Summary and introduction
The Delivery plan for recovering urgent and emergency care was published in January 2023, setting out a 2-year action plan from April 2023 – backed by a £1 billion improvement package and £200 million ambulance fund – with the ambition of reducing the time people spend in A&E or waiting for ambulances to arrive.
The plan set out a series of actions to achieve this under the headings of:
- increasing capacity
- growing the workforce
- improving discharge
- expanding and better joining up health and care outside hospital
- making it easier to access the right care
Over the first year of the plan, the NHS and social care have made significant and substantial progress on commitments made in the delivery plan.
As a result, improvements on the headline ambitions were achieved:
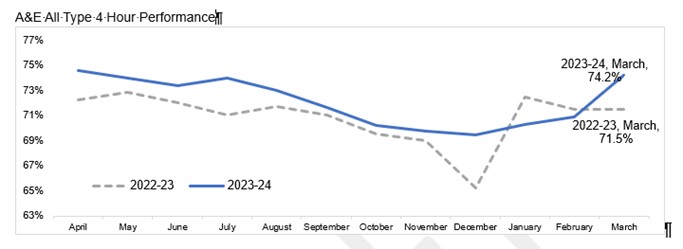
- in A&Es, the proportion of patients completing their treatment within 4 hours improved to 2% in March 2024. That is 2.7 percentage points better than the previous year – and overall 2023/24 is the first non-pandemic year since 2009/10 to see a year-on-year improvement
- in ambulance services, the average response time for ‘emergency but not life-threatening’ (Category 2) calls in 2023/24 was 36 minutes 23 seconds, over 13 minutes (27%) faster than the 2022/23 average of 50 minutes
This was achieved despite record demand, a challenging winter due to seasonal illnesses, and protracted industrial action affecting hospitals and wider health services.
Further work will continue to improve both measures, as well as the experience of patients, over 2024/25.
Delivering on our priorities
We have delivered, or are on track to deliver, on all the key actions in the plan:
- the target of 5,000 additional core general and acute beds, against previously planned levels, was met and consistently exceeded in January 2024, supported by £250 million for 30 capital schemes across the country
- we have met the ambition of ensuring all hospitals have a care transfer hub, which works across the NHS and social care to manage discharges for patients with more complex needs. There was an 11% increase in hospital discharges (1,000 patients per day on average) compared with the previous year, supported by the £600 million Discharge Fund, and we have seen a 13% increase in the number of supported discharges reflecting an increase in adult social care capacity
- continuing to build up new services in the community, which can provide an alternative to ambulance call-outs or trips to hospital – including consistently exceeding the standard for 70% of requests for an urgent community response to receive one within 2 hours, with current performance at 85% and 20,000 more referrals in the most recent data than the same month last year
- 604 double crewed ambulances were delivered, with that number expected to rise to 800 by the end of June 2024, as well as 28 mental health specialist ambulances. In December 2023 there were 5.8% more ambulances (overall hours on the road) than in December 2022
- created almost 12,000 virtual ward ‘beds’ allowing patients to receive hospital-level care at home, with 73% of this capacity used in March 2024 – the equivalent of 20 hospitals’ worth of beds
- increased the availability of packages of health or social care to help more people continue their recovery at home or in a community bed after being discharged from hospital
- systems planned 200 acute respiratory infection hubs between December 2023 and February 2024 to enable people to get help for common seasonal conditions and flare-ups of asthma
- system co-ordination centres are now live in all areas of the country to help ensure hospitals and other services have the right capacity in the right places
- all hospitals with major A&Es now operate same day emergency care services, with 84% of them operating for over 84 hours a week, enabling people to avoid an overnight admission where this is not necessary
- increasing the urgent and emergency care workforce – including a 4.7% growth in the paramedic workforce from April 2023 to December 2023 and continued growth in ambulance support staff
- supporting our most challenged systems has helped level up performance – with those receiving the highest level of support improving twice as fast as others
What this meant for patients
2023/24 was the first year outside the pandemic since 2009/10 where A&E performance (as measured by the proportion of people completing treatment within 4 hours) was better than the previous year. Over the year, over 2.5 million more people completed their A&E treatment within 4 hours compared to 2022/23.
Ambulance response times were also significantly better, with the average time taken for ambulances to arrive for emergency but not life threatening calls over 13 minutes faster.
Other benefits for patients included:
- tens of thousands more people received the care they needed to return home quickly and safely thanks to the expansion of same day emergency care services
- on average, around 500 fewer patients per day had to spend the night in hospital because of a discharge delay
- supported by the £600 million Discharge Fund, 13% more patients received a short-term package of health or social care to help them continue their recovery at home or in a community bed after being discharged from hospital – over 60,000 extra in total
- urgent community response teams provided 720,000 people with an alternative to going to hospital between April and January
- virtual wards have supported more than 240,000 people to get the hospital-level care and monitoring they needed in the comfort of their own home
Continuing progress
We are now beginning the second year of this 2-year plan. Building on the improvement already made by health and social care staff, the headline ambitions for 2024/25 are:
- improve A&E waiting times, compared to 2023/24, with a minimum of 78% of patients seen within 4 hours in March 2025
- improve Category 2 ambulance response times to an average of 30 minutes across 2024/25
Local NHS and social care teams are also asked to reduce the proportion of waits in A&E that are over 12 hours – including for those in mental health crisis – compared to 2023/24.
Key to delivering the improvements we want to see this year will be:
- maintaining and increasing the extra beds, ambulances and community capacity delivered through 2023/24
- improving processes so that people spend less time waiting – whether that is to be assessed in A&E, admitted to a ward if they need to be, and discharged when they are ready to be – at the same time as making care better and safer
- developing services that can help people with urgent needs get the right support in the right place, without the need for them to go to or stay in hospital
Details on these ambitions and the evidence-based actions that local teams can take to achieve them have been set out in letters to NHS leaders and local authorities.
£150 million of funding will support specific local improvement plans for urgent services, including for mental health care. These new improvements will support patients being treated more quickly in A&E or by other services in the community. A further £150 million will be available to incentivise the best performing areas and those that improve fastest.
The NHS and local authorities will also work together to expand intermediate care services, both in people’s own homes and in community beds, thanks to the additional £400 million Better Care Fund available to support further improvements in hospital discharge.
There will also be further improvements to, and co-ordination of, community-based services that support people to avoid ambulance call-outs and hospital admissions, by treating people in the most appropriate place for their level of need. This includes:
- more people benefiting from urgent community response services
- ensuring that patients with mental health needs and children and young people are explicitly included in plans to make further improvements in services
- more people supported by high intensity use services as a cost-effective intervention to both manage A&E demand and address health inequalities
- more proactive care for people most at risk to prevent people’s needs from escalating; for instance, through falls prevention, home adaptations and assistive technology, telecare, and healthcare input into residential and nursing home settings
Publication reference: PRN01288_ii