Introduction
This report describes the whistleblowing disclosures made to NHS England between 1 April 2023 and 31 March 2024. It summarises:
- the number and type of disclosures received
- how we responded to them
Jump to the sections on how many disclosures were made and what action was taken.
What are whistleblowing disclosures?
The Employment Rights Act 1996 protects employees who pass on information about wrongdoing when:
- they have a reasonable belief that they are acting in the public interest (protection is therefore not normally given for disclosures connected to personal grievances)
- the disclosure is about one of the following:
- criminal offences (including financial impropriety such as fraud)
- failure to comply with duties set out in law
- miscarriages of justice
- endangering someone’s health and safety
- damage to the environment
- covering up wrongdoing in any of these categories
NHS England is a ‘prescribed person’ according to the Public Interest Disclosure (Prescribed Persons) Order 2014. This means people can make disclosures to us under the Employment Rights Act 1996 and receive protection if they have a reasonable belief that the failure being disclosed falls within our remit and that the information disclosed is true.
Our remit as a prescribed person covers:
- primary care services (primary medical, dental, ophthalmic and pharmacy services)
- NHS trusts and NHS foundation trusts
- our workforce planning, training, and education functions
- integrated care boards
When information is disclosed to us that is about the NHS but outside this scope, we will still consider whether further action to address the issue raised is appropriate.
This report describes disclosures falling within our remit. These are described below as ‘in-scope’ disclosures. Disclosures falling outside the remit are described as ‘out-of-scope’.
Why are we publishing this report?
The Prescribed Persons (Reports on Disclosures of Information) Regulations 2017 require prescribed persons to report annually on the whistleblowing disclosures they receive.
This improves transparency and reassures people who speak up that disclosures will be taken seriously. For the purposes of this report, we use the term ‘whistleblowing’ to reflect the terminology in the government guidance but we also refer to this activity as ‘external Freedom to Speak Up’ at NHS England. Concerns raised with us are considered under our External Freedom to Speak Up policy for NHS workers.
We have written this report in line with the Department for Business, Energy and Industrial Strategy’s guidance on whistleblowing. No information has been included that would identify individuals who have spoken to us or people mentioned in the disclosures.
