Introduction
One obstacle to eliminating unwarranted variation in the distribution of nursing and non-registered staff across and within the NHS provider sector has been the absence of a single means of consistently recording, reporting and monitoring staff deployment.
Lord Carter highlighted this issue in his February 2016 report, Operational productivity and performance in English NHS acute hospitals: unwarranted variations. This led to the development of benchmarks and indicators to enable comparison across peer trusts as well as wards and to the development of the care hours per patient day (CHPPD) measure in line with the second of Lord Carter’s recommendations.
CHPPD has since become the principal measure of nursing, midwifery and healthcare support staff deployment on inpatient wards. It has now expanded to include all ward-based clinical professionals who are budgeted to the ward establishment and rostered into the 24/7 roster. This is important for considering how best to use staff to meet patient need, and it will be crucial for getting an integrated view of the staffing required to deliver patient care.
CHPPD has been developed since its introduction in April 2018. Then, it focused on acute and acute specialist trusts:
- including all inpatient areas that provide care over a 24-hour period but not accident and emergency departments
- excluding ward-based areas in community hospitals that provide day care/day-case services – for example, day surgery and other
Now, this updated guidance also includes community and mental health trusts, a wider workforce that includes registered and non-registered allied health professionals (AHPs), and all registered and non-registered nursing associates (NAs). CHPPD must include:
- all clinical staff within the ward establishment and budget who are rostered and contribute to care provision
- this may include specific roles such as enhanced care, facilitating patient groups, or other activities, including ward leadership.
CHPPD should not include:
- ward-based areas in community hospitals that provide day care/day-case services (eg day surgery and other diagnostics)
- it should not include professionals who deliver interventions to patients on the ward but work across several wards/services/pathways and therefore are not rostered as part of the ward
All trusts must submit CHPPD data via the Strategic Data Collection Service (SDCS).
What is CHPPD?
CHPPD is a measure of workforce deployment that can be used at ward level and service level or be aggregated to trust level.
It provides a view of all professions that deliver care in a ward-based setting and differentiates registered clinical staff from non-registered clinical staff. This ensures skill-mix is well-described and the nurse-to-patient ratio is considered when deploying the clinical professionals to provide the planned care, reflected alongside an aggregated overall actual CHPPD.
CHPPD is formally the principal measure of workforce deployment in ward-based settings and increasingly forms an integral part of a ward/unit/trust review and oversight of quality and performance indicators to inform quality of care, patient outcomes, people productivity and financial sustainability.
CHPPD is most useful at ward level; service leaders and managers can compare workforce deployment over time with similar wards in the trust or at other trusts, as part of a review of staff deployment and overall productivity. This measure should be used alongside clinical quality and safety outcome measures to understand and reduce unwarranted variation, and support delivery of high quality, efficient patient care.
The Model Health System
Monthly CHPPD data is routinely collected, recorded and reported through the Model Health System, available down to ward level for inpatient areas in each acute trust. The Model Health System retrospectively shows CHPPD data obtained from SDCS and safe-staffing monthly returns.
The Model Health System is an online digital tool provided by NHS England and NHS Improvement to help trusts identify and realise opportunities for improvement. It breaks down key metrics across all the activity of a trust.
The Model Health System brings together a wide range of data in one place, covering clinical productivity themes and is improvement-focused.
CHPPD and other nursing metrics are visible to other providers and users and allow trusts to see national comparison and benchmarking against peers. This helps identify and compare a trust’s position and provides insight into ‘what good looks like’ to assist in finding improvement opportunities.
How to calculate CHPPD
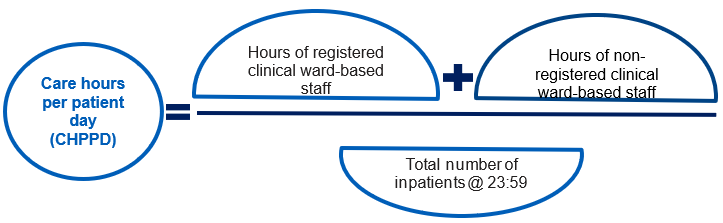
To calculate CHPPD, monthly returns for safe staffing and the daily patient count at midnight (ie the total number of patients on the ward at 23:59) are aggregated for the month. For maternity services, from 1st April 2021, the total number of patients will include babies. This will include transitional care areas and should include mothers who are registered as a patient and all babies.
