Introduction
This guide supports systems and trusts with the clinical prioritisation of their routine dermatology outpatient waiting lists. A focus on clinical prioritisation contributes to a reduction in the number of long waiting patients. This is a key priority supporting delivery of the NHS elective recovery plan.
The guide outlines an approach, based on a model used by the NHS England national clinical prioritisation programme, to identify those patients whose skin condition has deteriorated while waiting and most urgently need to be seen, and those whose skin condition has resolved and no longer require a consultation.
The guidance has been developed with stakeholders including Getting It Right First Time (GIRFT), clinicians, relevant professional bodies, such as the British Association of Dermatologists (BAD), Primary Care Dermatology Society (PCDS), British Dermatological Nursing Group (BDNG) and organisations that represent the views and interests of people with lived experience, including the National Eczema Society, Vitiligo Support UK and Psoriasis Association UK.
We recommend that this validation and clinical prioritisation approach to patients on routine dermatology waiting lists should be part of the wider recovery and transformation of dermatology outpatient pathways. In particular, it should be used in conjunction with implementing the use of specialist advice to optimise new referral activity, the redesign of the two-week wait (2WW) suspected skin cancer referral process, the Faster Diagnosis skin cancer pathway, patient initiated follow-up, the teledermatology roadmap, Ensuring equity of access to care when designing dermatology pathways and the Getting It Right First Time (GIRFT) pathways, all of which will help ensure that patients are seen at the right time, in the right place and by the right person.
Dermatology recovery: aims, benefits and principles
Aims
The dermatology recovery approach aims to:
- ensure only patients who require an appointment remain on the waiting list
- prioritise patients for outpatient appointments appropriately
- support providers in validating waiting lists for those waiting for routine, first dermatology outpatient appointments
- update patients on the waiting list about their options and support mutually agreed decisions about next steps
- manage clinical risk effectively and improve clinical outcomes
- prioritise high risk patients or those with potentially cancerous lesions on elective pathways based on appropriate validation steps (see Cancer waiting times monitoring dataset guidance, v11).
Clinical prioritisation programme principles
- Patients referred for a specialist dermatology opinion should be prioritised according to clinical need rather than waiting time. This is particularly necessary for skin conditions where the earlier the intervention the better the clinical outcome.
- Special consideration should be given to those patients on an elective skin lesion pathway who with revalidation are identified to be at risk of cancer.
- Patients on the waiting list should be reviewed by taking a holistic approach to their care and considering any alternative pathways that are appropriate, available and with capacity, eg intermediate or community dermatology services.
- Agreement of core principles between specialist and primary care providers is key to the success of clinical prioritisation.
- Dermatology teams that have already started prioritising their waiting lists and can demonstrate efficacy of their approach should not stop doing so; they should share their experience with others.
- Consideration should be given to narrowing health inequalities and certainly ensuring that the process does not widen these, in particular where teledermatology is used to support clinical prioritisation.
- The patient’s legal right to choice of provider must be maintained.
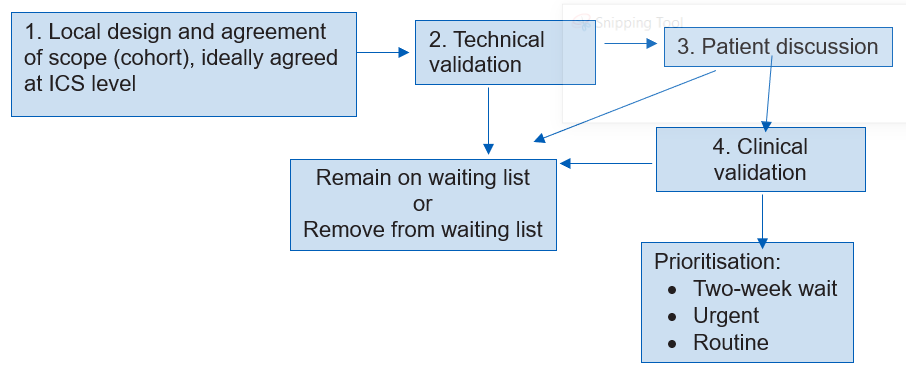
Stages of validation and prioritisation
The stages of the process are:
1. Agreement of scope
Scope will need to be determined locally in line with national clinical guidance to target patients deemed at higher risk, and agreed at integrated care system (ICS) level. Local systems will need to consider:
- Should all patients be reviewed or only those waiting longer than 52 weeks in the first instance?
