integrates population-based evidence with the characteristics of individual people to provide situation and patient-specific recommendations and support clinical decision-making. Tools range from those such as BMJ Best Practice (which provides accessible, step-by-step, evidence-based guidance), to those fully integrated with electronic health records (EHRs) and other digitised clinical workflows.
Healthcare data has accumulated over the last two decades and there has been a leap in computing power. The use of CDS systems represents an opportunity to harness the knowledge gained from this data by applying statistical methods to better understand and predict clinical decisions. Increasingly, clinical data is routinely captured through EHRs, allowing CDS systems to apply evidence-based and population-level insights to an individual patient’s record and provide structured guidance to support personalised decision-making. CDS systems are now one of the primary markers of digitally mature health services (Orenstein et al, 2019). Many clinical staff already use them in their routine practice: as clinical calculators, alerts, automated order sets or links to reference or educational materials within EHRs.
However, despite research suggesting their effectiveness, the uptake of CDS systems remains inconsistent and there are many barriers to widespread adoption. Used in the wrong way and implemented without consideration of the context and all stakeholders, CDS systems can disrupt clinical workflows and have unintended consequences such as alert fatigue. Effective implementation requires alignment of workflows, technology and end users, achieved through co-design and collaborative multidisciplinary projects (Sutton et al, 2020).
Digital leaders in organisations across all levels of maturity have a key responsibility for frontline digitisation. This implementation guide promotes a shared understanding of CDS systems in health and social care and supports digital and clinical leaders in implementing CDS as part of their digital transformation journey. It describes potential benefits and ways to overcome barriers. This guide also summarises relevant evidence and showcases examples of best practice.
Key considerations
In the rapidly evolving landscape of healthcare, the collaboration between digital and clinical leaders holds immense potential to transform patient care. The NHS Long Term Plan identifies mainstreaming of digitally enabled care across the NHS as a key priority. CDS systems are an invaluable tool to improve clinical outcomes and streamline processes. However, the successful implementation of CDS requires more than just technological solutions. Digital and clinical leaders bear a significant responsibility for carefully considering the implementation approach. By carefully addressing user needs, clinical workflows and patient safety, they can ensure CDS implementation is seamless, efficient and ultimately improves patient outcomes.
There is a diverse range of CDS system type and functionality, and tools can be deployed across a broad range of clinical settings. The critical first step involves establishing whether a CDS system is the appropriate intervention to achieve the intended clinical benefits. Each use case should therefore be validated in its specific context and type, with consideration of the significant academic evidence base for CDS.
Both technical and behavioural change are required for successful implementation of new technology (Greenhalgh et al, 2017). The mantra of digital transformation is technology, people and processes, so the following key elements should be considered for all CDS implementations.
Establishing the right multidisciplinary team
In addition to the digital and technical team, clinical leadership is essential to ensure decisions around design, procurement and implementation focus on clinical impact and patient benefit.
A multidisciplinary leadership team with senior organisational mandate should be established with the involvement of a designated chief clinical information officer or chief nursing information officer. Patient or citizen representatives should also be considered to identify priorities from a service-user perspective. Clinical safety officers and patient safety experts should be involved from the start to mitigate any risk of CDS systems resulting in negative outcomes or experiences.
Defining the problem
An organisation will need to establish existing technological, cultural, workforce and governance capabilities, to shape expectations of how CDS can be introduced and highlight where investment is required to maximise the potential of digital interventions.
Technology can rapidly analyse data and present actionable insights to support clinical decision-making. However, this only works if the CDS system ‘asks’ a specific and well-defined question. Thus, understanding current workflows and local policy to define the impact of CDS systems is critical.
A design-led approach can be used to define a CDS use case. This starts with gaining insights into the rate, severity and causes of the clinical problem in question from those closest to the clinical situation, the end users. This includes considering the wider change management, education and training that may be required for successful implementation, as well as exploring alternatives to CDS. Through this process there is an opportunity to reflect on current workflows and redefine ways of working if required. This needs to be an iterative process and through end-user input a solution-free problem definition should be agreed and documented to guide design of the preferred decision support solution.
Clinical safety
Clinical safety needs to be considered from the start of any project to ensure all potential hazards are adequately identified and mitigated.
Any health IT system that has the potential to impact on patient safety must comply with digital clinical safety standards DCB0129 and DCB0160. These standards place specific responsibilities on both the system manufacturer and the organisation using it, including identifying and listing potential risks on a hazard log and mitigating their impact. This helps to build the safety case for the product, which needs to be signed off by a clinical safety officer, and a framework for CDS governance.