Figure 1: How to calculate CHPPD
Care hours per patient day (CHPPD) = Hours of registered clinical ward-based staff + Hours of non- registered clinical ward-based staff / Total number of inpatients @ 23:59
This data is aggregated daily during the month in question. From this data return, CHPPD is calculated.
The 23:59 census does not fully represent the total and fluctuating daily care activity, patient turnover or the peak bed occupancy. However, it provides a reliable and consistent information collection point and a common basis for productive comparisons to measure, review and reduce variation at ward level within organisations and within similar specialties across different trusts.
Benefits of CHPPD
CHPPD was developed, tested and adopted to provide a single, consistent and nationally comparable way of recording and reporting staff deployment on all inpatient wards across all healthcare sectors.
- CHPPD produces a single comparable figure that represents both staffing levels and patient requirements, unlike actual hours or patient requirements
- It enables wards within a trust, and wards in the same specialty at other trusts, to be compared. As CHPPD is calculated after dividing by the number of patients, the value does not increase due to the size of the ward, enabling comparison between wards of different sizes. It offers the ability to differentiate registered and non-registered clinical staff for reporting purposes, to ensure skill-mix is well-described and the nurse-to-patient ratio is taken account of in staff deployment, along with an aggregated overall CHPPD.
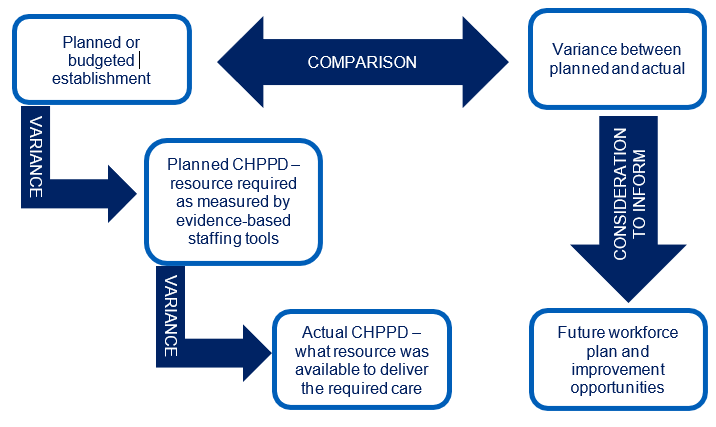
The CHPPD reflected in the planned establishment can be compared with the planned CHPPD on the daily roster, enabling this to be reviewed with what happened (ie the actual CHPPD delivered).
Daily and shift-to-shift considerations enhance CHPPD implementation (see Figure 2 below)
Figure 2: Comparing planned and actual CHPPD
CHPPD is therefore valuable because it consistently shows how well patient care requirements are met alongside outcome measures and quality indicators.
We recommend that organisational policy and practice include assessment of CHPPD, both on an operational basis (daily review and mitigation of planned versus actual) and retrospectively to inform bi-annual ward-level establishment setting, overseen at divisional and trust level.
Organisations best-placed to maximise the benefits of using CHPPD have:
- sound evidence-based establishment-setting processes
- high quality and clinically assured e-rostering
- an aligned process for assessing and recording evidence-based daily and shift-to-shift patient acuity and dependency.
Using CHPPD
Reviewing ward-based CHPPD daily and on an operational shift-to-shift basis can demonstrate the real-time staff deployment in a clinical area.
CHPPD monitoring and tracking can be delivered in or alongside e-rostering software platforms to help assess daily operational staffing requirements.
CHPPD can be used to enhance and strengthen e-rostering improvement efforts by transparently tracking the care hours that the set establishment would yield and comparing this with the care hours that the roster can deliver.
Comparing CHPPD reflected by the set establishment with CHPPD available on the roster can help ward leaders manage workforce to meet patient need. This data, particularly if tracked over time, provides an informative picture of staff deployment. It can be used in productivity and efficiency discussions, as well as highlighting areas that may require establishment setting or skill-mix review.
Important points to consider when using CHPPD as a benchmarking tool
1. CHPPD reported nationally in accordance with the Model Health System:
- Is there a clear process and governance for quality-assuring safe-staffing monthly returns as well as clinically validating them before submission? This will help ensure the accuracy, completeness and robustness of reported CHPPD data.
- Are the ward and specialty names routinely checked so they match other national data returns, and are they consistently referenced across all returns?
