1. What is oral medicine?
Version 2, 16 May 2023
1.1 Description of the specialty
Oral medicine is the specialty of dentistry concerned with the care of children and adults with a diagnosis of chronic, and recurrent medically related disorders of the mouth, face and jaws. The specialty of Oral medicine involves diagnosis and non-surgical management of those patients. Oral medicine is the specialty which interfaces between medicine and dentistry.
Oral medicine specialists currently work principally in dental hospitals and university dental schools. In these settings, specialists in oral medicine work alongside other specialists in dentistry and in areas of adult and paediatric medicine including, but not limited to: dermatology, gastroenterology, ophthalmology, immunology, infectious disease, neurology, neurosurgery, pain management, psychiatry and psychology, often as part of multidisciplinary (MDT) clinics.
Related specialties
The specialty of oral surgery deals with the diagnosis and management of pathology of the mouth and jaws that requires surgical intervention and is provided by both oral surgeons and by oral and maxillofacial surgeons (OMFS). This includes dentoalveolar surgery. Management of oral mucosal lesions, orofacial pain and disorders of the salivary glands is also provided by oral surgeons and by oral and maxillofacial surgeons in district general hospitals where there is no formal oral medicine department.
Oral and maxillofacial surgery is concerned with the diagnosis and treatment of diseases affecting the mouth, jaws, face and neck. Consultants in OMFS are trained in all areas of practice within the specialty (including the management of oral surgery and oral medicine conditions) and many develop sub-specialist interests in more than one field.
Oral medicine and oral surgery are classified as dental specialties by the GDC whereas the UK General Medical Council recognises ‘oral and maxillofacial surgery’ as a medical specialty (PDF).
Dental and maxillofacial radiology, oral and maxillofacial pathology and oral microbiology contribute to the oral medicine patient pathway.
1.2 Description of the workforce and training for those who provide oral medicine care
i. General dental practitioners (GDP)
A GDP on the NHS performer list should have the skills to assess and monitor the soft tissues of the mouth and be aware of changes that are not normal anatomy. A GDP should have the competency to manage simple benign oral mucosal problems such as recurrent oral ulceration that responds to simple topical measures. All other mucosal lesions and orofacial pain that a GDP does not feel confident in managing should be referred into an oral medicine department if one is available locally and if no oral medicine department is available locally then to a district general hospital providing oral surgery and oral and maxillofacial services.
ii. Dentists accredited to perform oral medicine level 2 complexity care
Currently dentists are not commissioned to undertake this level of oral medicine care and so won’t have the opportunity to have been accredited by a local accreditation panel as defined in the current guidance from the Office of the Chief Dental Officer on level 2 practitioners.
iii. Specialists in oral medicine
The award of the certificate of completion of specialty training (CCST) is the responsibility of the General Dental Council (GDC). Registered specialists can provide a full range of treatments within the competencies defined by the oral medicine specialist training curriculum. Some provide this treatment directly themselves, but others also provide the treatment as part of a wider team including supporting clinical psychologists and pharmacists.
iv. Consultants
Consultants are specialists who in addition to their clinical role also take on managerial and supervisory commitments including training of colleagues and other specialties.
Management of oral mucosal diseases may in certain situations, require a multidisciplinary team approach and this is often more appropriately offered by an individual at consultant level in a secondary care environment alongside colleagues from other medical specialties eg: rheumatology
Completion of training to consultant level and admission to the oral medicine specialist list is marked by passing the Intercollegiate Specialty Fellowship Examination (ISFE) after a 5 year training programme reduced in time if the trainee has undergone undergraduate medical training.
v. Additional oral medicine workforce
- Dental nurses with enhanced skills such as phlebotomy and smoking cessation advice
- Dietician – to work on gastroenterology and oral medicine MDT clinics
- Pharmacist for immunobullous drug monitoring
- CNS – to support MDT clinics
- Psychologist – facial pain and chronic diseases MDT
1.3 Description of the complexity levels
All procedures are to be planned as part of a comprehensive treatment plan and consideration should be given to a multi-disciplinary approach where appropriate. The level of complexity of oral medicine care to be provided may change depending several patient related factors such as a patient’s medical and social history.
