Version 4
1. Introduction
As part of the Emergency Preparedness Resilience and Response (EPRR) Framework, NHS organisations and providers of NHS funded care must show that they can effectively respond to disruptive events and maintain patient care.
Organisations should have procedures in place for evacuating their facilities and sheltering patients, the public and staff, in the event of major disruptions.
There are various events that may require an organisation to shelter and/or evacuate patients, the public and staff. These can include:
- a structural, power or other utility failure
- an explosion or suspect package
- adverse weather, eg flooding
- a fire
- a release of irritant fumes or hazardous materials
- a terrorist event.
1.1 Purpose
The purpose of this document is to provide guidance to providers of NHS funded care and services in the preparation and response to the evacuation and/or shelter of patients, staff and the public from, or within, healthcare settings.
The guidance supports all NHS funded organisations in England to comply with the requirements of the Civil Contingencies Act 2004 (CCA 2004), the NHS Act 2006, the Health and Care Act 2022 and the NHS Standard Contract. This guidance also supports, but does not supersede, the relevant regulations dealing with health and safety and fire.
While this guidance concentrates on the evacuation and shelter of hospital sites, the principles are sufficiently flexible to be adapted for use in respect of other buildings or facilities on healthcare provider sites or to wider primary, social and community care and independent sector facilities.
Evacuation and shelter plans should dovetail with other relevant generic and specific organisational plans and be developed in collaboration with partners and relevant stakeholders to ensure the whole patient pathway is considered.
Evacuation and shelter guidance for the NHS in England (2021) has replaced the Planning for the shelter and evacuation of people in healthcare settings (2015) guidance. As part of this, both the Health Evacuation Triage Priorities algorithm (Figure 1) and table (appendix 1) have been updated to address the following:
- Remove reference to Evacuation Priority 4 (EP4) Leave in Situ/Consider analgesia in the algorithm and table on the basis that all efforts should be made to evacuate all patients as appropriate in their turn. See section 5.2.4 Deferred evacuation register.
- An inaccuracy in the algorithm whereby patients who weren’t at risk of moving would be left in situ. This was counter-intuitive to the principles of the evacuation triage priorities.
- The evacuation priority numbers in the table (appendix 1) have been amended to reflect the order that should be considered for initial evacuation.
- The table (appendix 1) has been updated to reflect the outcomes of the algorithm.
As part of an annual refresh of this document in 2022, in addition to minor amendments, further changes have been made to the guidance including:
- the need to follow Joint Emergency Services Interoperability principles (JESIP) when making decisions to evacuate facilities, particularly in instances where other emergency services may have primacy of the overall incident response (section 1.2)
- the roles and responsibilities of Integrated Care Boards following their establishment as statutory bodies (section 2.3)
- the requirement that patients requiring additional support during a shelter and/or evacuation event should have their needs predetermined and documented (section 3.2)
- clarification of the requirement for Personal Emergency Evacuations Plans (PEEPs) for members of staff who may not be able to reach a point of safety unaided or within an adequate amount of time during an emergency evacuation (section 3.3.1).
1.2 Scope
Evacuation and shelter planning arrangements must be flexible to allow the response to be tailored to the event.
Evacuation and shelter planning is part of broader emergency preparedness, and should align with existing arrangements including:
- command and control
- major incident and mass casualty plans
- fire response plans
- business continuity
- mutual aid
- lockdown plans.
Providers without inpatient facilities can use this guidance as appropriate and applicable to their facilities and available resources.
NHS-funded organisations are responsible for the decision to evacuate their own facilities; however other emergency services may have primacy of the overall response depending on the type of incident resulting in the requirement to evacuate. In these circumstances it is important to follow JESIP principles in order that such decisions are jointly agreed based on joint understanding of risk and shared situational awareness.
NHS-funded organisations will remain responsible for patients evacuated from their facilities, and for the continued delivery of care and treatment – whether in healthcare premises or not – until those patients are formally discharged from their care.
Inevitably, in situations which call for prioritisation of resources, healthcare staff will be conscious of their responsibilities towards the group of patients in their care, as well as responsibilities to each individual patient.