- Is it appropriate to look at a particular group of patients, eg those with rashes or those with skin lesions? This would require a preliminary assessment of all referrals to group them appropriately.
- Are there patients on the waiting list who need to be identified because deterioration of their skin disease may have serious long-term consequences, eg delay in treating patients with basal cell carcinoma may mean they need a more invasive surgical procedure, or life-long scarring for those with inflammatory skin conditions?
2. Technical validation
Technical validation is the review and correction of data quality issues and potential errors, to provide as accurate and up-to-date a list as possible for clinical review. This validation process should include checking patient details such as contact information. Safety-netting systems must be in place to ensure that patients for whom information is missing or inaccurate are not ‘lost’ at this stage. Wherever possible, patient communication preferences should be documented so that these can be respected during the next stages of the validation process.
More information can be found in the Validation toolkit and guidance.
3. Patient discussion (administrative validation)
Once technical validation is complete, a list of patients will be created and these patients contacted in their preferred way by a locally agreed team to find out whether/how their skin problem has changed since they were referred for a specialist opinion and establish their preferred next steps. This is the patient discussion (administrative validation). Patients need to be made aware that this is a non-clinical interaction and that they should not expect clinical advice.
Patients will be sent information about the process of waiting list prioritisation and validation. An example letter is included in Appendix 1. Local providers will develop clear operating guidance for this process, ensuring appropriate follow-up of non-responders and that local safeguarding policies are followed.
Members of the locally agreed team will be competent to follow a scripted conversation with patients. They need:
- good communication skills
- good understanding of the relevance of clinical need and its link to validation and prioritisation
- ability to use relevant technology and systems.
The script needs to be locally agreed; Appendix 2 provides an example. The introductory statement should make it clear that the purpose of the patient discussion is to obtain an update about the patient’s skin problem, and should capture whether:
- the patient still wants to see a dermatology specialist
- the skin condition is the same, worse or better than when the patient was referred for a specialist appointment
- the skin lesion/mole has changed colour, size or shape, or been bleeding, itchy or crusting
- the patient has needed to seek advice from their GP practice about their skin condition/lesion since they were referred
- the patient’s work and lifestyle, family and carers, sleeping, etc have been affected by their condition
- the person can take and send photographs of their skin condition or travel to an agreed location to have photographs taken.
Where possible the script should include closed questions with a choice of answers that will act as markers for the severity of disease and link to the important points for the prioritisation process. Mental health and wellbeing questions should be included.
Patient will be asked to decide if they want to either:
- remain on the waiting list
or
- decline the appointment and be removed from the waiting list. Care will be returned to their primary care team who will be informed of this decision.
The record/pathway documentation will be amended accordingly.
To inform their decision patients should be given some idea of the waiting time for a routine referral and assurance that they will be advised of the prioritisation of their referral once the process is complete. This will be one of the following: upgrade to the urgent suspected skin cancer pathway (currently known as the 2WW pathway), urgent or routine appointment, discharge to primary care.
Patients should be informed that they are free to change their minds (within the timeframe stated by local access policies) and trusts should consider providing a dedicated contact telephone number and/or email for them to inform the service that they wish to do so.
Special consideration should be given to patients with skin lesions (who may have skin cancer) and it may be appropriate to ask all such patients to send images of their lesion and automatically consider them for clinical review – see the teledermatology roadmap for supporting guidance.
As soon as possible after this discussion and within a locally agreed timeframe, the patient should receive a summary communication about the decision, with a copy sent to their primary care team.
A list of patients who require clinical review will then be generated.
4. Clinical review and prioritisation triage
The clinical review process follows, informed by the patient discussion and agreed locally by dermatology providers working in partnership with administrative support staff and representatives from primary care.
The following information will be important to consider:
- Demographic information and the original referral letter, to confirm that the referral meets local referral guidance and any low priority framework guidance has been considered. (Providers should be mindful of any changes to low priority frameworks implemented while the patient has been waiting to be seen.)
- An idea of whether the patient’s skin condition is the same, worse or better than at the time of referral.