1.3.1. General principles
- Oral medicine treatment should only be undertaken in situations where it is believed to be in the patient’s best interests in terms of their oral health and/ or psychosocial
- In all situations, the clinical advantages and long-term benefits of oral medicine treatment should justify such treatment and outweigh any detrimental
1.3.2 General patient factors
The clinician should ensure that the co-operation, motivation, aspirations, and general health of the patient are consistent with the provision of any oral medicine condition management. Like orthodontics and other dental specialties their ability to maintain good oral hygiene is important to the outcome of any oral medicine care. The oral medicine team managing any patient should also ensure that the patient/carers are willing and able to commit to frequent attendance for monitoring and / or modification of treatment.
1.3.3 Clinically feasible and beneficial
Finally, the detailed clinical aspects of the proposed oral medicine treatment should be considered to ensure that it will be beneficial to the patient.
1.3.4 Complexity descriptors
The competency descriptors for the oral medicine workforce is described in Appendix 1
Level 1:
Treatment and care undertaken in NHS primary dental care mandatory contracts and NHS England commissioning expectations of care provided.
Level 2:
Treatment undertaken by practitioners with a formal link to a consultant-led MCN. This includes dentists and oral and maxillofacial specialists who have enhanced skills and/ or experience of medical management of oral mucosal lesions and conditions. Management of lesions and conditions at this level with normally be restricted to topical treatment only and would not be sufficiently complex to warrant multidisciplinary input.
Level 3a:
Treatment undertaken by practitioners who are on the specialist list for oral medicine with a formal link to a managed clinical network. This is predominantly delivered in a secondary care setting but could also be provided by a specialist visiting an oral and maxillofacial department in a district general hospital but also by visiting a community or primary care teaching and access hub where they exist.
Level 3b:
Treatment undertaken by practitioners who are on the specialist list for oral medicine and have undergone an approved period of training or who can demonstrate equivalence. Level 3b oral medicine is predominantly delivered in a dental hospital secondary care setting, but could also be provided by a specialist visiting an oral and maxillofacial department in a district general hospital but also by visiting a community or primary care teaching and access hub where they exist.
Draft framework of oral medicine complexity levels and procedures
Level 1 procedures/conditions
Recognition of conditions within the scope of oral medicine clinical practice, which include the predominantly non-surgical recognition and provision of immediate care of:
- Oral mucosal changes presenting as red, white, red/white, ulcerated, vesicular/bullous, pigmented lesions or soft tissue swelling, which may be asymptomatic or an incidental finding
- Changes in saliva and salivary gland presenting as oral dryness, excess saliva or salivary gland swelling
- Orofacial pain/dysaesthesia/paraesthesia/numbness not due to typical dental disease (caries and periodontal disease), altered oral sensations and other neurological abnormalities
Recognition of situations where the presenting complaint indicates referral, appropriate timing of this and choice of service:
- Priority: Suspicion of cancer (2-week pathway) or other conditions which may be life threatening if undiagnosed, such as vesiculobullous disease, immunosuppression , trigeminal neuralgia, allergic or immunologic conditions and other underlying complex systemic disease
- Co-morbid illness that may influence management of the presenting complaint
Initiation of care (e.g. identify and address concerns, information, oral hygiene, 1st line topical treatments) with appropriate follow-up and/or referral.
Level 2 procedures/conditions
Level 2 care should be provided for patients with complaints who fall within the scope of practice and require:
- Re-evaluation of diagnosis and the care pathway
- Standardised assessment with respect to the need for Level 3 input with referral as appropriate
- Initiation and evaluation of management not systemic therapy or requiring level 3 or multidisciplinary input
- Management as directed by Level 3
Level 3 procedure/conditions
Level 3 care should be provided for patients with complaints that fall within the scope of practice where:
- The diagnosis is unclear
- Interventions have not achieved a satisfactory outcome
- The presenting complaint may represent an orofacial manifestation of a systemic or multi-site illness. Patients may present with mental health issues that may complicate the diagnosis and management of the orofacial problem. However this must be recognised and these mental health problems must be managed by the appropriate mental health team or GP
- Management is complicated by significant co-morbid illness (physical or mental health) or the management of this
- Management requires potent topical or systemic interventions (such as immune-modulating drugs and drugs used for pain-control or altered sensations)
- Multi-disciplinary or multi-professional management is indicated.