NHS England’s functions and objectives
Listening to colleagues who speak up is vital for regulating the NHS and improving staff experience and patient care. It helps identify safety and quality issues and highlights areas for improvement in leadership and governance.
We continue to review and improve our approach to encouraging, receiving and handling disclosures. In doing so, we take account of the Department for Business, Energy and Industrial Strategy guidance, specialist advice, our own experience and the approaches taken by other prescribed persons.
We use in-scope and out-of-scope disclosures from NHS workers and other relevant information to inform our oversight of and support for NHS providers (in line with the NHS Oversight Framework). This includes sharing information with other relevant organisations and agencies (particularly the Care Quality Commission) to inform their regulation of healthcare providers.
In 2023/34, our remit as a prescribed person expanded to include matters for which Health Education England had previously been a prescribed person. In November 2023, the law changed to make us a prescribed body for speaking up about integrated care boards.
We have included some anonymised examples of disclosures in this year’s report to illustrate the issues raised and our approach to addressing them.
How many disclosures were received?
NHS England received 433 disclosures in 2023/24. Of these, 257 (59%) were ‘in-scope’ (falling under the ‘prescribed person’ remit described above) and 3 were still under review on 31 March 2024.
Figure 1: disclosures falling inside and outside our remit
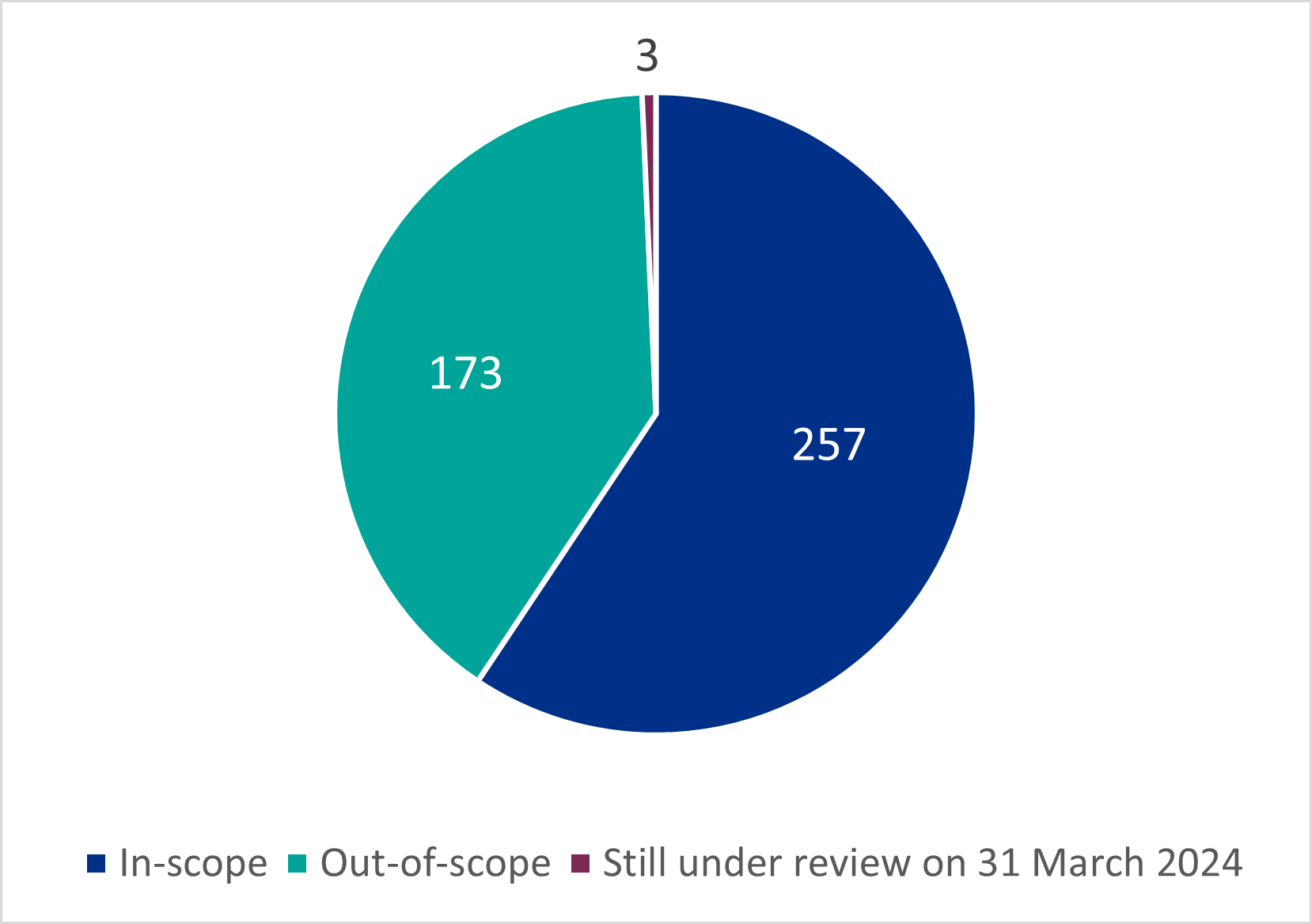
Figure 1 shows the proportion of cases classified as ‘in scope’ (within our remit as a prescribed person) compared to those that were ‘out of scope’ or were still being assessed.
Figure 2: what organisations were involved?
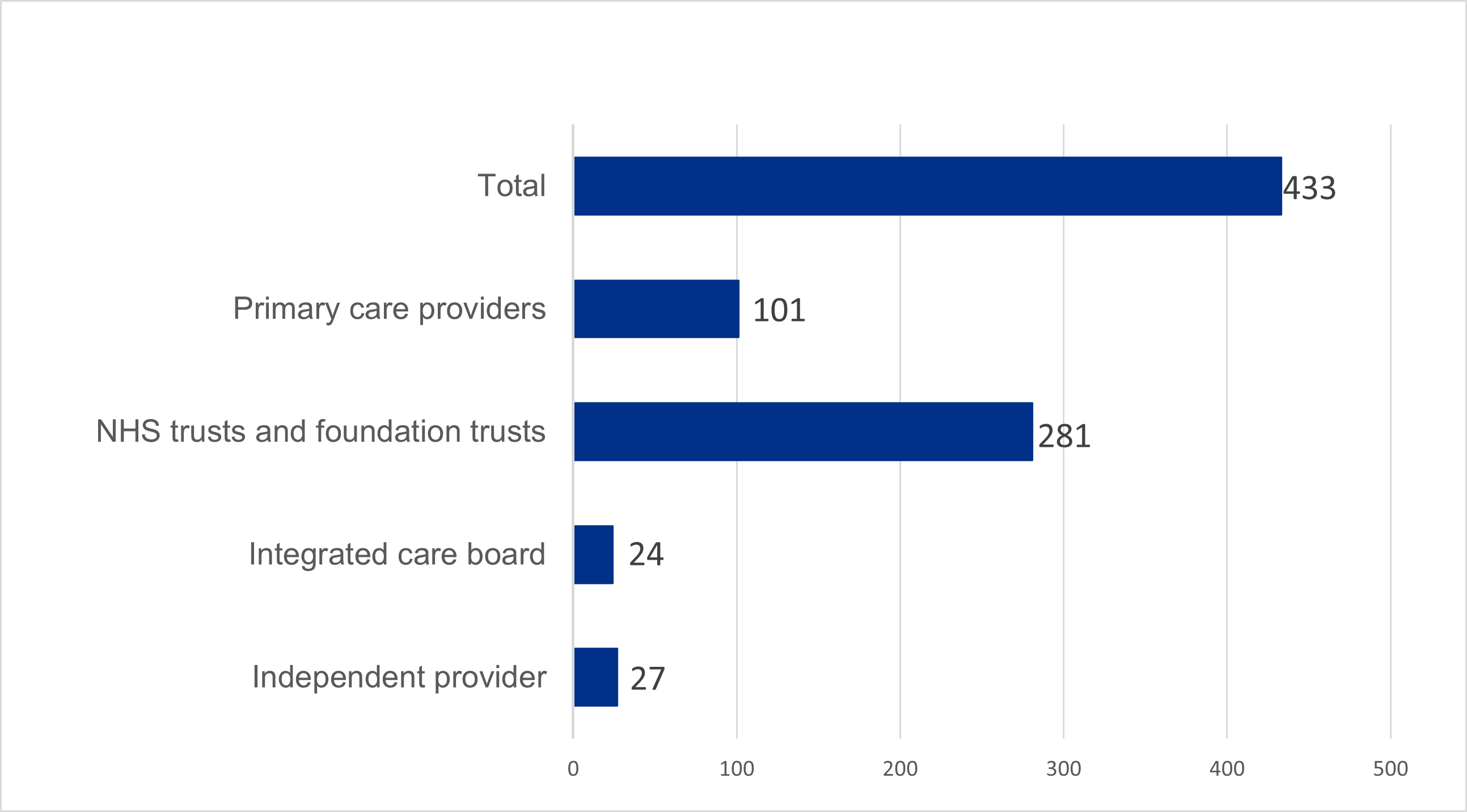
Figure 2 shows the types and number of organisations involved in disclosures:
- primary care providers: 101
- NHS trusts and foundation trusts: 281
- integrated care boards (ICBs): 24
- independent providers: 27
Speaking up about primary care providers (including host organisations for primary care services)
NHS workers can contact NHS England as a prescribed person with concerns about the delivery of primary medical, dental, ophthalmic, and pharmaceutical services in England, whether they are provided by individual organisations or supported and run by NHS trusts or foundation trusts. (In cases involving trusts, NHS England may need to assess their leadership and oversight of the service, as well as the commissioning).
