From ambition to action – improving heart and lung transplant services in England
Organ transplants not only save lives, they transform them. For our vital organs like hearts and lungs the impact of a transplant is priceless, and transcends not only immediate clinical outcomes, but also the long term impact on families and loved ones of donors and recipients.
We often talk about ‘life-course’ interventions in health care; transplantation services are the very forefront of this and it is therefore vital that we ensure patients and families alike get the best possible outcomes through the services we provide.
This is why NHS England has been undertaking a review of heart and lung transplantation services, building on a report commissioned by the Department of Health and Social Care (DHSC), Honouring the gift of organ donation, which was published in 2023.
How transplant services are organised
Adult heart and lung transplant services are currently commissioned (organised and funded) through five centres in England – Birmingham, Harefield, Manchester, Newcastle and Papworth (plus a sixth in Sheffield offering follow up services only). For children, two highly specialised centres undertake heart and lung transplants at Great Ormond Street in London and Newcastle. There are strong links with services in Scotland, Wales and Northern Ireland.
We undertake approximately 180 heart transplants and 120 lung transplants a year in England (for children and adults) and these services account for £80 million of NHS spend.
Patient outcomes
DHSC published their results of an information collation exercise for heart and lung transplant services in October 2024. Their work highlighted variation in clinical outcomes, as well as patient and staff experiences of services in England.
In response, our review team, including patient and public voice (PPV) representatives and national clinical advisors alongside NHS England staff, have worked with patients and heart and lung transplant centres to understand the root causes of why we, as a country, are not achieving the level of activity or outcomes that we need to. We have looked in depth at the whole system to understand actions that need to be taken – in transplant centres and at a national level. We have identified the following overarching goals for the programme:
- a significant increase in the number of transplants delivered
- substantial improvements in, and substantially reduced variation in, long term outcomes
- better patient experience of our heart and lung transplant services
- increased access to transplant, and reduced inequities in access to transplant
Our ambitions
The Programme Board, which is leading this work, includes NHS Blood and Transplant and the Department of Health of Social Care. It met in early July to agree a number of key ambitions that we are now sharing widely with patients, centres and wider stakeholders. These ambitions will be delivered through a number of workstreams and in partnership with transplant centres and patients.
The ambitions cover the foundations for change needed to achieve our goals alongside a set of clinical or service priorities. Figure 1 below shows the ambitions the Board agreed to prioritise. The accompanying pack of nineteen ambitions considered in detail by the board can be found on our Futures collaboration platform (login required). It also includes details of the stakeholder feedback which informed the Board.
Figure 1 – agreed ambitions for our work
Image text:
Agreed immediate priority ambitions for the programme lifetime
Clinical/pathway priorities
- Improved utilization of offered organs: Rapid short-term actions to improve organ acceptance decision-making through joint working across centres. Further actions to improve learning, accountability and incentives.
- Improved long-term outcomes: Consensus on and implementation of protocols for graft management, wider risks of immunosuppressants
- Better holistic care: Work at pace on best practice model, benchmarking of resourcing, financial case
- Improved access to transplant: Short term actions to understand unmet need and work with professional associations to promote referral pathways. Further actions to develop outreach
Foundations for long term change
- A single, integrated service model provided across multiple centres: A shared vision and view of ‘good’ care, a common strategy and plan, with dynamic quality improvement. Underpinned by two further ambitions: An open collaborative culture. An agreed whole-pathway dataset
- A resilient transplant workforce: Benchmarking, work with professional and training bodies
- Transparent funding that rewards centres for patients treated: Review of current trust income and spend, bottom-up costing of best practice care and review of tariff
Overarching goals
- Increased transplant rates
- Improved long term outcomes
- Better experience
- Improved access
Longer team priorities for implementation through a new business-as-usual
- Patient choice
- Waits
- Information-sharing
- A culture that invites and acts on feedback
- Integration with referrers
- Waiting list/allocation arrangements Service specifications
- Extension of the national registry
Following agreement of the ambitions, work has begun on establishing the workstreams and delivery mechanisms to drive change, with a focus on what immediate actions can be put in place.