Some CDS systems may also be classed as medical devices and must satisfy the medical device regulations set out by the Medicines and Healthcare products Regulatory Agency (MHRA). These should be considered early and expert advice sought to navigate this process as necessary.
Integration with existing systems
Information should be interoperable across care settings, to present a ‘single source of truth’ to clinicians. Poor integration with existing IT systems and EHRs is a key barrier to CDS adoption (Sharma et al, 2021). CDS should be developed and implemented with interoperability at its core wherever feasible, ensuring that it is meaningfully integrated with other clinical tools and systems in a non-disruptive manner. This includes keeping up to date with data standards in line with national NHS strategy. Importantly, CDS should be considered even in settings with limited digital capabilities, with implementation done in partnership with quality and safety leads.
Evaluation and improvements
A continuous cycle of performance measurement, iteration and sustained improvements can support the longevity of CDS, as illustrated by Learning Healthcare Systems. The Healthcare Quality Improvement Partnership describes a way to approach this in its guide to quality improvement tools.
One advantage of CDS systems is the electronic capture of performance data; this self-generated data can be used to trigger reviews and instigate improvements in the CDS tool and underlying algorithm over time. CDS systems must also be updated as new clinical knowledge and evidence emerges, or guidelines are released.
External factors may also impact on the relevance and use of CDS systems in clinical pathways. It is important to monitor whether a CDS system and the wording of its advice remain relevant as new treatments, investigations or public health interventions change the care landscape. As NHS providers continue their digital transformation journey, they should seize the opportunity to implement CDS into their clinical governance frameworks and in doing so adopt a learning approach to health systems.
Success factors
To enable systems to support staff to improve the quality of care and deliver on their potential to transform healthcare services, the 5 Rights and 6 i’s need to be considered. The 5 Right’s for a CDS system to effectively support clinical decision-making are:
Right information: evidence or guideline based CDS that incorporates stakeholder inputs and aligns with current improvement initiatives.
Right person: CDS must meet the specific needs of everyone in the multidisciplinary clinical team. Users should be aware of the purpose and limitations of the CDS, and how to report issues with its advice.
Right format: CDS formats must present information to clinicians in a manner that complements workflows; for example, best practice alert, visual dashboard, smart order set, customised referral. Those writing CDS advice should be aware of good practice in risk communication (for example, use 1 in 100 rather than 1% risk) and avoid interrupting clinical tasks unless there is an immediate risk of serious error.
Right channel: User experience needs to be considered. CDS should focus on the context of use, to ensure presented information does not disrupt workflows. Where possible and appropriate, it should be integrated within the primary EHR system.
Right time: CDS must be integrated and seamless within the clinical workflow. CDS should operate across different care settings.
Furthermore, effective design and implementation of CDS systems is illustrated by the 6i model.