In 2023/24, we received 101 disclosures for primary care. Of these, we considered 72 to be in scope.
The top 3 issues that workers spoke up to us about in primary care organisations in 2023/24 were:
- the safe running of a practice (predominantly pharmacy, GP or dental services)
- professional standards concerns about practitioners on the performers lists (GPs, optometrists and dentists)
- a bullying culture within a primary care organisation
Actions taken by NHS England in response to primary care disclosures
Since 1 July 2022, NHS England has delegated its commissioning responsibilities to ICBs. This includes a responsibility for ICBs to investigate whistleblowing concerns related to primary care when NHS England raises them.
In a high proportion of primary care cases, therefore, we asked the relevant ICB to assess whether the disclosures raised issues impacting on the commissioning or contractual obligations of the provider. In other cases, we thought the issues raised should be looked at by a different regulatory body, such as the Care Quality Commission (CQC) or Counter Fraud, or by the relevant professional standards team.
In 2023/24, NHS England, or an ICB acting under the delegation arrangements, took action in 46 of the 72 in-scope cases. In most cases, we made further enquiries as part of our performer list function or the ICB looked at contractual obligations.
Figure 3: actions taken in response to primary care disclosures
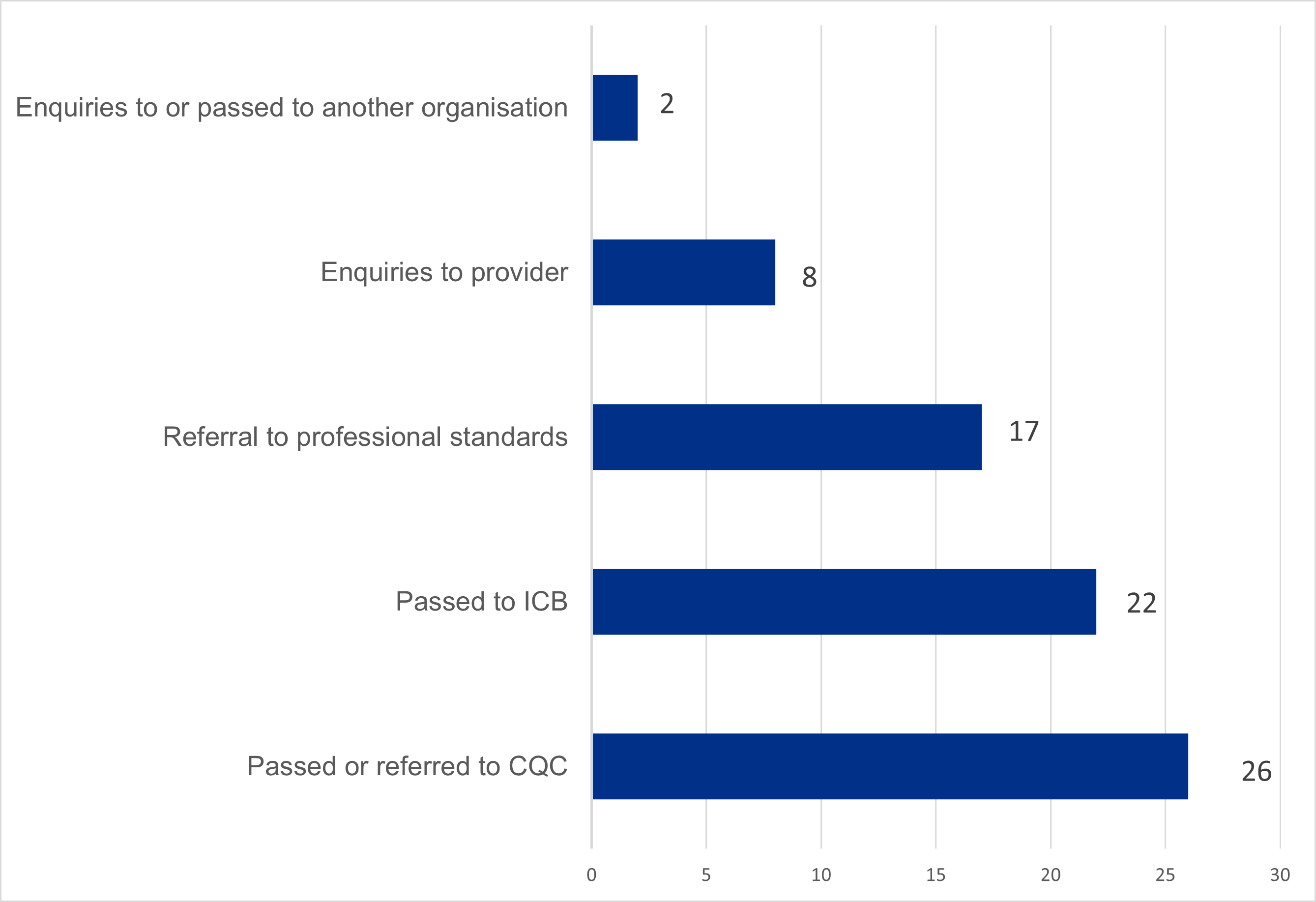
Figure 3 shows the number of actions taken by NHS England in the 46 ‘in-scope’ cases we acted on. This includes:
- enquiries to or passed to another organisation: 2
- enquiries to providers: 6
- referrals to professional standards: 17
- passed to ICBs: 22
- passed or referred to CQC: 26
The total number of actions exceeds the number of cases because a single case could lead to more than one action.
Because a large number of the disclosures involved patient safety, the most frequent action we took was referring the matter to or making enquiries of the CQC.
The information we received usually gave us enough assurance to conclude that no further action was necessary. In a few cases, these enquiries led to further action with individual performers and to recommendations for improvement. In some cases, other regulators took action due to concerns initially shared with NHS England.
A number of workers in a GP provider spoke up about safety, quality of care, and practice leadership. NHS England worked with CQC and the ICB to review all the concerns. The practice developed an action plan to respond to the required improvements, including improved administration, management and complaint response. An additional practice manager was employed to support with human resource issues.