1.3 Definitions
1.3.1 Evacuation
Evacuation is defined as the movement of patients, the public and staff from a building to a place of greater safety.
1.3.2 Partial evacuation
Partial evacuation involves moving away from the area of danger to a safe place within the same building, taking account of known potential hazards including structural integrity. This can be achieved by evacuating:
- ‘Horizontally’ to an area on the same floor. If fire is the cause of evacuation, movement should be to the next fire compartment section on that floor ie through at least one set of fire doors.
- ‘Vertically’ to the floor above or below the area of danger, as appropriate.
All areas should have plans for partial evacuation, developed with a Fire Safety Officer.
1.3.3 Full site evacuation
The total evacuation of a provider site, including all the buildings on it.
All inpatient care facilities should have incremental plans in place including whole site evacuation.
1.3.4 Off-site evacuation
Evacuation to an off-site location to provide an area of safety away from the affected site, which may be a temporary location until patients are either redirected to another healthcare setting or are discharged/taken home.
Common choices for off-site evacuation locations may include:
- churches
- town halls
- community centres
- local authority rest centres.
1.3.5 Shelter
Shelter is defined as taking refuge or cover in the current location. Shelter locations should consider local fire compartment planning.
1.3.6 Evacuation clearing station
An area – usually on site, although it can be off site – which can provide a place of temporary shelter for those being evacuated.
1.3.7 Patient dispersal arrangements
Pre-defined arrangements outlining the dispersal of patients evacuated to other organisations.
Patient dispersal arrangements should form part of the organisation’s off-site evacuation plan, made in consultation with multiagency partners.
To ensure system wide tracking and interoperability all providers should ensure that they have in place appropriate and robust arrangements for both the sending of patients (where they are the affected site) and receiving of patients from other providers that they may reasonably be expected to receive patients from.
Any system must have the ability to track a patient from end to end to ensure appropriate clinical governance arrangements are in place.
1.3.8 Mutual aid
An agreement between responders – within the same sector, or across sectors and across boundaries – to provide assistance, through additional resource, during incident response which may go beyond the resources of an individual responder. (See section 3.9 Mutual Aid for more information.)
1.3.9. Lockdown
The process of controlling access and egress to a facility, site, service or building.
2. Roles and responsibilities
2.1 Providers of NHS-funded services and care
NHS funded organisations should develop shelter and/or evacuation arrangements for each site or building with assistance from the organisation’s EPRR manager. The following internal stakeholders should also be involved in this process:
- estates/facilities departments
- fire safety officer
- health and safety advisors
- clinical teams
- on site retail establishments
- patient transport services
- communication teams
Organisations – particularly with inpatient facilities – may wish to consider developing off site plans with external partners. These arrangements should include a patient dispersal plan if patients are to be moved off site. Recognising different healthcare environments, provider organisations are responsible for considering the patient cohorts, specialties and services for which they provide care when identifying suitable off-site arrangements.
2.2 Ambulance services
Ambulance services have a role in assisting the evacuating organisation if necessary. Assistance should be provided as appropriate through:
- patient transportation to other organisations/locations
- redirecting ambulances to other organisations
- providing a tactical and/or strategic commander to attend the multiagency tactical co-ordination group/strategic co-ordination group (TCG/SCG) as appropriate.
2.3 Integrated care boards
Integrated care boards (ICBs) are required to work with NHS England in discharging their EPRR function. ICBs should ensure integration and collaboration of planning arrangements across an ICS to deliver a unified response to any emergency.
During an evacuation and/or shelter event, ICBs are responsible for:
- establishing strategic and tactical leadership arrangements and support structures to effectively manage and co-ordinate the NHS response and recovery across their integrated care system, representing the NHS at Strategic Coordination Groups and Tactical Coordination Groups when required
- providing leadership should mutual aid arrangements be activated to support an evacuation and/or shelter incident
- ensuring robust escalation procedures are in place through the EPRR command structure in line with the NHS EPRR Framework.
2.4 NHS England
NHS England should ensure integration of planning arrangements across the region to deliver a unified response to any emergency in line with this guidance. This includes supporting organisations during the response and recovery phases of an incident or emergency.
