Foreword
In 2020, the NHS became the first healthcare system in the world to commit to becoming net zero.
This commitment was made in response to the evidence that climate change is no longer a distant threat but is already affecting the health and wellbeing of patients and communities across the country.
The benefits of taking action not only reduce the future impacts of climate change, but also deliver more immediate benefits for health.
Such action sits alongside the urgent need to adapt the NHS to the impacts of climate change, which will be felt hardest by the most vulnerable in our society, and will place significant strain on NHS infrastructure, staff and finances.
Healthcare in England is estimated to contribute between 4% and 5% of national emissions, and around 40% of all emissions generated by the public sector.
Not only does the NHS have a clear responsibility to minimise its environmental impact, building a more sustainable NHS offers a unique opportunity to deliver better patient care while minimising cost and impact on future services.
NHS England committed to regular reviews of progress, and this report is the first assessment.
To support this work, the NHS Net Zero Expert Panel – comprising global leaders and specialists in environmental sustainability, healthcare and carbon analytics – was convened to provide guidance on the next stages of this critical journey.
Despite the challenges over recent years, NHS staff have demonstrated extraordinary dedication. They have embraced sustainability principles, implemented impactful solutions and driven change.
Thanks to their efforts, NHS Carbon Footprint emissions have already decreased by 14% since the strategy to deliver a net zero NHS was published, and over 68% since 1990 – an impressive achievement given the context, and a reflection of their commitment.
Fit for the Future: 10 Year Health Plan for England sets out a clear and ambitious pathway. National demographic changes and an evolving burden of disease will increase demand on the NHS.
These challenges will be compounded by the impacts of climate change and will include more frequent extreme weather events and an increased prevalence of vector-borne diseases.
The NHS remains on track to achieve its interim target of an 80% reduction in direct emissions by 2032.
We recognise there is much more work to do, but are confident recent investments in solar power, battery storage, energy efficiency and charging infrastructure will further reduce emissions while delivering substantial financial savings.
However, the NHS cannot achieve net zero in isolation.
Decarbonisation of the electricity grid, acceleration of low-carbon heating options, wider electric vehicle infrastructure and more sustainable production of medicines are all essential.
We expect that the Greener NHS team will continue to refine data, modelling and analytical services to monitor and report the NHS carbon footprint with increasing precision, working with partners effectively to ensure interventions will enhance resilience, reduce costs and improve patient care.
We extend our sincere thanks to all NHS staff working towards a greener NHS for their continued commitment to this shared ambition.
Together we are building a healthier, more sustainable future for patients, communities and generations to come.
NHS Net Zero expert panel
Professor Mike Davies, Institute for Environmental Design and Engineering, University College London
Professor Matthew Eckelman, Department of Civil and Environmental Engineering, Northeastern University
Professor Piers Forster, Member of the Climate Change Committee, Director of the Priestley Centre for Climate Futures, University of Leeds
Professor Kamila Hawthorne, Chair, Royal College of General Practitioners
Professor Victoria Tzortziou-Brown, RCGP Vice Chair External Affairs and RCGP Chair-elect and Professor in Primary Healthcare and Health Policy, QMUL
Chris Naylor, Senior Fellow, The King’s Fund
Zoë Abrams, Director of Communications and Engagement, The King’s Fund
Dr Josephine Sauvage, Chief Medical Officer, North Central London Integrated Care Board
Dr Richard Smith, Chair, UK Health Alliance on Climate Change
Professor Nick Watts, Director, Centre for Sustainable Medicine, National University of Singapore
Introduction
Climate change poses a major risk to health and wellbeing. The impacts on health can be seen across the UK but are particularly harmful for those who are at greatest risk of poor health. Alongside heat-related mortalities, 38,000 deaths a year are attributable to poor air pollution, and there is an increase in the number of new vector-borne diseases in the UK.
Between 2020 and 2024 in England, the UK Health Security Agency (UKHSA) estimated there were a total of 10,781 heat-associated deaths as a direct consequence of heatwaves.
Projections suggest heat related deaths are set to rise to around 11,000 per year by the 2050s without adaptation and mitigation efforts. UKHSA estimates that currently heat-related mortality in England costs £6.8 billion annually, and is likely to increase to £14.7 billion per year by the 2050s.
In response to the growing threat of climate change to the health service and public health, in 2020 the NHS became the world’s first health system to commit to reaching net zero and take action to reduce the future impacts of climate change. The Delivering a net zero NHS strategy sets 2 targets against a 1990 baseline:
- Net zero by 2040 for the emissions the NHS controls directly (the NHS Carbon Footprint), with an 80% reduction by 2028 to 2032.
- Net zero by 2045 for the emissions the NHS can influence (the NHS Carbon Footprint Plus), with an ambition to reach an 80% reduction by 2036 to 2039.
Since the Delivering a net zero NHS strategy was published, the UK has faced 2 of the warmest years on record. Rapidly rising global temperatures are now 1.1°C above pre-industrial levels. These are projected to exceed 1.5°C, the temperature at which scientists warn there will be irreversible environmental damage, undermining long-term resilience.
In addition to the detrimental impact on health outcomes, climate change poses a significant service delivery and financial threat to the NHS, impacting both infrastructure and services for patients. As the number and intensity of flooding incidents and heatwaves increase, interruption to critical NHS services, highlighting the necessity of adaptation alongside mitigation efforts.
In the 5 years the NHS’s commitment to deliver a net zero health service has been strengthened by national and international action:
- The Health and Care Act 2022 introduced new duties for trusts and integrated care boards (ICBs) to consider climate change in their operations, making the NHS the first healthcare system to embed net zero in legislation.
- Lord Darzi’s independent investigation of the NHS in England reinforced the benefits of tackling climate change, stating that ‘there is no trade-off between climate responsibilities and reducing waiting lists. Indeed, often health and climate are mutually reinforcing goals’.
- All trusts and ICBs, encompassing more than 1,000 hospitals and healthcare facilities, now have a green plan – a local strategy for reaching net zero, and are required to provide annual updates on progress to their board.
- Following in the footsteps of the NHS, over 40 countries have set their own net zero targets for their healthcare systems and more than 90 countries around the world have committed to deliver low carbon, sustainable health systems, strengthening the resolve to reduce emissions and improve global supply chain resilience.
