Introduction
A series of ‘urgent and emergency care improvement guides’ have been designed for providers and systems to consider embedding as good practice to reduce ambulance handover delays.
The contents have been drawn from the Winter Improvement Collaborative which was set up to identify solutions to the problems facing the system over the winter period.
Members of the collaborative were asked to co-design a series of plans and potential improvement measures, to be adapted and trialled at local level.
Throughout the process there were opportunities to understand what is working and what is proving challenging, and to iterate the approach to ensure it has maximum benefit.
The learnings from the programme cover a range of areas including the flow of patients within hospitals from emergency services to wards, streaming patients into the most appropriate services, and standardising operational processes to be as efficient as possible.
The example trust used in this document has been anonymised.
Each trust is different and will need its own bespoke approach; examples are provided to inform local decision-making and action.
Same day emergency care flow
Over the last decade same day emergency care (SDEC) has become a widely used and accepted model of care for the management of acutely unwell patients: creating improved patient flow from referral to arrival, supporting early senior clinical decision-making and maximising the opportunity to complete patient care within the same day.
A patient may need to return to hospital for additional treatment and monitoring and should be facilitated where this is clinically appropriate.
The standard definition of SDEC is: same day emergency care (SDEC) allows specialists, where possible, to care for patients within the same day of arrival as an alternative to hospital admission, removing delays for patients requiring further investigation and/or treatment.
Teams across England continue to develop and improve their SDEC service appreciating its vital role to rapidly assess, treat and discharge home will support patient flow across urgent and emergency care.
Overall description of intervention
In this example, the combined assessment unit (CAU), which supports both medical/ surgical, is adjacent to the emergency department (ED).
The unit provides the ability for patients with an emergency/ urgent need to be seen within an SDEC service and allowing ED to concentrate on the critically ill patients.
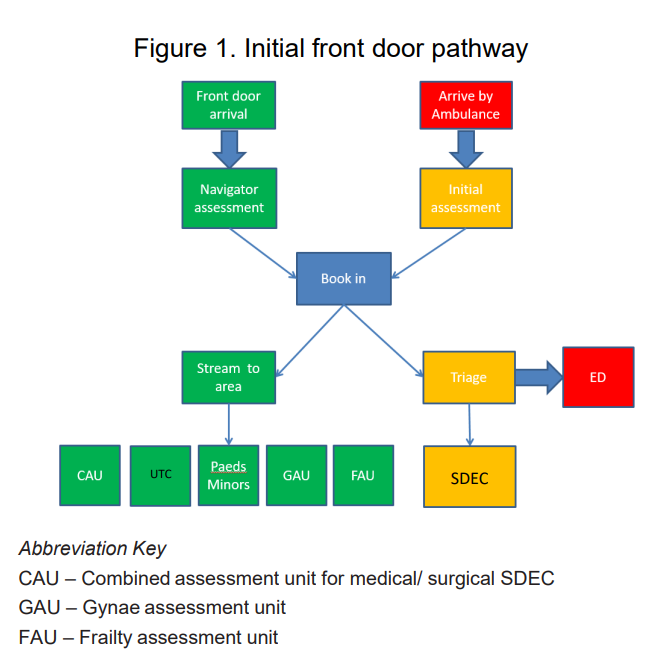
Figure 1 below highlights the initial front door pathway for both self-presenting ‘walk-in’ patients (green line) and ambulance arrivals (red/ yellow line). Both pathways have the ability for the patient to be seen within an SDEC service.
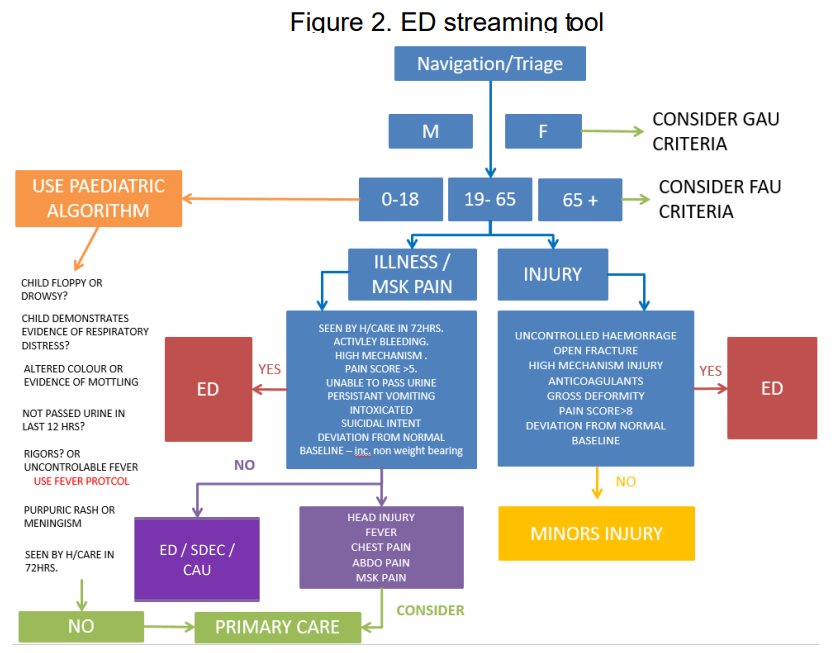
There is a senior nurse at the front door, who undertakes the streaming to the right service (see figure 2 below).