- Level 3b is a condition that requires systemic management1 Illustrative journey
2. Illustrative journey
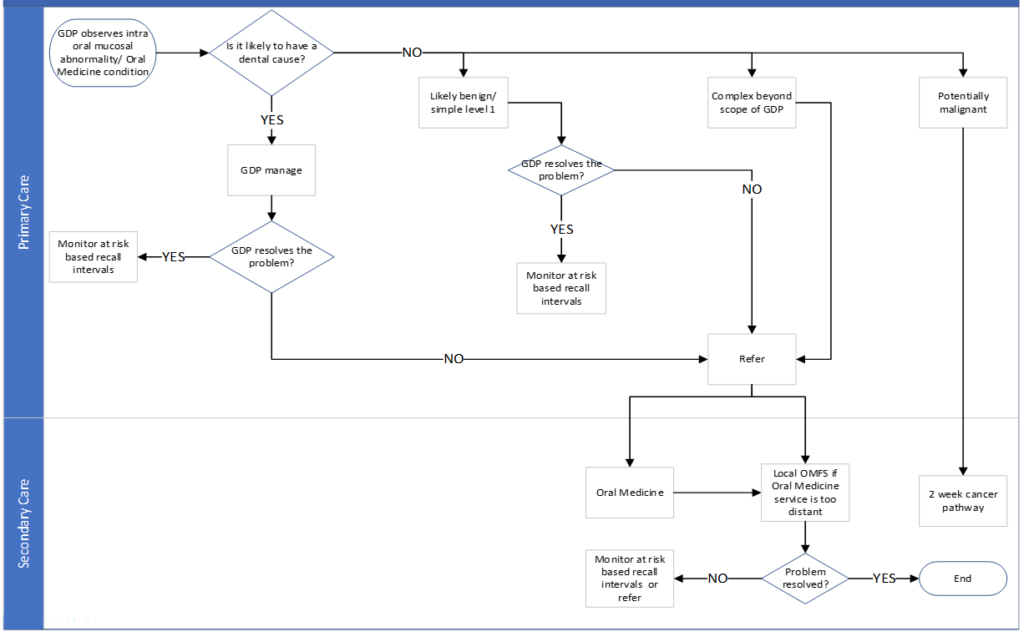
Oral medicine pathway
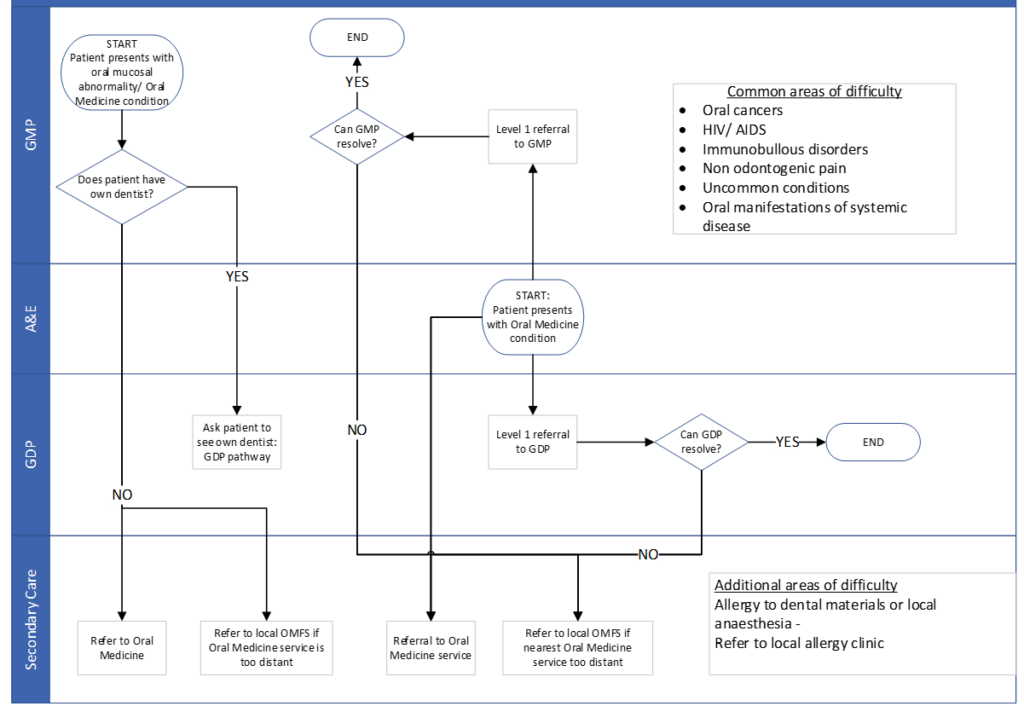
Oral medicine pathway – from GMP or A&E
3. Assessment needs
For the majority of oral medicine conditions, no specific needs assessments or guidelines exist. Therefore, commissioners and consultants in dental public need to rely on proxy measure and service activity data.