We took no substantive action in 26 cases. The main reasons for not taking action were:
- the issue being raised was already known about and being addressed
- we did not have sufficient detail to take any action
- local resolution was underway
Speaking up about NHS trusts and foundation trusts (including ambulance, community and mental health care trusts)
NHS workers can contact us with concerns about the quality of care or services and the financial and operational performance of NHS trusts and NHS foundation trusts.
In 2023/24, we received 281 disclosures relating to these organisations. Of these, NHS England considered 158 to be in-scope disclosures.
The top 3 issues that workers spoke up to us about in these organisations in 2023/24 were:
- unsafe care regarding patient safety and quality of care
- staffing issues compromising safety and effectiveness
- quality and safety oversight by leaders
Figure 4: actions taken in response to disclosures in NHS trusts and foundation trusts
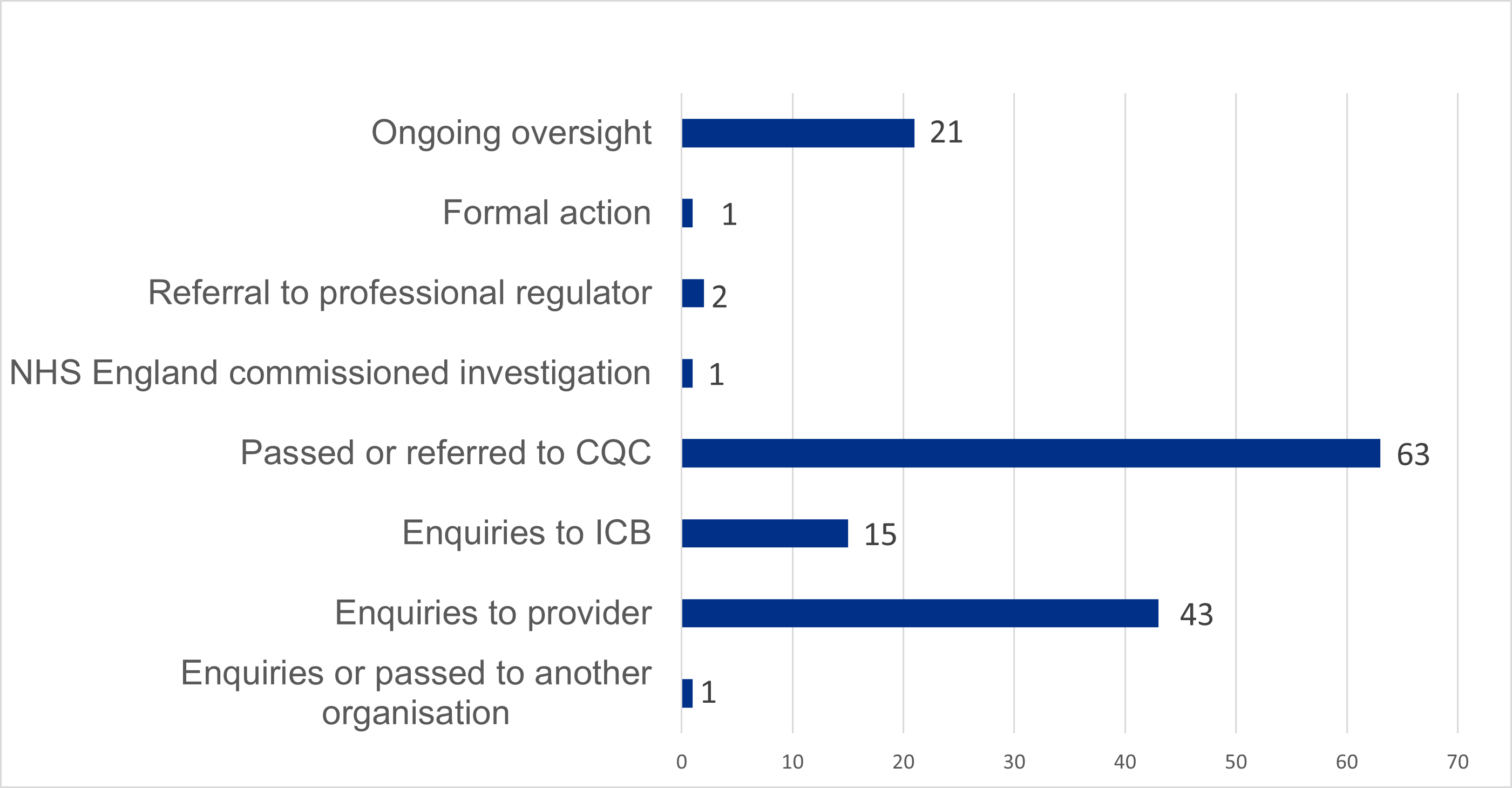
Figure 4 shows the number of actions taken by NHS England in the 85 ‘in-scope’ cases we acted on. This includes:
- ongoing oversight: 2
- formal action: 1
- referral to professional regulator: 2
- NHS England commissioned investigation: 1
- passed or referred to CQC: 63
- enquiries to ICB: 15
- enquiries to provider: 43
- enquiries passed to another organisation: 1
The total number of actions exceeds the number of cases because a single case could lead to more than one action.
We acted in response to 85 of the 158 disclosures about NHS trusts and foundation trusts that were considered in scope. In many cases, this involved making further enquiries as part of our oversight of and support for providers (in line with the NHS Oversight Framework).
The information we received usually gave us enough assurance to conclude that no further action was necessary.
In one case, it led to NHS England commissioning an investigation and in other cases we asked providers to commission investigations. These resulted in recommendations for improvements, usually to overall governance, quality of care and services or leadership.
In many cases, we shared the information with or referred the case to the CQC. In some, we decided that another regulatory body should also consider the disclosure.
We took no substantive action in 73 cases. This was usually because the issue being raised was already known about and being addressed by our regional teams or the ICB. In some cases, we did not have sufficient detail to take action.