During an evacuation event, NHS England are responsible for supporting:
- ICBs in brokering mutual aid requests to assist evacuating organisations
- the multi-agency response through attendance at TCG/SCG as appropriate
- escalating incidents as appropriate through the EPRR command structure.
This can be supported by the activation of national and/or regional incident response plan as necessary.
3. Planning considerations for evacuation and shelter
3.1 Communications
Communications during a shelter and/or evacuation event should come from a single source which is regarded as authoritative and represents the response. Consistent messaging is important and reduces the risk of miscommunication as well as conflicting messages.
Organisations should make arrangements to communicate to patients, the public and staff on and off site during the event.
Evacuation messages on site should include:
- additional security requirements
- responsibilities for staff
- specific action to take (eg evacuate the building, help others where possible, etc)
- directions to assembly points/evacuation clearing stations.
Off-site evacuation messages should include:
- advice on how to continue to access services (maternity and emergency care)
- where family members can get information on the evacuation (specifically where their loved one(s) are now located)
- advice on the process for urgent visits.
When developing communication strategies, organisations should consider:
- methods of communicating using on site communications, eg public address systems, to activate an evacuation plan and direct patients, the public and staff as appropriate
- methods of communicating with patients, the public and staff who:
- do not speak English as a first language
- do not hear
- may have difficulty understanding complex messages
- have specific communication needs.
- using social media, eg Twitter and Facebook, to direct people away from the site and provide updates on the incident and resumption of services
- how strategies link to the wider Local Resilience Forum (LRF) warning and informing strategy
- maintaining up to date contact details of staff and relevant stakeholders
- communication methods if the building is compromised
- the use of alternative methods of communication, eg staff as ‘runners’
- a means of ensuring message clarity
- a method of communicating a full site evacuation if a fire alarm system is being used.
3.2 Patients who may need additional support
Particular consideration should be given to patients who may need additional support during the planning and response of shelter and/or evacuation events.
This may include, but are not limited to those:
- in high dependency units
- in critical care
- in theatres recovery
- in maternity units
- in isolation units
- in secure inpatient settings
- with a disability or health condition that may affect their mobility
- who are frail
- with dementia
- in mental health inpatient settings
- with severe mental illness
- who have a learning disability
- who are autistic
- with speech, language and communication needs.
When evacuating and/or sheltering those who need additional support, considerations should be given, but not limited to:
- the patients’ specific needs, including patients who need to be isolated
- reasonable adjustments for people with a disability
- the number of staff required to accompany the patient
- ensuring appropriate equipment is available during transit
- legal restrictions on the person in a mental health (including secure) inpatient settings
- maintaining adult and child safeguarding arrangements
- ensuring the shelter/evacuation location has sufficient resources eg drugs, fluids, consumables, etc.
Patients requiring additional support during an evacuation and/or shelter event should have their needs predetermined and documented as part of general care planning. Recognising that a patient’s condition and therefore their support needs to evacuate may be transient, this information should be kept under review. This information might be noted in patient case notes and/or ward boards but should be accessible and referred to as soon as notification of a potential evacuation has been received in order to inform patient assessment and evacuation triage process (see section 5.2).
3.4 Staff safety
Accounting for staff during an evacuation can be challenging. Organisations have a duty of care to know which staff are working within a building at any one time, including contractors who may be working on site.
Staff rotas can be used to provide a list of staff at work and should be available at short notice in most work areas.
Staff should not be asked to undertake a role they are not comfortable performing or trained to undertake, nor should they be expected to put themselves at risk or in danger of injury.
3.3.1 Personal Emergency Evacuation Plans (PEEP)
A Personal Emergency Evacuation Plan (PEEP) is a bespoke plan for individual members of staff who may require additional support during an evacuation and/or shelter event.
The PEEP should consider assistance required during the evacuation process and include any necessary equipment and security arrangements/ reasonable adjustments to keep the person safe.