- Whether the patient has needed to contact their primary care clinician about their skin condition since they were referred and if so, roughly how many times.
- Whether the skin condition stops the patient from doing day-to-day activities (eg going to work, looking after family, impact on family and carers, sleep pattern).
- The patient’s ability to take and send photographs of their skin condition, or to travel to have photographs taken and sent securely to the provider.
Prioritisation triage will take place without direct patient interaction. All available information, including outcome of patient discussion, referral letter and recent images where available, will be reviewed, and each patient prioritised to reflect their need and urgency for a face-to-face consultation; this prioritisation will be the same as for newly referred patients.
The process will consider whether a patient could be seen in an intermediate rather than secondary care dermatology service. Secondary care dermatology services may have large numbers of patients on routine waiting lists and limited capacity to take on this clinical prioritisation activity, so the process needs to be as efficient as possible. This activity must be timetabled/job planned as extra direct clinical care, in the same way as specialist advice (advice and guidance).
Once the prioritisation triage process is complete, patients and their GP will be informed by letter about next steps.
Other models may already be in place and working well; these should be continued. Case studies are available on FutureNHS.
Images
The local clinical team may decide that recent clinical images from the patient would help validation and prioritisation. Systems will need to agree:
- who will take the images and where: patient, primary care setting, community image taking hub or specialist-led image taking hub
- how the images will be sent securely to the provider, stored and collated with the other patient information before clinical review.
Patients will need to be given information explaining why they are being asked for images and how these will be used. The teledermatology roadmap provides information about approaches to taking and sending high quality images, and a range of resources are available in the digital playbook and on the BAD website.
Suitably trained members of the clinical team
Providers will need to agree who in the clinical team is suitably trained to undertake the clinical reviews. This may be a consultant, associate specialist, a GP with an extended role (GPwER), an experienced junior doctor under supervision, a dermatology consultant nurse or a clinical nurse specialist with appropriate expertise and experience to perform this task.
The healthcare professional’s skill set should include:
- an excellent knowledge of a broad range of dermatology conditions, with an emphasis on diagnostic skills
- experience of dermatology clinical triage, including reviewing and grading dermatology referral letters and images
- ability to identify and safety net patients expressing mental health issues, particularly suicidal ideation.
Outcome of the clinical review
Through clinical review the patient will be prioritised using existing priority codes to urgent suspected skin cancer pathway (currently known as the 2WW pathway), urgent or routine or discharge back to primary care, and this and the date of review recorded.
Providers should ensure that a process is in place for patients who need to be seen immediately because their skin problem has deteriorated or their skin lesion needs to be upgraded to an urgent suspected skin cancer referral (currently known as 2WW pathway).
The clinician has the following options:
- expedite the patient’s care to an urgent suspected skin cancer referral (currently known as a 2WW referral)
- arrange an urgent appointment if they have become a higher priority since they were initially referred
- agree that the patient is seen routinely.
The process of validation and prioritisation should safeguard the clinical care of those who need to be upgraded to a suspected skin cancer referral (2WW referral) or seen urgently. Patients and their primary care clinician should be made aware of the decision in writing, and patients clearly informed when they can expect to be seen for review and what to do in the meantime if their problem worsens. A sample letter is available in Appendix 3.
Resources and administrative support
Administration staff
Robust clerical and administrative support systems working closely with the dermatology team are key to successful implementation; clinician time is then only drawn on where this is essential.
Ideally, a designated team of administrative and clerical support staff will undertake the non-clinical aspects of the approach, including contacting patients to ascertain whether they still require a specialist appointment; advising patients about the need for clinical images; setting up the clinical review process; and managing clinicians’ work lists and booking further appointments as required. Clear safety-netting procedures for non-clinical staff, agreed between primary and specialist services, should be in place.
The size of the team and their contractual hours will depend on the number of patients on the waiting list.
Resources for specialist healthcare professional capacity
The clinical review of patients is activity over and above the day-to-day clinical activity of the dermatology team and will need to be resourced appropriately as additional activity. Systems will need a flexible approach to agreeing activity numbers locally; guidance is available from specialist organisations, eg the BAD job planning guidance. Local providers may wish to consider outsourcing this work or incentivising local clinicians to take on additional activity.