- Where there is a legitimate reason for a ward to be renamed, is there a trust process for validating and updating the Model Health System in accordance with the revised change form?
- Is there a way of exploring the level of variation across the trust for nationally reported CHPPD in the Model Health System, and whether this is warranted or unwarranted?
- Is there an understanding of reported CHPPD by ward or specialty compared to national averages and to similar wards at peer trusts?
- CHPPD and establishment setting:
- Are ward establishments set using NICE-endorsed evidenced-based tools such as the Safer Nursing Care Tool (SNCT) and Mental Health Optimal Staffing Tool (MHOST) and other workforce planning tools?
- Are these in line with the National Quality Board’s expectations and that of the Developing Workforce Safeguards guidance then further underpinned by auditable clinical judgement?
- Guidance on safe, sustainable and productive staffing can be found on our website covering:
- Are such tools used consistently and exactly as instructed in the implementation guidance in an auditable manner?
- Is the set establishment – signed off at budget setting by finance, workforce, operational and clinical leads – expressed in terms of care hours (and therefore convertible to CHPPD), to enable comparisons and cross- checking with nationally reported CHPPD?
- CHPPD and rostering:
Planned CHPPD:
- Do trusts have systems and processes to capture the CHPPD planned on their daily roster that has been set by the SNCT to create establishment?
- Can this be reviewed on a shift-to-shift basis?
Actual CHPPD:
- Do trusts have systems and processes to capture the CHPPD delivered on their daily roster?
- Can this be reviewed on a shift-to-shift basis?
- Can this then be compared and tracked against establishment CHPPD?
CHPPD and daily acuity and dependency:
- Reviewing CHPPD on a daily and shift-to-shift basis where systems are locally available can form a transparent and helpful basis for levelling and redeploying staff between wards.
- Daily and shift-to-shift comparisons, auditable, evidence-based methods that are clinically assured and clearly aligned with guidance are required to capture patient acuity and dependency.
6. Future CHPPD considerations
Work is ongoing to consider how patient acuity and dependency can be integrated into CHPPD calculations for all areas currently using CHPPD. This would include adding a required CHPPD which is based on evidence based classification of patient acuity and dependency. There is also exploratory work looking at the efficacy of linking CHPPD to specific patient outcomes
There is also work ongoing to develop a Care Hours Per Patient Attendance (CHPPA) metric for Emergency Departments.
7. SDCS return CHPPD
All trusts are required to submit CHPPD data to the Strategic Data Collection Service (SDCS).
Timeframes
This is a monthly data collection that must be returned by 12 noon on the 11th working day of the subsequent month. It will be posted and made available in the Model Health System in the month following submission. For example, data for 1 to 28 February 2023 had to be returned by 12 noon on 15 March 2023 and was posted in the Model Health System in April 2023.
Data extraction and entry
For ease of data extraction from your e-rostering systems, ensure you have configured the templates to map to the data points required. This will enable more accuracy of data extraction and lessen burden of additional separate entries. It is also useful to check Electronic Patient Record (EPR) for fluctuation in bed numbers to ensure escalations can be accurately reflected in the CHPPD outcomes.
SDCS template
- The template for inputting the data can be downloaded from the SDCS Check the ‘News’ section on SDCS for updates.
- Enter data in the white cells. The values in green cells will be calculated automatically from the data
To upload data to SDCS, which is run by NHS England, trusts should contact Data.Collections@nhs.net to obtain a username for the system. Full instructions and guidance will then be provided.
The upload template is called Safe Staffing (Rota Fill Rates and CHPPD Collection).
Should your query be of a technical nature, contact nhsi.modelhospitaloperations@nhs.net
Contact details
For all questions about this guidance, or the current or future collection, please contact The Model Health System team.
