Action required
The Board is asked to note the information provided in this paper.
Background
1. The Darzi review highlighted that there have been differing interpretations of the roles of ICBs since their establishment in 2022 and that alongside the system leadership and commissioning roles they were set up with a range of delivery functions. The report concluded that responsibilities of ICBs needed to be clarified to provide more consistency and better enable the strategic objectives of redistributing resource and integrating care. Following this conclusion, the Secretary of State set out last November that ICBs would focus on being strategic commissioners.
2. In line with every ICB moving to focus on strategic commissioning, the NHS England Chief Executive wrote to NHS leaders on 1 April highlighting the critical role ICB will play in the future system architecture. However, alongside this given the financial context there was a necessity of all ICBs moving in Q3 2025/26 to the same level of efficiency in their administrative costs and that on average there would need reduce their costs by approximately 50%, spending no more than £18.76 per head of the ICS’s population. The letter undertook to issue at the end of the month a model to inform ICB redesign and support the development of plans to deliver the running cost reduction: the draft Model ICB Blueprint.
3. To deliver on this commitment NHSE rapidly convened a group of ICB leaders including clinical representatives to start to develop the Blueprint, the work was split into three areas, (i) defining a vision and future functions of ICBs (ii) Mapping functions and duties across the system, and (iii) managing safe transition
i) Defining the future vision as strategic commissioners
4. The draft Model ICB Blueprint affirms that ICBs are essential to the future success of the NHS, delivering the Government’s priorities. It commits to building the capabilities of ICBs and the strategic commissioning skills of their staff through a national commissioning development programme which be scoped over the summer.
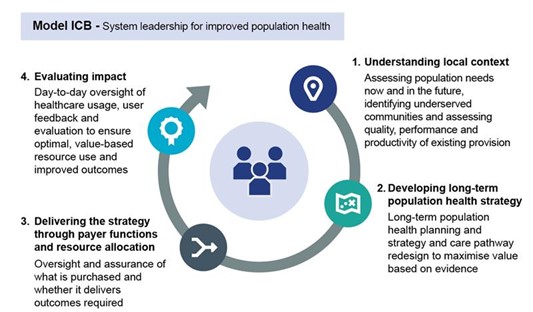
5. The Blueprint makes clear that as strategic commissioners, ICBs will focus on providing system leadership for population health, setting evidence based and long-term population heath strategy and working as healthcare payers to deliver this, maximising the value that can be created from available resources.
ii) Mapping functions to determine how functions are delivered across the system
6. In having determined the core role and functions of ICBs in the future, the working group considered how ICB current functions should be mapped to ICB and across the system going forward. The Blueprint sets the expectation that ICBs will:
- grow those capabilities and functions necessary for them to undertake their role as strategic commissioners successfully
- selectively retain and adapt the governance and management functions that enable delivery of strategic commissioning e.g. quality management, board & corporate governance, clinical governance and core operations
- review for transfer to other parties, those functions that are not core to strategic commissioning and may be better undertaken by others in future.
7. For the areas which will be reviewed for transfer, there is recognition that further work and engagement is required. There is an acknowledgment that, even with this flexibility, transferring functions requires careful consideration of interdependencies with other functions and the readiness of partner organisations to receive the function. Responsibility for some of these functions may ultimately need comprehensive resolution through legislative change.
8. NHS England with ICBs is engaging partners to work through these issues, including setting up joint working groups with the Local Government Association to consider Continuing Healthcare, Special Educational Needs and Disability (SEND) and Safeguarding. In addition, to the specific working groups described above, there will be co-development with partners and wider colleagues on options and solutions.
Managing and supporting transition
9. The Blueprint recognises that the ask on ICBs this year is significant both in terms of developing and implementing their future redesign and ensuring delivery of 2025/26 plans. The working group developed high level principles to support ICBs develop their plans, balancing the need for some consistency of approach but allowing flexibility for ICB boards to develop their plans taking account of the local context.
10. Guidance includes further clarity on the cost envelope and what is included, importance of supporting staff through transition, principles to adopt in reviewing leadership structures and managing risk through transition including an expectation that all ICBs will set up transition committees.