Figure 1: The 6i model for CDS systems
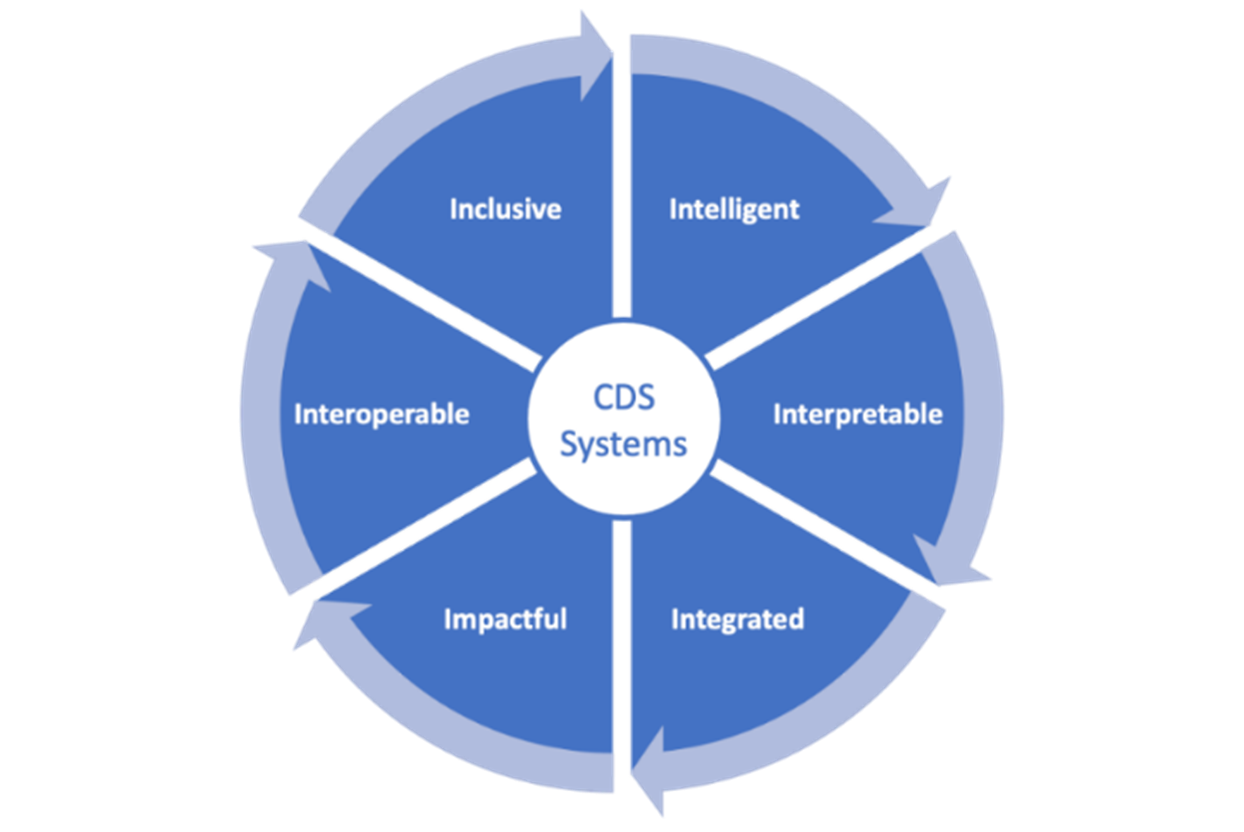
CDS Programme, NHS England (based, with permission, on previous work by Prof Sir Munir Pirmohamed, University of Liverpool)
Intelligent: CDS systems need to be evidence based and address real-world clinical decisions that would benefit from best practice support. Self-generated data can be used to guide iterative improvement.
Interpretable: CDS systems need to consider the healthcare professional’s knowledge of the topic, use clear and unambiguous content, and demonstrate validity and reliability of recommendations by linking to relevant explanations or evidence.
Integrated: CDS systems need to be designed to complement workflows. Integration with clinical systems can increase impact by embedding decision support in clinical workflows.
Impactful: CDS systems need to consider the experience of users, improve productivity and outcomes, and be clinically safe with mitigations made to reduce potential risks.
Interoperable: CDS systems need to interpret clinical data from systems to minimise manual data entry and present result data within relevant clinical systems by using open application programming interfaces (API) whenever possible. Where a relevant computable knowledge library is available, the CDS system should be configured to import high quality knowledge objects coded using global knowledge standards (Wyatt and Scott, 2020).
Inclusive: CDS systems need to consider a broad range of end users, be based on trusted clinical data that is representative of the target population and help minimise health inequities by standardising care.
Models such as the Plan, Do, Study, Act (PDSA) cycle can be used for iterative improvement.
Common barriers
As importantly as considering the success factors, teams need to understand the barriers to CDS system implementation and plan mitigation strategies in advance.
Managing alert fatigue
Many CDS systems provide clinicians with information at specific timepoints to support their decision-making. However, if clinicians are presented with inappropriate alerts or an overwhelming number of alerts they can suffer alert fatigue (Khalifa and Zabani, 2016). If an appropriate ‘threshold’ of sensitivity and sensitivity is not set, up to 95% of alerts are inconsequential, and sometimes clinicians will distrust, disagree with or ignore them (Ash et al, 2007). The CDS system design needs to ensure that only clinically meaningful recommendations are presented. Alerts should appear at the right time and provide context-relevant information that influences clinical decision-making, in a practical, standardised format.
If not managed appropriately, there is a risk the CDS system has unintended consequences, most commonly manifest as ‘over-alerting’. The context in which a CDS system is being implemented is an important consideration; they form a part of wider care pathways in a complex adaptive environment. CDS systems that trigger out of context and do not consider multiple patient factors will likely lead to inappropriate alerts, and with this users can lose confidence in the alerts and thus not engage with them even when they are relevant (Wasylewicz et al, 2018).
Workforce engagement
CDS adoption is dependent on preparation and engagement of the workforce (Greenhalgh et al, 2017). It is vital that the workforce feel they jointly own and have co-designed the CDS system and its implementation. Workforce awareness of what CDS systems are and their intended benefits can help engage and incentivise staff to be a part of the process.
