Classification: Official
Publication reference: PRN01930
To:
- NHS trust and foundation trust chief executives
- NHS trust and foundation trust chairs
- Integrated care board chief executives
- Integrated care board chairs
cc.
- NHS England regional directors
Dear Colleague
Working together in 2025/26 to lay the foundations for reform
When we met on 13 March, I committed to writing out on day one to help give more clarity on what we need to do in the coming weeks and months.
Before getting into the detail, I would like to thank you for your support over the last few tricky weeks. I’ve been really encouraged by both the recognition of the challenge we face and the collective response you’ve shown to it – most notably through the revised planning submissions. It is very much appreciated.
2025/26 planning
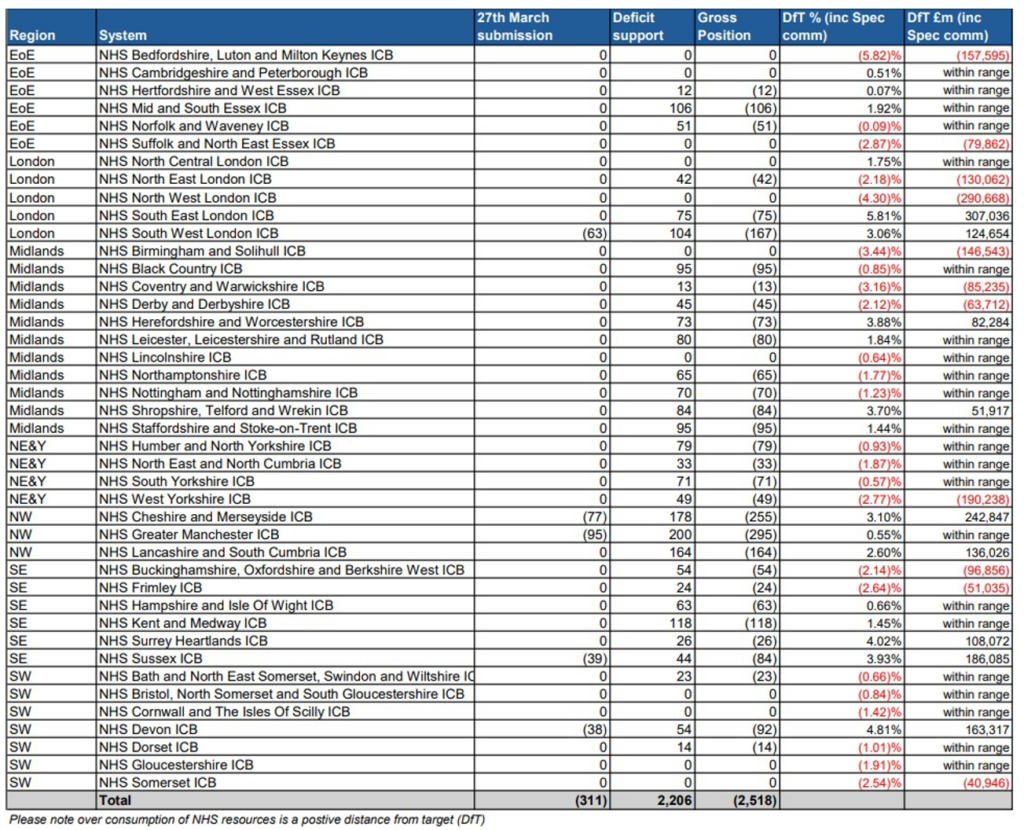
Your efforts over the past two weeks have put our plans for 2025/26 in a much stronger position, so please pass on my thanks to everyone who has worked so hard to make this improvement. As it stands, we have a headline deficit of £311 million (appendix 1) (after accounting for the £2.2 billion deficit support reflected in the allocations, so £2.5 billion versus the £6.6 billion referenced on 13 March). This is a significant shift, and there has also been positive progress on the key operational standards.
We are currently working through plans, and delivery confidence, and our regional teams will be working with you to finalise all of this over the next few weeks. Hopefully, this will build confidence and help establish a clear path to balancing the books in 2025/26 and delivering on our key operational imperatives.
Whilst the movement on the numbers is clearly very welcome, I’m even more encouraged by the broader leadership response from you all.
Moving to a different way of working together as leaders
The publication of the 10 Year Health Plan and the outcome of the Spending Review will give us the ingredients to shift towards a medium-term approach to planning. We will initiate a process with you to shape how we make this work between June and September this year, when the outcome of the Spending Review is known. Ideally, I would also like to use that process to both set out parameters for 2026/27 and, as far as possible, obviate the need for further Planning Guidance later this year, leading to a smoother planning process for next year. Again, we will be discussing this with you in more detail over the coming weeks as part of our new way of working.