11. As part of managing the transition NHS England has established a central programme team under the leadership of the Financial Reset and Accountability Director to provide co-ordination, support and a check and challenge on ICB plans. The central programme team will ensure appropriate guidance is co- developed to facilitate the transition, best practice is shared and there is meaningful engagement and co-development with national partners and wider colleagues on the future functions of ICBs.
Communications approach
12. A communications and engagement plan was developed and implemented to support the cascade of the Model ICB Blueprint using a ‘system first’ approach.
13. Careful thought was given to cascading the draft Model ICB Blueprint to ensure that system leaders received the message directly, once local elections communications restrictions were lifted, to enable them to prepare communications to colleagues and local teams in a controlled, timely and reassuring manner. Communications and engagement activities were carefully sequenced to achieve this goal.
14. Further engagement with stakeholders is ongoing and has included a call with ICB chief executives to discuss the content of the draft Model ICB Blueprint following cascade, as well as a number of regional and national workshops and roundtables to give further opportunity for feedback and for issues to be explored.
Interdependencies and risks
Interplay with the 10 Year Health Plan and NHSE Integration with DHSC
15. While the Government has fixed that ICBs will be strategic commissioners, wider questions on the future operating model for the NHS – the respective responsibilities of the centre, regional teams, ICBs, providers, and indeed local government – remain under consideration in developing the forthcoming 10 Year Health Plan and in expectation a health bill will be introduced into Parliament. National and regional colleagues from NHS England and the Department of Health and Social Care are working closely together to support this process which will facilitate alignment with the Model ICB programme.
16. In particular, Regional Directors – working alongside the Director of Financial Reset and Accountability – have started design thinking on the role of the regional teams during this transition building on the assumptions for potential transfer to Regions set out in the Blueprint. As this design work develops further it will be set out in a blueprint for the Model Region which will be aligned with the design of the future administrative Centre of the NHS. The Model Region document will be finalised over the coming weeks.
Meeting 50% running cost reduction by Q3 2025/26
17. By 30 May, ICBs must submit to NHS England their initial plans and financial templates for achieving the administrative costs reduction in Q3 2025/26 i.e. to achieve in aggregate a running cost of £18.76. There is a recognition that this is a challenging timeline and a significant reduction of costs. To support the development of credible plans the central team will undertake a supportive check and challenge process and will facilitate the sharing of good practice. This process will help ICBs to review their approach with their peers, bringing the necessary consistency and application of best practice across ICBs as they all move towards focusing on strategic commissioning.
18. There is a recognition that not all transferring functions can be done this year, particularly those rooted in ICB statutory duties, and some changes will require legislation, and all will need a safe transition path to a ready and willing receiver. We anticipate that most savings will come from streamlining approaches, identifying efficiency and at scale opportunities afforded through greater collaboration, clustering and where appropriate eventual mergers. There will need to be clarity from the Local Government Reform process of future local authority footprints before final ICB merger decisions can be made, ensuring interdependencies can be considered
Engagement with partners to refine the Model ICB Blueprint
19. It was necessary to produce the draft Blueprint at pace to set the overall direction for ICBs and support the development of plan submissions at the end of May. Given this timeline we were not able to undertake the breadth and depth of co-development normally undertaken with our national partners. To support the further development the Model ICB we are rapidly setting up engagement fora to ensure views of partners and potential receiving organisations are understood and built into plans going forward.
Conclusion
20. ICBs have a positive vital future, undertaking the same role as strategic commissioners in every integrated care system.
21. Transition into their new role will require ICBs to undertake major change so they all:
- run on efficient administrative budgets
- operate at a scale that allows resilient and specialised teams to be deployed
- over time, focus on the functions core to strategic commissioning
- build their organisational capabilities and staff skills as strategic commissioners
22. NHS England through the central co-ordination programme will provide ongoing support, sharing of good practice and rapid policy resolution where necessary to enable ICBs to make this transition safely, effectively and efficiently and manage interdependencies.