Planning should seek early senior endorsement and build trust among clinicians with an emphasis on transparency and bidirectional communication. Consulting clinicians during development ensures CDS systems are designed to meet the end-user’s needs and are developed for the right level of complexity and skill, and encourages frontline buy-in during implementation. Senior clinicians can be engaged to champion the development and implementation process, facilitating conversation across different levels.
Furthermore, understanding how to support the workforce is crucial, such as by providing the necessary training resources or protected time. Lack of digital literacy can inhibit engagement with CDS systems (Leslie et al, 2016). Planning teams should aspire to create an innovative culture and safe space where staff are encouraged to raise problems and supported to solve them.
Governance and quality assurance
Continuous improvement of the CDS system ensures it remains clinically relevant and operationally stable. This can be achieved by developing a systematic approach to learning and improvement, and adopting an appropriate governance structure. Processes should be established to ensure ongoing review of content. Creating modular and standards-based infrastructure may also support this.
Governance should be emphasised across clinical and operational levels. CDS should be meaningfully embedded within an organisation’s clinical governance system. Clinical governance entails ensuring that recommendations, thresholds and algorithmic guidance are updated with consideration of performance data, outcome measures and change in evidence base, and are in line with local guidelines and national best practices. Operational governance includes ensuring that the systems, applications and databases that power the CDS system are updated in accordance with the latest standards. This should be clinically owned, with the involvement of senior stakeholders.
Examples of use
CDS systems are being used throughout the NHS to support care delivery across diverse levels of digital maturity and priorities. These common applications may be a useful starting point for local teams when considering CDS implementation. Teams should consider applicability within their local context, factoring in diversity between systems and tools.
Highlighting important patient information
Recognising deteriorating patients (Cambridge University Hospitals NHS Foundation Trust): CDS was used to generate an electronic alert when a patient’s clinical observations meet the sepsis criteria. A series of electronic prompts within the EHR guides clinicians through the actions and tests needed to diagnose sepsis. Within the system clinicians then select and order the most appropriate antibiotics to treat the source of the infection, with the system recommending the correct dose and frequency in accordance with the patient’s clinical status and in-built national medication guidance.
Developing a neonatal electronic patient record (EHR) for paediatric intensive care unit (Alder Hey Children’s NHS Foundation Trust): A bespoke EHR was developed for use in paediatric intensive care with in-built capabilities for clinical decision support. This alerts staff to important patient information, including allergies, escalation plans and safeguarding, and important clinical issues such as infection control or difficult intubation.
Electronic observations: Fluid balance and sepsis screening tool (North Tees and Hartlepool NHS Foundation Trust): After introducing an EHR with functionality to capture clinical information, North Tees introduced additional modules to capture electronic observations, including fluid balance, and sepsis screening tools. After input of observations, a visual rule flags whether a patient is at low, medium or high risk of clinical deterioration, prompting clinicians to escalate the case if necessary. Where a clinician completes a sepsis screening tool, the visual rule appears and prompts escalation and the start of treatment.
Medicines management
The benefits of implementing an EPMA system (Gateshead Health NHS Foundation Trust): Gateshead implemented an EPMA system with in-built CDS capabilities to facilitate safer prescribing, more efficient workflows and better data use for auditing. Various alerts, such as for allergies, have made prescribing safer with fewer adverse outcomes. The system also supports decision-making around prescribing the most cost-effective medication, reducing annual costs by £72,500.
Safer prescribing through CDS (North Tees and Hartlepool NHS Foundation Trust): An electronic prescribing and medicines administration (EPMA) system was rolled out to facilitate safer, more efficient prescribing. This includes alerts for drug contraindications and allergic reactions and interactions to reduce medication errors and provide guidance for inexperienced prescribers. Implementation was supported by clear multi-platform communication that made the agenda and progress visible across the trust, a multidisciplinary working group formed early in the planning process, and continuous engagement with stakeholders including the supplier, frontline clinicians and key decision-makers. A phased approach was taken to allow for continued development and issue resolution, and to ease the transition.
Increasing compliance with clinical pathway guidelines
Electronic observations (South Tyneside and Sunderland NHS Foundation Trust): Decision support was integrated into clinical documentation for several clinical pathways in an acute care setting. To promote best practice, clinicians are provided with pathway guidance and alerts are used to promote compliance. Furthermore, provision of decision support enables tracking to ensure patients are on the correct pathways.
