Introduction
As part of the NHS Oversight Framework (NOF), NHS England will assess NHS trusts’* capability, using this alongside providers’ NOF segments to judge what actions or support are appropriate at each trust. As a key element of this, NHS boards will be asked to assess their organisation’s capability against a range of expectations across 6 areas derived from The insightful provider board, namely:
- strategy, leadership and planning
- quality of care
- people and culture
- access and delivery of services
- productivity and value for money
- financial performance and oversight
These will inform a self-assessment which is intended to strengthen board assurance and help oversight teams take a view of NHS trust capability based on boards’ awareness of the challenges their organisations face and subsequent actions to address them. The purpose of this is to focus trust boards’ attention on a set of key expectations related to their core functions as well as encourage an open culture of ‘no surprises’ between trusts and oversight teams. NHS England regional teams will then use the assessment and evidence behind it, along with other information, to derive a view of the organisation’s capability.
This document is designed to help boards make this self-assessment, set out the process and what organisations can expect along the way.
* NHS trust is used throughout this document to refer both to NHS trusts and NHS foundation trusts. The expectations set out in the document apply equally to both types of organisation.
The self-assessment
This process set out here should not be seen as a ‘tick box’ exercise. As outlined above, the purpose is to promote self-awareness and transparency at NHS trust boards regarding their organisation’s capabilities, strengths, weaknesses and the challenges they face. It also provides a consistent framework for regional oversight teams to engage with NHS trusts, identify key risks and, over time, assess management’s track record in delivering performance and/or identifying and addressing issues to ensure strong, sustainable organisations able to deal with challenges as they emerge. Trusts will have 8 weeks to carry out this self-assessment and return it to regions.
Where boards already conduct effectiveness reviews, they should consider the degree to which these overlap with this self-assessment. In addition, and to avoid duplication, relevant evidence gathered to support NHS trusts’ annual governance statements can also support the self-assessment.
Summary of the capability assessment cycle
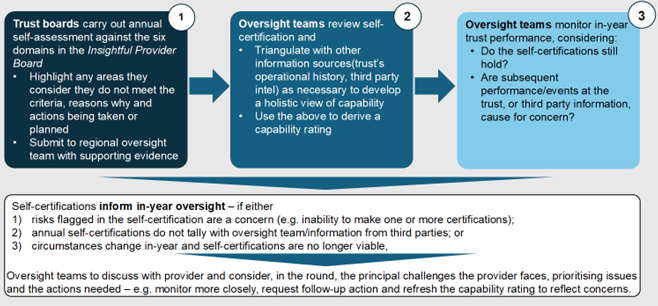
Figure.1: the capability assessment process
Accessible text:
Figure 1 above sets out the self-assessment process which will take a number of stages across the year:
1. NHS trust boards carry out an annual self-assessment against the 6 domains in The insightful provider board and:
- highlight any areas for which they consider they do not meet the criteria, the reasons why and the actions being taken or planned then, within 2 months
- submit the completed self-assessment template to their regional oversight team with supporting evidence
2. Oversight teams review the self-assessment and:
- triangulate this with other information including the trust’s recent operational history and track record of delivery and third-party intelligence (see below) as necessary to develop a holistic view of capability
- assign a capability rating to the trust
Oversight teams will discuss the capability rating with the NHS trust and consider, in the round, the principal challenges the organisation faces, prioritising issues and the actions needed – for example, monitor something more closely, request follow-up action(s) and/or refresh the capability rating to reflect concerns if necessary.
3. Oversight teams will, across the financial year, use the capability assessment to inform oversight, for example where:
- risks flagged in the self-assessment are a concern (for example, inability to make 1 or more certifications), or
- annual self-assessments do not tally with oversight team’s views or information from third parties, or
- subsequent performance/events at the trust or third-party information are a cause for concern such that elements of the self-assessment are no longer valid and, in order to assess ‘grip’, teams may wish trusts to review the basis on which they made the initial assessment.
The self-assessment
Below we provide indicative examples of the evidence boards should use or lines of enquiry they might consider taking to assess whether they can positively self-certify against each criterion. These should not be seen as exhaustive, and we expect trusts will have developed specific approaches to gain assurance in particular areas.