The 10 Year Health Plan sets out how the NHS must change to create a modern health service, designed to meet the needs of our changing population, through 3 shifts from: hospital to community; analogue to digital; and sickness to prevention.
The plan also reinforced the government’s commitment to a net zero NHS, stating: we will prioritise the NHS’s existing commitments set out in Delivering a Net Zero Health Service – including achieving net zero by 2040 for the emissions the NHS controls and by 2045 for the emissions it can influence.
This report provides an overview of progress over the last 5 years and an updated baseline for emissions based on improved data and methodological approaches, and considers next steps required to deliver a net zero NHS.
The progress towards net zero, as this report details, clearly demonstrates the ways in which the NHS is already supporting the government’s 3 priorities through initiatives that save money, improve health, drive growth and build a more sustainable healthcare service.
Methodology
In 2020, the NHS published the world’s first comprehensive healthcare system carbon footprint analysis. The work, developed with a team of academics and published in the Lancet Planetary Health journal, found that the NHS was responsible for around 4% to 5% of the country’s emissions.
The approach has since been adopted by other healthcare systems around the world and helps support healthcare professionals in understanding where they can make most impact.
Distributed across over 13,500 acute care, mental health, ambulance, community services and general practice buildings, employing over 1.5 million staff and delivering 1.7 million patient interactions everyday – carbon footprinting the NHS in England is a complex task.
The Greener NHS team has continued to improve its modelling approach by incorporating new and more granular NHS-specific data, improving data quality and availability, and using the best available evidence to ensure estimates of NHS emissions remain robust.
This has allowed a consistent methodology to be retrospectively applied across all years and previously published estimates to be improved and updated.
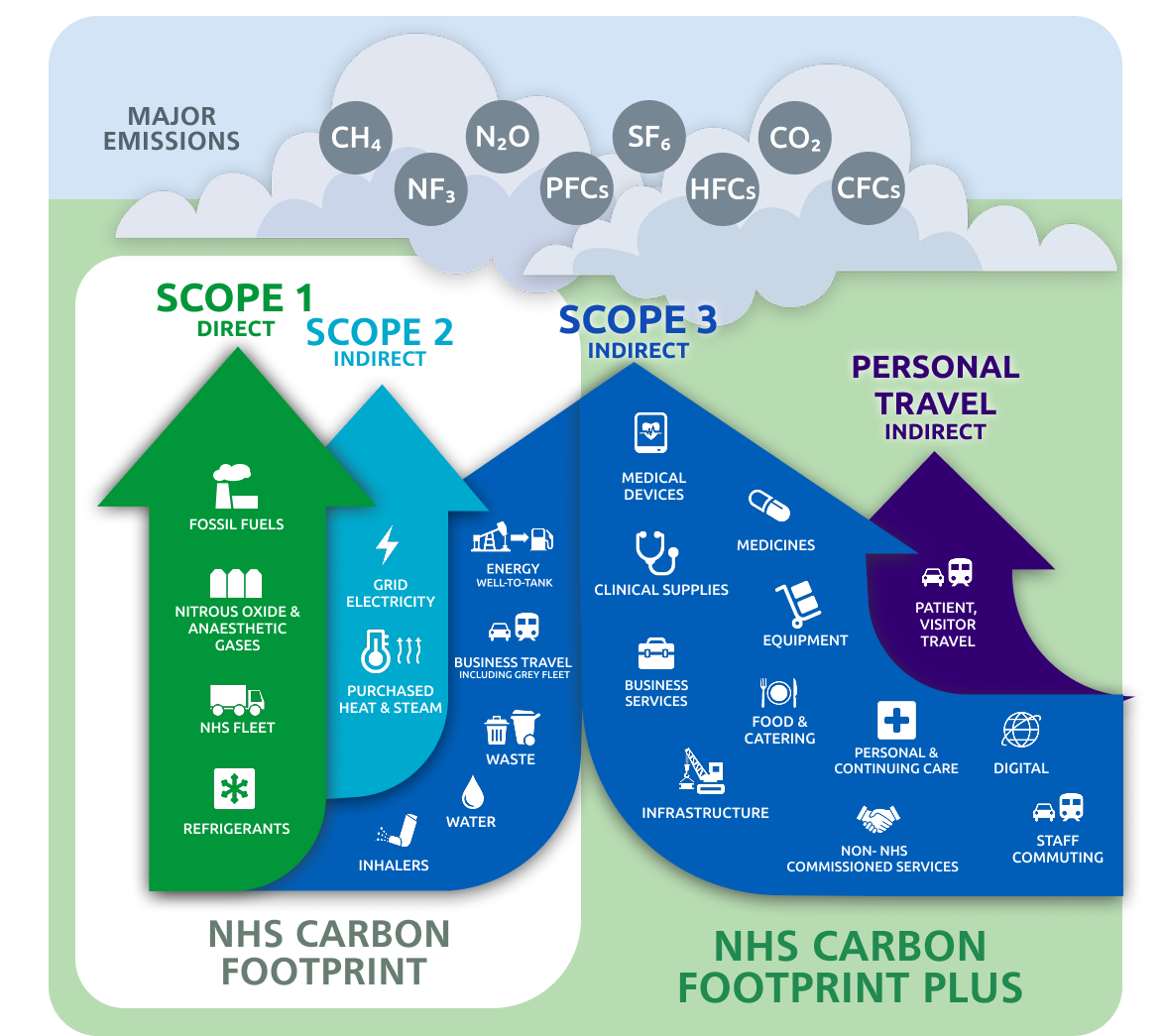
Figures 1 and 2 give a breakdown of emissions, representing an improved understanding of the emissions’ sources that were published in 2020 and a more granular breakdown. The NHS Carbon Footprint Plus encompasses all emissions associated with NHS activity, while the NHS Carbon Footprint is a subset that includes the NHS’s direct emissions (GHG scope 1, 2 and a subset of scope 3).
Within the NHS Carbon Footprint, 66% of emissions are from estates (buildings’ energy, waste, water and refrigerants), 14% from transport (fleet and business travel), and 20% from medicines (inhalers and anaesthetics gases).
See Annex 1 for an explanation of Greenhouse Gas Protocol scopes.
Notable methodological improvements include:
- the addition of refrigerant emissions
- estimates of waste treatment and fleet emissions are now based on NHS-specific data
- supply chain emissions are now based on financial data from individual NHS organisations; and new emissions categories have been identified
Overall, this improved understanding of NHS emissions will help to further prioritise and track actions nationally and locally. A comprehensive overview of the updated methodology has been published alongside this report.
