Purpose of this guidance
This publication aims to improve treatment and care for adults with chronic obstructive pulmonary disease (COPD). It provides commissioners with strategies and recommendations for frontline care, service transformation and population health approaches.
The guidance has been shaped by experts, including clinicians, commissioners, patients and people with lived experience, professional societies and the voluntary, community and social enterprise (VCSE) sector.
It aligns with the Model ICB Blueprint’s principles of data-driven, equitable, and value-based care. It also supports the 10 Year Health Plan’s ambition to move towards proactive prevention and care delivered closer to home, guided by population health intelligence.
Context for change
COPD costs the NHS around £2 billion a year and can be life-limiting for patients. It is the second leading cause of hospital admissions, and exacerbations account for 45% of total COPD spend.
Biologic therapies offer a new treatment for patients with frequent exacerbations, elevated eosinophil counts, and ongoing symptoms despite optimised care.
With dupilumab receiving a positive National Institute for Health and Care (NICE) recommendation and more biologic therapies expected, there is potential to reduce exacerbation-related harm and improve outcomes.
For more information about the impact of COPD and the evidence for biologic therapies, see Business case guidance chronic obstructive pulmonary disease biologics.
Population health and community focus
This guidance is informed by the NHS neighbourhood health model, which aims to tackle health inequalities and improve the overall health and wellbeing of the population and cites population health management (PHM) as a core component.
Appendix 1 provides a view of stratifying COPD patients in line with a population health management approach.
1. Understanding local population needs
Services should be based on a proactive, data-led approach to understanding and meeting local COPD population needs.
Actions
- Use system-level data to assess care quality, identify unwarranted variation, and inform strategic planning for local services, including modelling demand for biologic therapy. A range of tools and sources are listed below to support this work.
- Apply population health management principles to identify and prioritise high-risk COPD cohorts for treatment optimisation, particularly those in underserved communities. Validated search tools, such as those developed for the OPTIMISE model (Futures login required), can be used to support risk stratification, including identifying COPD patients with frequent exacerbations, repeated oral corticosteroid use or deteriorating symptom control.
Resources
- NHS Federated Data Platform PHM Tool
- National Respiratory Audit Programme
- Strategic Health Assessment Planning Evaluation (SHAPE)
- OPTIMISE model
- Health Innovation North West Coast – Fuel poverty toolkit
2. Planning service capacity
Strategic population-led approaches to planning COPD services will need to focus on clinical complexity rather than patient volume alone. This includes aligning service capacity, workforce modelling and care pathways to ensure timely, equitable and high-value care.
Actions
- Model workforce needs based on population size, clinical complexity, and intensity of care required. This includes ensuring sufficient COPD specialist capacity and supporting extended and enhanced roles across primary and community care settings.
- Review and optimise COPD pathways, using an integrated neighbourhood team approach. This may include multidisciplinary teams and should involve upskilling primary care, respiratory and pharmacy teams in line with care pathways. Teams should be equipped to implement shared decision-making and deliver culturally competent, personalised care and support.
- Use national evidence and audit insights (see resources below) to inform local capacity assessments, workforce development strategies and pathway design. These resources offer practical guidance for safe, efficient, and scalable delivery of COPD care, including biologics.
- For service design:
- involve patients and carers with lived experience of COPD and healthcare inequalities
- collaborate with local respiratory clinical networks to identify service gaps and implement whole-pathway improvements, such as standardised OPTIMISE protocols in primary care
- appoint a named COPD clinical lead to oversee biologics implementation and drive system-wide improvement
Resources
- British Thoracic Society respiratory workforce report
- Getting It Right First Time (GIRFT) respiratory report
- National Respiratory Audit Programme organisational audit 2024
- Primary Care Respiratory Society (PCRS) ‘Fit to Care’
- NHS England Co-production resource toolkit
3. Designing clinical pathways
COPD service design should align with the latest evidence, established clinical standards and best practice to enable the delivery of optimal, clinical care for patients with unstable disease and who are potentially eligible for biologics.
