Linking urgent community response (UCR) and technology enabled care (TEC) provision
There are over 200 technology enabled care (TEC) providers nationally, providing:
- Equipment such as pendant alarms and motion sensors and connection to 999 when the equipment if triggered;
- Responder services which will attend the location of triggered equipment.
Many local authorities commission TEC providers, but some provision is private. There is also variability in the size and footprint of provision; some is local to one place, whereas other TEC providers are national bodies. The TEC Services Association (TSA) Quality Standards Framework (QSF) is a United Kingdom Accreditation Service (UKAS) accredited scheme for TEC providers which aligns with the standards of a regulated service.
Ambulance services across the country receive around 2,600 calls every day from TEC providers, equating to around 3% of all calls. Redirecting a proportion of these calls into urgent community response (UCR) services can ease pressure on ambulance services, and most importantly, ensure people receive the rapid response they need to remain well, and in the place they call home.
The 2022 going further on our winter resilience plans guidance asked all ICBs to consider deploying QSF-certified TEC responder services to people who fall, as clinically appropriate, and suggested that onward referral shifted from a 999-first model, to one which referred direct into UCR.
Whilst a proportion of calls will always require an emergency response for life-saving treatment, some areas have already seen massive benefits in connecting their UCR services and TEC provision. Dudley has seen the number of ambulance callouts for injured fallers reduced by 85%, with an audit by North West Ambulance Service (NWAS) showing 68% of callouts remaining at home.
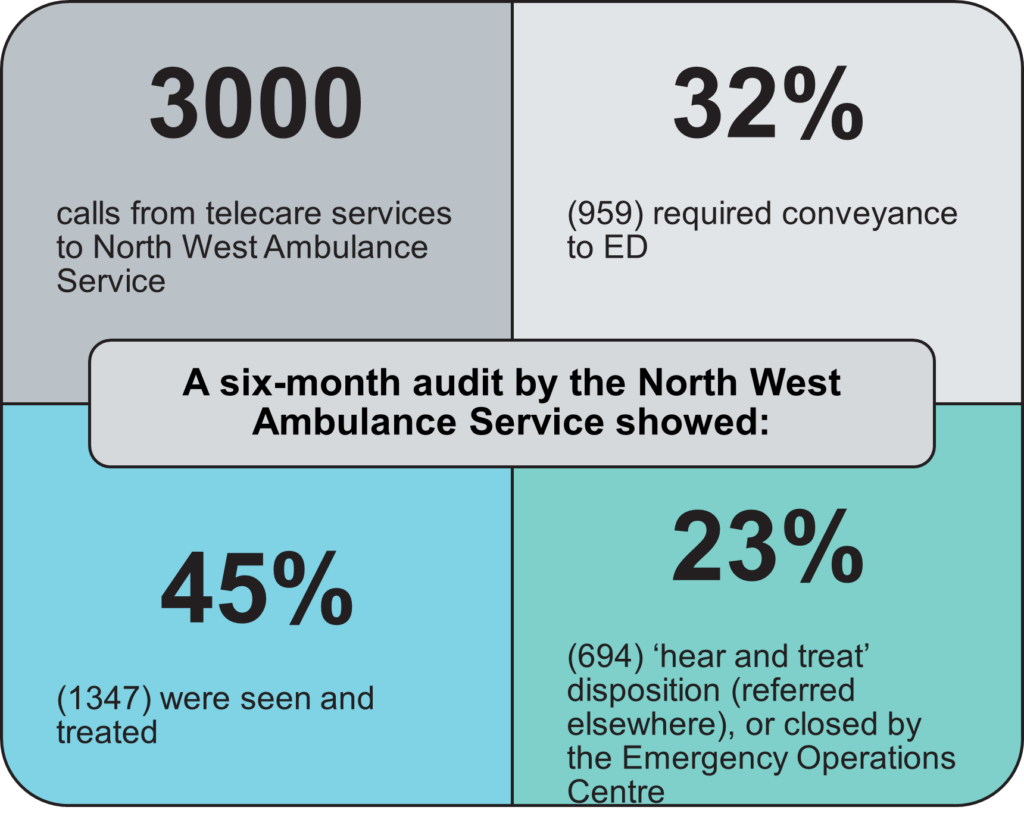
A six-month audit (October 2020 – April 2021) by the North West Ambulance Service showed: 3000 calls from telecare services to North West Ambulance Service, 32% (959) required conveyance to ED, 45% (1347) were seen and treated and 23% (694) ‘hear and treat’ disposition (referred elsewhere), or closed by the emergency operations centre.