Where workers were not aware of or hadn’t used internal processes and where we considered that local resolution would be the most appropriate action, we encouraged workers to use their internal speaking up processes, if they felt able to so.
A worker in an acute NHS foundation trust spoke up to NHS England about the way their trust managed a particular clinical service and how they felt about the way a senior leader had responded to these concerns.
NHS England commissioned an independent review that made some recommendations for improvement, including the development of a trust wide safety strategy and improved processes to ensure delays within clinical administration were rectified. The trust accepted the recommendations. The improvements are being overseen by the regional team and the trust.
Speaking up from ICB workers
NHS workers can contact NHS England with concerns about the financial, oversight and governance performance of ICBs.
In this reporting period we received 24 disclosures for ICBs. We considered 14 to be in scope.
The top 4 issues that workers spoke up to us about in these organisations in 2023/24 were:
- bullying by a manager
- executive or senior staff conduct demonstrating poor cultural leadership
- commissioning decisions
- the oversight of quality of care and safety
Actions taken by NHS England in response to ICB disclosures
NHS England approached the relevant ICB to make further enquiries in 6 of these cases. In most, this provided us with enough assurance that no further action was needed.
A small number of cases led to recommendations for improvements. usually relating to ICB governance or leadership.
We took no substantive action in 8 cases. This was usually because the issue being raised was already known about and being addressed by our regional teams or because we received insufficient information to make any further enquiries.
NHS England received a disclosure about the leadership and financial governance of a large department in an ICB. Enquiries were made to the ICB and a review of the information shared was undertaken by the relevant NHS England department. This highlighted some concerns with the way information was being reported. NHS England had not been aware of these issues and they are now being monitored by the ICB leadership and the relevant NHS England department.
Speaking up about matters related to healthcare education and training (previously covered by Health Education England)
In 2023/24, NHS England did not receive any disclosures about the provision of healthcare education and training.
Where we received concerns from healthcare trainees about matters related to their work placement, these cases are included in the data related to that workplace.