Actions
- Commission proactive COPD care that prioritises accurate diagnosis and early intervention to reduce avoidable exacerbations and unplanned admissions, which are associated with increased cardiovascular risk and reduced survival rate (see COPD Voices report). This includes ensuring access to quality-assured spirometry and clinical review, which underpins appropriate treatment decisions and biologic eligibility.
- Sustain and strengthen core COPD care in line with NICE guidance, including:
- vaccination
- tobacco dependence treatment
- pulmonary rehabilitation
Practical improvements can be informed by the PCRS consensus and Managing COPD guidance. Care pathways should be clearly defined for both stable disease management and responsive support during exacerbations (for example, 7 day support, same day emergency care assessment, early supported discharge).
Where appropriate, patients should also have access to advanced interventions, such as:
- lung volume reduction
- home oxygen therapy
- domiciliary ventilation support
- transplant assessment
- Build proactive risk stratification into service design. The OPTIMISE model offers a practical framework for improving outcomes for patients at increased risk of winter exacerbations. To improve outcomes and reduce pressure on acute services, care should also address wider needs through:
- social prescribing
- mental health support
- welfare advice
- Explore and implement innovative care models that enhance local provision and improve patient experience and outcomes (see Innovative care model case studies).
- Refer to the forthcoming British Thoracic Society (BTS) Clinical Statement on biologic therapies, with publication anticipated in summer 2026. This will outline clinical best practice in the treatment of COPD with biologic medicines.
Resources
- COPD Voices report
- Commissioning standards for spirometry
- Commissioning standards for pulmonary rehabilitation
- NICE guideline NG115
- PCRS consensus on the treatment of COPD
- Asthma and Lung UK: Managing COPD
- Impact and learning from the OPTIMISE approach
- Innovative care model case studies
- BTS Clinical Statement on biologic therapies and COPD
4. Monitoring and outcomes
Robust data collection and reporting are critical in driving equity in outcomes for people living with COPD. Local strategies should reflect the evolving roles and responsibilities as set out in the Model ICB and Model Region blueprints.
Actions
- Implement systems and support commissioned services to contribute to national audits and data dashboards for system-wide evaluation of core COPD interventions, such as OPTIMISE, pulmonary rehabilitation and biologic uptake. Service models should include governance measures to ensure secure, consistent data collection, transfer, and compliance with data protection requirements.
- Promote the use of automated, user-friendly platforms, such as the NHS Federated Data Platform, to support consistent data sharing, reduce manual data entry, and enable multidisciplinary use. Reliable commissioning and clinical decision-making rely on:
- standardised data definitions
- timely reporting
- transparent validation and audit processes
- Regularly review data to identify variance in care and outcomes, including analysis by locality, deprivation and ethnicity. Key indicators should include:
- diagnosis rates compared to expected prevalence of COPD
- uptake of OPTIMISE components (for example, tobacco dependency support, pulmonary rehabilitation)
- bed occupancy and premature mortality rates
Resources
Appendix 1. COPD: A population health management approach
This provides a guide to COPD interventions throughout each stage of disease and the appropriate positioning of biologic therapies. The fundamentals of COPD care should be treated as essential and consistently optimised across all pathways.
