This resource pack includes case studies and resources to help local areas put in place priority actions over the winter months, as set out in the letter Going Further for Winter: more detail on mental health actions.
Introduction
This guidance supports local areas with the following actions:
- Strengthening ambulance response to mental health need
- Optimising flow through mental health inpatient settings
- Raising profile of all age 24/7 urgent mental health helplines
- Supporting children and young people with mental health needs in acute and paediatric settings.
Overview of winter actions for local systems
1. Strengthen ambulance response to mental health need
Actions required:
- Deploy multi-disciplinary mental health professionals to support 999 mental health demand across all ages 24/7 (either co-located or remotely from 999 call centres) over winter months.
- All integrated care services who have not yet committed funding to place mental health professionals into 999 call centres on a 24/7 basis, as part of the Long Term Plan, should do so over winter and longer term using Long Term Plan funding.
Read further guidance on strengthening ambulance response to mental health needs.
2. Optimise flow through mental health inpatient settings
Actions required:
- Launch action on the ‘Mental Health Discharge Challenge (informed by learning from the 100-day Challenge for the acute sector) and note inclusion of mental health discharges in scope of the adult social care discharge fund over the winter period.
- Review escalation protocols for admissions to acute settings, to eliminate delays to admissions caused by financial sign-off processes for out-of-area placements.
- Ensure system control centres have adequate mental health clinical input.
Read further guidance on optimising flow through mental health settings.
3. Raise the profile of 24/7 urgent mental health helplines for all ages
Actions required:
- Update all Directories of Service (DoS) in relation to mental health for 999/111 operations centres.
- Run local communications campaigns to raise the profile of 24/7 urgent mental health helplines and urgent and emergency care mental health pathways for all ages.
Read further guidance on raising the profile of mental health helplines.
4. Support children and young people with mental health needs in acute paediatric settings
Actions required:
- Encourage local systems to adopt a new integration framework for systems to support children and young people (CYP) with mental health needs within acute paediatric settings (including training resources).
- Encourage uptake of Health Education England commissioned CYP crisis telephone training to support crisis mental healthcare staff to be able to respond effectively to the needs of CYP and their parents and carers presenting in mental health crisis by telephone.
Read further guidance on supporting CYP in acute paediatric settings.
Overview of available funding
The following funding is available to support urgent and emergency care mental health pressures in 2022/23.
- £10.8 million of additional funding has been reprioritised across mental health budgets specifically to support winter pressures (already allocated to all integrated care systems).
- The use of Better Care Fund in 22/23 to support mental health discharge should be encouraged, including the additional £500 million adult social care discharge fund.
- We have allocated £150 million of capital funding to upgrade urgent and emergency mental health care pathways and are approving bids on a rapid basis to ensure as many facilities are in use as possible for winter 2022/23.
Strengthening ambulance response to mental health need
This case study shows the impact of having mental health professionals embedded in the Emergency Operations Centre (EOC). This reduces ambulance dispatch and conveyance and ensures people in mental health crisis receive the right care in their community.