Any resulting additional activity, such as clinics or skin surgery lists to see patients within an appropriate timeframe for the priority to which they have been triaged, will need to be resourced in addition to current job planned activity. Where this activity is ‘outsourced’, clear and explicit arrangements should be in place about where clinical accountability for patient care lies.
Resources to support and monitor the process
Providers will need to carefully map the validation process and agree steps with primary care colleagues. The process will be supported by a range of standard template letters that are relevant and specific to the needs of people with skin conditions. Examples might include:
- preliminary letter to patients asking whether they still require a dermatology appointment
- communication to patients who do not respond after an agreed time and appropriate reminders advising them that they have been discharged back to primary care
- information about how patients should send recent images of their skin condition securely, an if they cannot do so the relevant disclaimer needs to be included in patient information
- letter summarising the outcome of the clinical review and how the patient’s referral has been prioritised, and information about what the patient should do if their condition worsens (see appendixes).
Trusts should monitor the process of clinical validation of waiting lists to check no groups are being disadvantaged, with an emphasis on ensuring that all steps have been taken to contact patients before they are discharged from the service.
Standards and proposed metrics to monitor and evaluate outcomes are included in Appendix 4.
A validation toolkit and guidance to support the implementation of validation, with examples and case studies, is available.
Appendix 1: Example letter about process of validation and clinical validation
This example letter can be adapted for local use – download a Word version.
Trust name
Team/directorate
Address 1
Address 2
Postcode
Telephone
Email address
Date
Ref: Patient’s NHS number
Recipient’s name
Address 1
Address 2
Postcode
Private and confidential
Dear [patient’s name]
Important information regarding your dermatology appointment
We are writing to you regarding your referral to our dermatology service. We are very sorry that you have not yet been offered an appointment.
We have arranged for one of our team to call you on [date and time] to discuss your condition and to agree the best next steps.
We are contacting all our patients in this way to be able to prioritise patients appropriately and make sure that those who require an urgent appointment are seen as quickly as possible.
How to prepare for your phone call
Before your phone call with us on [date and time] it would be helpful to think about the answers to the following questions:
- How would you describe your current condition?
- Has your condition changed since you were first referred?
- Do you still want an appointment? If not, why not?
Please have your NHS number to hand when we call if possible – this can be found on the top left-hand side of this letter.
What to do if you have any questions or need to reschedule
If you have any further questions or would like to reschedule the date/time of your phone call please call us on [phone number (including opening hours)] or [email address].
What to do if you no longer need an appointment
We understand your circumstances may have changed whilst you’ve been waiting. If you no longer need an appointment please let us know as soon as possible on [phone number] or [email address].
Your sincerely
[Named contact in service/department]
Appendix 2: Example patient discussion script
This is an example script for trusts to use when contacting patients to find out whether/how their skin problem has changed since they were referred for a specialist opinion. It can be adapted and agreed for local use.
We expect that the usual identity checks will be completed to ensure discussion is with the right patient.
General introduction
Hello, I’m [insert name]. I’m ringing from [insert name of hospital]. I am a member of the dermatology appointments booking team. Do you have time to speak now? YES/NO
If NO, agree a convenient date and time to phone back.
If the answer is YES:
We are very sorry that you are still waiting for an appointment.
I am not a healthcare professional, so I cannot answer any medical questions you may have about your skin condition, but I am calling to find out a bit more about how things are with you and your skin condition.
I will ask you a standard set of questions and keep a record of your answers on our system. I will then pass on the information to our dermatologists to help them decide the best next steps for you and your care. Are you happy for me to proceed?
I will take you through some questions about the skin problem that led to your referral to the dermatology service.
We are contacting all of our patients to ask these questions. Your answers will help us to ensure we see everyone according to their clinical need and in particular make sure that patients who require an urgent appointment are seen as quickly as possible.
Introductory questions
First, I would like to understand the reason you were referred to the dermatologist:
- Do you think you were referred because of a change in a small area of the skin, a lump or bump – what would be called a lesion on the skin? YES/NO/NOT SURE
- Do you think you were referred because many areas or patches of your skin are affected, a skin rash? YES/NO/NOT SURE
- Was it a problem with your hair or nails, or something else? YES/NO/SOMETHING ELSE/NOT SURE
- Do you still want to see one of our dermatology specialists about this skin complaint? YES/NO
- If NO, why? PROBLEM GONE/BEEN SEEN ELSEWHERE/FREE TEXT RESPONSE
- Have you been given a diagnosis for your skin condition? YES/NO
- If YES, free text diagnosis.
