Capturing the impact of new ways of working for Allied Health Professionals arising from the COVID-19 response
The coronavirus pandemic has focused our health and social care system towards a common purpose – coming together to overcome coronavirus, ensuring capacity to help those who have been affected and minimising the impact on the health and well-being of the overall population.
Never have we been forced to change our working patterns so radically in such a short period of time. This has been a challenge and as Allied Health Professionals (AHPs) we should be proud of our response. There have been some excellent examples of teamwork, innovation, excellence in practice and leadership.
We have staffed the new Nightingale hospitals within a matter of days; services have been run virtually using digital technology; there has been a rapid upskilling of staff at scale; many AHPs have adapted their roles in order to help where the demand was greatest; students have been continuing their education remotely; some have been working from home and AHPs have stepped up to show their leadership qualities.
Now we are starting to think about the future, our current strategy AHPs into Action already asks us to think about what we should start, stop or do differently and there will be many service improvements we should maintain in the post coronavirus era. The pandemic initiated changes that needed a radical disruption to give permission and freedom to be innovative. Changes that moved us out of our comfort zone and enabled rapidly new ways of doing things, such as virtual consultations. This blog gives a helpful description of considering our crisis response measures, framed as end, let go, amplify and restart.
As the health and care system moves forward and the focus shifts to re-establishing services and supporting the ongoing health and well-being of people who have been in isolation; there will be opportunities for further learning and innovation.
In the next year we will be developing a new national strategy for AHPs to replace AHPs into Action. As with AHPs into Action, we will be crowdsourcing the priorities starting with what matters to our citizens, before focusing in on what AHPs can do the meet their needs in the future. Learning from our experience of this pandemic will shape the health and care system of the future.
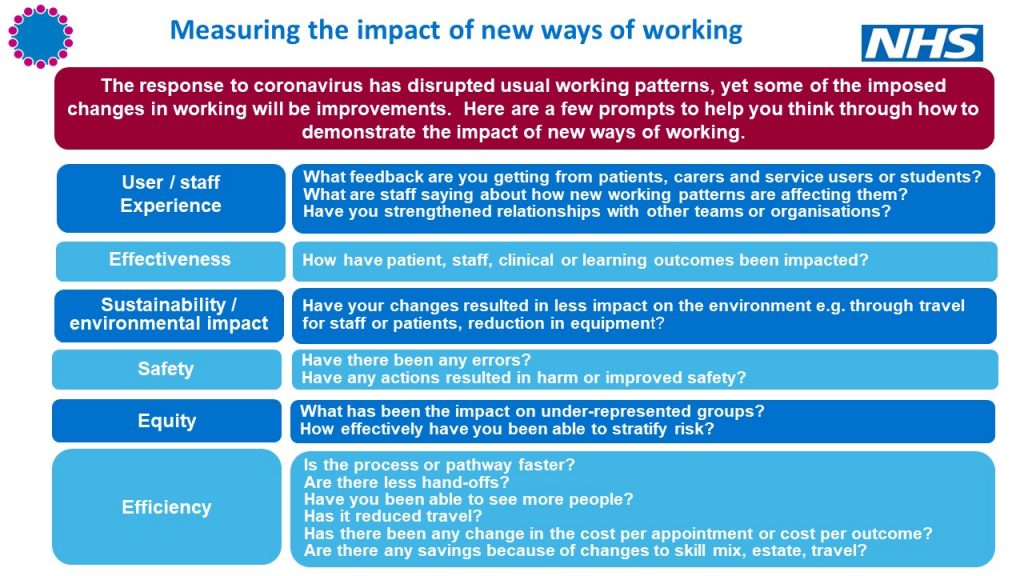
Now is the time to start describing those service improvements you are undertaking as part of the COVID response and considering what evidence we may need to create a case to continue the good practice. Whilst detailed data capture and evaluation might not be top of the to do list now, it is crucial to avoid leaving it too late to measure the impact of improvements. So, I ask – what could we be doing now to measure impact and are we capturing data already that could be developed or utilised to demonstrate and evidence the improvements created through changes in working practices? This could include measures about the structure, process, outcome or unintended consequences.
AHPs are still busy responding to the immediate and after effects of COVID-19 and therefore measures need to be pragmatic. The graphic below has been developed to support AHPs to consider the different ways they may be able to evidence the impact of new working practices.
Documenting quality outcomes for learning and new ways of working
We have created a space on the National AHP Virtual Hub to share examples of changes you have made and see what other AHPs have done. The National AHP team will use your examples to inform policy decisions. If you haven’t already registered for the AHP virtual platform, you can get access by emailing magortu.margai@nhs.net This is one of several ways to share and learn from others, I would also recommend #NHSChangeChallenge which enables AHPs to contribute to learning related to specific clinical pathways.
I thank AHPs from across the health and care system for everything you have done to respond to the coronavirus pandemic so far. I am proud of your actions and I know you will continue to adapt and improve to protect and care for the people we serve.