Recommendations
Recommendations for community pharmacy
- Ensure community pharmacy teams act as antimicrobial stewards and promote antimicrobial stewardship and infection prevention and control
- Ensure all patient-facing community pharmacy staff that provide advice on medicines or healthcare in the pharmacy are aware of the principles and can practice effective antimicrobial stewardship (AMS) and infection prevention and control (IPC).
- Pharmacy teams should promote AMS by pledging to be Antibiotic Guardians and should have an awareness of their current local antibiotic formulary and know how to access it.
- Encourage patients to complete the TARGET antibiotic checklist
- The TARGET antibiotic checklist was designed for patients to complete whilst waiting for their prescription to be dispensed enabling the pharmacy team to initiate AMS conversations and actions. The TARGET antibiotic checklist is available digitally and translated in multiple languages. In addition, the managing common infection (self-care) leaflets are also available digitally and translated in multiple languages. These resources can be used for patients accessing services remotely. Pharmacy staff are asking patients the questions in the patient section which may inhibit embedding the use of the antibiotic checklist into day-to-day practice. We recommend asking patients to complete it themselves to promote efficiency and aid uptake of use.
- Utilise TARGET toolkit resources to support awareness and education
- There are a range of TARGET resources that have been developed and are now available for use in community pharmacy. The TARGET antibiotics hub contains a toolkit that aims to helps influence healthcare professionals and patients’ personal attitudes, social norms and perceived barriers to optimal antibiotic prescribing. It includes resources that can each be used to support prescribers’ and patients’ responsible antibiotic use.
- The resources for use in community pharmacy include:
- How to use pharmacy resources (containing a community pharmacy flowchart)
- TARGET Antibiotic Checklist
- Community pharmacy counselling checklist
- UTI Women Under 65 Leaflet for community pharmacies
- RTI leaflet for community pharmacies
- Other TARGET leaflets that can be used in community pharmacy
- Pharmacy teams should continue to educate patients on AMR and the use of antibiotics using the TARGET resources and distribute the patient information leaflets to promote patient recall of advice given.
- The leaflets should be used to support patients with antibiotic prescriptions, patients referred via the Community Pharmacist Consultation Service (CPCS) and walk-in patients for minor illnesses and become part of day-to-day practice.
- Promote influenza vaccinations
- Pharmacy teams should continue to promote vaccinations to protect patients whilst simultaneously contributing to reducing the prevalence of AMR. Community pharmacy teams can use completed Antibiotic Checklists to identify patients for influenza and COVID-19 vaccination.
Recommendations for NHS bodies
- Community pharmacy integration with multidisciplinary teams
- Integrated care boards (ICBs) should ensure community pharmacy are effectively integrated with multi-disciplinary teams to promote optimum care and antimicrobial stewardship.
About this report
This report is intended for:
- Community pharmacists, primary care pharmacists and all healthcare staff responsible for prescribing, dispensing or reviewing antibiotic use.
- NHS leaders responsible for patient safety, medicines optimisation and primary care contracts.
- Pharmaceutical Services Negotiating Committee (PSNC) and other national pharmacy bodies.
Purpose
This report has two aims:
- To report key findings of the Pharmacy Quality Scheme’s (PQS) AMS requirements from 2020/21 to 2021/22 and specifically to review and evaluate the findings from the implementation of TARGET Antibiotic Checklists as a tool to support AMS in community pharmacy.
- To make recommendations to support improving AMS through community pharmacy for implementation in the 2023/24 PQS.
Background
AMR is a global problem, impacting people worldwide. The UK’s 2019-2024 national action plan for AMR has three overarching aims:
- reducing the need for, and the unintentional exposure to antimicrobials
- optimising the use of antimicrobials
- investing in innovation, supply and access.
In the UK, rising AMR will cause people to suffer longer infectious illnesses as they become more difficult to treat, and the number of human deaths and suffering attributable to infectious disease will increase as will the socio-economic costs associated with treating ill health.
In 2020, 80% of antibiotic prescribing occurred in primary care in England (72% in general practice; 4% dental; 4% other community settings) demonstrating that primary care is still responsible for the majority of antibiotics prescribed to people and therefore a key setting for AMS.