This should help us get back to having honest and transparent conversations about how we’re all going to lead the recovery across the service. When we met on 13 March, I committed to greater transparency and moving back to a fair shares allocation policy over time, while unravelling some of the complexities that now exist around the money. A schedule is attached to this letter to confirm what allocations would have been if we had distributed allocations on a fair share basis (appendix 2). We will need to develop an affordable pace of change policy, but I think it’s important that you can see where we are heading.
Key to all of this is not just creating a fair playing field but also getting back to a place where the solutions to the challenges we face lie in our own hands as leaders. I think the shift to greater openness and transparency will help us become more accountable to our public and our staff and less so to the centre.
Ultimately, I’d like us to focus on more of a devolved, rules-based system that is built on strong Board accountability. We should target creating a net surplus going forward, so that we can shift away from focusing so much of our leadership energy on deficit reduction and create the bandwidth to do much more on quality (including wider population health), access and leading our organisations and local systems.
Integrated care boards (ICBs) are central to future plans
ICBs have a critical role to play in the future as strategic commissioners and this is going to be central to realising the ambitions that will be set out in the 10 Year Health Plan.
The 10 Year Health Plan will also set out the key components of an operating model that is rules-based, provides earned autonomy and incentivises good financial and operational performance. Importantly, alongside Penny Dash’s (NHS England’s new Chair) great work on quality, I am confident it will help reset and restore the focus on quality that we all want to see.
Reducing costs of ICBs by 50% will be a challenge, but it’s important we move on this as quickly as possible to retain talent and seize the opportunities of ICBs acting primarily as strategic commissioners.
Our collective challenge over the coming weeks and months will be to manage the transition as carefully as we can while recognising:
- the need to maintain some core staff, such as recently delegated commissioning staff and, in the short term until further options are considered, continuing healthcare staff
- the need to maintain or invest in core finance and contracting functions in the immediate term
- the need to invest in strategic commissioning functions, building skills and capabilities in analytics, strategy, market management and contracting
- the need to commission and develop neighbourhood health, with the delivery being a provider function over time (GPs, PCNs, community and mental health trusts, social care, acute trusts or others)
We will share soon what we think is a reasonable running cost per head of the population via regional directors and the functional output of the Model ICB work will be shared by the end of April. ICBs are expected to use this information to create bottom-up plans that are affordable within the reduced running cost envelope – for sign off by the end of May – and implement the plan during Quarter 3. ICBs are encouraged to expedite these changes as any in-year savings can be used on a non-recurrent basis to address in-year transition pressures or risks to delivery in wider system operational plans. We are in discussion with government colleagues about the impact this may have in terms of staffing reductions, and we are discussing the mechanisms this may entail, together with the costs and approvals of any exit arrangements. We will update you as soon as there is a clearer picture.
To meet this expectation, you should look carefully at functions where there is duplication. This includes:
- a number of assurance and regulatory functions (for example, safeguarding and infection control) where this is already done in providers and, in some cases, regions, without compromising statutory responsibilities
- wider performance management (as opposed to contract management) of providers which again already takes place in providers and at regional level
- comms and engagement which similarly exists in local authorities, providers and regions
Regional Directors will hold the ring with ICB Chief Executives on identifying how we are going to make the reductions, recognising that successfully reducing these costs will, in part, rely on cross-system arrangements going forward.
Reversing corporate cost growth in NHS providers
Since 2018/19, corporate costs in NHS providers have risen by 40% (£1.85 billion), excluding pay and pensions (56% including pay and pensions). While some of this cost growth has likely been necessary to improve clinical efficiency, we are now requesting that
all NHS providers reduce their corporate cost growth by 50% during Quarter 3 2025/26. These savings should be reinvested locally to enhance frontline services.
Some of these savings will be most effectively realised at a geographical or system level. Regional Directors will share benchmarking data for each provider and lean into this work to ensure that systems are collaborating, where appropriate, to determine the best approach. Also, in future, we will collect corporate cost data monthly to track progress and ensure delivery against this requirement.
Since 2019, there has been a substantial increase in the number of non-patient facing corporate nursing roles across NHS providers and ICBs. These roles have supported significant improvements within the nursing workforce, such as sustained post pandemic low leaver rates and reductions in vacancy levels.