Figure 1: a breakdown of emissions by proportion of the NHS Carbon Footprint Plus, represented as a pie chart
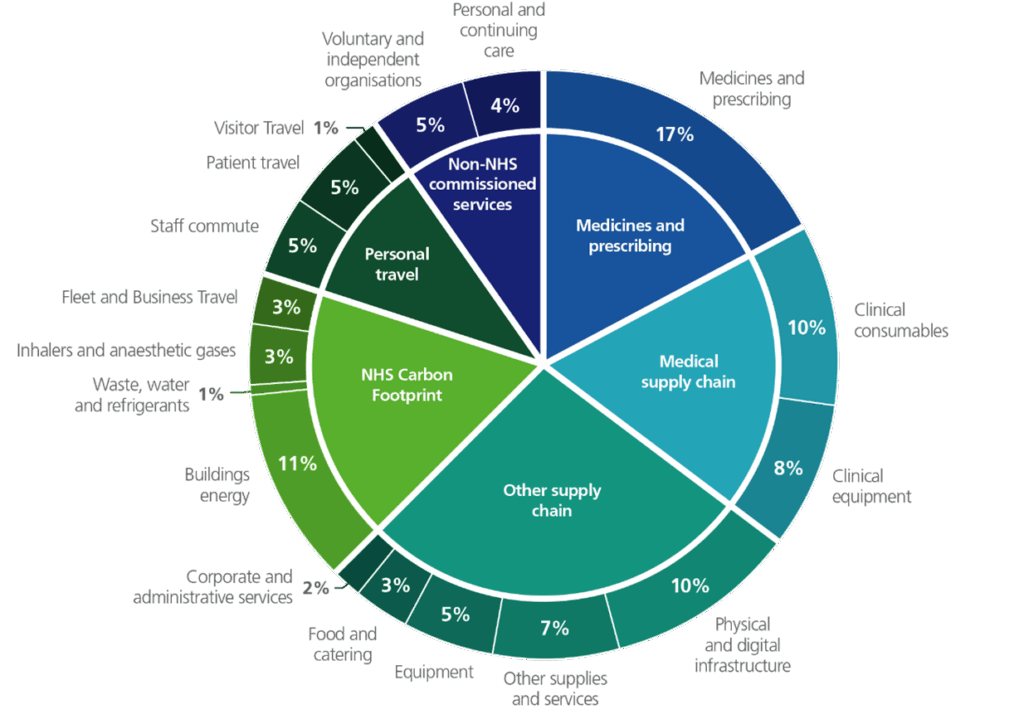
Figure 2: a breakdown of emissions by proportion of the NHS Carbon Footprint Plus, represented as a table
| Group | Emissions category | GHG emissions as % of CF+ |
|---|---|---|
| Medicines and prescribing | Medicines and prescribing | 17% |
| Medical supply chain | Clinical consumables | 10% |
| Clinical equipment | 8% | |
| Other supply chain | Physical and digital infrastructure | 10% |
| Other supplies and services | 7% | |
| Equipment | 5% | |
| Food and catering | 3% | |
| Corporate and administrative services | 2% | |
NHS carbon footprint | Buildings energy | 11% |
| Waste, water and refrigerants | 1% | |
| Inhalers and anaesthetic gases | 3% | |
| Fleet and business travel | 3% | |
| Personal travel | Staff commute | 5% |
| Patient travel | 5% | |
| Visitor travel | 1% | |
| Non-NHS commissioned services | Voluntary and independent organisations | 5% |
| Personal and continuing care | 4% |
Overall progress
Applying our improved footprinting methodology to carbon emissions’ calculations from the past 5 years, we can see that for the NHS Carbon Footprint, emissions in 2024/25 are estimated to be 4.7 MtCO2e.
Compared with a revised estimate of 14.5 MtCO2e for 1990 emissions, this represents a total reduction of 68% and means the NHS is on track to meet its interim target by 2032.
This follows a reduction of 14% in the 5 years since the publication of the NHS’s net zero strategy – equivalent to 1 million people flying from London to New York.
Figure 3: (table) annual total NHS Carbon Footprint and Carbon Footprint Plus (MtCO2e) for 2019/20 to 2024/25, updating figures published previously to be consistent with improved data and methodology. Please note the figures have been rounded to one decimal place
| Figure 3 | 2019/20 | 2020/21 | 2021/22 | 2022/23 | 2023/24 | 2024/25 |
| Total NHS Carbon Footprint (MtCO2e) | 5.5 | 5.2 | 5.3 | 5.0 | 4.8 | 4.7 |
| Which consists of: | ||||||
| Buildings energy, waste, water and refrigerants | 3.5 | 3.3 | 3.3 | 3.2 | 3.2 | 3.1 |
| Fleet and business travel |
0.7 |
0.7 |
0.7 |
0.6 | 0.7 | 0.7 |
| Inhalers and anaesthetics gases | 1.4 | 1.2 | 1.2 | 1.1 | 1.0 | 0.9 |
| The NHS Carbon Footprint is encompassed within the NHS Carbon Footprint Plus: | ||||||
| Total Carbon Footprint Plus (MtCO2e) | 27.3 | 30.5 | 29.9 | 27.5 | 26.8 | 27.3 |
Meeting the 80% reduction target in NHS Carbon Footprint emissions would require emissions to fall to 2.9 MtCO2e by 2032, a reduction of 1800 ktCO2e (38%) over the next 8 years, or an average of 225 ktCO2e per year. While this will be challenging, the actions set out in this report and the projected emissions reductions associated with them demonstrate this is achievable.
Key actions will include:
- improving respiratory care and introducing inhaler propellants with lower global warming potential
- supporting the government to make Britain a clean energy superpower through the delivery of a £100 million Great British Energy and NHS renewable energy programme
- the increased roll-out of zero emission vehicles in the NHS fleet
- the adoption of low-carbon heating solutions and energy efficiency measures across the NHS estate
This will be supported through the Government’s clean energy mission that will seek to decarbonise the electricity grid.
We have made progress in understanding our NHS Carbon Footprint Plus emissions. NHS Carbon Footprint Plus emissions increased in 2020/21 and 2021/22, driven by the NHS response to the COVID-19 pandemic, but returned to pre-COVID levels in 2023/24 and 2024/25.