In principle there are three mainelements to assessing oral medicine treatment need:
- Normative need – the professionally-judged need in a population cohort
- Expressed need – patients with need presenting for treatment
- Demand (felt need) – a patient’s perception of need. This is generally a poor proxy for need and often reflects supply and other social factors. At present there has been a demand in 2 WWW referrals from both GDPs and GPs as a result of the Covid-19 pandemic in 2020. It remains to be seen if this demand will continue in the future
Undertaking population oral medicine needs assessment and reviewing existing service provision as a minimum, should include:
- the oral mucosal lesions and condition needs of the local population
- and if population projections will alter this needs assessment over the coming years
- audit of current providers and their service and contract delivery performance
- assessment of whether local oral medicine services are sufficient to serve the population and are currently in the right locations
4. Understanding current provision
4.1 Current provision
Currently, oral medicine services are largely provided by specialist practitioners operating within a dental hospital environment, and by oral and maxillofacial surgeons in district general hospitals.
Under current arrangements, it is largely the referring GDP and some GPs who determine if, where and when a patient is referred.
4.2 Quality and effectiveness
This standard has been produced to promote consistent delivery and quality of specialist oral medicine care provision to patients in England to ensure that resources invested by the NHS in specialist care is used in the most effective way, provide the best possible quality and quantity of care for patients, and meet need rather than serve demand.
This will be achieved though effective partnership working between commissioners, oral medicine specialists, oral and Maxillofacial specialist and dentists working in primary care. This will be most effectively delivered through the structures of a fully functioning specialist led oral medicine managed clinical network, with links to other MCNs such as oral.
For oral medicine service provision this may not mean directing much of the available resource for high quality patient care to primary care settings, as it can be for orthodontics, because the infrastructure of primary care workforce having the knowledge and expertise to manage conditions considered as level 2 complexity cases does not exist yet. However most district general hospital oral and maxillofacial surgery departments have this knowledge and expertise and so could be commissioned in a hub and spoke manner ensuring that only those patients with greatest complexity are referred for care within a specialist oral medicine secondary care setting.
As responsible clinical stewards, oral medicine specialists can assist in leading this change and provide a more effective use of constrained resources by broadening their influence within a MCN with other specialist providers and primary care clinicians and to ensure that referrals are timely and valid, and that oral medicine care is delivered effectively and efficiently.
4.3 Outcomes
Oral medicine is one specialty where a clinical outcome measure have not yet been developed.
5. Current models
The following bullet points summarize the current models of care operating for the provision of oral medicine services and have been discussed previously in the guide.