The UK AMR National Action Plan recognises that one of the most successful initiatives to embed AMS into practice has been the use of TARGET Antibiotic Toolkit. The toolkit provides a range of resources to support health professionals whilst educating patients on the appropriate use of antibiotics. Effective use of the TARGET Antibiotic Toolkit supports appropriate antibiotic use as well as reducing the opportunity for resistance to develop.
This work builds a critical foundation for community pharmacy on which to build the future role of community pharmacy described in our delivery plan for improving access to primary care where pharmacists will be able to supply prescription medicines, including antibiotics and antivirals where clinically appropriate.
Summary
Antimicrobial Stewardship (AMS) requires effective teamwork between healthcare professionals, with patients receiving consistent messages from all healthcare professionals on the appropriate antimicrobial use. Patient education may reduce patients’ expectations to receive antibiotics for self-limiting conditions and reduce the pressure on primary care clinicians to prescribe antibiotics. Since 2020, the Pharmacy Quality Scheme (PQS) has incentivised AMS activities in community pharmacies. Each year, the PQS aims to build upon previous initiatives to maximise the learning and development in bite-size chunks as well as embed initiatives into day-to-day practice.
The PQS is an opt-in incentive scheme which forms part of the Community Pharmacy Contractual Framework. The scheme has incentivised activity related to AMS in community pharmacy since 2020, including the use of the TARGET Antibiotic Checklist. This report summaries the results from the PQS, AMS initiatives up until and including PQS 2021/22.
In 2020/2021, 10,488 (>90%) pharmacies declared that 54,399 registered pharmacy professionals (nearly all registered professionals working in those pharmacies) had completed the AMS e-learning and Infection Management e-learning. The introduction of the Antibiotic Guardian pledge as part of the PQS in 2020/21 led to a vast increase in UK pledges from pharmacy teams in 2020 (28,369 pledges) which was sustained in 2021 (27,334 pledges).
In 2021/22, 9,950 (89%) community pharmacy teams throughout England engaged in AMS activity using the TARGET Antibiotic Checklist. They provided indication-specific education to patients and positively impacted the uptake of influenza vaccinations. During the four-week data collection period, 8,374 pharmacies collectively submitted data from 213,105 TARGET Antibiotic Checklists. In total, 69,861 patient information leaflets were provided to patients to support knowledge about their condition and treatment. 62,544 (30%) checklists were completed for patients with a respiratory tract infection (RTI); 43,093 (21%) for a urinary tract infection (UTI); and 30,764 (15%) for tooth/dental infections. Prompted by discussions whilst using the Antibiotic Checklist, an additional 16,625 (8% of all Antibiotic Checklists) influenza vaccinations were delivered by community pharmacies.
44% of pharmacies submitting data surpassed the required number (25 checklists) to qualify for the PQS incentive. Pharmacy teams reported checking: duration, dose, appropriateness of antibiotic and patient allergies and medicine interactions (94 – 95%); antibiotic prescribing guideline adherence (89%); and checking the patient’s previous use of antibiotics (81%). The prescriber was contacted for 2,741 (1.3%) of the Antibiotic Checklists, the most common reasons were around dose and duration, and possible patient allergy.
Full details of the results have been published in the following papers:
- The Use of the TARGET Antibiotic Checklist to support Antimicrobial Stewardship, in England’s community pharmacies through the Pharmacy Quality Scheme.
- National implementation of a Community Pharmacy Antimicrobial Stewardship Intervention (PAMSI) through the English Pharmacy Quality Scheme 2020 to 2022.
Community pharmacy teams recognised the need to implement AMS activities in their day-to-day practice. They are in a unique position to provide triage for common primary care conditions and educate the public about AMR. Effective communication, collaboration and teamwork between pharmacy teams and other healthcare professionals is imperative for successful AMS.
Results of the Antimicrobial Stewardship initiatives
Since 2020, the PQS has incentivised AMS activities in community pharmacy. These activities include completion of the Antimicrobial Stewardship for Community Pharmacy by all patient-facing pharmacy staff that provide advice on medicines or healthcare; Infection Prevention and Control – Level 1 (for non-registered pharmacy staff); Infection Prevention and Control – Level 2 (for registered pharmacy professionals); developing an action plan detailing how to promote AMS in their pharmacy; and a commitment that all patient facing staff that provide advice on medicines or healthcare become Antibiotic Guardians and have an awareness of the local antibiotic formulary.
