Three costing principles underpin good costing processes and enable high-quality patient-level costing in all sectors and for all services delivered by relevant providers.
They offer a solid framework on which to construct costing data in conjunction with the costing standards and National Cost Collection guidance.
Where a unique situation arises, applying these principles should ensure a true and fair view of the cost of delivering patient care. For more information see Costing in the NHS.
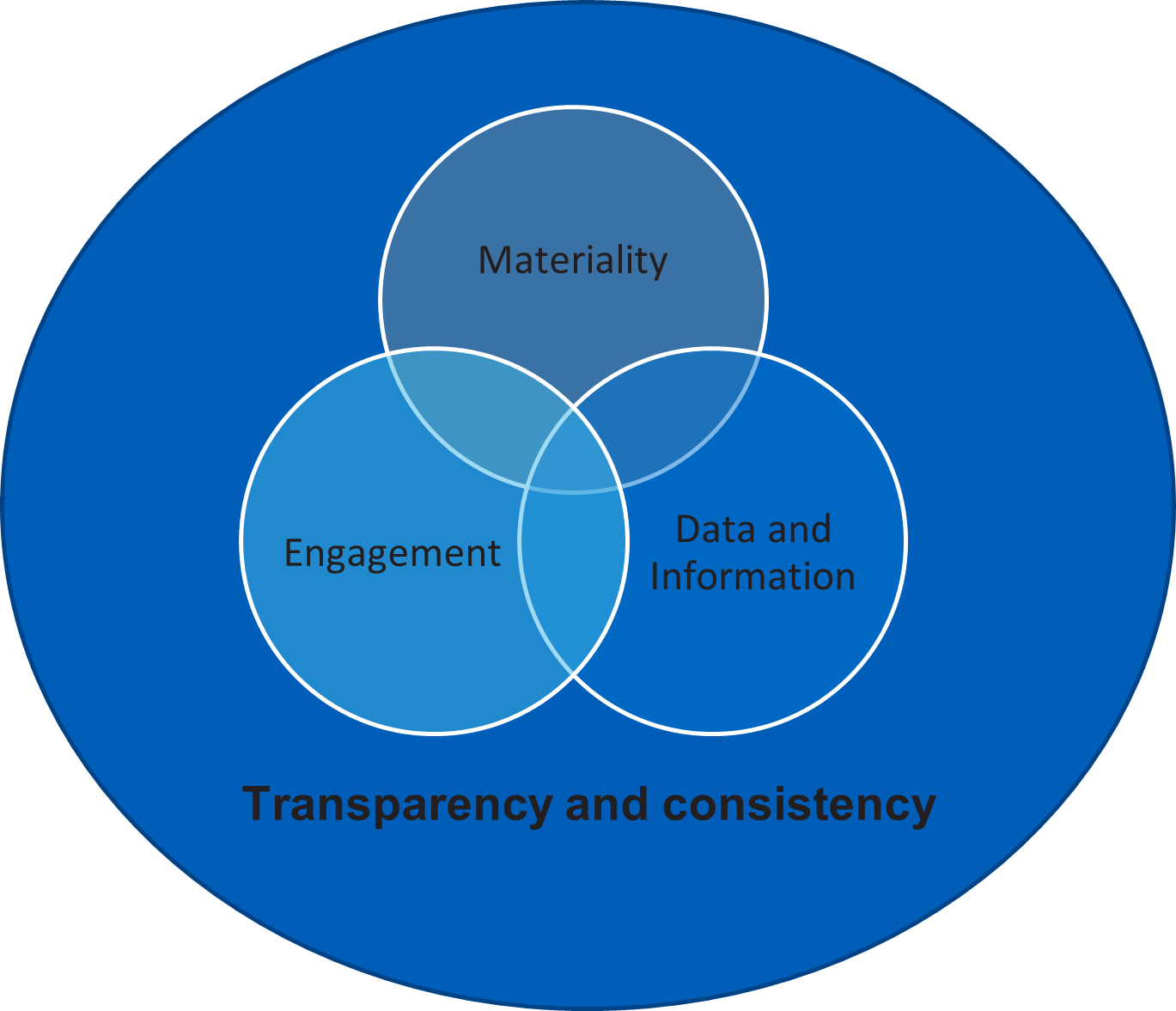
High-quality costing requires all three principles. Using them in the development of your costing programme locally will be key to your success. They have equal weight and if one is missing, it may stop you from achieving the full potential of your costing data. See Figure 1: Costing principles below.
Figure 1: Costing principles
Costing principle 1: Materiality
Those responsible for resources can manage them in patients’ best interests only if they understand what drives the larger elements of the cost incurred. Time is a scarce resource. Therefore, to make the most improvement in the cost model, focus on improving the costing for high-value and high-volume services.
In most instances costing practitioners should agree an appropriate materiality level with service leaders. Trusts can set their own materiality level of activity and cost with their costing steering group, and the impact of the decisions will be assessed by NHS England as part of the costing submission. Where this is not possible, or practitioners wish to start with a baseline for a discussion, we suggest applying a materiality threshold of more than 0.05% of your organisation’s expenses, or more than 5% of a specialty’s overall costs.
When defining the materiality level, consider the threshold above which missing or incorrect information is considered to have an impact on the decision-making of users.
Cost and activity that fall below the materiality threshold must still be included in the costing process but you should focus on high-value or high-volume areas first during your implementation and as part of your cycle of updates.
Costing principle 2: Data and information
To ensure the organisation costs are a true and fair representation, combine high-quality activity information with financial information. The costing process will transform raw and unorganised facts (data) into useful information. Increased data accuracy improves confidence in the resulting patient-level costs and enables managers to improve patient care.
Ensure that costed activity shows the true pathway and clinical interactions of the patient journey. This transparency will help get clinicians and managers to accept the numbers are correct and to act on the results.
Data accuracy is everyone’s responsibility but especially those supplying and inputting operational data, their managers and informatics leads. Costing practitioners are their internal customers, using the data to produce clear cost information.
Costing practitioners are ideally placed to flag data quality issues and explain the uses of the data for costing and decision-making, ensuring those responsible for it understand their importance in the costing process.
In the short term, while an organisation is working to improve its data quality generally, it is reasonable for costing practitioners to perform some data cleansing so the resultant cost data can continue to be used in a meaningful way.
Keep documentation up to date as the data is checked/cleansed and the costing process is continuously improved. Use the integrated costing assurance log (ICAL) to assure the board about the process undertaken.
Costing principle 3: Engagement and use
The costing practitioner, when effectively partnering with services, should be a change agent as well as someone who provides costing information. Stakeholder engagement is crucial for productive use of costing information. When combined with clinical feedback and actively used by frontline staff, costing information is a powerful driver of service efficiency.
This principle is about creating an active and productive relationship between clinical, management and corporate support teams. Costing patient-level activity does not only include patient-facing costs, and therefore it is important to ensure good stakeholder management with all functions of the organisation.
Engagement time should be a significant element of the annual costing cycle. By actively engaging with stakeholders, costing teams can:
- understand the audience for costing data – who uses it, how they use it and where the effort will achieve the highest impact
- ensure costing is more accurate, locally relevant and used by clinicians to drive improvements
- improve business intelligence by working with those delivering patient care, and so develop an understanding of how resources are consumed and assess how they could be better used.
The engagement process is an ongoing endeavour continually evolving towards robust and accurate Patient-Level Information and Costing Systems (PLICS). This in turn will support clinicians to use data for better decision-making, driving improvements to the patient journey.