Delirium and dementia electronic assessment (Salford Royal NHS Foundation Trust): Delirium is a poorly recognised and under-diagnosed clinical syndrome that can prolong admissions and worsen outcomes. To improve delirium assessment and management, an assessment tool and care plan was embedded in the EHR for patients identified as possibly having delirium. Staff are prompted to do an early assessment for delirium in newly admitted or confused patients. The number of identified cases has risen by 34% and the length of stay has reduced by 11%, saving an estimated £1.7 million in the first year.
Supporting and digitising clinical pathways
A digitised paediatric appendicectomy pathway (Alder Hey Children’s NHS Foundation Trust): CDS systems, e-messaging and performance dashboards were used to implement a digitised paediatric appendicitis pathway. The CDS tools have standardised the use of an in-built validated risk assessment tool, with alerts prompting consideration for next stages of care in the pathway. By making key information more prominent, transfers of care have also improved.
Remote monitoring of COVID-19 patients using a cloud-based digital solution in primary and secondary care (NHSX in partnership with North West London COVID-19 ‘hot hubs’ and West Hertfordshire NHS Hospitals Trust): Remote monitoring supported local trusts and authorities to monitor COVID-19 positive patients in the community, high risk patients in self-isolation and those at high risk during the pandemic. This was implemented to provide escalated care clinics in primary care and ‘virtual hospitals’ in secondary care. The technology-enabled remote monitoring process allowed clinicians to rapidly identify clinically deteriorating patients and make reactive decisions based on the data presented to them, all while managing large numbers of acutely unwell patients. This increased clinical productivity, gave patients a better experience, and reduced unplanned and unnecessary admissions.
Developing and using electronic transfusion processes (Oxford University Hospitals NHS Foundation Trust): An end-to-end electronic transfusion process was implemented to reduce the risk of the wrong blood being transfused and the inappropriate use of blood. It uses barcoded patient wristbands and electronically controlled blood fridges and is integrated with the electronic patient record and laboratory system. Users are guided to complete certain processes to ensure safety and process completion, such as checking identification wristbands and printing labels. The electronic process has greatly improved the safety and efficacy of transfusion, with cost savings of £1.2 million in the last 4 years.
Predictive analytics
Management and supervision tool (MaST) (Mersey Care NHS Foundation Trust): Mersey Care developed a management and supervision tool that uses artificial intelligence (AI)-powered algorithms to analyse mental health data from multiple sources, and from this determine the likelihood of a patient accessing crisis services within the next 28 days. This insight supports decision-making based on patient needs and guides the grouping of patients into cohorts to enable their appropriate allocation to safe and effective care.
Keeping mothers and babies together (Royal Free London NHS Foundation Trust): Clinical Practice Groups created a CDS platform to provide standardised care pathways that reduce variation and improve delivered care. The platform identifies ‘at risk’ babies through clinical algorithms and allows them to be tracked through EPR for task prioritisation. As a result, clinicians are using a single, standardised pathway to provide enhanced postnatal care to vulnerable babies alongside their mothers, and admissions of term babies into the neonatal unit has reduced from 13% to 6%.
Personalised and precision medicine
Implementing pharmacogenomic-based prescribing in primary care (North West Genomic Service Alliance): Pharmacogenomics-based prescribing can improve the effectiveness of medications and reduce potential harm from adverse drug events. However, this requires in-context alerts integrated into existing prescribing workflows. The team are exploring the design of a pharmacogenomic service for the NHS in England by applying user-centred design and prototyping to establish real-world needs and requirements.
Risk stratifying elective surgical waiting lists using AI (Mersey and Cheshire Integrated Care System): By collaborating with an industry partner, Mersey and Cheshire ICS transformed its manual waitlisting process to an AI-driven dashboard. This allows granular risk stratification and prioritisation of patients at highest risk of deterioration.
- Recommended actions
To maximise the opportunities afforded by CDS, digital and healthcare leaders are encouraged to:
- review local digital transformation strategies to identify and incorporate opportunities for CDS-enhanced care provision, with emphasis on safety and quality issues
- understand existing CDS functionalities within their organisation(s)
- work with clinical leaders and service users to consider and agree CDS development, procurement and implementation priorities
- evaluate workforce engagement strategies, ensuring multi-stakeholder representation in discussions around CDS systems implementation
- consider how CDS systems can integrate with existing systems, designing implementation with interoperability at its core wherever feasible
- build communities of best practice, adopting a learning approach and sharing effective practices within and beyond local teams.
Glossary
- Clinical decision support (CDS): Electronic tools that apply knowledge systems which use two or more items of patient data to generate case-specific advice, to improve clinical decision-making.