In the PQS 2021/22, the prevention domain also required community pharmacy teams to use the TARGET Antibiotic Checklist for patients presenting with an antibiotic prescription. The TARGET Antibiotic Checklist is designed to be completed by appropriately trained pharmacy staff with patients, and asks patients to report their infection, risk factors, allergies, and knowledge of antibiotics which is used by the pharmacy team to ensure that the antibiotics and advice that patients receive are safe and tailored to suit the individual’s needs. Results of the PQS 2020/21 implementation of Antimicrobial Stewardship; Infection Prevention and Control e-learning and Antibiotic Guardian pledge are below.
Antimicrobial stewardship for Community Pharmacy e-learning
The AMS e-learning was launched on the e-learning for healthcare website at the start of 2020 and was freely available for any healthcare staff to complete. In the 2020/2021 PQS, 10,488 pharmacies declared that 54,399 registered pharmacy professionals had completed the AMS and Infection Prevention and Control e-learning. Data from HEE found that there had been 145,950 total session launches of the e-Learning: Antimicrobial Stewardship for Community Pharmacy since January 2020 to March 2022. The highest number of sessions were in 2020 (80,717, 56%) and 2021 (54,936, 38%). The most frequently represented job roles that undertook the training were pharmacy dispensers (55,760, 38%), pharmacists (29,659, 20%) and pharmacy assistants (25,129, 17%).
Infection Prevention and Control e-learning
In addition, 217,001 total sessions were launched of both the Infection Prevention and Control e-learnings (Level 1 and Level 2 combined) since January 2020 to March 2022. The highest number of sessions were in 2020 (101,973, 47%) and 2021 (115,028, 53%). The most frequently represented job roles that undertook the infection management training were pharmacy dispensers (31,912, 53%), pharmacists (14,008, 23%) and pharmacy assistants (10,194, 17%); pharmacy technicians (6.315, 10%) and trainee pharmacists (2,694, 4.5%). These findings collectively coincide with the PQS incentivisation. These results are summarised in Table 3
Table 3: Results from the implementation of AMS and IPC e-learning in Community Pharmacy
|
|
January 2020 to March 2022 |
2020 |
2021 |
|
Antimicrobial stewardship for Community Pharmacy |
|
|
|
|
Total Number of sessions launched |
145,950 |
80,717 (55%) |
54,936 (38%) |
|
Pharmacy dispenser |
55,760 (38%) |
|
|
|
Pharmacist |
29,659 (20%) |
|
|
|
Pharmacy assistant |
25,179 (17%) |
|
|
|
Infection Prevention and Control Level 1 and 2 |
217,001 |
101,973 (47%) |
115 028 (53%) |
|
Pharmacy dispenser |
31,912 (53%) |
|
|
|
Pharmacist |
14,008 (23%) |
|
|
|
Pharmacy assistant |
10,194 (17%) |
|
|
|
Pharmacy Technician |
6,315 (10%) |
|
|
|
Trainee Pharmacist |
2,694 (4.5) |
|
|
Antibiotic guardians
Table 4 shows the number of antibiotic guardian pledges from individuals identified from pharmacy teams located in the UK from 2015 to 2021. Antibiotic guardians consisted of academic pharmacists, community pharmacists, pharmacy assistants, pharmacy technicians, primary care pharmacists, and secondary care pharmacists. Introduction of the antibiotic guardian pledge as part of the PQS in 2020/21 led to a vast increase in UK pledges from pharmacy teams in 2020 which was sustained in 2021.
Table 4: Number of antibiotic guardian pledges between 2015 and 2021 from the United Kingdom
|
2015 |
2016 |
2017 |
2018 |
2019 |
2020 |
2021 |
Total |
|
8,259 |
1,983 |
2,687 |
1,536 |
2,211 |
28,369 |
27,334 |
72,379 |
PQS 2021/22 prevention domain
9,950 community pharmacy teams throughout England engaged in AMS activity using the TARGET Antibiotic Checklist. Data was submitted by 8,374 community pharmacy teams, with 213,105 TARGET Antibiotic Checklists being completed with patients as they collected antibiotic prescriptions. There was variation in the number of Antibiotic Checklists submitted by the 8,374 participating pharmacies (range: 1 – 181) (Table 5). Of participating pharmacies, 87% met and/or exceeded the number of patients they were asked to complete the checklist for in the PQS criterion (25 TARGET Antibiotic Checklists per pharmacy over a four-week period; or up to eight weeks if the if the minimum number of patients were not achieved within four weeks). 44% exceeded the requirement and 14% submitted less than stated in the criterion.