Continuous review and subsequent improvement of SDEC services is crucial in supporting flow.
Benefits
- Improved patient flow, preventing crowding of departments.
- Provides an admission alterative to patients, to enable capacity and flow within the acute care system.
- Improved patient experience.
- Improved ambulance handover delays.
Lessons learned and advice to those who want to implement
- Early identification of SDEC suitable patients is key to ensuring that the patient is directed to the right place first time and improves the experience of care for the patient.
- Staff engagement is crucial in the development of the pathway, gaining momentum and achieving a sustainable model.
- Relationships with the wider UEC system is important in maintaining conversations to support real improvements.
- Clinical and executive leadership is crucial in starting, developing and improve the SDEC offer.
- The lack of inpatient bed capacity can mean that the SDEC estate can be used to support additional bed space, a clear procedure should be in place should the estate need to be used and only invoked by the executive team.
- Consider the use of combined SDEC services to support knowledge exchange and combined workforce models.
Enablers
- ED, SDEC and patient flow all sit within one clinical division unit, meaning everyone has a part to play in the overall patient journey from the front door.
- Executive clinical leadership and oversight.
- Staff engagement across specialties.
- Project management team resource including key support services such as business informatics (BI).
| Barriers | Cause | How the barrier was addressed |
| Logistical challenge managing large number of referrals | Increased demand | Well-resourced administrative team is critical in supporting clinical decision makers |
| Impact on waiting times for patients | Workforce capacity | Minimise unnecessary waits – input from senior clinical leaders and swift discharge |
| Bedding of SDEC estate | Use of SDEC estate as additional inpatient capacity | Review of site escalation plan, action card and benefit evidence on the impact of not bedding SDEC |
Supporting documents used/developed by trust
- Standard operating procedure (SOP) for the service, with an exclusion criteria.
- Combined system UEC action plan.
- Site level project plan and/or organogram which includes a risk register.
- Business informatic dashboard to track improvements.
- Qualitative information from Patient, Advice and Liaison Service (PALS), Datix, Complements, Friends and Family Test feedback and complaints reports.
Links to guidance and best practice
Roles and responsibilities that enabled intervention delivery
Chief operating officer (COO)
- Operational oversight of the service and general management team and the transformation / project management office (PMO) team.
- Also responsible for communications and business informatic support.
Medical director
- Clinical and risk oversight of the service.
- Lead for signing off clinical risk and oversight factors.
Chief nurse
- Clinical and risk oversight of the service.
- Lead for signing off governance, including workforce and patient experience risk (physical risk assessment lead).
Roles critical in implementation
- Divisional director: providing clinical oversight of the service
- PMO/transformation team: tracking delivery and review of impact
- Operations (ops) team: operational delivery and performance
- Service clinical leaders: liaison with staff and implementation
- Communication (comms) team: staff engagement
- Business informatics (BI): review of performance.
Metrics (top 6 to review) |
|
| Ambulance | Ambulance referrals directed to SDEC/ambulance referrals accepted |
| In ED | Type 1 patients seen by senior decision maker within 60 minutes |
| In hospital | 111 referrals directed to SDEC/111 referrals accepted |
| Time in department in SDEC | |
| Number of patients referred for direct access by pathway | |
| Conversion rate to admission via SDEC |
Critical implementation path in reviewing SDEC
Weeks 1 to 2 – process
- Review of existing service provision.
- This should include representatives from the wider UEC forum, such as community, ICB colleagues, social care.
- Guidance materials are available on the NHS SDEC Futures platform: Guidance – SDEC Collaboration Platform – FutureNHS Collaboration Platform
Lead: Divisional director, Ops team, clinical leaders
Week 2 onwards – process
- Develop a joint improvement plan which spans across the wider UEC and includes key actions such as the review of services standard operating procedure, workforce and demand and capacity planning.
- Weekly meetings should be set to ensure pace is gathered and traction gained.
Lead: PMO lead/SROs
Week 3 onwards – workforce
- Review workforce model within the service. The review should include:
- Review tasks performed within SDEC compared to the skill set available. This can then support articulate gaps or where staff with specific skill sets can provide support.