Overall, in the last 5 years the NHS Carbon Footprint Plus has reduced by 15% per real pound of the NHS budget, and by 7% per finished admission episode (FAE), which suggests the NHS and its suppliers are making progress. As the Net Zero Supplier Roadmap is implemented, a full assessment of progress against targets for the NHS Carbon Footprint Plus will be made in future years.
The updated overview of emissions demonstrates that the NHS’s actions to improve patient care and deliver financial savings, while reducing emissions, have been successful. A detailed breakdown follows, outlining progress and next steps.
Medicines
Emissions associated with medicines include direct emissions from inhalers and anaesthetic gases, and indirect emissions from medicines manufacture and supply.
Emissions from inhalers and anaesthetic gases, including nitrous oxide, are responsible for 20% of the NHS Carbon Footprint.
The emissions from the manufacture and supply of all other medicines and prescribing contribute 17% of the NHS Carbon Footprint Plus (4.7 MtCO2e).
Emissions from medicines are encompassed within other areas of the NHS Carbon Footprint Plus, such as those used within healthcare commissioned outside the NHS. The NHS will prioritise further improving its approach to calculating medicines emissions in the coming years.
Progress
Working with NHS staff, royal colleges and industry, major progress has been made since 2020 to reduce NHS Carbon Footprint medicines’ emissions. Overall, the total emissions from inhalers, nitrous oxide and volatile anaesthetics have reduced by 470 ktCO2e or 33% since 2019/20. Actions taken include:
- working with the Royal College of Anaesthetists and Association of Anaesthetists to decommission desflurane in favour of safe and clinically appropriate alternatives has delivered a 41 ktCO2e (98%) reduction in desflurane emissions
- improving respiratory care and optimising the use of inhalers, which is supporting patients to better manage their respiratory conditions and reducing direct emissions from inhalers
- emissions have fallen by over 340 ktCO2e (33%) since 2019/20
- progress is expected to continue following the recent publication of updated asthma clinical guidelines which further support better outcomes for asthma patients and a lower environmental impact
- accelerating efforts to reduce nitrous oxide waste through leaner supply and stock management, with emissions reductions of over 80 ktCO2e resulting in £2.3 million in avoided costs per annum compared with 2019/20
In addition, the NHS has taken action to reduce polypharmacy and overprescribing through the recommendations of the National Overprescribing Review Report (2021).
Next steps
- Work to reduce nitrous oxide waste continues with £600,000 invested during 2025, contributing to a total of £1.5 million since 2023. This investment and widespread implementation to reduce waste could save up to £4.5 million per year, building on the existing £2.3 million savings to date.
- Efforts will continue to promote best practice in respiratory care, supporting the use of clinically appropriate low-carbon inhalers, when supported by individual patient choice. The NHS will collaborate with inhaler manufacturers to foster innovation of the next generation propellants for metered-dose inhalers, ensuring availability for patients who need them, while ensuring supply resilience and best value for the taxpayer.
- The NHS will continue to implement the Net Zero Supplier Roadmap milestones proportionately within national medicines frameworks. This includes requirements for suppliers to publicly report targets, emissions and have a plan in place to reduce them for relevant Scope 1, 2 and 3 emissions from 2027, and the considered introduction of product-level requirements from 2028. The approach will be underpinned by ongoing collaboration with our supply chain partners, recognising and supporting the leadership already demonstrated by medicines suppliers. This continued partnership will aim to drive meaningful progress towards a lower-carbon medicines supply chain while maintaining patient safety and access.
This continued collaboration with the pharmaceutical industry will include work with the Office for Life Sciences, manufacturers and the British Standards Institution to facilitate the development of product category rules for Medicines Life Cycle Assessments, to better understand the footprint of individual products.
The NHS will continue to access and align decarbonisation opportunities with best practice in prescribing, deprescribing and medicines optimisation to improve patient outcomes, while reducing waste and delivering the best value for patients.
In collaboration with clinical teams, system partners and industry, the NHS will promote the use of low-carbon alternatives where clinically appropriate, and will explore how climate change considerations could be included in the Single National Formulary as announced in the 10 Year Health Plan.
Travel and transport
The NHS fleet is the second largest fleet in the country, consisting of over 20,000 vehicles travelling over 460 million miles every year. In 2019/20 emissions from travel and transport were calculated at approximately 655 ktCO2e.
In 2024/25 emissions were estimated to be around 700 ktCO2e or 14% of the NHS Carbon Footprint. 140 ktCO2e of these emissions are associated with the ambulance fleet, 30 ktCO2e with NHS owned and leased fleet, and 520 ktCO2e with other transport and transport services.
In October 2023, the NHS Net Zero Travel and Transport Strategy was published setting out a roadmap to decarbonise travel and transport, with a clear vision of achieving a zero-emission fleet by 2040. Doing so is expected to deliver annual operational savings of £59 million and over £270 million a year in wider health and societal benefits.
As well as the expected direct cost savings from electrification of travel and transport, there are health benefits associated with reduced air pollution and increased physical activity through active travel.
The Royal College of Physicians warns that air pollution affects almost every organ in the human body, with an economic cost of £27 billion a year in the UK due to healthcare costs, productivity losses and reduced quality of life.
When wider impacts such as dementia are accounted for, evidence suggests the economic cost may be as high as £50 billion a year. Critically, alongside our net zero goals, the NHS has committed to halving its contribution to poor air quality by 2032.
Progress
- Zero-emission vehicles (ZEVs) have been widely adopted across the NHS fleet, with 1 in 10 now being ZEV, compared to 1 in 100 in 2021.
- Ambulance trusts have concluded a successful pilot of 21 zero-emission emergency vehicles, including 6 dedicated mental health response vehicles. As a result, ambulance services are increasingly adopting electric vehicles. For example, Yorkshire Ambulance Service NHS Trust has ordered 35 fully electric non-emergency Patient Transport Service vehicles that provide a full day’s operational service with 130 miles range from a single charge. In addition, 12 electric 19-tonne trucks are now in operation across the NHS.
- Drones have been piloted across the country, including in the delivery of vital chemotherapy drugs to the Isle of Wight, reducing a 4-hour journey time by road and sea to a 30-minute flight, minimising waste, treatment delays and reducing carbon emissions.