Table 5: Summary of the numbers of TARGET Antibiotic Checklists submitted by participating pharmacies
|
Total number of Antibiotic Checklists submitted |
213,105 | ||
|
Number of pharmacies who submitted Antibiotic Checklists |
8,374 | ||
|
Range of Antibiotic Checklists submitted. |
1 – 181 | ||
|
Completion of criteria |
Number |
Percentage of submitting pharmacies (n = 8,374) |
Percentage of total pharmacies in England on the pharmaceutical list (n = 11,232) |
|
Pharmacies who completed 25 Antibiotic Checklists |
3,572 |
43% |
32% |
|
Pharmacies who completed more than 25 Antibiotic Checklists |
3,653 |
44% |
33% |
|
Pharmacies who completed less than 25 Antibiotic Checklists |
1,149 |
14% |
10% |
Of the 213,105 TARGET Antibiotic Checklists submitted, 83% (177,092) were completed in full, with all sections completed by pharmacy staff and/or patients. The remaining 17% (36,013) were either partially completed, 16% (35,672) with at least one section missing data or not completed at all and 0.2% (341) with no data for any of the sections. For those partially or not completed 81% (29,042) provided an explanation for why it was not possible to collect data in full. The main reasons were due to lack of access to patient information, i.e., a patient representative was collecting on behalf of the patient and therefore did not know the indication and subsequent information (34% of 29,042, 10,019 Checklists), or the patient declined to complete all or some sections of the Checklist (25% of 29,042, 7,263 Checklists).
Pharmacy team antibiotic checks
The TARGET Antibiotic Checklist prompted the community pharmacy team to conduct and record a series of safety and appropriateness checks against each prescribed antibiotic; completed for 99.5%of prescriptions (212,124). Figure 1 highlights the high frequency of checks reported by the pharmacy team, particularly the dose, duration, appropriateness of the antibiotic and for patient allergies and interactions (94 – 95% of prescriptions).
Figure 1: Proportion of antibiotic safety checks completed by the pharmacist or pharmacy team, prompted by the Antibiotic Checklist for 99.5% of prescriptions
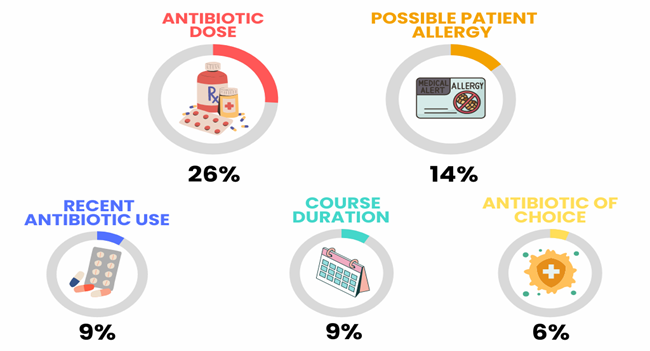
Pharmacy teams contacted the prescribing clinician to discuss 1.3% (2,741) of prescriptions. Of these, 62% (1,703) provided a reason for why they contacted the prescriber, see Figure 2 for the most reported reasons. The reasons for contacting the prescriber related to the appropriateness of the prescription against recommendations, including the dose (26%), duration (9%), and quantity (6%). Other reasons related to information the patient had provided via the TARGET Antibiotic Checklist, including potential allergy to an antibiotic (14%), recent antibiotic use (9%), choice of antibiotic for the indication and patient (6%), risk factors reported by the patient (4%) and medicine interaction (4%).
Of those who contacted a prescriber, 33% (900) provided information on the outcome of the discussion. This included that:
- the prescription dose, formulation, directions, strength, or duration was changed for 34% of prescriptions (312 of cases where a clinical discussion took place).