A PEEP should be accessible and referred to as soon as notification of a potential evacuation has been received. There may be other groups who require a PEEP as determined by local risk assessment (eg regular visitors, volunteers, contractors etc.). For more information and guidance on PEEPs, you should liaise with your local Fire Safety/ Health and Safety Officer.
3.4 Equality and diversity
During an incident requiring shelter and/or evacuation, organisations should continue to maintain arrangements for reducing inequalities in the access to treatment and healthcare.
It will also be necessary to enhance the organisation’s communication arrangements for people with specialist needs, including provision of key phrases in different languages, or language free instructions.
An equality and health inequalities impact assessment (EHIA) has been undertaken to demonstrate the consideration given to the potential impact of this guidance for protected characteristic groups and groups who face health inequalities. Particular consideration has been given to the hospital evacuation triage priorities.
It is recognised that some aspects of this guidance may indirectly negatively impact certain groups who may experience reduced mobility and increased dependency. To reduce adverse impacts, careful consideration should be given to individual patients’ needs and reasonable adjustments made to provide appropriate support and/or assistance as necessary as set out in section 3.2.
3.5 Security
Building security is a principal concern while a site is being evacuated. The use of lockdown arrangements to control the access and egress to a building or area is an effective way of achieving this and can also prevent further safety issues.
The local police force will attend the site if there is a criminal act taking place.
3.6 Stakeholder engagement
It will be necessary to engage with external stakeholders including local resilience forum (LRF) partners in the development of and response to events resulting in either shelter and/or evacuation. Organisations should ensure their facilities are appropriately risk assessed through the community risk register, and specific plans are in place for the ‘high risk’ sites.
Ambulance service(s) should be engaged with if a redirection of incoming emergency patients from the site is required. Ambulance services can also be approached to assist in the provision of transport.
Local authorities will be able to assist with the identification of off-site relocation sites, and transportation by commercial providers.
During the planning phase, police service(s) will be able to provide advice on the counter terrorism threat. During response, they will be able to provide a reactive response to criminal activity on site, as well as assistance with traffic management.
During the response to an evacuation event, fire and rescue service(s) will provide a firefighting and rescue service to organisations. They may also be able to provide advice and assistance where there is difficulty moving a patient.
Neighbouring NHS organisations will be essential for the provision of support with mutual aid requests and assistance with transportation.
3.6.1 Emergency service liaison
Organisations should consider identifying an individual able to liaise with the emergency services on site. This individual should be familiar with the site layout including pedestrian and vehicle access routes and have access or the ability to access all areas on site. This individual could be responsible for:
- coordinating any emergency service activity required on site
- allowing the emergency services on site
- directing the emergency services to an appropriate rendezvous point.
3.7 Transportation
Organisations will need to consider the transportation required to support shelter and/or evacuation. This may form part of existing mutual aid agreements the organisation has in place with multiagency partners.
Particular attention will need to be given to the transfer and movement of patients:
- on site, between buildings
- to places of shelter on site
- from one healthcare site to another
- to shelter and/or evacuation areas off site
- to their home.
Organisations should identify possible sources of transportation. These could include:
- ambulance services
- patient transport services
- private companies
- secure patient transfer
- voluntary services.
Consideration should be given to the following:
- Liaison with local health partners and the LRFs to ensure that several organisations are not dependent on the same transport organisations.
- Transport arrangements with safe routes identified both on and off site.
- Relevant requirements and command arrangements should be written into private ambulance transport contracts.
- Transfer of patient information if transport is provided by a non-NHS organisation.
3.8 Equipment
Organisations should consider the need for evacuation equipment and an accessible store of appropriate equipment – including (not exhaustive):
- evacuation sheets
- ski pads
- evacuation chairs
- stretchers, etc.
Where appropriate organisations should make provision of bariatric evacuation equipment which can be deployed as needed.
All evacuation equipment should be tested on a regular basis to ensure staff are familiar with how to use it and appropriate records maintained.
3.8.1 Evacuation packs
Organisations may want to consider evacuation packs in appropriate locations eg inpatient areas to assist staff during an evacuation.
If safe to do so, the evacuation packs should be collected by a staff member during the evacuation of the area.