- Electronic health record (EHR): A digitised version of a patient’s care record that makes data available instantly and securely to authorised users.
- Electronic prescribing and medicines administration (ePMA): An electronic system that allows health professionals to prescribe, administer and review medications for patients.
Application programming interface (API): A software intermediary that allows two applications to communicate and share data with one another.
Acknowledgements
We are grateful to the following organisations for their contributions to the implementation guide: Faculty of Clinical Informatics (FCI), Health Data Research UK, Health Education England (HEE), Mobilising Computable Biomedical Knowledge (MCBK), National Institute for Health and Care Excellence (NICE), National Knowledge and Decision Support programme, NHS Scotland.
And to individuals in the following organisations for their involvement in CDS workshops and expert calls: Alder Hey Children’s NHS Foundation Trust, Birmingham and Solihull NHS Mental Health NHS Foundation Trust, British Computer Society (BCS), Cambridge University Hospitals NHS Foundation Trust, The Christie NHS Foundation Trust, University of Edinburgh, First Databank (FDB), Great Ormond Street Hospital for Children NHS Foundation Trust, Hampshire Hospital NHS Foundation Trust, Health Foundation, Imperial College Healthcare NHS Trust, Intermountain Healthcare, Jönköping Region County, Sweden, Lancashire and South Cumbria NHS Foundation Trust, University of Manchester, Mersey Care NHS Foundation Trust, University of Michigan Department of Learning Health Sciences, NHS Horizons, Northumbria Healthcare NHS Foundation Trust, Nuffield Trust, Oxford University Hospitals NHS Foundation Trust, Royal Free London NHS Foundation Trust, Salford Royal NHS Foundation Trust, South Tyneside and Sunderland NHS Foundation Trust, South West Academic Health Science Network, Surrey and Sussex Healthcare NHS Trust, St Helens & Knowsley Teaching Hospitals NHS Trust, System C, UCL Partners, University College London Hospitals NHS Foundation Trust, University Hospitals Birmingham NHS Foundation Trust, West Suffolk NHS Foundation Trust.
References
- Ash JS, Sittig DF, Campbell EM, Guappone KP, Dykstra RH. Some unintended consequences of clinical decision support systems. AMIA Annu Symp Proc 2007: 26-30.
- Greenes RA, ed. Clinical decision support: the road ahead. Elsevier, 2007.
- Greenhalgh T, Wherton J, Papoutsi C, et al. Beyond adoption: A new framework for theorizing and evaluating ngronadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res 2017; 19(11): e367.
- Khalifa M, Zabani I. Improving utilization of clinical decision support systems by reducing alert fatigue: strategies and recommendations. Stud Health Technol Inform 2016; 226: 51-54.
- Kwan JL, Lo L, Ferguson J, et al. Computerised clinical decision support systems and absolute improvements in care: meta-analysis of controlled clinical trials. BMJ 2020; 370: m3216.
- Leslie SJ, Hartswood M, Meurig C, et al. Clinical decision support software for management of chronic heart failure: development and evaluation. Comput Biol Med 2006; 36(5): 495-506.
- Orenstein EW, Muthu N, Weitkamp AO, et al. Towards a maturity model for clinical decision support operations. Appl Clin Inform 2019; 10(5): 810-819.
- Sharma V, Ali I, van der Veer S, et al. Adoption of clinical risk prediction tools is limited by a lack of integration with electronic health records. BMJ Health & Care Informatics 2021;28:e100253.
- Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med 2020; 3: 17.
- Wasylewicz ATM, Scheepers-Hoeks AMJW. Clinical decision support systems. In: Kubben P, Dumontier M, Dekker A, eds. Fundamentals of clinical data science. Cham (CH): Springer; 2018.153-169.
- Wyatt J, Scott P. Computable knowledge is the enemy of disease. BMJ Health Care Inform 2020;27(2):e100200.
Resources
- NHS Long Term Plan (2019) – NHS England
- An overview of clinical decision support systems – Sutton et al (2020)
- BMJ Best Practice – The British Medical Journal
- Clinical risk management standards – NHS Digital
- Global digital exemplar blueprints – NHS England
- Regulating medical devices in the UK – MHRA
- Shared decision-making implementation checklist – NHS England
- A guide to quality improvement tools – Healthcare Quality Improvement Partnership
- Plan, Do, Study, Act cycles – Aqua
- Realising the potential of learning health systems – The Learning Healthcare Project
Publication reference: PRN00018