- GDPs decide where and when to refer a patient
- Service provided in secondary care settings
- Variable local referral pathways used with no nationally agreed care pathway
- A variety of factors influence where patients are referred including:
- General access to primary dental care
- Historic referral patterns/ local care pathways
- Patient satisfaction/preference
- Geography (transport links) and availability of oral medicine services
- Teaching needs, for example postgraduate and undergraduate programmes
- Contracts and available resources (primary and secondary care)
- Experience and knowledge of GDPs
- MCNs/ LCNs are in existence but specific management/ effectiveness of these differs from region to region
- Limited patient experience measures are collected and reported in primary care
5.1 Workforce implications
- Multidisciplinary care managed through local MCNs
- Consultant-led with administrative support required
- Liaison with other medical specialties – namely rheumatology, dermatology, ophthalmology, gastroenterology, psychology, neurology and pain specialists
- Liaison with oral and maxillofacial surgery and oral surgery MCNs
- Liaison with restorative dentistry MCNs
- Liaison with special care dentistry MCNs
- Liaison with paediatric dentistry MCNs
- Appropriate workforce available to deliver care
- Effective communication with commissioners and local dental network (LDN) through oral medicine MCNs to ensure high quality patient care
- Development of training models to improve quality and cost effectiveness to deliver additional benefit to patients
Framework for maintenance of core skills and enhance
6. Illustrative care pathway and related standards
This illustrative patient journey should be considered locally:
Identifying care pathway for patients – oral medicine
Level 1/ level 2/ level 3 complexity
Level 1 GDP
| Illustrative patient journey | Standards | Metrics | Enablers |
|---|---|---|---|
| Recognise Evaluate the potential need for oral medicine treatment. | Timely valid referrals | Data submissions aligned with that expected of GDS contract Referral quality and validity: Referrals should adhere to the standards for transfer of patient data including images and radiographs such as via secure NHS mail | Consultant led local Oral Medicine MCN communicating with GDS/PDS primary care contractors under the umbrella of a local professional network. If too many referrals are being sent without an oral examination first then the referral pathway locally can be modified locally by agreement through the local Oral medicine MCN |
| Ensure patient is: Aware of the importance of maintaining good oral hygiene throughout oral medicine treatment. Primary care dentists should explain to patients what oral medicine treatment may involve. Be able to make valid and timely referrals adhering to NHS England Oral Medicine referral guidelines (to be developed ) Monitoring post oral medicine department discharge |
Referral
| Illustrative patient journey | Standards | Metrics | Enablers |
|---|---|---|---|
| · Referrer completes the referral form ensuring consistent required data set is complete (to be developed) · The referral must include all relevant medical history · The referral must include any available relevant photographs and radiographs which must be sent over a secure email system. In compliance with IG requirements · Preferred providers for the appropriate level of specialist care required. · Dentist referring within one week of the decision to refer being made | · Only refer patients who want oral medicine care · Referrals adhere to oral medicine referral guidance, including timely referral requirements · Consistent and accurate data set of referrer details · Consistent and accurate data set of patient demographics and contact details · Specific relevant medical history communicated to oral medicine provider · Patient has good oral hygiene or other special needs/modifying factor is noted Images Radiographs should adhere to the NHS DICOM standard – Current Edition (dicomstandard.org) Photographs should adhere to the NHS Information standards | · % of referrals received that have complete referrer details · % of referrals received that have complete patient demographic and contact details · % of patients who are informed and understand what oral medicine treatment may entail · % of patients who meet NHS criteria, want and are suitable for oral medicine care or advice · % of patients who are referred within 1 week of decision to refer. · % of referrals with relevant images (photographs) | Electronic pro-forma and referral processes Agreed data set and national orthodontic referral guidance Waiting lists, outcome and performance indicators of all specialist providers available to referrers |
Specialist care level 2/3
| Illustrative patient journey | Standards | Metrics | Enablers |
|---|---|---|---|
| · Patient has all information about · Ensure valid consent · Information on · Patients are fully informed about the risks and benefits of. Referral process includes assessment for advice regarding on- going management. | · Competence and qualification · Formal appraisal, peer review and outcome measures in place for all clinicians through a managed clinical network · Access to appropriate premises and equipment such as radiographic facilities dental panoramic tomography, cone beam computerised tomography radiograph and any drugs and equipment made available as recommended by British National Formulary and Recuses Council UK · Disability Discrimination Act, Equality Act and CQC compliant · Patient has choice of appointment time subject to availability of provider, but all providers should be able to offer appointments multiple sessions over a working week All providers are working within an MCN and not working in isolation. | · % of referral forms that are deemed valid · % of referrals forms received that confirm patient need, want and are suitable for oral medicine care or advice · % of DNAs/ cancellations by patient · Provider CQC compliance | Appropriate contracting mechanisms |
Level 2 and 3 care
| Illustrative patient journey | Standards | Metrics | Enablers |
|---|---|---|---|