Evacuation packs may contain the following:
- evacuation plan
- a mobile phone programmed with ‘useful numbers’
- notebooks and pens
- head torches
3.9 Mutual aid arrangements
As part of off-site evacuation planning arrangements, it may be necessary to transfer patients to other organisations. Therefore, arrangements need to include the dispatch and receipt of patients outside of normal transfer processes, and in large numbers.
All organisations should consider how they could accommodate transferred patients including outlining arrangements for:
- accessing patient documentation
- registering patients on relevant systems
- prescribing of and access to essential drugs
- transport of the patient to the evacuation location, including an escorting staff resource.
Mutual aid arrangements can be drawn on to provide support in the coordination of the evacuation and information on the capacity/capability of ‘assisting’ and ‘requesting’ organisations during evacuation.
3.10 Recovery
Both business continuity and recovery planning should start as soon as possible, ideally during the incident. Early consideration of recovery and patient repatriation options will ensure a smooth transition through each stage of the incident.
The recovery team should be led by a senior director, independent of the incident management team, but liaising closely with them.
3.11 Community evacuation
Community evacuation, where the population of a large area may need to be evacuated, needs to be considered by NHS organisations. The Cabinet Office has developed guidance for LRF members to support the development of evacuation and sheltering arrangements in these circumstances.
This guidance is available on the gov.uk website
Although an organisation’s primary responsibility in an evacuation will be the evacuation of its own healthcare facilities, they need to consider how they will support this wider planning for community evacuation. Specifically, organisations need to be involved in the development of arrangements for:
- Medical and emergency aid cover at any established evacuation centre, or reception centres, this may include emergency provision at transport hubs. This provision should be considered in the context of the wider evacuation, and available resources for undertaking evacuation.
- Ensuring information relating to vulnerable people can be gathered and collated quickly from across the community being evacuated for use by the emergency responders and those coordinating the evacuation. This will need to include information held in primary and secondary care.
- Assessing the suitability of evacuation centres for use by those that are currently under care. This may include ensuring centres have areas suitable for patients under the care of mental health providers, or suitable access facilities.
- Continued patient care of those in the community, this may be the continuation of the care being received from an organisation, or the tracking of the patient into the care of another provider in the receiving community or area. These patient groups are likely to be under the care of outreach or district nursing teams in their own homes, so any evacuation may occur prior to the organisation becoming aware.
- Although evacuees are asked to take supplies of medicines with them, health services will need to be prepared for a surge in demand following any community evacuation as patients present to replace medications. Consideration also needs to be given to those who are reliant on others for the administration of their medicines. It is highly likely there will be further healthcare demands following large scale evacuation on mental health providers.
- Ensuring that the organisation is made aware of the areas under evacuation and continues to maintain the safety of its own staff during this evacuation. The ability to rapidly communicate with teams working within the community where the evacuation is happening will be necessary.
- Some or all of your staff may have been placed under the evacuation order. As such it will be necessary to consider their welfare arrangements and reassure them during the evacuation. It is also important to ensure they are aware of arrangements for the evacuation of schools and care homes in their area.
4. Shelter
In some scenarios, such as a chemical plume or marauding terrorist incidents, it may be safer to take refuge or cover in the current location. This sheltering in situ may lead to a subsequent evacuation. Therefore, while sheltering, staff should be preparing for an evacuation.
When developing plans for in situ sheltering the organisation must ensure that it has considered the following:
- The building’s integrity – ie can windows and doors be closed to prevent any contamination if there is a chemical plume. It may be necessary to compartmentalise buildings into areas which are safer for sheltering.
- Some sheltering situations may need patients to be away from windows or doors to prevent possible injury from flying glass. This will result in a smaller shelter footprint than the building size.
- How access to the building will be maintained if it is not directly connected to a main site. Smaller buildings may not be suitable for long term occupation, this will be especially important if emergency teams need to access the building or supplies need to be sent to the building.
- Is there on-site access to toilets, kitchen/food provision and other facilities for maintaining the comfort of those people contained within the building. These facilities should be able to support the number of people in the building.
- Where possible buildings will need to be resilient to the loss of essential services such as power for a period of time. Where buildings have no resilience, they should be flagged for earlier evacuation.