- the prescriber confirmed the prescription was appropriate and did not need to change for 25% of prescriptions (234 of cases where a clinical discussion took place).
- an alternative antibiotic was prescribed for 21% of prescriptions (197).
Other less reported reasons included:
- patient information being confirmed (87 prescriptions, 9%)
- patient referred to prescriber/patient requiring a further re-consult (40 prescriptions, 4%)
- prescription was cancelled (30 prescriptions, 3%).
Figure 2: Content analysis themes of why pharmacists contacted a prescriber.
Image text:
- Antibiotic dose 26%
- Possible patient allergy 14%
- Recent antibiotic use 9%
- Course duration 9%
- Antibiotic choice 6%
Findings from the use of the Antibiotic Checklist
78% (163,446) of the submitted TARGET Antibiotic Checklists were completed for patients who were collecting their own antibiotics and the remainder on behalf of patients for whom a representative was collecting their antibiotics. From the submitted Checklists, 51% (107,360) of patients reported taking other medications alongside their antibiotics (see Table 6). 79% (165,383) of patients reported that they were not allergic to any antibiotics.
Table 6: Findings from the use of the Antibiotic Checklist
|
|
Were the antibiotics for the individual collecting? % |
Was the patient taking any other medicines? % |
Was the patient allergic to any antibiotics? % |
|
Yes |
163,446 (78) |
107,360 (51.4) |
25,574 (12) |
|
No |
42,123 (20) |
90,764 (43.4) |
165,383 (79) |
|
Don’t know/missing |
1,954 (1) |
8,307 (4.0) |
14,867 (7) |
|
No Response |
1,335 (1) |
2,427 (1.2) |
3,034 (2) |
|
Total |
208,858 (100) |
208,858 (100) |
208,858 (100) |
Patient infections and antibiotics dispensed
The most common indication for which an Antibiotic Checklist was completed was for a RTI representing 29% (62,664) of submissions followed by UTI with 20% (43,093) of submissions, and tooth infections with 14% (30,764) of submissions (see Figure 3).
Figure 3: The frequency of infection type reported by patients collecting antibiotic prescriptions.
Note: Some checklists had two conditions ticked.
The most frequently prescribed antibiotics were amoxicillin accounting for 35% (73,921) of submissions, followed by nitrofurantoin (30,459, 14%), flucloxacillin (24,093, 11%), doxycycline (19,420, 9.2%) and metronidazole (13,720, 6.5%) (see Figure 4). Where two antibiotics were prescribed the most common antibiotic combination was amoxicillin and metronidazole which accounted for 0.8% (1,754) of submissions.
Figure 4: The frequency of antibiotics prescribed to patients for whom the TARGET Antibiotic Checklist was completed.
Provision of information to patients
Pharmacy teams reported providing 69,861 patient information leaflets, to patients dispensed antibiotics, to aid patients’ knowledge about their condition and treatment (see Figure 5). Most leaflets corresponded to the indication given by patients.
Figure 5: Number and type of supporting information leaflets provided to patients by the Antibiotic Checklist reported indication.
The TARGET Antibiotic Checklist aims to facilitate targeted information sharing between the patient and pharmacist to address concerns and give appropriate counselling. Patients most frequently requested further information from the pharmacy team about side effects of their antibiotics (16.6%, 34,560), how to take their antibiotics with food (15.5%, 32,247) and how long their symptoms would last (15.5%, 32,247). Patients reported requiring less information about why they must take their antibiotics according to healthcare professional instruction (8,809, 4.2%), why they must never share or keep their antibiotics for later use (12,030, 5.8%) and knowing when to seek further help with their infection (14,656, 7.0%) (see Figure 6).
Figure 6: Patient self-reported knowledge of specific information relevant to infection and safe and effective antibiotic treatment.
In the patient section of the TARGET Antibiotic Checklist, patients reported in 17% (36,097) of cases that they had previously received the same antibiotic in the last three months. Pharmacy staff discussed antibiotic resistance with the patient (or their representatives) for 42% (87,975) of checklists (see Table 7).