Reasons for speaking up to NHS England
We ask workers who speak up to NHS England why they chose to come to us rather than their employer.
This helps us to understand the barriers to speaking up locally and helps NHS organisations to improve their speaking up arrangements.
Figure 5: why do workers speak to NHS England rather than their employer?
Where possible we collect the reasons for people making whistleblowing disclosures to NHS England rather than using their own organisation’s processes.
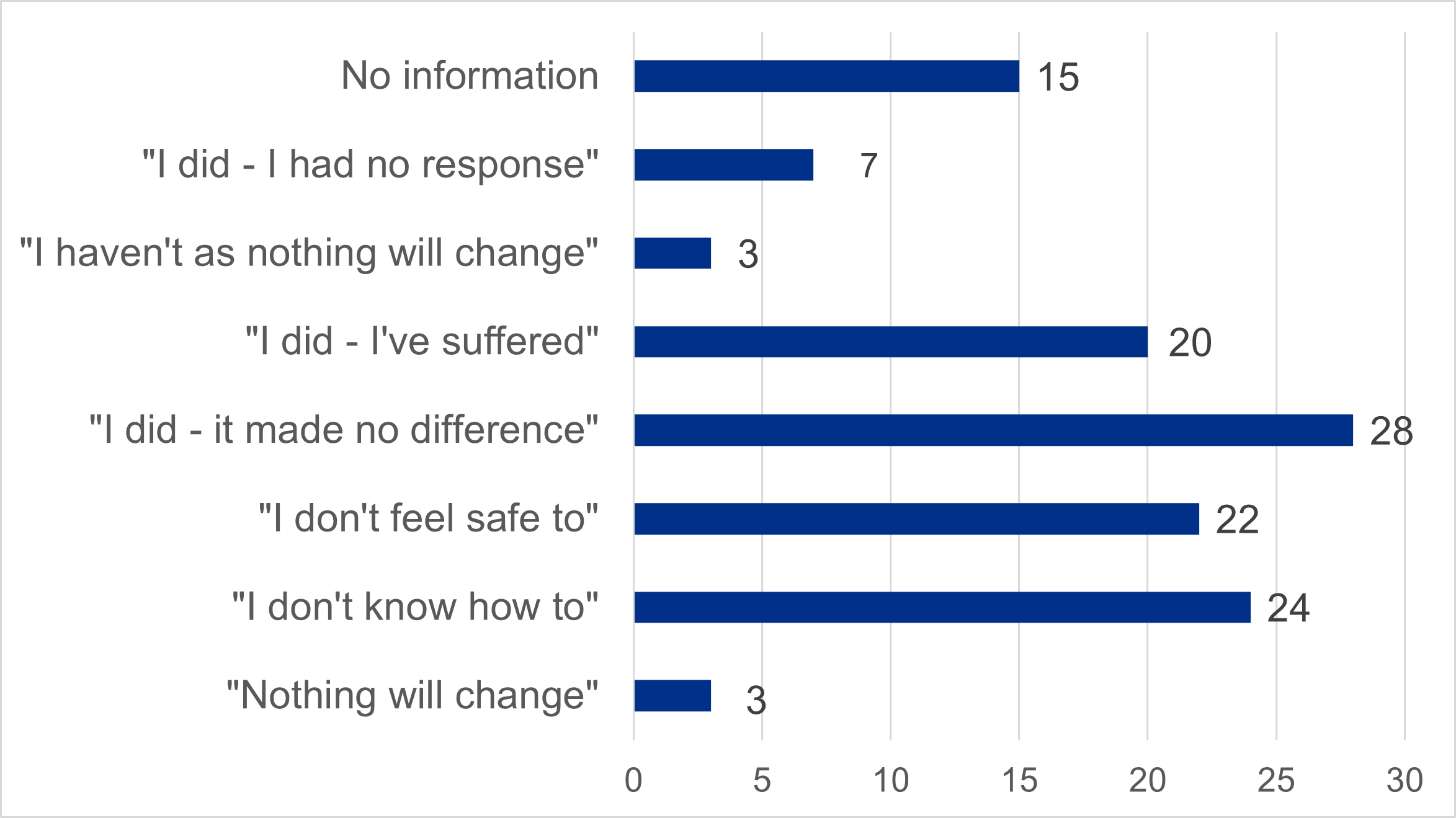
Figure 5 shows the reasons for people making whistleblowing disclosures to NHS England rather than using their own organisation’s processes, and the number of people who gave these reasons. It also shows where people did not disclose the reason for this.