- In July 2025, the Department for Transport and the Department of Health and Social Care (DHSC) announced the NHS ChargePoint Accelerator scheme. The investment of £8 million, funded by the Office for Zero Emission Vehicles, will support the installation of on-site electric vehicle chargepoints on NHS sites. This is expected to deliver average operational savings of £5.2 million annually and £130 million over the next 25 years, and a further £96 million in wider social benefits from reduced vehicle emissions and improved air quality.
Next steps
- From 2030, all new ambulances will be zero emission. In preparation, in 2024, the NHS piloted and rolled out its first fully electric double crewed ambulance, with plans to increase the number in service to nearly 80 by the end of 2025/26.
- From 2027, all new vehicles owned or leased by the NHS will be zero emission (excluding ambulances).
- By the end of 2026, all NHS trusts and ICBs are required to develop a sustainable travel strategy.
Patient and visitor travel accounts for over 40% of total NHS transport emissions. The NHS will continue to work with local authorities and transport organisations to develop ways to accurately measure and understand travel patterns to support more inclusive and sustainable travel options for all those travelling to and from NHS sites.
The NHS will also continue working with government and other partners to identify funding routes to support providers to maintain their momentum in the transition of the NHS fleet.
Case study: The Christie at Home team has introduced a fully electric fleet
The Christie, a specialist cancer centre providing cancer treatments to patients in the comfort of their own home, now operates with a fully electric fleet of vehicles for nurses to deliver the service that covers more than 85,000 miles a year.
The new fleet is made up of 7 electric cars, each with a daily range of around 240 miles – more than enough for the service’s busiest travel days, which rarely exceed 150 miles.
It is estimated that by switching from petrol to electric, the Christie at Home team will save over 14 tonnes of carbon per year – equivalent to the annual emissions of around 4 average UK households.
Alongside reducing the trust’s contribution to air pollution, the change will save The Christie more than £20,000 annually on vehicle costs.
Estates and facilities
The NHS is the UK’s largest single public energy user, with an annual energy bill that has nearly doubled since 2019 to over £1.4 billion for trusts alone, supplying energy to over 13,500 buildings spanning 27 million m2.
Overall estates emissions have reduced by 10% since 2019/20. Across the secondary care estate energy consumption has reduced, with emissions associated with the consumption of grid electricity dropping by over 220 ktCO2e (21%).
Emissions associated with electricity will continue to fall as the government delivers against its clean energy mission and the national grid decarbonises. The NHS will continue to deliver on-site renewable energy projects to bring down electricity costs, improve energy efficiency and resilience, and increase the potential for lower cost low carbon heating in future years.
However, emissions associated with the use of gas (primarily for heating) accounted for around 40% of the NHS Carbon Footprint in 2024/25 and have reduced by just 1% since 2019/20.
Progress
NHS trusts have leveraged low-carbon investment opportunities to reduce carbon emissions across their estates, delivering substantial long-term savings and improvements to patient care. This progress has been bolstered by the NHS Net Zero Building Standard and the Green Lease Framework.
- Since 2020, the NHS has secured over £1.4 billion in additional capital funding through the Government’s Public Sector Decarbonisation Scheme. This is funding over 100 projects which are expected to reduce energy bills, reduce emissions by over 125 ktCO2e, and provide a more comfortable environment for patients through building management systems.
- Over £135 million has been invested in energy efficiency measures, including LED lighting, solar panels, upgrades to building infrastructure and enhanced building energy management systems. Over 50% of the secondary care estate is now equipped with LED lighting, and solar generation has tripled since 2019.
- In March 2025, Great British Energy announced they would co-fund, with DHSC, a package of £100 million to install solar power and battery storage solutions to help drive down energy bills across the NHS. These projects are expected to deliver savings of around £8.6 million a year and up to £260 million over their projected lifetime.
- Since 2020/21, trust waste emissions have reduced by 32%, with clinical waste volumes declining for 3 consecutive years – avoiding £22 million in costs and reducing landfill disposal to just 2%.
Case study: Harnessing solar power to save millions
Hull University Teaching Hospitals NHS Trust set itself an ambitious target to be net zero by 2030, supporting the wider NHS’s plan to become the world’s first carbon net zero national health service.
The trust’s 11,000-panel solar farm – funded through a government grant of £4.2 million – means that during the summer the organisation saves around £230,000 a month in energy bills.
The panels generate more than 4.2 million kilowatt hours every 12 months, equivalent to powering around 1,400 UK households a year.
The trust recently received a grant of over £6 million, as part of the first major project for Great British Energy, and the additional panels are predicted to save the trust up to £9.5 million over their lifetime.
Next steps
- The NHS will continue to improve energy resilience and enhanced metering across the estate and seek to remove all oil-led primary heating systems by 2028. This will be supported by all trusts either having or being in the process of developing and updating heat decarbonisation plans ready to transition away from fossil fuel systems to low-carbon alternatives.
- All new buildings within scope will design and deliver health facilities in compliance with the NHS Net Zero Building Standard.
- The NHS will identify opportunities to both mitigate and adapt to the impacts of climate change the estate is already facing.
- Where onsite renewable energy is not viable, the NHS will explore alternative financing opportunities with the Department for Energy Security and Net Zero and the National Infrastructure and Service Transformation Authority and assess the potential for Power Purchase Agreements through the central NHS energy buying partnership with the Crown Commercial Service.
Heating remains one of the largest sources of emissions across the NHS estate. Achieving the scale of change required will depend on sustained investment, access to technical expertise and long-term heat and decarbonisation planning.
Following the Public Sector Decarbonisation Scheme, the NHS will continue working with government and partners to identify investment to maintain momentum in decarbonising estates, including for onsite renewable energy generation that can deliver cost savings.
As well as lowering costs and reducing emissions, work across the NHS estate will support compliance with the UK Emissions Trading Scheme and seek to minimise the risk of financial penalties for NHS organisations.
Food
Nutritious diets can improve clinical outcomes for hospitalised patients, reducing complications, length of stay and readmissions. Catering staff across the NHS are working to improve the health of patients while reducing food-related emissions and minimising waste.
Emissions associated with food and catering services are estimated to be around 3% of the total NHS Carbon Footprint Plus.
Progress
- National Standards for Healthcare Food and Drink were published to ensure that healthy, nutritious and sustainable food and drink options are readily available and accessible.