Table 7: Response from both the patient and pharmacist of using the same antibiotic in the last 3 months (n=number of checklists)
|
Response |
patient-reported prescription of the same antibiotic(s) within previous 3 months (%) |
pharmacy staff conversation with patient about resistance due to prescription of the same antibiotic(s) within the previous 3 months (%) |
|
Yes |
36,097 (17) |
87,975 (42) |
|
No |
156,836 (75) |
35,168 (17) |
|
Not applicable |
0 |
67,210 (32) |
|
Don’t know/missing |
13,203 (6.3) |
9,320 (4.5) |
|
No response |
2,722 (1.3) |
7,490 (3.6) |
|
Total checklists |
208,858 |
207,163* |
* This was filtered to exclude Checklists where multiple answers were ticked, i.e., if yes and no were ticked.
Influenza vaccinations
Overall, 47% (97,463) of submitted Checklists confirmed that the patient had already received the influenza vaccination; of which 26% (53,592 of the total Checklists) were eligible for a free NHS influenza vaccination (see Table 8). Out of the eligible population (52,592) who were entitled to free NHS influenza vaccines, 76% (39,960) of the Antibiotic Checklists indicated that the patient had already received it; for the subgroup of patients aged over 65 years, 77% (36,712) of patients confirmed they had already received it. As a result of the interventions from the use of the Antibiotic Checklist, 16,625 additional influenza vaccinations were delivered by community pharmacy, with 30% (5,019) being for patients eligible for free NHS influenza vaccinations and 70% (11,606) for patients not eligible for a free NHS vaccination.
Table 8: The number of TARGET Antibiotic Checklists indicating patients were eligible to receive a free NHS influenza vaccination
|
Influenza Vaccination Eligibility Category |
No of patients (% of total) |
No of influenza vaccines already received. (% by eligibility criterion) |
Gave the patient an influenza vaccine on site. (% of those who had not yet received vaccine) |
|
Over 65 years |
47,622 (23) |
36,712 (77) |
4,431 (41) |
|
Problem with kidney function* |
2,968 (1.4) |
1,648 (56) |
265 (20) |
|
Problem with liver function* |
740 (0.62) |
388 (52) |
85 (24) |
|
Pregnant* |
2,262 (1.1) |
1,212 (54) |
238 (23) |
|
Total |
53,592 (26) |
39,960 (76) |
5,019 (36) |
*Under 65
Conclusion
The PQS has effectively promoted AMS activities in community pharmacy. There was high engagement with the AMS criteria first introduced in 2020/21 and built upon in 2021/22. These findings have demonstrated that the TARGET Antibiotic Checklist can support community pharmacy teams to play a crucial role in AMS, by tailoring patient education and addressing patients’ concerns about antibiotic use. The data shows how the use of the Antibiotic Checklist has allowed patients and pharmacists to discuss antibiotic specific queries such as side-effects, how to take their antibiotics and how long their symptoms would last (see Figure 2). In addition, community pharmacy teams have shown collaboration with their general practice colleagues and should continue to do this to optimise patient care. This may further reduce patient expectation to receive antibiotics for self-limiting infections and reduce pressure on prescribers in primary care to prescribe antibiotics.
Whilst engaging with patients in conversations about their antibiotic prescriptions, community pharmacy teams have provided additional indication-specific education materials to reinforce their counselling and increased influenza vaccinations uptake. The PQS for 2022/23 built further on the clinical role of pharmacy teams by embedding shared decision-making tools to support consultations for patients with respiratory and urinary tract infections. Results of this are currently being collated and will be reported. All AMS initiatives have been renewed for the 2023/24 PQS with the addition of advice on safe disposal of unused or expired antibiotics.
Our findings further highlight and recognise the essential clinical role that community pharmacy staff have in AMS activities and collaborative working with other primary care colleagues as well as ongoing and continued public education to ensure the safe and appropriate use of antibiotics. The clinical discussions with prescribers resulted in appropriate changes to prescriptions in line with AMS principles. These findings add to the evidence that community pharmacy can play a vital role in AMS and support the NHS in England to tackle the significant threat of AMR to public health.
These AMS initiatives and findings form a solid foundation of knowledge and experience for community pharmacy to build on as the Pharmacy First service is introduced. This service has been outlined in the delivery plan for improving access to primary care. Community pharmacists will be able supply prescription-only medicines including antibiotics for seven common conditions.
Publication reference: PRN00052