I. Strategy, leadership and planning
|
Self-assessment criteria |
Indicative evidence or lines of enquiry |
|
1. The trust’s strategy reflects clear priorities for itself as well as shared objectives with system partners. |
|
|
2. The trust is meeting and will continue to meet any requirements placed on it by ongoing enforcement action from NHS England.
|
|
|
3. The board has the skills, capacity and experience to lead the organisation. |
|
|
4. The trust is working effectively and collaboratively with its system partners and NHS trust collaborative for the overall good of the system(s) and population served. |
|
II. Quality of care
|
Self-assessment criteria |
Indicative evidence or lines of enquiry |
|
5. Having had regard to relevant NHS England guidance (supported by Care Quality Commission information, its own information on patient safety incidents, patterns of complaints and any further metrics it chooses to adopt), the trust has, and will keep in place, effective arrangements for the purpose of monitoring and continually improving the quality of healthcare provided to its patients. |
|
|
6. Systems are in place to monitor patient experience and there are clear paths to relay safety concerns to the board. |
|
III. People and culture
|
Self-assessment criteria |
Indicative evidence or lines of enquiry |
|
7. Staff feedback is used to improve the quality of care provided by the trust. |
|
|
8. Staff have the relevant skills and capacity to undertake their roles, with training and development programmes in place at all levels. |
|
|
9. Staff can express concerns in an open and constructive environment. |
|
IV. Access and delivery of services
|
Self-assessment criteria |
Indicative evidence or lines of enquiry |
|
10. Plans are in place to improve performance against the relevant access and waiting times standards. |
|
|
11. The trust can identify and address inequalities in access/waiting times to NHS services across its patients. |
|
|
12. Appropriate population health targets have been agreed with the integrated care board. |
|
V. Productivity and value for money
|
Self-assessment criteria |
Indicative evidence or lines of enquiry |
|
13. Plans are in place to deliver productivity improvements as referenced in the NHS Model Health System guidance, the Insightful board and other guidance as relevant. |
|
VI. Financial performance and oversight
|
Self-assessment criteria |
Indicative evidence or lines of enquiry |
|
14. The trust has a robust financial governance framework and appropriate contract management arrangements. |
|
|
15. Financial risk is managed effectively and financial considerations (for example, efficiency programmes) do not adversely affect patient care and outcomes. |
|
|
16. The trust engages with its system partners on the optimal use of NHS resources and supports the overall system in delivering its planned financial outturn. |
|
Inability to make a positive self-assessment
The board may not be able to make a positive self-assessment either because it considers the risks in a specific area are too great or its organisation is already manifestly failing in a specific area (for example, delivering on access targets). In these situations – and in line with the ‘no surprises’ ethos – in the self-assessment template boards should provide:
- the reasons why a positive self-assessment cannot be made against specific criteria and the extent to which these have been outside the trust’s control to address (for example, industrial action, system-wide factors)
- how long the reasons have persisted
- a summary of any mitigating actions the trust has taken or is taking
- if not already shared with oversight teams, a high-level description of trust plans to address the issue, how long this is likely to take and KPIs or other information the trust will use to assess progress
Oversight teams will use this information to form their view of the overall capability of the trust and tailor their oversight relationship with it.
Material in-year changes
In addition to the annual self-assessment, if the board becomes aware in-year of a significant change to its ability to meet any of the self-assessment criteria – for example, an external report reveals material quality risks or an unforeseen cost will affect its financial performance – it should inform the oversight team along with the actions it is taking to address the issue. Such in-year changes will likely inform the ongoing regulatory relationship with the NHS England region.
The NHS provider trust capability rating
Regional oversight teams will review the trust’s submitted self-assessment and consider the statements and evidence. Using a range of considerations, including the historical track record of the trust, its recent regulatory history and any relevant third-party information, the oversight team will decide the trust’s capability rating and share this with it, including the rationale for the rating.
Rating: Green
- High confidence in management.
Indicative criteria
- No concerns evident from the self-assessment or subsequent performance.
- No concerns arising from third-party information.
- High confidence in the trust’s ability to deliver on its priorities based on track record over past 12–24 months.
Rating: Amber–green
- Some concerns or areas that need addressing.
Indicative criteria
- After discussion with the trust, some concerns emerging across more than 1 domain, but these as yet are not affecting quality of care, delivery of core services, finance or the wider reputation of the NHS.
- Trust has prepared plan(s) to address any problems with associated timeframe for delivery.
- Historical issues/track record mean NHS England does not (yet) have full confidence in the board.
Rating: Amber–red
- Material issue needs addressing or failure to address major issues over time.
Indicative criteria
- Issues with self-assessment or subsequent issues across multiple domains.