- The NHS Recipe Bank has allowed chefs and catering managers to access over 200 lower-carbon recipes for easy menu design and dish swaps.
Next steps
- The NHS will publish and implement guidance on reducing food waste. This will include using electronic meal ordering and improving crockery which has been shown to reduce food waste by 20% and 15% respectively.
- The NHS will support trusts to identify food and food waste carbon hotspots so they can take action to develop healthy, nutritious, low carbon meals.
Case study: Low-carbon menus into patient and retail catering
The catering team at University Hospitals of Morecambe Bay NHS Foundation Trust – which operates 3 acute hospitals in Lancashire and South Cumbria – developed a new patient and retail menu.
The team uses low carbon recipes from the NHS Great Food Good Health Food Platform in addition to dishes from their existing menu.
The project reduced carbon emissions by 18% and reduced costs by 10% while continuing to offer patients a balanced choice of meat, fish and plant-based choices.
Delivering low carbon healthcare
Everyone involved in the design and delivery of clinical care has a part to play in transforming their practices towards low carbon, high quality, efficient, equitable and cost-effective healthcare delivery.
Progress
- The Delivering Low Carbon Care for a Healthier Future framework will provide guiding principles for all NHS staff involved in service design to support inclusive care design and delivery. This aligns with our net zero commitments and prioritises patient health, and highlights carbon and cost savings.
- In partnership with the Greener NHS team, the Getting It Right First Time (GIRFT) programme has developed ‘GIRFT greener pathways’, a cross-specialty approach to decarbonising clinical care featuring high impact climate recommendations. A guide to decarbonising the bladder cancer pathway has been published, which estimates that implementation of the 12 recommendations would reduce carbon emissions by 2470 tCO2e, reduce costs, increase same-day diagnosis rates and mean patients spend less time in hospital.
- The Design for Life roadmap is currently being implemented in partnership with DHSC, to transition from all avoidable single-use medical technology products to a functioning circular system by 2045. This will be achieved by identifying opportunities to maximise reuse, recycling, re-manufacture, economic growth and resilience, and by working with staff to support behaviour change across the health and care system. A recent series of pilots with 6 trusts sought to explore the impact and enablers of large-scale transitions to reusable medical technology.
Next steps
The NHS has now demonstrated it can provide low carbon high quality care that delivers cost savings. Over the next 5 years, our mission is to embed this further, reducing variation and achieving carbon and cost savings at scale. To achieve this:
- net zero principles, in line with the NHS climate duties, will be considered in pathway design and service change programmes at trust and ICB level, adopting the South East Clinical Senate approach where environmental sustainability is embedded at the outset of service redesigns as a guiding principle
- all new and refreshed GIRFT reports will consider environmental sustainability from conception
- more greener pathways guides are being developed, including on elective hip, elective knee and skin cancer surgery, and these will be implemented across a range of clinical specialties
- GIRFT will support the ongoing delivery of low carbon care through its national network of clinically led programmes
- in partnership with NHS Supply Chain, Design for Life, royal colleges, GIRFT and other representatives of clinical professions, the NHS will reduce the use of products, clinical interventions and infection prevention and control practices that evidence has shown are clinically unnecessary or outdated, carry a high cost or carbon burden on the NHS, or where circular solutions are ready for adoption across the system
- this includes a commitment to reduce single-use glove and gown use by 25% by 2030
- to prepare for a circular future, the NHS will work with the Design for Life programme to survey the existing decontamination infrastructure available to the NHS to support reusable products and develop a strategy for maximising this capacity
Research and innovation
Research and innovation are key enablers to support the transition towards a more sustainable healthcare system and are driving better and more efficient care for patients and delivering value for the taxpayer.
Since 2021 the Small Business Research Initiative Healthcare programme, hosted by the Accelerated Access Collaborative, in partnership with the Greener NHS team and the Health Innovation Network, has awarded over £10 million to innovation projects that benefit patients and accelerate a more sustainable NHS.
These include pioneering circular economy and decontamination initiatives to allow reuse of devices; development of virtual care models; specialist surgical textiles designed for reuse; and drones to transport medical packages.
Since 2021, the Medical Research Council, the National Institute for Health and Care Research and UK Research and Innovation have invested over £50 million in research funding on decarbonisation and adaptation of healthcare.
This includes £25 million of research funding over a 5-year period for decarbonising health and social care, and investment of £12 million into 2 transdisciplinary research hubs that will focus on circularity and delivery of low carbon care.
Case study: Reducing plastic waste and building a circular economy
Currently 99% of the clinical and laboratory plastic waste worldwide is sent to landfill or incinerated, and less than 1% of lab-grade consumables are made from recycled materials.
Supported by the Small Business Research Initiative’s competition 24, LabCycle has developed an innovative solution that enables a circular economy model for clinical and research plastic waste.
The system allows single-use plastics, such as syringes and specimen pots, to be decontaminated and recycled into high-quality lab consumables, including test tubes and petri dishes.
This solution reduces carbon emissions by approximately 90% compared to incineration. Pilot projects across a number of NHS sites have yielded positive results with carbon savings from Somerset NHS Foundation Trust estimated to be 1929kgCO₂e annually.
Workforce
Staff continue to be supportive of the NHS taking action on net zero with 9 in 10 supporting this ambition. Across the NHS small changes in behaviour have unlocked improved patient outcomes, efficiencies, cost savings and greater staff retention. The ambition is to now embed behaviour change at all levels across the workforce to deliver these benefits.
Progress
- Collaboration with royal colleges, regulators, clinical associations and societies has led to a range of specialty specific guidance being developed for the clinical workforce. This includes:
- the Royal College of General Practitioners’ Net Zero Hub
- the Royal College of Emergency Medicine’s GreenED framework
- Green Impact – Dentistry Toolkit
- the UK Health Alliance on Climate Change’s Green Surgery Report
- the Royal College of Psychiatrists’ Net Zero resources and guidance
- this work offers guidance to clinicians and staff on how to improve patient health, deliver financial savings and reduce emissions
- Numerous specialty specific sustainability networks have been set up, including the Nursing and Midwifery Sustainability Network, to share best practice net zero initiatives.
- In the last 5 years over 100,000 staff in England have completed training on sustainable healthcare, with several clinical regulators integrating sustainability into professional standards and training curricula.
Next steps
- As part of their green plans, all trusts and ICBs should have an established clinical lead with oversight of net zero clinical transformation as well as formal links into board level leadership and governance.