- How communication between buildings and sites will be maintained especially if there is disruption to routine communication methods and if the use of runners is inappropriate.
- Ready to respond to the needs of those who may find changes in environment and increase sensory disturbance/ overload challenging.
5. Evacuation stages
5.1 Stage one: decision to shelter and/or evacuate
The decision to shelter and/or evacuate should be made by a nominated individual on behalf of the organisation’s chief executive officer, eg director on call. A ward or facility within a building will be evacuated based on a risk assessment conducted by the senior clinician on duty.
The following should be considered:
- nature of incident (including any known infrastructure risks)
- overall risk to patients, the public and staff
- nature and diversity of patients cared for on site
- staffing available
- command and control arrangements required
- risks associated with the location(s) of certain types of patients
- substances kept on site and the cordoning arrangements for this.
Organisations will be required to establish incident management arrangements and an incident co-ordination centre (ICC) in response to an event requiring shelter and/or evacuation of their site and therefore will need to consider activating other incident response plans. An alternative ICC location may also be required if the primary location is unavailable.
5.2 Stage two: patient assessment
5.2.1 Initial patient triage
In the event of an incident requiring evacuation it is essential that proper mechanisms are in place to triage and track patients. The initial evacuation triage process should determine the:
- patient’s mobility and resources required to evacuate the patient
- patients ongoing care needs
- type of transport required to facilitate the onward evacuation of the patient.
When considering whether to move a patient, there are a number of factors which should be considered including the:
- difficulty of movement eg mobility of the patient and what equipment is required to ensure patient care
- time required to move one patient versus moving other patients
- risk to the:
- patient if moved
- patient if remaining in situ
- staff
Organisations should ensure there is a robust mechanism for evacuating patients along with their notes. This is the responsibility of the clinician caring for the patient.
Conducting an initial triage of patients will allow direction to the most appropriate care setting and establish an order for evacuation based on mobility – the most mobile patients should be moved first, especially those who are able to walk, through self-evacuation.
An initial triage should assign patient mobility as one of the following:
- able to walk
- chair required
- bed/stretcher required
- more complex needs, eg bariatric, ventilated.
Additionally, the patient should be assessed as:
- not requiring ongoing care
- requiring ongoing care.
- those who will need to be transferred off site for continued care.
Inpatient consultant led speciality teams and nursing staff will have a key role prioritising patients for inter-hospital transfer, if required.
Following any evacuation, it is likely there will be a requirement to reassess (re triage) patients.
5.2.2 Healthcare evacuation triage priorities
The healthcare evacuation triage priorities table (appendix 1) is a reversed adaption of the national ambulance service major incident triage card system (eg TSG Associates Smart cards) based on mobility and dependency to determine evacuation priority by categorising patients into ‘very dependent’, ‘dependent’, and ‘independent’ groups.
The healthcare evacuation triage priorities table has been developed to assist healthcare staff with making decisions on whom to evacuate and in what order. It should be noted that the definitions of each category in the table in appendix 1 are not prescriptive or exhaustive. It is important to remember that any triage process is dynamic and iterative, and should be repeated at appropriate intervals.
The triage should be undertaken based on the practicality of evacuating individual patients as a result of their own mobility, dependency and resource required, including staffing, equipment and time. Patients should not be eprioritised/deprioritised solely in terms of their pre-existing conditions (i.e. in isolation of the impact on an evacuation situation).