- Failure to deliver on agreed plans to address a material issue.
- Potentially in breach of licence.
Rating: Red
- Significant concerns arising from poor delivery, governance and other issues.
Indicative criteria
- Material or long-running concerns at the organisation that management has been unable to grip.
- NHS trust in breach of licence or likely to be.
Third-party information
As set out in the NHS Oversight Framework, third-party information relating to the organisation’s governance and risk profile, staff morale and quality of care provided may inform NHS England’s view of NHS trust capability. We expect that where trusts receive information that impacts on their self-assessment they should share this with NHS England. Relevant third parties include:
- other bodies with regulatory responsibilities, where concerns can reflect weaknesses in internal governance and systems of internal control and oversight – including the Information Commissioner, Human Tissue Agency and NHS Blood and Transplant
- professional representative bodies, reflecting issues with working conditions, staff morale, operating culture and safety – including the General Medical Council, Nursing and Midwifery Council and Royal Colleges
- patients and the public, reflecting issues in areas such as patient experience and culture via groups like Healthwatch
- staff information, reflecting issues in internal culture and inability to speak up, for example via staff survey or whistleblowers
- integrated care board partners, covering areas like the trust’s willingness to collaborate and deliver shared goals
- other NHS England teams, reflecting knowledge from central programmes like quality, cyber assurance or digital maturity
- relevant oversight groups, including joint strategic oversight groups (JSOG) and system and regional quality groups
- other sources as relevant to the NHS trust, including coroners, Parliamentary Health Service Ombudsman, local government and Social Care Ombudsman, Ofsted, the trust’s internal and external auditors and even the police
For further information on relevant information from third parties please see annex 1.
Annex 1: Bodies with relevant information on NHS trust capability
NHS England
Responsibilities
- Uses the conditions in the NHS trust licence it issues to NHS foundation trusts (and which also applies to NHS trusts in shadow form) to regulate trusts across a range of areas, including delivery of services, quality governance and efficiency, economy and effectiveness of management.
- Oversees the training of healthcare staff. Trusts liaise with it on matters like resident doctor training and NHS England has the power to remove resident doctors from trusts if conditions are unsatisfactory.
- Operates a cyber assurance service to build cyber security across the NHS, assessing alignment to key standards relating to the cyber assessment framework and indicators of good practice.
Considerations/areas to look at for NHS trust capability
- Meeting national standards.
- Compliance with the NHS trust licence.
- Resident doctor survey.
- Delivering NHS objectives.
- Collaborating with NHS trusts.
- Cybersecurity.
Care Quality Commission
Responsibilities
- Registers organisations to provide care in England, sets regulations covering the care trusts provide, runs an inspection and monitoring regime and publishes NHS trust ratings.
With NHS England:
- Provides joint strategic leadership and alignment for quality through the National Quality Board (NQB).
- As co-signatories of the NQB guidance for system quality management, work together as part of a culture of open and honest co-operation to identify opportunities for improvement, early warning signs, concerns and risks, and take collaborative action, working with systems to mitigate and manage quality.
- Ensures coherent oversight arrangements are in place for systems, integrated care boards (ICBs) and NHS trusts to ensure services are safe and effective.
- Shares learning and information about quality risks/concerns in a timely and proactive way, through system quality groups, regional quality groups and wider discussions, and respecting regulatory frameworks.
Considerations/areas to look at for NHS trust capability
- Quality of care – are any sites or services operated by the NHS trust classed as ‘inadequate’?
- Governance and culture – are there concerns for NHS England arising from the CQC’s well-led review across the whole organisation?
Medicines and Healthcare products Regulatory Agency
Responsibilities
- Regulates medicines, medical devices and blood transfusion components.
Considerations/areas to look at for NHS trust capability
- Systems in place to ensure proper and safe use of medical equipment.
Human Tissue Authority
Responsibilities
- Regulates the removal, storage, use and disposal of human bodies, organs and tissue.
Considerations/areas to look at for NHS trust capability
- Systems in place to safely and legally handle human tissue.
The Human Fertilisation and Embryology Authority
Responsibilities
- Regulates and inspects all clinics in the UK providing in vitro fertilisation (IVF), artificial insemination and the storage of human eggs/sperm/embryos – this may include some trusts.
Considerations/areas to look at for NHS trust capability
- Systems in place to meet standards associated with IVF and related procedures.
The Health and Safety Executive
Responsibilities
- Has a national remit over matters like workplace safety, estates conditions which covers trusts.