- As part of the Design for Life programme, a training and skills framework and a behaviour change plan will be developed, which will support staff to deliver the financial, carbon, resilience and patient safety opportunities that circular and low carbon products provide.
- The NHS will continue to support staff to develop their skills and knowledge to adopt more sustainable practices to unlock improved patient outcomes and cost savings.
Supply chain and procurement
A large proportion of the NHS Carbon Footprint Plus is associated with the supplies and services purchased by NHS organisations, with over 600,000 products purchased from 80,000 national and global suppliers.
Supply chain emissions from ‘medical’ and ‘other’ supply chain are estimated to be 12.4 MtCO2e in 2024/25. This includes MedTech products that are encompassed in a range of categories including ‘clinical equipment’, ‘clinical consumables’ and ‘other equipment’.
Improvements to the methodological approach for calculating supply chain emissions, along with greater engagement with suppliers, mean NHS organisations now have a better understanding of supply chain emissions, categories and sources.
The improvements will enable better targeting of action and development of policy. However, the methodology’s reliance on economic (spend-based) emissions’ factors currently limits the NHS’s ability to measure progress.
Overall, estimates indicate that supply chain emissions have fallen since the COVID-19 pandemic, suggesting the NHS and its suppliers are making progress, but a fuller assessment will be made in future years.
Progress
The Net Zero Supplier Roadmap, published in 2021, set out clear steps to help suppliers align with the NHS’s ambition to decarbonise its supply chain, up until 2030. The initial milestones have been implemented, providing useful proxy indicators for progress:
- From April 2022, the NHS adopted a 10% weighting for net zero and social value across all new NHS procurements. From April 2023, implementation of the Cabinet Office Procurement Policy Note 006 began, requiring suppliers for all new contracts above £5 million per annum to publish a Carbon Reduction Plan (CRP). From April 2024, the NHS proportionately extended this requirement to all new procurements.
- Under the 2024 policy, almost 90% of NHS non-pay spend is in scope of CRP or net zero commitment requirements, with a near 100% pass rate for CRP requirements across NHS Supply Chain frameworks and NHS England medicines’ tenders.
- Over 2,000 suppliers have signed up to the Evergreen Sustainable Supplier Assessment, a tool for suppliers to engage with the NHS on their sustainability journey and demonstrate progress.
Healthcare supply chains are global, and action to reduce emissions and improve resilience will require global collaboration. The Greener NHS team has collaborated with health systems in countries including Ireland, Norway, Australia, Germany and France (Ministry of Health) to seek to align supplier requirements that will improve adoption, efficiency, costs and resilience globally.
In addition, the NHS is working through the Sustainable Markets Initiative, initiated by HRH The King and made up of key pharmaceutical and med-tech companies, to drive more transparent carbon footprinting in the production of medicines, alongside optimising care pathways and supply chains.
Next steps
- From 2027, the NHS will implement new, proportionate requirements for suppliers to publicly report targets, emissions, and a plan to reduce them for all their relevant Scope 1, 2 and 3 global emissions
- Some suppliers already apply environmental considerations at a product level. The NHS will continue to collaborate with suppliers, regulators and international health systems to help co-produce the approach to the 2028 product carbon footprinting requirements but will not expect life cycle assessments for every product at this stage. The focus will be proportionate and prioritised on understanding high-emission areas, particularly pharmaceuticals, medical technologies, and digital where more granular carbon insights can deliver value on the NHS’s journey to net zero. The NHS remains committed to aligning with emerging international standards and relevant government initiatives, ensuring the approach is both globally coherent and locally impactful
- The NHS will work closely with suppliers and procurement staff as it develops guidance to implement these milestones and produce the next phase of the NHS Net Zero Supplier Roadmap for 2030 onwards.
Case study: Global suppliers supporting net zero
The Evergreen Sustainable Supplier Assessment is an online tool which enables suppliers to engage with the NHS on their sustainability journey and align with the NHS net zero and sustainability ambitions, including those in the NHS Net Zero Supplier Roadmap.
The assessment, which can be completed by any supplier to the NHS in England and the devolved nations, has been submitted by over 2,000 suppliers.
Global brands and strategic healthcare suppliers including AstraZeneca, Sodexo and GSK have actively engaged with the NHS’s goals and been awarded the highest level of recognition for their sustainability efforts, including validated 2045 net zero targets for their global emissions.
Digital
The shift from analogue to digital will transform the way that care is delivered in the NHS, by increasingly putting care into the hands of patients through technology. This digital transformation will need to meet the needs of patients and users efficiently and sustainably, while ensuring IT systems are resilient to climate change risks.
Emissions associated with digital services contribute to categories throughout the NHS Carbon Footprint and NHS Carbon Footprint Plus including hardware, software and MedTech – all of which contribute to emissions associated with energy usage.
Progress
- The creation of more than 12,000 virtual ward ‘beds’ is allowing patients to get the care they need at home safely and conveniently. The NHS is increasingly introducing virtual wards to support people at the place they call home, including care homes. This is expected to deliver savings of up to 100 ktCO2
- The NHS App outpatient booking service allows patients to book outpatient appointments quickly and easily. This service could save 29 ktCO2e, 63 million sheets of A4 paper and 152 million minutes of staff time each year.
- Measures to reduce the energy consumption of idle computers have been piloted across the country, in one case saving 590 tCO2e and £440,000 annually.
Next steps
- The NHS will ensure that implementation of the 10 Year Health Plan’s digital aspirations are as environmentally sustainable, resilient and responsible as possible, supported by the launch of Greener by Design requirements for health system digitisation as part of the One Architecture approach in 2026/27, with the ambition to reach system wide implementation by 2029/30.
- The NHS will implement the Government’s sustainable AI principles to ensure NHS AI deployment meets government requirements for sustainability and environmental impact.
- In line with 2028 supplier roadmap ambitions, we will the NHS will support the continued disclosure and reduction of emissions related to NHS IT software, hosting and hardware related emissions.
Adaptation
Even as the NHS decarbonises, the impacts of climate change will continue to increase, threatening the delivery of essential NHS services and population health.
As set out in the NHS and UKHSA’s Fourth Health and Climate Adaptation Report, more frequent floods, heatwaves and worsening air pollution are already impacting the population. Without appropriate safeguards these hazards will affect staff, damage infrastructure and disrupt critical services such as water, energy and transport.