- no information: 15
- “I did – I had no response”: 7
- “I haven’t as nothing will change”: 3
- “I did – I’ve suffered”: 20
- “I did – it made no difference”: 28
- “I don’t feel safe to”: 22
- “I don’t know how to”: 24
- “Nothing will change”: 3
Reasons by sector
Figure 6: top 3 reasons for speaking up to NHS England in secondary care
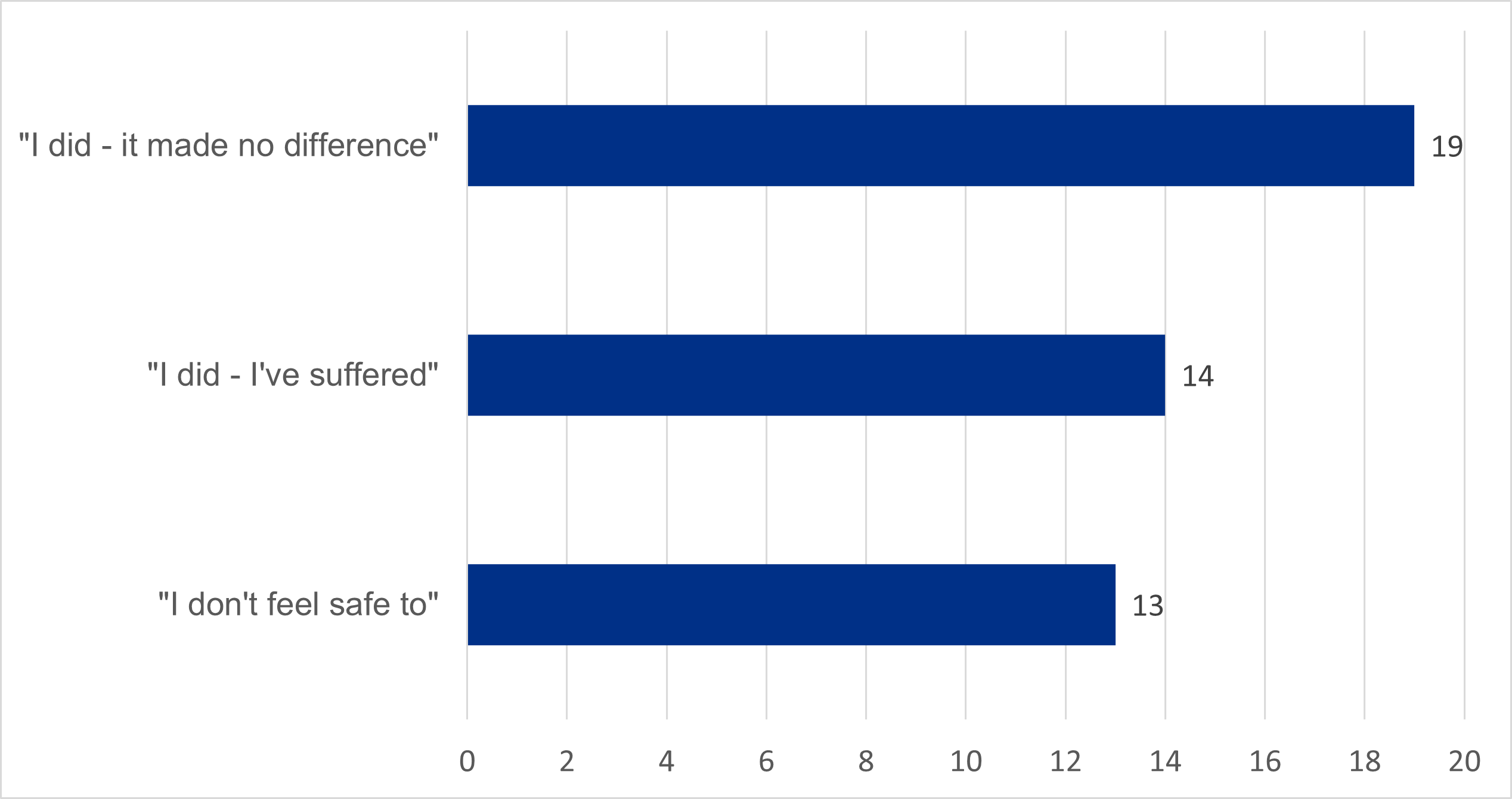
Figure 6 shows the top 3 reasons for speaking up to NHS England in secondary care and the number of people who gave these reasons. This includes:
- “I did – it made no difference”: 19
- “I did – I’ve suffered”: 14
- “I don’t feel safe to”: 13
The most common reason for speaking up to NHS England in the secondary care sector was a perception that speaking up within their organisation had made no difference.
The next most common reasons involved experiencing negative treatment for speaking up and not feeling safe to speak up internally.
This treatment included being excluded, ignored, demoted or being put through disciplinary processes.
NHS England received a disclosure from a worker at an ambulance trust about the speaking up process itself. They had raised issues internally and no one had given a clear plan for addressing them. The concerns were shared by NHS England with the ICB, who were already working with the trust on their CQC oversight plan. The ICB ensured the issues raised were addressed by the trust.
NHS England works with NHS organisations to ensure that they listen to their workers when they speak up and that they take action to resolve issues. We expect organisations to provide clear explanations and feedback to people reporting issues, while maintaining appropriate confidentiality. We monitor improvements using the NHS national staff survey.