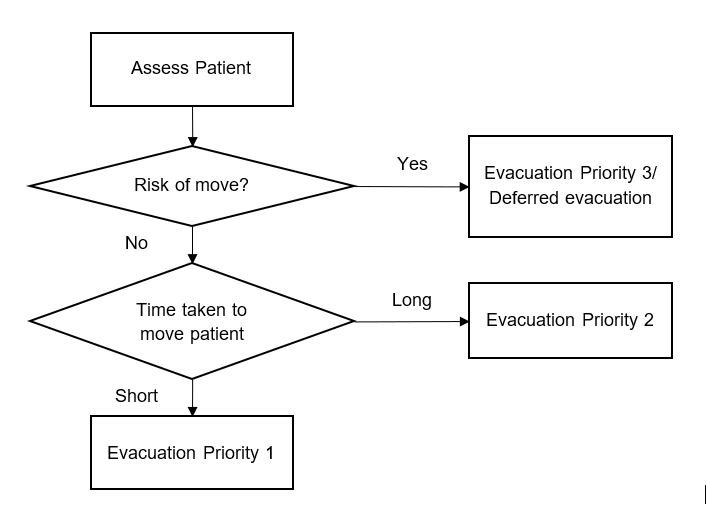
The principles of the healthcare evacuation triage priorities can be set into a simple algorithm below:
Figure 1: Health evacuation triage algorithm
5.2.3 Evacuation register
At all stages of evacuation, a record/register should be maintained of patient movements for each area being evacuated. The evacuation register should be retained by someone trained and competent, e.g. a senior ward sister.
When leaving an area, the patient’s details, mobility and care requirements should be recorded in an evacuation register along with their intended destination.
5.2.4 Deferred evacuation register
In some situations, it may be appropriate to defer the evacuation of a patient. For example, if there is limited equipment/staff available initially to evacuate them.
The decision to defer evacuation of a patient for medical reasons should be made by two clinicians. This must be recorded on a ‘deferred evacuation register’ along with the reason they are deferred.
The organisation should then appoint a senior clinician to have oversight of all deferred evacuation registers. This person will assume responsibility for ongoing patient care.
This person must assess the reasons for deferral and make all reasonable attempts to resolve them. This can include, where appropriate, a discussion with the fire and rescue service regarding the availability of additional or specialist resources to facilitate patient evacuation.
In extreme circumstances, where a patient is deemed unfit to survive evacuation, the demands of the situation outstrip available resource, or staff are likely to be put at risk of moving a patient, it may be appropriate to leave a patient in situ until appropriate resource or mitigations of risk become available. As above, this decision to leave a patient in situ should be made by two clinicians and recorded on the deferred evacuation register along with the reason.
The incident management team should provide formal approval to continue or stop further rescue attempts for a patient who cannot be moved. These attempts should not place staff at risk of harm.
5.3 Stage three: dispersal
5.3.1 Evacuation clearing station
Once assessed, patients can be directed to an appropriate evacuation clearing station. These should provide a:
- place of temporary shelter for evacuees
- safe place to assist in managing the onward movement of patients requiring further care.
Initial triage can also identify patients eligible for early discharge to create additional capacity in inpatient facilities.
For example, evacuees can be directed to a specific clearing station according to their need:
- patients with immediate/urgent healthcare needs
- patients without immediate/urgent healthcare needs.
The organisations may need to establish multiple clearing stations, which could be on or off site.
The naming convention for any clearing stations, and potential locations should be shared with multiagency partners to avoid confusion during an evacuation.
5.3.2 Patient Dispersal Team
When undertaking an evacuation, organisations may wish to consider establishing a patient dispersal team (PDT). This team should be made up of staff able to identify available capacity and allocate patients for evacuation according to their care need.
As appropriate to the organisation, a Patient Dispersal Team could consist of:
- senior doctor
- senior nurse
- decision loggist
- casualty bureau liaison officer
- transport officer
- other health organisations able to offer support, eg ICB, community trusts, adult social care representatives.
The PDT should receive evacuation registers, and match patient care and transport needs with the available resources.
Patients should be allocated transport and resources eg beds, based on their care needs and their priority categorisation as determined by the evacuation clearing station.
As soon as care is allocated, the evacuation clearing station must be informed of the estimated time of arrival for transport to ensure the patient is ready.
The PDT should be informed when the patient has been transferred off site and should update the Patient Dispersal Register with the transfer time.
5.3.4 Transport team
When undertaking an evacuation, organisations may wish to consider establishing a transport team. Working closely with the PDT, the transport team is responsible for transporting patients to an appropriate location.
During multiagency responses and/or off-site evacuation, these teams will need to be made up of multi-agency partners.