Maturity indicators for UCR and TEC pathways
Indicators to self-assess the maturity of your local provision
5 ‘gold standard’ indicators for areas to work towards:
1. There are direct referral routes in place from locally operating Quality Standards Framework (QSF) -certified TEC responder services into the UCR service, which don’t rely on clinician-to-clinician referral.
2. Only activity which is inappropriate for UCR response is directed to 999, with responsibility being maintained by the TEC provider until this transfer of care occurs.
3. The UCR service has open lines of communication into its locally operating QSF-certified TEC responder services, which limit the amount of rejected referrals due to capacity limitations.
4. Training on appropriate referral reasons is available to local QSF-certified TEC responder services, with the UCR service having an ‘accept all’ approach to referrals from providers who’ve completed this training.
5. Induction and refresher training for TEC to UCR pathway is co-designed and co-delivered frequently, with at least quarterly plan-do-study-act (PDSA) approaches to understand the reason for and mitigate against future rejected referrals.
Guiding pathway principles
How to establish and maintain pathways from TEC providers into UCR
Identify and understand
Whether in operation already or in set-up stage, UCR services and their locally operating QSF-accredited TEC responder services should undertake a baseline assessment identifying the current pathway within their local area.
Identify:
Who your local TEC providers and UCR services are.
- Ensuring TEC providers are certified to TSA Quality Standards Framework.
- Establish point of contacts in both, and start to build relationships.
- Some TEC providers cover large footprints – it may be helpful to work across larger than place footprints to design the pathway.
What data is obtainable, using it to understand the size of the opportunity a pathway presents. Suggested data could include:
- the overall volume of calls, split by the amount currently passed to 999 / other services;
- the time of day calls are made;
- the acuity of the calls, and general reasons for calls (e.g., falls, generally unwell);
- geographical coverage of alarm users (and calls); and
- any health inequalities which might be exacerbated.
What existing arrangements and relationships are in place between TEC responder services and other local services:
- Such as falls services, in line with going further on our winter resilience plans and self-referral routes to falls response services, in line with 23/24 priorities and operational planning guidance.
- If not in place, then begin to develop
Understand:
What is already in place by undertaking a mapping exercise to determine:
- what UCR and Community/Falls Responder and Falls services are available locally, and the services they provide;
- their hours of operation (if not the standard 8am – 8pm, 7 days a week UCR offer) along with the hours they accept referral, and any ‘acceptance criteria’;
- capacity of the services to a) accept referrals from TEC providers and b) any training needs in both the UCR services and the TEC providers to ensure a safe, effective pathway; and
- how referrals are made to them, confirming they will take direct calls from locally operating QSF-certified TEC providers.
The gaps and opportunities to develop the offer of local responder services, if not in place.
Information governance barriers and how to overcome them such as information flow of patient data from TEC to UCR.
Opportunity to enhance or expand pathways, including exploring joint commissioning of services or alternative financial models,.
Cultural barriers, such as between clinicians and non-registered colleagues, working to identify how these can be overcome.
Develop and implement
Once the current pathway is identified, UCR services and their locally operating QSF-accredited TEC responder services should collaboratively start to develop and implement the referral routes and pathways.
Develop:
A project team to:
- Bring the right people together to further develop relationships including UCR, Responder Services and any relevant local commissioners.
- It’s suggested this is led by regional/place-based leadership to ensure scale of pathway.
- Determine the dedicated project resource needed to help establish the pathway and manage then project
- Develop and deliver a shared understanding and buy-in of what needs to be achieved
The pathway:
- Clarify the pathways already in place to connect these services, ensuring clear onward referral processes are in place.
- Develop a shared understanding of the services that are being connected.
- Understand any barriers to implementation, how to overcome them, and who can help.
- Determine use of the TEC Quality Decision Support Tool (DST), and the requirements for using DST.
- Develop process for direct referral including telephone numbers, a minimum information standard, referral acceptance criteria, etc. with the ambition of making referral straightforward and minimising rejections.
- Determine the training requirements of both the UCR and TEC workforce.