Questions for rashes
- Is your skin condition the same, worse or better than when you were referred for a specialist appointment? SAME/WORSE/BETTER/NOT SURE
- Have you needed to contact your GP practice about your skin condition since you were referred? YES/NO
- If YES, roughly how many times?
- If NO, follow up with: Is this because things are better? YES/NO. If NO, follow up with free text reply.
- Does your skin problem stop you from doing anything? YES/NO
- If YES, ask specific questions about whether the problem stops the person doing anything at work, school, caring, hobbies. YES/NO/OTHER
- Does your skin problem affect your sleep, leaving you feeling tired during the day? YES/NO
- Are you using prescribed treatments for your skin condition? YES/NO
- Can you easily obtain prescribed treatments for your skin condition? YES/NO
- Do you feel your skin problem is affecting your mental health, eg making you depressed and/or anxious? YES/NO
- If YES, capture in what way
Question for lesions
- Is the skin lesion growing/changing/staying the same? GROWING/CHANGING/ SAME
- Has the skin lesion been bleeding, itchy or crusting?
Images
It would really help us if we could see some recent photographs of the affected areas of your skin, without these photographs it will be difficult to make a decision about the next steps for your care.
- Do you have a phone, tablet or digital camera that you or someone close to you could use to take photographs of your skin condition? YES/NO
- If YES, we will send you information about how to take the images and how to send them to us. We would be grateful if you could get them to us as soon as possible.
- If NO, please would you be able to travel to [xxx location] to have some photographs taken? YES/NO
Explain next steps
Thank you. I will pass on the information you shared with our dermatologists to help determine the best next steps for your care. They will also look at the:
- initial referral letter we received from your primary care health care professional (eg your GP or nurse)
- images we receive of your skin condition.
We will write to you and your GP practice with a suggested timescale for your appointment and, where appropriate, provide some information about what you and your GP might be able to do to help manage your condition while you wait. It may be more appropriate for you to be seen by a different team/in a different location. If this is the case we will let you know.
We understand your circumstances may change before we contact you. If your symptoms worsen or if no longer need an appointment, please let us know as soon as possible on [phone number].
Thank you for your time.
Appendix 3a: Example letter communicating the outcome of the validation and clinical prioritisation [remain on waiting list]
This example letter can be adapted for local use – download a word version.
Trust name
Team/directorate
Address 1
Address 2
Postcode
Telephone
Email address
Date
Ref: Patient’s NHS number
Recipient’s name
Address 1
Address 2
Postcode
Private and confidential
Dear [patient’s name]
Important information regarding your dermatology appointment
We contacted you recently to discuss your referral for a dermatology appointment. We have now reviewed the original referral letter from your doctor and the recent information you gave when you were contacted by colleagues in our booking team on [date the patient discussion took place]. We have also looked at the recent photographs of your skin that you provided, thank you.
Based on our review of this information, we think the best way forward is for you to remain on our outpatient waiting list.
Our booking team will contact you within [timescale, i.e. the next two months] to offer you an appointment. If you do not hear from us within this time, please contact [telephone number and opening hours] or [email address].
Support for you whilst you wait to hear from us
To help manage your symptoms whilst you wait for your appointment, it is recommended you: [insert recommendations].
In the meantime, if any of your symptoms change or you have any questions please contact us on [telephone number (including opening hours)] or email [email address].
What to do if you no longer need an appointment
If you no longer need an appointment, please let us know using the contact details above.
Your sincerely
[Named contact in service/department]
N.B. A copy of this letter has been shared with your GP.
Appendix 3b: Example letter communicating the outcome of the validation and clinical prioritisation [discharge]
This example letter can be adapted for local use – download a Word version.