- The review should also include demand vs activity linked to staffing.
- Tools available on the SDEC NHS Futures platform can assist with all of the above: Supporting Workforce Planning – SDEC Collaboration Platform – FutureNHS Collaboration Platform
Lead: Ops team/clinical leaders
Weeks 3 to 4 – activity volumes
- A review across the system should take place around activity volumes and include colleagues within the ICB.
- The purpose of this is to ensure that there is a clear understanding of the current activity through the service and any further potential to increase.
- This could be ascertained through a missed opportunity audit conducted jointly across the system in reviewing retrospective patients who attended ED and may have been best placed being seen elsewhere
Lead: SROs/Ops team/clinical leaders/system partners
Weeks 2 to 5 – standard operating procedure (SOP)
- Staff engagement in developing the SOP including wider system partners such as ICB, ambulance, primary care, NHS 111 provider.
- Involving staff within the service early on will support model delivery and sustainability.
Weeks 3 to 5 – SOP
- Collaboratively create a SOP and metrics to be monitored.
- The SOP should include how patients will be identified for SDEC, how to access the service, diagnostics available and timings, procedures, roles and responsibility of staff in the service.
Lead: PMO lead/SROs/Ops and clinical leaders
Week 4 onwards – comms
- Communications plan drafted and initiated.
- This should include active engagement with NHS 111, ambulance, community providers and primary care.
Lead: PMO lead/Ops team/Comms
Weekly – comms
- Weekly service improvement meeting to track delivery, comms approaches and to address risks/issues
Lead: PMO lead/SROs/Comms
Weeks 2 to 4 – Business informatics (BI)
- Key metrics to track improvements set and agreed.
Lead: Ops and clinical leaders
Daily/weekly – BI
- Daily and weekly metric monitoring and reporting
Lead: BI team
Activity within SDEC
As part of the example used within this UEC Improvement guide, 26.8% of the urgent and emergency care attendances were seen via SDEC following the review of the model:
| Activity | |
| Surgical | 5.3% |
| Children’s | 2.7% |
| Medical | 11.0% |
| Frailty | 6.7% |
| Gynae | 1.1% |
| Total | 26.8% |
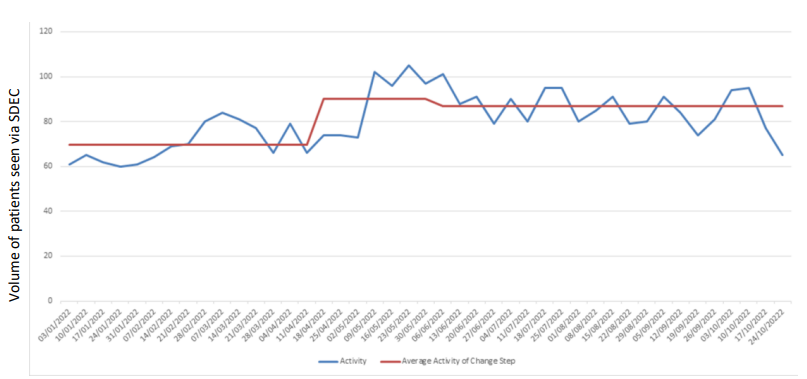
Impact on non-bedding of SDEC estate
Through commitment to not use the SDEC estate space as additional inpatient capacity, SDEC throughput improved by approximately 20% compared to baseline:
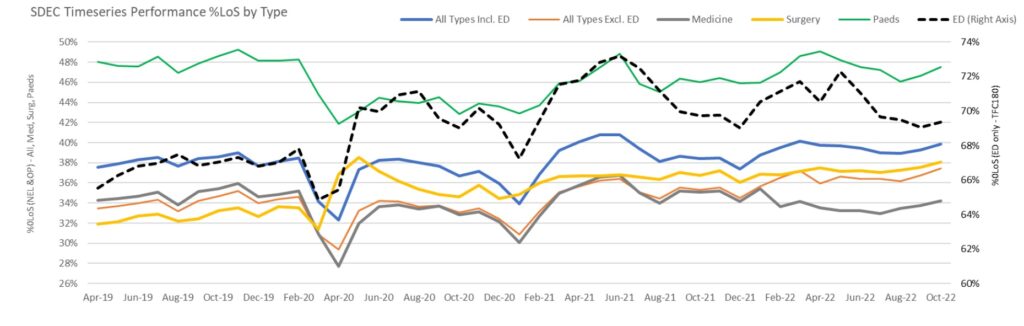
National SDEC activity 0LOS (proxy measure)
The national position for SDEC activity based on a 0 day Length of Stay (LoS) position.
The information highlights the recovery of SDEC services post-pandemic and the increased use of SDEC across specialities.