Ensuring the healthcare system is resilient to the impacts of extreme weather is essential to maintain healthcare delivery and protect NHS sites and services.
Progress
- The Third National Adaptation Programme (NAP3) sets out the key NHS actions for 2023 to 2028, including updated standards for facilities’ resilience planning.
- The Fourth Health and Climate Adaptation Report sets out the NHS’s climate resilience priorities to protect service continuity, supported by tools such as the NHS Climate Change Risk Assessment tool, which enables trusts and system leaders to identify risks to local sites and services, assess potential impacts and plan effective responses.
- The Emergency Preparedness, Resilience and Response core standards mandate robust business continuity plans across all NHS trusts for incidents such as flooding, extreme heat and severe cold.
Next steps
The NHS will build on its strong emergency preparedness by coupling acute response with longer-term strategic adaptation, recognising that evolving climate risks require proactive, system-wide action to protect health, infrastructure and services. Next steps include:
- in line with Green Plan guidance, rolling out the Climate Change Risk Assessment tool across all trusts and systems, ensuring local response plans are informed by comprehensive risk assessments of local sites and services
- conducting an emergency response exercise on adverse weather and health in every NHS region by 2030. These exercises will assess response capabilities, communication pathways and resource coordination among organisations and partners
- the NHS collaborating with its partners, including UKHSA, to raise awareness of climate impacts and responses among NHS staff
While considerable progress has been made in strengthening healthcare resilience to the growing impacts of climate change, challenges in addressing vulnerabilities, improving infrastructure, and empowering the health workforce to lead and deliver adaptation efforts remain.
Adaptation must be integrated as part of mitigation plans to maintain healthcare delivery, protect infrastructure and safeguard patients and staff during extreme weather events.
By acting now, the NHS can protect the most vulnerable, strengthen resilience and ensure the health system continues to deliver for patients.
Summary
The Delivering a Net Zero NHS Strategy set an ambition considered to be achievable but challenging. The dedication shown by NHS staff – with tangible actions highlighted throughout this progress report – confirms that the original ambitions have so far been met and the NHS is considered to be on track to meet its interim targets.
During the last 5 years, the NHS has not only seen emissions in the Carbon Footprint fall, but it has witnessed a profound energy, passion and pride from those NHS staff wanting to make a difference to this commitment.
There is also now clear evidence that taking action offers wider benefits – efficiencies have been achieved across our estate, in our fleet and in how we seek to deliver better care to our patients.
Part of this progress is in knowing where, as well as how, to take action. The ability to do this has been driven by a better understanding of where our emissions occur.
The NHS’s understanding of its carbon footprint has improved substantially over the last 5 years. The Greener NHS team will continue to improve data, refine methodology against best practice, and report appropriately through the NHS Sustainability Board, annual emissions updates and as part of future progress reports.
Through improved understanding and independent scrutiny resources can be deployed effectively and to where they can make the most difference.
The Delivering a Net Zero NHS Strategy is still considered to be the right approach to decarbonisation of the NHS. Over the next 5 years, the NHS will maintain its commitment and accelerate the momentum created.
Refreshed green plans will help staff understand where they can make a difference in their own trust or integrated care board and replicate evidence-based, best practice models of care to wider parts of the health system.
The objectives set out in this report will be underpinned and reinforced by the 10 Year Health Plan’s commitments to deliver more care out-of-hospital, expand the use of digitally enabled care where clinically appropriate, improve prevention of ill health, and reduce health inequalities.
The foundations have been set to deliver the first interim ambition for 2032. With continued support and guidance, and the acknowledgement that taking action can deliver a more sustainable health system, NHS staff can be encouraged to meet the ambitions to 2040 and 2045.
Annex 1: Greenhouse Gas Protocol scopes explained
The Greenhouse Gas Protocol is a global standard for measuring and managing greenhouse gas emissions. It defines 3 ‘scopes’ that apply to any organisation, not just the NHS.
Within the NHS:
- Scope 1 emissions come from sources that NHS organisations own or control directly, such as the burning of gas in boilers, or use of fuel in NHS vehicles.
- Scope 2 emissions are from the generation of energy used by NHS organisations – although the NHS doesn’t generate these emissions directly, it is responsible for the emissions because it consumes the energy.
- Scope 3 emissions are produced outside the NHS, through the products and services procured by the NHS.
We make a distinction between the NHS Carbon Footprint, which includes emissions under NHS direct control (scope 1, 2 and some of scope 3), and the NHS Carbon Footprint Plus, which includes all emissions the NHS has influence over (including all of the NHS Carbon Footprint plus the remaining scope 3 categories).
The Climate Change Act 2008 set national targets for the reduction of carbon emissions in England, against a 1990 baseline. Since then, the NHS has been working to deliver on these targets, most closely approximated by the NHS Carbon Footprint.
NHS Carbon Footprint
The NHS Carbon Footprint includes:
Scope 1 emissions included in the NHS Carbon Footprint:
- fossil fuel combustion
- nitrous oxide and anaesthetic gases
- the NHS vehicle fleet
- refrigerant gases
Scope 2 emissions included in the NHS Carbon Footprint:
- electricity from the national grid
- purchased heat and steam
Scope 3 emissions included in the NHS Carbon Footprint:
- the emissions produced during the extraction, refining, and transportation of fuels before they are used by the NHS
- emissions from travel by NHS staff for work purposes (including public transport and use of personal vehicles for work but not including commutes)
- emissions from treatment and disposal of waste generated by NHS operations
- emissions associated with the supply, use, and treatment of water in NHS facilities
- propellant gases that contribute to greenhouse gas emissions when released during use or disposal
- emissions associated with the manufacture of inhalers, nitrous oxide, and anaesthetic gases.
NHS Carbon Footprint Plus
The NHS Carbon Footprint Plus includes all the emissions within the NHS Carbon Footprint, plus the remaining scope 3 emissions categories. These include emissions associated with the procurement, manufacture, transportation and provision of:
- digital services
- medical devices
- clinical supplies
- medicines
- equipment
- non-NHS commissioned services
- personal and continuing care
- business services
- infrastructure
- food and catering
- staff commuting
- personal travel by patients and visitors
Figure 3: Greenhouse Gas Protocol scopes in the context of the NHS
Publication reference: PRN01951