| Ensure good communication with patient’s GDP throughout treatment. Referral to MDT e.g. Restorative, Oral Surgery, Maxillo-facial Surgery, Paediatric Dentistry, Plastic Surgery if necessary Monitor patient’s compliance of oral hygiene throughout treatment and inform patient/ carer and GDP if support is necessary. Undertake Oral medicine treatment to a high standard and in a time efficient manner. Patient has all necessary information on advised self-care and who to contact during treatment should there be a problem. | · Start treatment within 18 weeks of initial assessment if patient meets necessary referral criteria (excluding those patients referred in via a 2WW pathway whose standards are different) · Timely management of problems during treatment · Consistent and accurate record keeping · Patients able to contact the Oral Medicine providers during surgery hours throughout the course of treatment and maintenance period · Inter-visit length i.e. length between appointments should be appropriate to meet optimal clinical standards · Ensure valid consent for treatment is obtained throughout the course of treatment Appropriate supervision of non-specialist providers | · % of patients who are ready for treatment and commence within 18 weeks or decision to treat · % of incomplete or abandoned treatments · Robust external audit of outcome measures reported and reviewed through the managed clinical network | Effective use of resources e.g. skill mix Consistent diagnostic and procedure used by all Level 2 and 3 care providers The workforce with the relevant training to deliver care Access to appropriate MDT involving Medical specialties such as Rheumatology; Dermatology, Gastroenterology, Pain specialists and Psychologists where required. Clear distinction between levels of care |
Discharge maintenance
| Illustrative patient journey | Standards | Metrics | Enablers |
|---|---|---|---|
| · Patient has all necessary information at end of active management and who to contact should there be a problem · What to expect in the monitoring period · At discharge from the Oral medicine provider, patient is given all the necessary information regarding on-going management of retention and what they can expect from their GDP. | · Patient-friendly information available in a number of formats including information on what to expect and who to contact and what to do if problems occur · GDP and GP informed of patient’s discharge within 1 month GDP , GP and patient given discharge and retention plan | · PROMs collected and reported on routinely within one month of completion of care Through provider home check reporting and surveys · Did you get what you needed? · Did you have any problems over course of treatment? · Did you need to seek advice or assistance outside of scheduled appointments? · If the problem you were referred with caused you to be unable to eat comfortably or socialise with confidence – is that now resolved? Would you recommend this provider to a friend? | Provider has all details of referring dentist and GP (where registered) correct from initial referral data Discharge information to referrer Responsive administrative support |
7. Clinical standard
Minimum clinical standard requirements
All level 2 and level 3 care must meet the minimum clinical standards for all level 1 care together with the additional elements as described below.
Primary care and level 2 care
Staff Composition/ Workforce
The staff composition will be as follows:
- Suitably trained and experienced dental healthcare professionals for example dental nurses/ hygienists
- A qualified dental nurse who will support the dentist at all times
The provider will ensure:
- That all staff supplied have valid registrations and evidence of continuing professional development for on-going registration including participation in peer review and audit
- That the performers have the skills to manage vulnerable patients who may have addiction, mental health illnesses and anxiety/ days/ hours of operations
- The service must be provided at times most convenient to patients, including early mornings and late afternoon appointments to ensure school children are not discriminated against. Consideration should be given to evening or weekend appointments
Patient focus
Providers will ensure that patients are provided with relevant verbal and written. information in a variety of formats, where necessary using an interpreting service, outlining the service.
They will also be required to provide information concerning the outcome of the assessment, such that the patient is clear why a specific treatment opinion has been selected.
Prior to initiation of treatment, the patient and/ or carer should be provided with the following information verbally and in writing:
- Treatment plan including length of treatment and frequency of visits
- What to expect during treatment?
- What is expected of them including self-care, compliance and under what circumstances treatment will be terminated e.g., poor attendance, poor oral hygiene, abusive behaviour
- Any additional costs the patients may experience e.g., payment for medicines
The information should be given in such a way that it supports the patient’s ability to give formal consent to initiate treatment.
Providers will be required to:
- Ensure the patient has a clear understanding in advance of what will happen to them during the treatment, who will be responsible for delivering each element of care and why
- Ensure valid consent is gained from all patients prior to initiating assessment and/ or treatment
- Have effective and robust arrangements in place to promote and safeguard the health and wellbeing of young people and vulnerable adults
- Have in place a policy that meets the Commissioners’ and CQC requirements for Safeguarding Child/ Young Person and adults
Equipment/facilities
- Ensure that all equipment conforms with health and safety regulations and nationally accepted standards and is maintained regularly in line with national and manufacturers guidelines
- Be responsible for the funding of consumables and biopsy equipment access to phlebotomy and pathology services, transport to and from the laboratory and provision of dental appliances if required
- Ensure any dental laboratory services used meet with GDC guidance and current legislation
- Ensure that safe processes and working environment are in place. This will include training of staff in relevant processes and procedures
- Ensure all legal requirements relating to radiological guidance are
Appropriate premises and equipment such as radiographic facilities e.g., Dental Panoramic Tomography, Lateral Cephalometric radiograph and any drugs and equipment made available as recommended by Research Council UK Other
All providers will be required to become active
Level 3 care
As level 2 care, but to include:
Suitably experienced and qualified specialist in oral medicine with the following qualifications: IFSE (level 3b) or equivalent and must be on the GDC oral medicine specialist list.