A third of the total non-elective activity should be seen via SDEC services with an increase year-on-year.
The 0 day LoS position can be used at site level to track improvements.
Supporting roles and responsibilities
The following represents a list of ‘responsibilities’ that were shared by members of the collaborative on subjects that were barriers/ enablers to implementing this intervention. These have been allocated against suggested roles that could provide support on these items.
The collaborative has worked with subject matter experts in the national UEC team who have developed suggested actions that regulatory/national/regional/system/local teams may wish to consider in supporting solutions to those asks and, ultimately, would be at their discretion.
National responsibilities
- Guidance on improving clinician-to-clinician confidence.
- Effective streaming from front door.
- Avoid patients sitting in ED before moving to SDEC.
- Development of surgical SDEC.
- Avoidance of bedding SDEC.
Action that could be taken:
- National UEC team to reiterate and share good SDEC practice.
Regional responsibilities
- Ensure all have a clinical SDEC lead and regional working group.
Action that could be taken:
- Identify regional, system and trust SDEC leads who are requested to attend a monthly SDEC-focused forum.
System responsibilities
- Improve and standardise SDEC referrals from GPs/ambulances/HCPs.
Action that could be taken:
- System to appoint a project lead to audit SDEC referral prevalence.
- Work with system and acute clinical leaders to create an improvement action plan that results in improved direct SDEC referrals from the community/ambulances.
Local responsibilities
- Ensure clinical ownership of SDEC.
- To maximise capacity by ensuring SDEC services are not bedded.
- Actively pull SDEC patients out of ED.
- Review 0-day length of stay in assessment units to identify alternative treatment options.
Action that could be taken:
- Ensure there is an SDEC triumvirate leadership group (clinical lead/lead nurse/manager) in place to ensure consistency and leadership of service. This team should ensure:
- there is a full SDEC oversight governance in place
- SDEC has a performance dashboard
- there is an improvement action plan for the development of appropriate SDEC activity.
- Executive commitment to never bed SDEC and to source alternative solutions to flow challenges.
- SDEC triumvirate to ensure open access criteria is in place to encourage referrals and also a culture of pulling patients from ED is empowered within SDEC daily working.
- SDEC triumvirate group to perform monthly audit on 0 length of stay in order to establish missed opportunity for SDEC activity growth. The results of this should feed the SDEC improvement plan.
Metrics
Top 6 metrics
| Flow area | Possible metric | Locally collected / already reported | Level of visibility | Type of measure |
| Ambulance | Number of patients referred for medical / surgical SDEC over the number of patients accepted to medical / surgical SDEC | Collected through ambulance daily collection – trusts may require ambulance service to share | Ambulance service | Outcome |
| In ED | Type 1 patients streamed to medical / surgical SDEC within 60m | Collected on UEC Daily SitRep | Trust, region | Balancing |
| In ED | Number of patients referred to medical / surgical SDEC out of hours | Locally collected | Trust | Balancing |
| In hospital | Average time in department prior to discharge from medical / surgical SDEC | Locally collected | Trust | Process |
| In hospital | Average time in department prior to discharge from medical / surgical SDEC | Locally collected | Trust | Process |
| In hospital | Number of return patients seen in SDEC within 72 hours | Locally collected | Trust | Balancing |
Further metrics
| Flow area | Possible metric | Locally collected / already reported | Level of visibility | Type of measure |
| Ambulance | Ambulance arrivals direct to SDEC | Locally collected | Trust | Process |
| In ED | Number of patients in ED by hour | Locally collected | Trust | Process |
| In ED | Type 1 patients seen within 60 minutes | Collected on UEC Daily SitRep | Trust | Process |
| In ED | Type 1 patients seen by senior decision maker within 60 minutes | Locally collected | Trust | Process |
| In ED | 4h A&E performance | Collected on UEC Daily SitRep | Trust, region | Process |
| In ED | 12h waits from decision to admit | Collected on UEC Daily SitRep | Trust, region | Balancing |
| In ED | 12h waits from arrival to ED | Collected on UEC Daily SitRep | Trust, region | Balancing |
| In ED | Clinically ready to proceed | Should be collected on ECDS – data quality may be poor | Trust, region | Balancing |
| In ED | Re-attendance rate | Locally collected | Trust | Balancing |
| In ED | Mean time in ED by chief complaint/age | ECDS | Trust | Balancing |
| In ED | Comprehensive geriatric assessment (CGA) within 30 minutes of arrival | |||
| In hospital | 1+ day LoS | SUS/HES | Trust | Balancing |
| In hospital | Activity by hour | Locally collected | Trust | Process |
| In hospital | Number of direct referrals to SDEC from 111/999 | Locally collected | Trust | Process |

Classification: Official
Publication reference: PRN00402