Considerations/areas to look at for NHS trust capability
- Systems in place to ensure staff, patients and the public work in a safe environment.
The Information Commissioner’s Office
Responsibilities
- Has a national role to uphold information rights in the public interest May be in contact with trusts regarding patient confidentiality, for example setting data requirements.
Considerations/areas to look at for NHS trust capability
- Systems in place to manage data securely and in compliance with all relevant standards.
NHS Counter Fraud Authority
Responsibilities
- Investigates reports of fraud, bribery and corruption across the NHS.
Considerations/areas to look at for NHS trust capability
- Systems and culture in place to ensure zero tolerance of fraud, bribery and corruption at the NHS trust.
Professional regulators
- General Medical Council
- Nursing and Midwifery Council
- General Chiropractic Council
- General Dental Council
- General Optical Council
- General Osteopathic Council
- General Pharmaceutical Council
- Health and Care Professionals Council
- Social Work England
Responsibilities
- Together with NHS England, ensure proper standards of practice in respective professions to protect, promote and maintain the health and safety of the public.
- Most have responsibilities across the UK and all regulate professionals regardless of whether they work in the NHS or the independent sector.
- As a designated body, NHS England has a statutory duty under the responsible officer regulations for GPs on the national performers list and for responsible officers from designated bodies across a wide variety of sector organisations.
- NHS England must inform professional regulators where professionals fail to meet the standards. This can lead to an investigation and potentially sanctions such as conditions on practice, suspension or removal from a professional register.
- Responsible for quality assuring the education and training of healthcare professionals. Most can inspect organisations that commission, oversee or provide education, and they have powers to withdraw approval from training programmes, posts or NHS trusts if they are not satisfied that education or training is being provided in a safe or effective way. In April 2023, NHS England took on the previous powers of Health Education England to regulate training NHS trusts and placement hosts.
Considerations/areas to look at for NHS trust capability
- Staff can work in and contribute to a safe, sustainable environment that ensures good morale and a healthy working culture that supports high quality care.
Local government and Social Care Ombudsman
Parliamentary and Health Service Ombudsman
Responsibilities
- Provide an independent complaint handling service.
Considerations/areas to look at for NHS trust capability
- Evidence of patient or staff concerns at health and care NHS trusts.
Health Service Safety Investigations Body
Responsibilities
- Investigates serious patient safety risks that span the healthcare system, operating independently of other regulatory agencies.
Considerations/areas to look at for NHS trust capability
- Quality assurance arrangements at NHS trusts.
Healthwatch
Responsibilities
- Shares learning and information through system quality groups, regional quality groups and the NQB to ensure that the views and experience of people and the public informs quality improvement and risk management discussions.
- Note: The Dash Review recommends abolishing Healthwatch. If followed through, this will need to go through a number of steps before being enacted in legislation, likely in late 2026/early 2027. Until then, Healthwatch will continue to gather patient views and evidence and work together with NHS trusts and commissioners to improve local services.
Considerations/areas to look at for NHS trust capability
- The NHS trust uses patient and public information in reviewing the care provided at the organisation.
- Is there any evidence of patient concerns that might indicate issues with the provision and oversight of care provided?
Ofsted
Responsibilities
- Inspects education settings, including secure children’s homes and SEND services.
Considerations/areas to look at for NHS trust capability
- Is there any evidence of patient concerns that might indicate issues with the provision and oversight of care provided at specific sites managed by the NHS trust?
Coroners
Responsibilities
- Coroners investigate deaths that are unnatural or violent or where the cause is unknown or that took place in prison, police custody or another type of state detention, such as a mental health hospital.
Considerations/areas to look at for NHS trust capability
- Is there any evidence of concerns or issues – for example, organisational culture or governance – that may have led to a death at the institution?
Royal Colleges
Responsibilities
- The professional bodies that oversee and regulate various medical specialties. These colleges set standards for training, examinations, and continuing professional development for doctors in their respective fields. They also play a role in policy and advisory work related to their specialties.
Considerations/areas to look at for NHS trust capability
- Do information from Royal Colleges – for example, anonymised data from surveys of their members – highlight cultural, quality of care or patient safety concerns at the trust?
Local authorities
Responsibilities
- Along with other roles, local authorities help develop the population health needs assessment. Trusts are expected to work with system partners to meet these needs.
Considerations/areas to look at for NHS trust capability
- Is there any evidence that the trust is not an effective system partner across its geography?
Publication reference: PRN01888_i