Trust name
Team/directorate
Address 1
Address 2
Postcode
Telephone
Email address
Date
Ref: Patient’s NHS number
Recipient’s name
Address 1
Address 2
Postcode
Private and confidential
Dear [patient’s name]
Important information regarding your dermatology appointment
We contacted you recently to discuss your referral for a dermatology appointment. We have now reviewed the original referral letter from your doctor and the recent information you gave when you were contacted by colleagues in our booking team on [date the patient discussion took place]. We have also looked at the recent photographs of your skin that you provided, thank you.
Based on our review of this information, we think that the best way forward for you is to discharge you and transfer you back to the care of your primary care team in [XXX] days. This is because [insert reason here]. Your condition has improved and/or support to manage your condition can be provided by your GP and you do not need to be seen by a specialist at present.
What to do if your condition gets worse
If your condition gets worse, please contact your GP. They will provide you with the care and support you need. Your GP will contact us if they need to.
Your sincerely
[Named contact in service/department]
N.B. A copy of this letter has been shared with your GP.
Appendix 4: Standards and metrics for a dermatology elective recovery service mapped to the guidance
Below is a checklist of processes to support the validation and prioritisation of dermatology waiting lists, with suggested metrics to assess success. You may find this particularly useful where you involve private providers, to ensure relevant checks are in place.
Standard 1: Scope of the validation and prioritisation is agreed
Metrics:
- Has the scope been agreed and clearly stated? YES/NO (urgent suspected skin cancer referrals (currently known as 2WW referrals) should be clearly stated as outside the scope).
- Confirmation with all parties that urgent suspected skin cancer referrals (currently known as 2WW referrals) are outside the scope. YES/NO
- Confirmation that consideration has been given to the potential impact of the process on those who are digitally deprived. YES/NO
- Confirmation that alternative arrangements have been made for those who may not be able to engage in the agreed process so that they are not disadvantaged. YES/NO
Standard 2: Technical validation is completed for all patients
Metrics:
- Has a technical validation been completed of data quality issues and potential errors to provide as accurate and up-to-date list as possible for clinical review? YES/NO
- How many patients were excluded as a result of this measure?
Standard 3: A non-clinical patient discussion takes place
Metrics:
- Has a patient discussion taken place using an agreed script? This is a non-clinical interaction with the patient to understand whether/how their skin problem has changed since they were referred for a specialist opinion. YES/NO
- As a result of the patient discussion, how many patients fall into the following groups:
- wish to remain on waiting list
- declined appointment and removed from waiting list. Care returned to the GP and GP informed of this decision.
- Is there a process in place for non-responders? YES/NO
How many non-responders? - Is a system in place for patients to provide images to support the clinical prioritisation exercise? YES/NO
- What proportion of patients were able to send images?
Standard 4: All patients are clinically prioritised using the original referral letter, the outcome of the patient discussion and relevant up-to-date clinical images where required.
The clinical reason for the prioritisation decision is communicated to the patient and primary care clinician, and stored by the trust that received the referral.
Metrics:
- For the clinical prioritisation, was the following information available? YES/NO for each:
- demographic information
- original referral letter
- outcome of patient discussion
- recent images where relevant and available
- confirmation that the referral meets local referral guidance and any low priority framework guidance has been considered.
- Outcome of the clinical prioritisation. How many patients were identified for each category?
- expedite the patient’s care to an urgent suspected skin cancer referral (currently known as 2WW referral)
- arrange an urgent appointment if they have become a higher priority since they were initially referred
- agree that the patient is seen routinely.
Specific note for outsourced models
Where a secondary care provider outsources elective activity, it must ensure that all relevant information governance standards are met, particularly those relating to documentation of any patient interaction. We expect the above standards will be met.
If, in addition to prioritising the clinical activity, a management plan is agreed for the patient using this ‘virtual model’, the following information should be collected:
- Total number of patients offered a ‘virtual interaction’.
- Number requiring a face-to-face consultation.
- Prioritisation of those requiring a face-to-face consultation: urgent suspected skin cancer (2WW referral), urgent or routine
- Number referred back to the GP with a management plan and discharged from specialist care.
- Confirmation that information about the interaction is communicated to the referring primary care clinician and a statement made about how this takes place.
Confirmation that clinical information and images from the outsourced interaction (including clinical decision-making) are communicated to the referring secondary care organisation and stored in the patient record so that they are accessible in the event a clinical validation or management decision is questioned.
Publication reference: PR1841