However, initial analysis indicates significant sector and regional variation with the deployment and proportion of these roles within NHS providers. To ensure optimal deployment of the corporate nursing workforce, Duncan Burton, Chief Nursing Officer for England, will lead a benchmarking analysis to identify potential unwarranted variation and utilise this knowledge to set an appropriate threshold which we will ask systems and providers to align to in 2025/26. We aim to complete this work by the end of April 2025.
With regard to Wholly Owned Subsidiaries, we have adjusted our approval approach to subsidiary transaction assurance to reduce the burden on providers while ensuring that certain conditions are met. We will provide guidance shortly, informed by discussions with Unions nationally.
Enabling recovery through the NHS Standard Contract
We will shortly be publishing the response to the NHS Standard Contract consultation and the payment rules consultation for 25/26, which will set out a much more flexible approach to planning elective activity, including removing the elective payment limit, and proposals to strengthen the current activity management provisions within the contract.
This will be a first step in developing and strengthening commissioning, where commissioners and providers, where possible, jointly agree on affordable activity levels to meet key standards at the start of the year. This activity plan will be the basis on which providers and commissioners will work together during the year.
We will run a series of webinars to provide further details of the changes to the contract and outline the escalation routes we are putting in place.
Moving at pace to streamline the centre
As announced previously, Penny and Alan Milburn are jointly sponsoring the programme to bring together NHS England and the Department of Health and Social Care to create a single aligned centre. It is very clear that our staff want and need to see things progress with speed and fairness, and we are all committed to deliver on this.
On Thursday, we had the last NHS England Board before the Interim NHS England Executive Team formally takes up their posts today. The Board was keen to publish the NHS Performance Assessment Framework for 2025/26, this being an important part of our oversight system and can be a useful instrument. This is very hard to get right given our current operational context. So, we agreed we would consult on the updated framework and allow some testing in Q1 before using the framework in earnest from then on.
We will also publish our Urgent and Emergency Care Delivery plan shortly, and it is essential that we are better prepared for winter this year. This will be a test of whether we are pivoting to the right approach, so I’d value your feedback. We’ll use the UEC/winter planning activity to get some early conversations between the Interim NHS England Team and local leaders in the coming weeks and months.
Finally, I would like to reiterate how very grateful I am for Amanda’s support through this transition and handover, and for all she did in her tenure. We all wish her well back at Guy’s and St Thomas’ when she starts there in the autumn.
I will do all I can in the time I am in this role to help lead us through this tricky phase, alongside all of you. It has been very clear to me in the few weeks I have been involved, before starting properly today, how committed you all are to helping get the NHS back on its feet and delivering all we want and need to for our patients and staff.
Thanks again, all the best and keep going.
Sir James Mackey, Chief Executive, NHS England
Appendix 1 – 2025/26 financial plan summary as at 31 March 2025
Table: Regional 2025/26 financial plan submissions
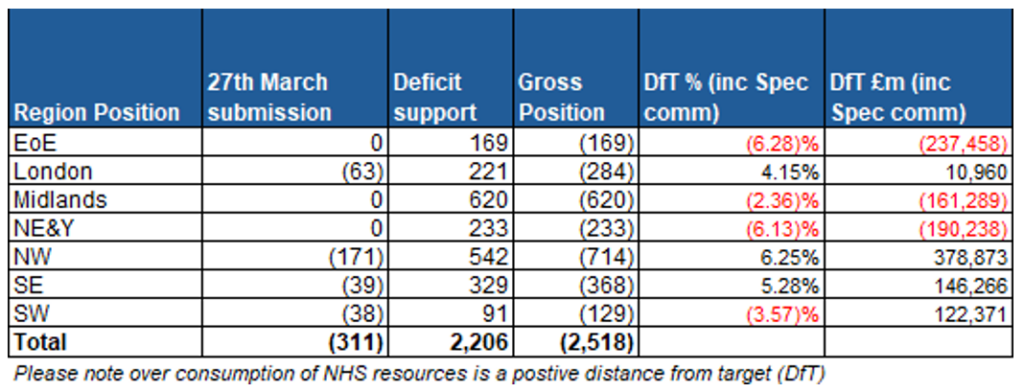
Table: ICB 2025/26 financial plan submissions
Appendix 2 – Distance to fair shares allocation by system
| Region | System name | Including specialist commissioning | Excluding specialist commissioning | ||