Training:
- Develop modules collaboratively so that each service understands how the other works, any standard operating procedures processes and communication requirements
- This should include a focus on integration and collaboration between providers, creating a “better together” culture
Service development indicators to measure success (examples below), which its suggested are collated by the UCR services:
- number and type of referrals from TEC providers
- time to respond from initial call
- outcome of response
- service user experience
- number of rejected referrals and reason
Requirements for NHS Service Finder:
- As a minimum, UCR services (and others identified as part of the mapping exercise) are represented on the Directory of Service (DoS), flagged for NHS Service Finder and accepting referrals from all health and social care providers, including TEC providers.
- Ensure NHS Service Finder / DoS is up to date including the hours referrals are accepted, clear instructions on how to access the service, clear inclusion and exclusion criteria (though this should be kept to a minimum in line with ‘accept all’ policy) and the geography the service covers.
Implement:
The pathway as agreed by the project team through the development stage, carrying out:
- Implementation of any phased approach etc.
- Ensuring referral routes are active and all staff are aware; and
- Any new software or systems are in place and tested.
Training:
- Deliver training to all the workforce on new processes and pathway including DST, where applicable;
- Ensuring all of the workforce are aware of relevant processes and pathways.
Measure and review
When appropriate, UCR services and their locally operating QSF-accredited TEC responder services should jointly measure the impact of the service, adopting a continuous improvement approach.
Measure:
The service development indicators (SDIs) set established in the development stage:
- Measure these SDIs on a regular basis;
- Provide updates to workforce on the progress of the SDIs; and
- Review the SDIs to add/remove any, at regular intervals.
The impact of the service on the patient:
- Through Patient Reported Outcome Measures (PROMs), Patient Reported Experience Measures (PREMs) and Clinical Outcome Measures (CLOMs).
Through submissions to the Community Services Data Set (CSDS):
- Currently TEC isn’t a standalone referral source, but this should be available shortly but could be supported through any local data collection.
Review:
Be explicit about the idea to be tested.
Undertake a plan, do, study, Act (PDSA) approach to constantly understand how the pathway can be refined and improved:
- Implement changes collaboratively.
Each stage of the implementation process:
- Ensure issues identified are resolved and improvements made.
- Highlight successes and learn from these.
Continual reviews should be undertaken:
- Ensuring sustainable improvements are being delivered.
- Lessons identified are implemented where appropriate.
Implement regular reviews of NHS Service Finder and Directory of Service:
- Ensure information provided is always up-to-date and accurate.
Case studies
Examples of gold standard pathways
Colchester
Overview:
- Telecare and an Urgent Community Response (UCR) team have been working together over the last year in a collaboration that’s helping to alleviate pressure on Ambulance Services in North Essex.
Outcome:
- The partnership has resulted in a rise in referrals between the two services. Crucially, the UCR takes referrals directly from the Ambulance Service and many are now passed on to Helpline 24/7.
- Between December 2022 and February 2023, it sent an average of 27 Ambulance Service referrals a month to Helpline 24/7 – helping to prevent hospital admissions and unnecessary 999 call outs.
Dudley
Overview
- The project involved the monitoring centre of Dudley Telecare who take the alarm calls. Their non-clinical operators then assess and refer to appropriate pathways. This includes using their TEC Responder Service and where necessary collaboration with the UCR team who would arrange a joint meet at the property
Outcome
- In the space of little more than a month, a collaboration between Dudley Telecare and Urgent Community Response teams has seen the number of ambulance callouts for injured fallers reduced by 85%.
- To date, all callouts alongside UCR teams have been reached within 45 minutes.
Lancaster
Overview
- TEC providers, Responder, UCR and Ambulance Services working together to ensure vulnerable people get the most appropriate support in the right place whilst reducing pressure on frontline services
Outcome
- Between January 2022 and February 2023, Progress responded to more than 13,000 falls-related calls of which 94% remained at home
- Plans are now in place to implement these new arrangements across the area covered by the Lancashire and South Cumbria ICB
Warrington
Overview
- Connecting TEC providers, UCR and Responder services together to develop blueprint for integrated services to ensure speedier response when someone is at home and in need of support.
Outcome
- Services are available 24/7 with attendance in usually less than 60 minutes on average reducing pressure on ambulance services.
- Outcomes are positive with 80% of people remaining at home following a visit.
Publication reference: PRN00806