5.4 Secondary triage
While in a place of safety a secondary triage can take place. This process would involve recording the patient’s:
- main health complaint(s)
- allergies
- additional information eg care requirements and isolation
- National Early Warning Score 2 (NEWS2) and corresponding evacuation priority, eg P1, P2 or P3.
- transport requirements.
Once secondary triage has been conducted, the patient’s main complaint and priority should be recorded on a ‘Patient Dispersal Register’ along with the following patient requirements as appropriate:
- type of bed
- care
- details of the transport type required.
The PDT can use this information to allocate the required resources, eg appropriate bed, equipment, and mode of transport.
The secondary triage to determine priority for onward transfer has been integrated into the Healthcare Evacuation Triage Priorities table (appendix 1)
5.5 Patient receipt
A record should be kept of all patients received at an ‘assisting organisation’. This record should include details of the patient’s new location and reported back to the requesting organisation.
Systems in place across geographies must ensure that they have suitable arrangements as part of their pre-determined triage and tracking system that are interoperable.
6. Training
Organisations should ensure staff are familiar with evacuation and shelter arrangements.
It is important that all staff understand what is expected of them, their role and responsibilities during a shelter and/or evacuation event.
Staff should be involved in the development and review of training.
Where evacuation equipment is provided, staff should be adequately and regularly trained in how to use it correctly. There should be sufficient numbers of appropriately trained staff on duty at all times. A training record should be maintained.
7. Exercising
Exercising using an evacuation and shelter scenario should be a formal part of the organisation’s EPRR exercise programme.
Staff should be given the opportunity to practice their use of all available evacuation equipment during exercises.
Any new evacuation equipment purchased should be tested in house to ensure that it is compatible with the building infrastructure, eg testing new beds and ensuring all equipment fit through fire escape routes identified for use, etc.
Learning from exercises should form part of the organisation’s continuous improvement cycle, incorporating lessons identified into evacuation arrangements, and other response plans.
Appendix 1: Healthcare evacuation triage priorities
|
Category |
Reverse Triage – Evacuation Priority | Descriptor | Priority for Onward Transfer |
|
Independent | EP1 These patients require minimal assistance and can be moved FIRST. Patients are ambulatory, and 1 member of staff can safely lead several patients to a temporary/shelter location for secondary triage | Patient can get out of bed and dress in adequate clothing with no or minimal assistance AND mobilize independently, whether walking or by wheelchair, at the same pace and for the same distance as a member of staff. | P3 These patients can safely be moved LAST from the temporary/ shelter location to another healthcare facility/reception centre or be discharged home. |
|
Dependent |
EP2 These patients require some assistance and should be moved SECOND in priority. Patients may require wheelchairs, assistance in walking or be bed bound but require 1-2 members of staff to aid transportation | Examples might include: a. patient can only be moved on his/her bed b. patient is connected to 1 piece of apparatus (eg drainage bag) c. patient must be moved in a wheelchair by another person d. patient requires more than minimal assistance or is unwilling to be dressed in adequate clothing requiring therefore 1 or more persons to assist e. patient cannot be left without supervision f. patient can walk unaided for less than 5 metres |
P2 These patients will be moved SECOND in priority as transfers to another hospital |
|
Very dependent |
EP3 These patients require maximum assistance to move. In an evacuation, these patients move LAST. These patients may require 2-4 members of staff to evacuate (eg bedbound attached to equipment or on-going high care needs) | Examples might include: a. patient is on assisted ventilation b. patient requires the assistance of 2 or more staff to effect evacuation c. patient cannot be disconnected from 1 or more pieces of apparatus for more than 60 seconds d. patient is connected to life support machinery e. patient is unconscious and/or in life threatened state f. patient requires more than 7 minutes to be disconnected from 1 piece of equipment g. patient is undergoing surgery h. patient has undergone major surgery under general anaesthetic i. patient can only be moved on his/ her bed AND requires 2 or more staff to effect evacuation j. patient is in critical condition/attached to more than 1 piece of apparatus k. patient requires one-to-one supervision |
P1 These patients require maximum support to sustain life. These patients move FIRST once stable from temporary/ shelter location to another hospital. |
Publications reference: B1951