| Distance to target | Distance to target £m value (to +/- 2.5% range) | Distance to Target | Distance to Target £m value (to +/- 2.5% range) | ||
| EoE | NHS Bedfordshire, Luton and Milton Keynes ICB | (5.8)% | (89.9) | (3.8)% | (29.3) |
| London | NHS North West London ICB | (4.3)% | (121.6) | (3.7)% | (71.8) |
| Midlands | NHS Birmingham and Solihull ICB | (3.4)% | (40.1) | (5.9)% | (127.8) |
| Midlands | NHS Coventry and Warwickshire ICB | (3.2)% | (17.9) | (2.9)% | (9.4) |
| EoE | NHS Suffolk and North East Essex ICB | (2.9)% | (10.2) | Within Range | Within Range |
| NE&Y | NHS West Yorkshire ICB | (2.8)% | (18.3) | Within Range | Within Range |
| SE | NHS Frimley ICB | (2.6)% | (2.7) | Within Range | Within Range |
| SW | NHS Somerset ICB | (2.5)% | (0.6) | Within Range | Within Range |
| London | NHS North East London ICB | Within Range | Within Range | (2.6)% | (6.6) |
| SE | NHS Buckinghamshire, Oxfordshire and Berkshire West ICB | Within Range | Within Range | (3.1)% | (23.5) |
| Midlands | NHS Derby and Derbyshire ICB | Within Range | Within Range | Within Range | Within Range |
| SW | NHS Gloucestershire ICB | Within Range | Within Range | Within Range | Within Range |
| NE&Y | NHS North East and North Cumbria ICB | Within Range | Within Range | Within Range | Within Range |
| Midlands | NHS Northamptonshire ICB | Within Range | Within Range | Within Range | Within Range |
| SW | NHS Cornwall and The Isles Of Scilly ICB | Within Range | Within Range | Within Range | Within Range |
| Midlands | NHS Nottingham and Nottinghamshire ICB | Within Range | Within Range | Within Range | Within Range |
| SW | NHS Dorset ICB | Within Range | Within Range | Within Range | Within Range |
| NE&Y | NHS Humber and North Yorkshire ICB | Within Range | Within Range | Within Range | Within Range |
| Midlands | NHS Black Country ICB | Within Range | Within Range | Within Range | Within Range |
| SW | NHS Bristol, North Somerset and South Gloucestershire ICB | Within Range | Within Range | (4.3)% | (41.9) |
| SW | NHS Bath and North East Somerset, Swindon and Wiltshire ICB | Within Range | Within Range | Within Range | Within Range |
| Midlands | NHS Lincolnshire ICB | Within Range | Within Range | Within Range | Within Range |
| NE&Y | NHS South Yorkshire ICB | Within Range | Within Range | Within Range | Within Range |
| EoE | NHS Norfolk and Waveney ICB | Within Range | Within Range | Within Range | Within Range |
| EoE | NHS Hertfordshire and West Essex ICB | Within Range | Within Range | Within Range | Within Range |
| EoE | NHS Cambridgeshire and Peterborough ICB | Within Range | Within Range | Within Range | Within Range |
| NW | NHS Greater Manchester ICB | Within Range | Within Range | Within Range | Within Range |
| SE | NHS Hampshire and Isle Of Wight ICB | Within Range | Within Range | Within Range | Within Range |
| Midlands | NHS Staffordshire and Stoke-on-Trent ICB | Within Range | Within Range | Within Range | Within Range |
| SE | NHS Kent and Medway ICB | Within Range | Within Range | Within Range | Within Range |
| London | NHS North Central London ICB | Within Range | Within Range | Within Range | Within Range |
| Midlands | NHS Leicester, Leicestershire and Rutland ICB | Within Range | Within Range | Within Range | Within Range |
| EoE | NHS Mid and South Essex ICB | Within Range | Within Range | 3.0% | 13.6 |
| NW | NHS Lancashire and South Cumbria ICB | 2.6% | 5.2 | 4.0% | 67.0 |
| London | NHS South West London ICB | 3.1% | 23.0 | 2.9% | 14.8 |
| NW | NHS Cheshire and Merseyside ICB | 3.1% | 47.1 | 2.8% | 22.6 |
| Midlands | NHS Shropshire, Telford and Wrekin ICB | 3.7% | 16.8 | 5.5% | 36.2 |
| Midlands | NHS Herefordshire and Worcestershire ICB | 3.9% | 29.3 | 4.6% | 39.4 |
| SE | NHS Sussex ICB | 3.9% | 67.8 | 3.8% | 53.7 |
| SE | NHS Surrey Heartlands ICB | 4.0% | 40.8 | 4.7% | 50.0 |
| SW | NHS Devon ICB | 4.8% | 78.5 | 4.8% | 67.8 |
| London | NHS South East London ICB | 5.8% | 174.9 | 3.3% | 35.4 |