Figure 7: top 3 reasons for speaking up to NHS England in primary care
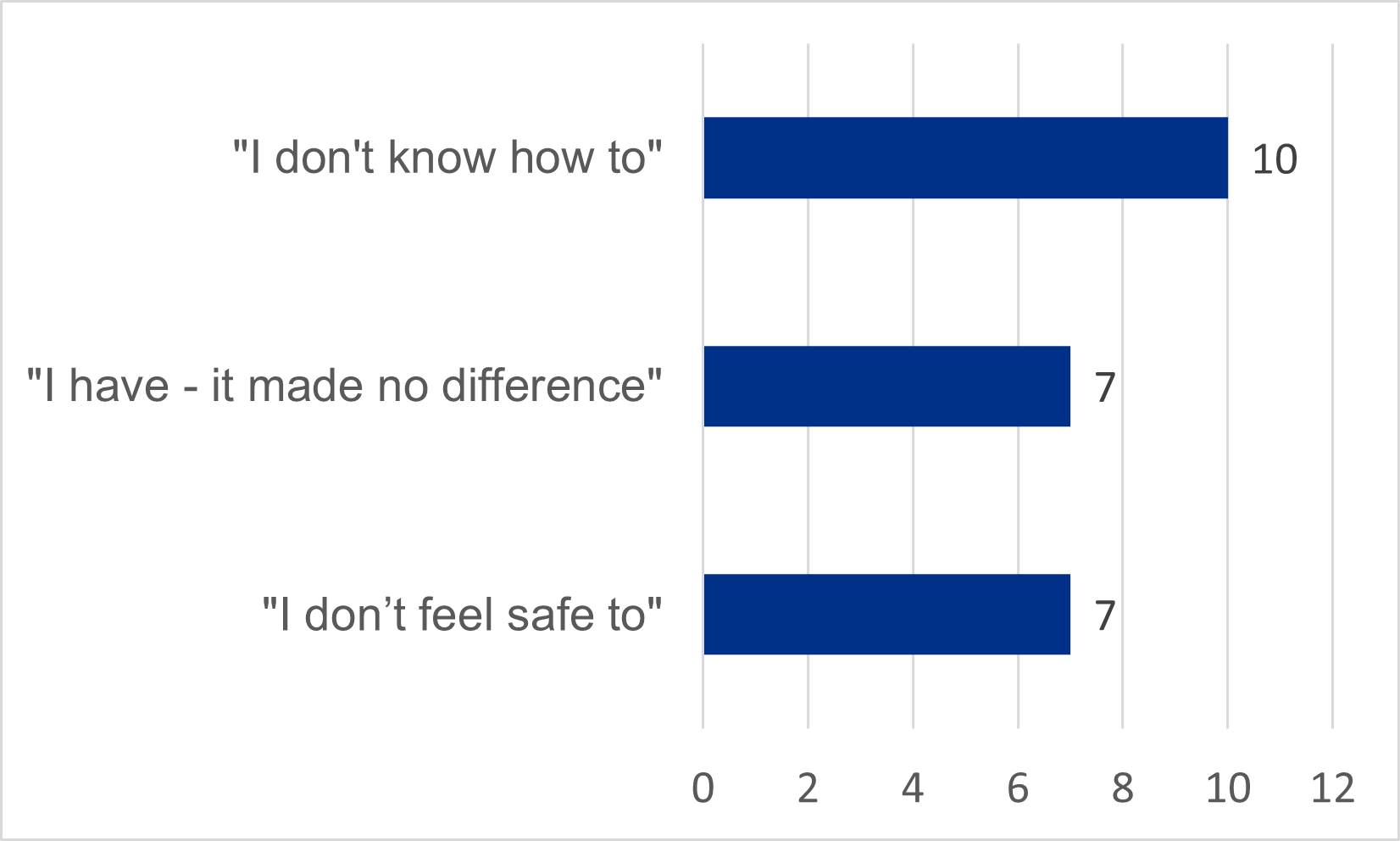
Figure 7 shows the top 3 reasons for speaking up to NHS England in primary care and the number of people who gave these reasons.. This includes:
- “I don’t know how to”: 10
- “I have – it made no difference”: 7
- “I don’t feel safe to”: 7
Within primary care, the most common reason for speaking up to us was a lack of knowledge about how to speak up within their organisation.
The small number of workers speaking up on ICB-related issues made it difficult to find a pattern, but a mixture of fear of speaking up internally, poor experiences of having done so in the past and feelings of futility about speaking up internally were reported.
We received a disclosure about the way a GP practice was managing break times and annual leave, with apparent disparities between different ethnic groups. The worker was new to the practice and were not sure how to raise the issue. We signposted the worker to advice and support, and they came back a few weeks later to say they had resolved the issues within the practice.
The NHS England Freedom to Speak Up team will review the reasons why workers speak up to NHS England and make recommendations to NHS organisations about how to improve their speaking up functions.
Improving the experience of workers speaking up to NHS England
Improving our own processes
We recognise that the speaking up process can be a stressful for those involved. Over the past 6 months, we have worked to improve our processes by strengthening triage and decision-making and ensuring more senior oversight of the most complex cases. We have worked closely with leads in each NHS England region on the new approach and will be rolling out and testing it over the next 12 months.
Ensuring all NHS workers know how to speak up
We have asked ICBs to ensure their Freedom to Speak Up arrangements provide safe routes for speaking up and to ensure all providers within their systems (including primary care) adopt the national template Freedom to Speak Up policy.
NHS England has also asked ICBs to consider how they will ensure all primary care workers have access to safe routes for speaking up and ensure they feel safe to use them.
Publication reference: PRN01398