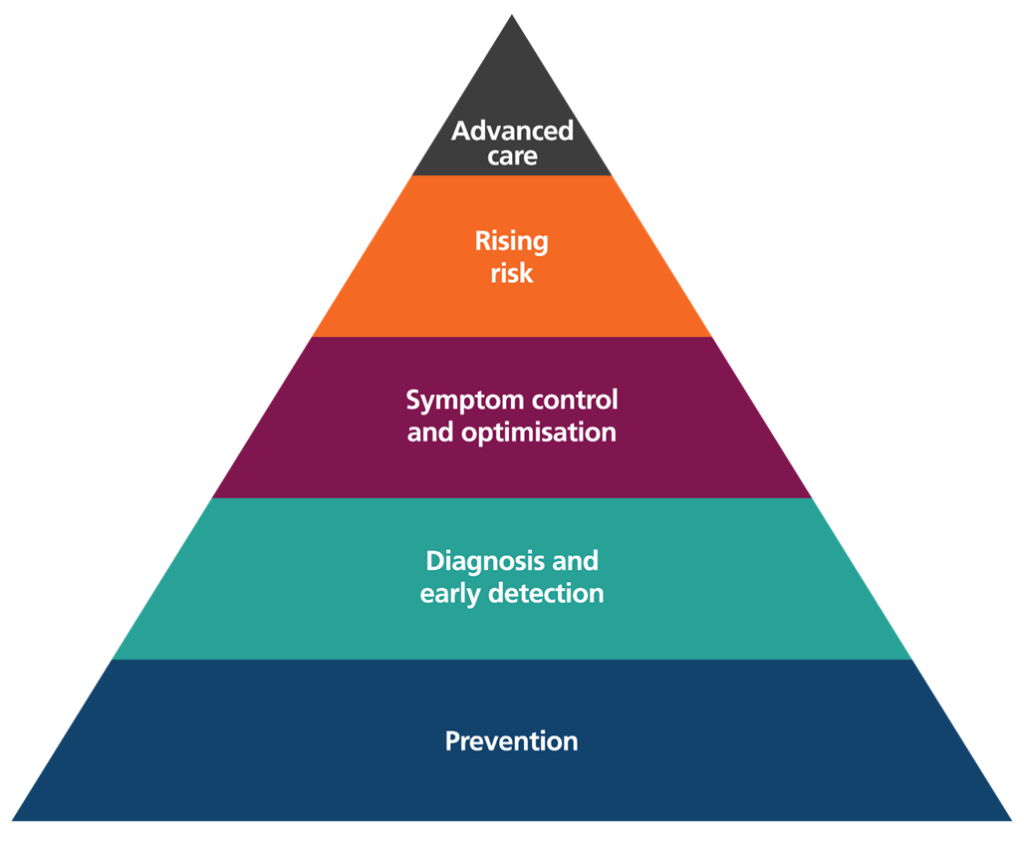
Prevention
Cohort
- Healthy population
Approach
- Define and identify at risk groups for review
Intervention
- Address wider social determinants of health
- Modify risk factors across the life course
- Promote healthy lifestyle
Diagnosis and early detection
Cohort
- Adults over 35 years old
- Current or ex-smokers with 10 or more pack year history
- History of exposure to other risk factors and or significant passive smoking
- Routine and manual workers, or those from high-risk occupations
- People living with deprivation, serious mental illness, addiction, homelessness
- Symptoms of cough, sputum, wheeze and/or breathlessness
Approach
- Proactive case finding
Intervention
- Equitable access to quality assured diagnostic spirometry and breathlessness pathways
- Integrated neighbourhood models of care
Symptom control and optimisation
Cohort
- Patients with quality assured diagnosis of COPD and daily symptoms
Approach
- OPTIMISE COPD
- Integrated neighbourhood models of care
Intervention
- Vaccination
- Tobacco dependence treatment and support
- Pulmonary rehabilitation
- Evidence based inhaler treatment as appropriate
- Personalised care
- Self-management support (including the use of digital apps)
- Optimisation of risk factors and co-morbidities
Addressing rising risk
Cohort
- Patients with quality assured diagnosis of COPD with exacerbations, significant breathlessness or both
Approach
- Integrated care with specialist review
Intervention
- Assessment of biomarkers and consideration for biologic therapy
- Assessment of infection markers and consideration for antimicrobials
- Consideration for lung volume reduction intervention
- Assessment and support for psychosocial needs
- Hospital at home offer
- Specialist review
Advanced care
Cohort
- Patients with quality assured diagnosis of COPD who present with severe symptoms, severe exacerbations, respiratory failure or secondary complications
Approach
- Specialist led care
Intervention
- Oxygen therapy or non-invasive ventilation
- Nutritional support
- Personalised advance care planning and support
- Consideration for lung transplantation
Publication reference: PRN02144_i