8. SDCS template explanations and definitions
|
Number |
Term |
Explanation/definition |
|
1 |
Reporting period |
The calendar month. |
|
2 |
Hospital site code |
Select your hospital site code from the dropdown box. All hospital sites can be added to one overall return for each trust. |
|
3 |
Ward name |
Enter the ward name or number. All wards with inpatient beds and delivery suites must be included, except:
We are considering workforce productivity measures for these currently excluded areas to improve productivity and enable transparent comparisons. Please ensure that each ward name for data submitted for the safe-staffing return is consistent with the ward names used on the Friends and Family Test and Safety Thermometer submissions, so it matches NHS Choices, My NHS and the Model Health System. Please do not use abbreviations. If ward names cannot be aligned, CHPPD data may not be reportable. If ward names or ward specialty codes are changed, the ward will be reported as a new ward and you will not be able to compare trend. |
| 4 | First specialty | Select the first specialty for the ward from the dropdown box. |
| 5 | Second specialty | If there is more than one, select the second specialty for the ward from the dropdown box. Enter data for the whole ward. If the ward covers more than two specialties, please select the two for which there are most patients. |
| 6 | Night | The shift period within which midnight falls. |
| 7 | Day | All periods not included in the night shift. |
| 8 | Registered nurse/midwife | A member of registered nursing or midwifery staff on the duty rota dedicated to the inpatient area. Include all such staff. |
| Nursing associates | The role is a new generic nursing role in England that bridges the gap between health and care non-registered workers and registered nurses, to deliver hands-on care for patients as part of the nursing. | |
| Registered AHPs | A registered AP on the duty roster dedicated to the inpatient area. This could include (but is not limited to): occupational therapists physiotherapists speech and language therapists dietitians. | |
| Non-registered AHPs | A non-registered staff member on the duty roster dedicated to the inpatient area with delegated responsibility from a registered AHP. This includes: · activity co-ordinators · occupational therapy assistants · peer support workers · physiotherapy assistants speech and language therapy assistants. | |
| 9 | Non-registered nursing | Include any non-registered clinical staff on the duty rota dedicated to the inpatient area who have delegated responsibility from a registered nurse/midwife. Examples are:
|
| 10 | Assistant practitioners | Workers who deliver health and social care with a level of knowledge and skill beyond that of a traditional healthcare assistant/support worker. They are currently excluded from the returns; further guidance will follow the conclusion of national pilots. |
| 11 | Students | Students are excluded. |
| 12 | Total monthly planned staff hours | Enter the total monthly planned hours for:
|
| 13 | Total monthly actual staff hours | Enter the total monthly actual hours worked (paid) for:
|
| 14 | Patient count at midnight | Enter the number of patients (both mother’s and babies in maternity services and transitional care units) on the ward at 23:59 on the date of the shift (trusts will need to add together each day within the month for the return) Include patients who are being cared for in other health facilities by your ward staff. Do not include patients ‘on leave’. |
| 15 | CHPPD | This information is automatically calculated from the data entered on the template. The CHPPD is calculated by taking the actual hours worked divided by the number of patients at midnight split by all clinical ward established workforce (registered and non-registered). |
| 16 | Staff to be included | Count in all staff on the duty rota dedicated to the inpatient area. This includes: · all registered clinical workforce who are embedded and working on the ward as part of the establishment multidisciplinary team on the duty rota dedicated to the named inpatient area · all non-registered clinical workforce on the duty rota dedicated to the inpatient area; this includes: – ward co-ordinators – staff rostered from a pool – staff specifically booked to provide escorts – staff who are providing enhanced care and supervision to patients being nursed in alternative settings such as an acute/community trust – staff who are booked to ‘escort patients’ – staff working additional hours on top of their booked shift should have their extra hours included – bank and agency staff – nursing assistants – midwifery assistants – healthcare assistants – support workers – OT assistants – physiotherapy assistants – dietetic assistants activity co-ordinators. |
| 17 | Exclude staff not included on the staff duty rota – usually:
|
9. SDCS template supporting information
Wards closed at midnight: For wards closed at night that have zero patients at midnight, log the patient count as zero.
Permanent ward closures: If a ward is permanently closed, the ward should no longer be reported, and you should remove this ward from NHS Choices. The person in your organisation who has editor’s permissions to amend the NHS Choices system must do this.
Temporary ward closures: If a ward has a temporary planned closure partway through the month, the planned and actual staffing days when the ward is open should be reported as normal. The actual and planned-for days when the closure occurs should be recorded as zero. Reflect the variance in the staffing and patient count in the monthly submission, with the reason for it.
Mixed in/day/out/patient wards: If the ward is a mixed inpatient and day patient/outpatient unit, include only those staff delivering inpatient care. We are carrying out further analysis to find a more appropriate solution where this may not be possible. Please indicate where this is the case on the returns.
External staff: Include external staff hours if they support care of inpatients for more than two hours.
Publications approval reference: B0473