8. Quality and outcome measures
The illustrative patient journey suggests metrics that can be applied across the Oral Medicine Care Pathway. It is expected that Commissioners and local MCNs will select and develop reporting mechanisms for locally relevant metrics along with the required PROMs and PREMs measures, as detailed below.
8.1 Patient reported outcome measures (PROMs) and patient reported experience measures (PREMs)
The use of appropriate PROMs and PREMs will be essential to benchmark services. The measures should be patient-focused and consider potential inequalities throughout the patient journey. Appropriate tools should consider the different ways in which service users can provide feedback and different service users’ communication needs.
PROMs/ PREMs should include data which can be collected by services at a local level, as well as data which can be collected centrally using national surveys and, where possible these data should be triangulated. There should be evidence to demonstrate that PROMs/ PREMs are representative of the patient groups treated and not just those who can easily provide feedback.
Generic PROMs & PREMs have been developed for all specialist services and these can be referenced in the overarching Guide for specialist dentistry services.
a. Clinical outcome measures
MCNs in oral medicine should audit and review clinical outcomes to support improved quality.
b. Dental assurance framework
NHS England’s dental assurance framework provides a set of indicators that provide high level assurance for the MCN and commissioners, whilst recognising that no one set of indicators could, in itself, provide absolute assurance of quality, nor could it necessarily identify best practice. It is designed to give assurance that providers are on course to meet their obligations under their contract/ agreement.
Appendix 1 – competency framework
Competency framework for oral medicine practitioners
N.B. The professional qualifications and training requirements listed in this table apply to individuals who are currently undertaking training or who wish to undertake training in the future. Existing practitioners and providers may not necessarily have followed the recently established training pathways and may not hold any or all of these qualifications but have demonstrated clinical excellence in oral medicine for many years. These practitioners should not currently be excluded from consideration of provision within the commissioning process.
| Assurance criteria | Primary care dentist (non-specialist) | Dentist with enhanced skills and competence | Specialist in oral medicine | Consultant in oral medicine |
|---|---|---|---|---|
| Experience | Registered as a dentist with the GDC. | GDC-registered primary care dentist with enhanced skills and competence in Oral Medicine | Must be on GDC oral medicine specialist list. | Must be on GDC oral medicine specialist list. |
| Qualifications | No additional qualifications necessary. | Additional experience, enhanced skills and competence assured by MCN | Must be on GDC oral medicine specialist list. | Must be on GDC oral medicine specialist list. |
| Training in oral medicine | No specific training in oral medicine. | No specific training in oral medicine. Evidence of experience, enhanced skills and competence | Must be on GDC oral medicine specialist list. | Must be on GDC oral medicine specialist list. |
| Teaching and education | Undergraduate teaching in oral medicine. May have attended relevant postgraduate oral medicine courses. | Evidence of attendance at relevant postgraduate oral medicine courses. Evidence of experience, enhanced skills and competence. | Supervision of higher training in oral medicine and provision of mentorship for dentists with enhanced skills and competence who provide primary care oral medicine services. Involvement in undergraduate &/or postgraduate training | Leading higher training in oral medicine and provision of mentorship for dentists with enhanced skills and competence who provide primary care oral medicine services. Involvement in undergraduate &/or postgraduate training. |
| Referral base | Providers must provide level 1 care. | Providers will accept referrals as defined by the terms of the oral medicine care pathway. It is not expected that level 1 care will be provided. Management of lesions and conditions at this level will primarily be restricted to topic treatment and would not need a multidisciplinary approach. | Providers will accept level 2 referrals as defined by the terms of the oral medicine care pathway. | Providers will accept level 3 referrals as defined by the terms of the oral medicine care pathway. |