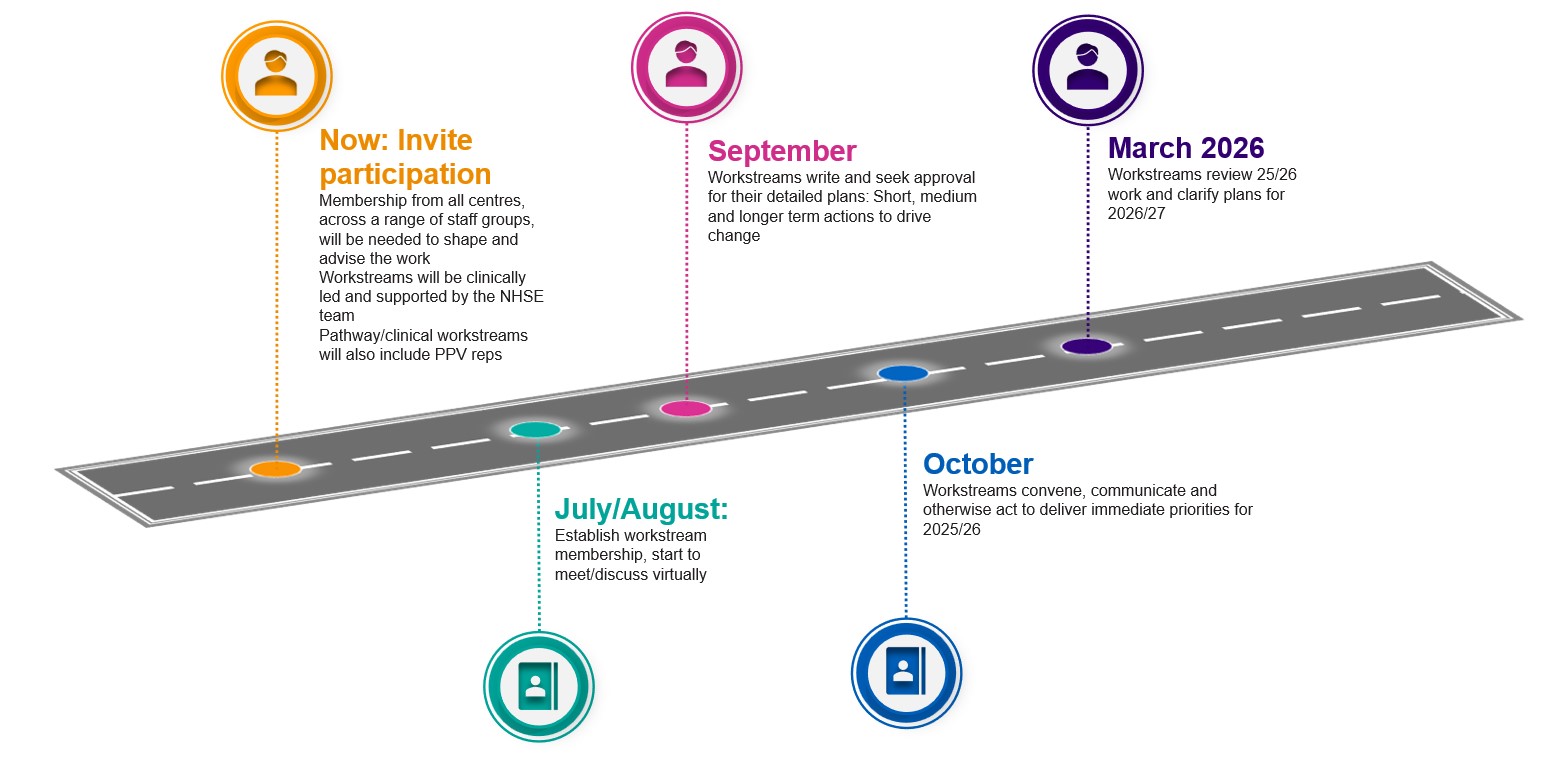
Figure 2 – our forward plan
Image text:
Now: Invite participation
- Membership from all centres, across a range of staff groups, will be needed to shape and advise the work
- Workstreams and subgroups will be clinically led and supported by the NHSE team
- Pathway/clinical workstreams will also include PPV reps
July/August
- Establish workstream membership, start to meet/discuss virtually
September
- Workstreams write and seek approval for their detailed plans. They identify rapid, medium and longer term actions to drive change
October
- Workstreams convene others, communicate and otherwise act to deliver immediate priorities for 2025/26
March 2026
- Workstreams review 25/26 work and clarify plans for 2026/27
Co-production with patients and next steps
Co-producing our ambitions with patients has been central to the review. This is why we have included people with lived experience of transplant services as core members of the programme team and Board and are ensuring our plans are co-designed with patient input. A patient consultation event was undertaken to support the shaping of our ambitions. We are also seeking further representations to support our delivery workstreams to drive the change that is needed to ensure improvements. These will cover access to transplant, long term outcomes, effective use of the organs that are offered, and holistic care and support which we know are vital to both clinical outcomes, and quality of life for patients and families following a heart or lung transplant.
To find out more about the programme, you can view the full slide deck which sets out our ambitions for this work and how they will be delivered on Futures. If you have any problems accessing the slides or would like further information on the programme please email england.scengagement@nhs.net. You can also sign up as a registered stakeholder to keep up to date as work progresses.
Contributors and acknowledgements:
Maggie Kemmner, Head of Heart and Lung Transplant Transformation, and the programme team; Marius Berman, National Specialty Advisor (NSA) for heart transplant, Ellie Johnson NSA for transplant coordination, and Anna Reed NSA for lung transplant; and our patient voice representatives Robbie Burns, Rosie FitzGerald, and Andrea Mistry.