The Bristol, North Somerset and South Gloucestershire (BNSSG) emergency mental health dispatch pathway – South West Ambulance Service (SWAST)
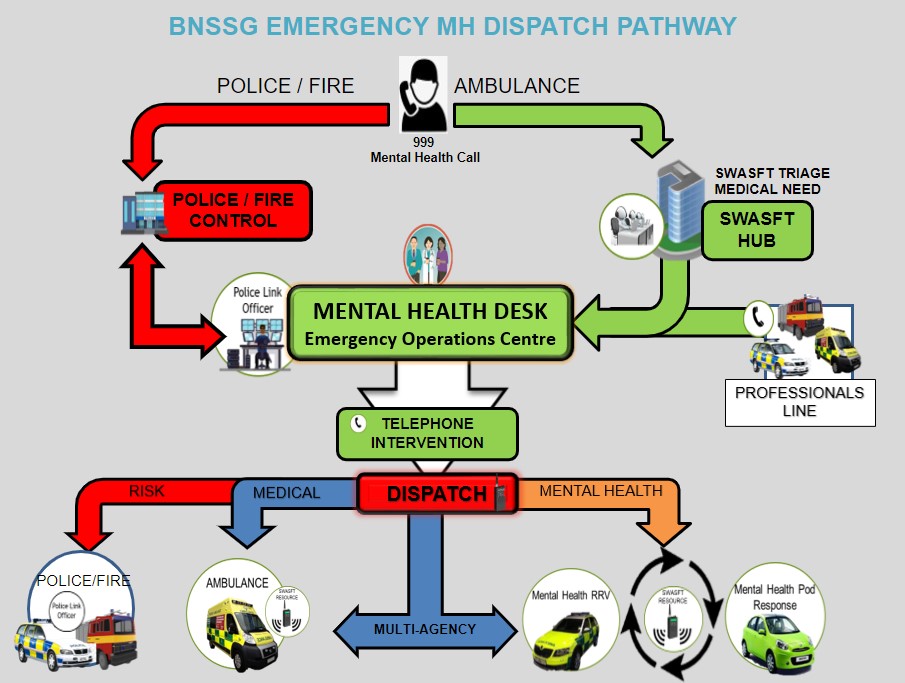
Image description:
A dispatch pathway that shows how 999 mental health calls are received and the partnership between mental health, police and ambulance to determine best response. It shows the integration into emergency operations centres between system partners.
Hear and treat results before and after the launch of mental health desk in 999 EOC
The following graph, from SWAST and the BNSSG system, shows that when there are mental health professionals working jointly with ambulance colleagues in 999, more people with mental health needs are being treated over the phone without the need for an ambulance to be dispatched.
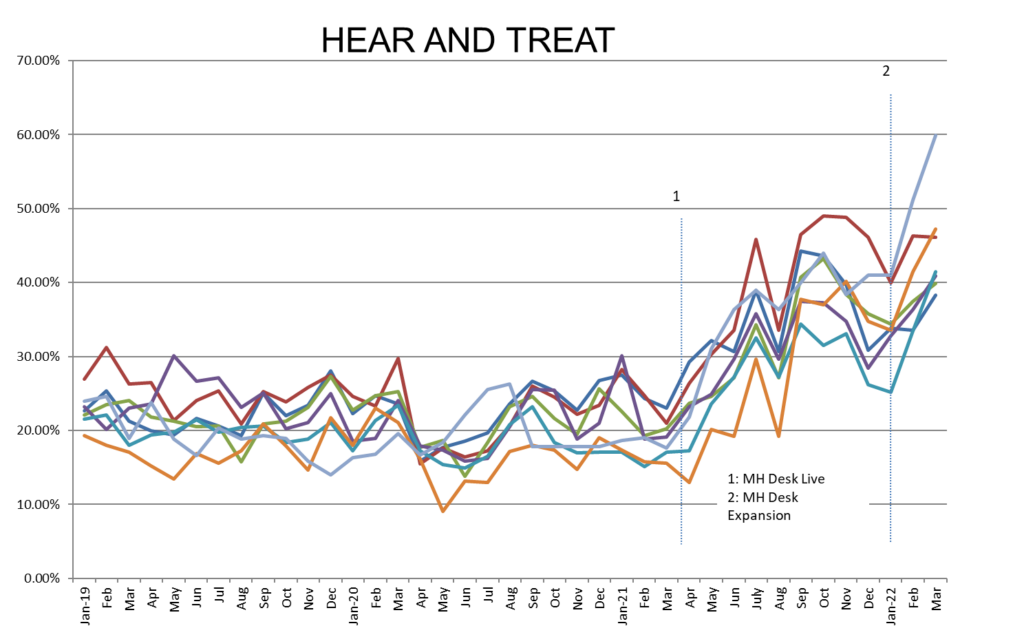
Graph description:
Each of the lines on the graph represents a different phone line that links into SWAST and BNSSG’s ambulance dispatch pathway (e.g. professionals’ line, police link officer), and from point 1 onwards (when the mental health desk went live in the EOC), the proportion of calls that could be managed over the phone increased significantly across all the different entry points into the EOC.
See and convey results before and after the launch of mental health desk in 999 EOC
The following graph, also from SWAST and BNSSG system data shows that after the introduction of mental professionals in emergency operations centres, fewer people with MH needs calling 999 are conveyed to A&E.
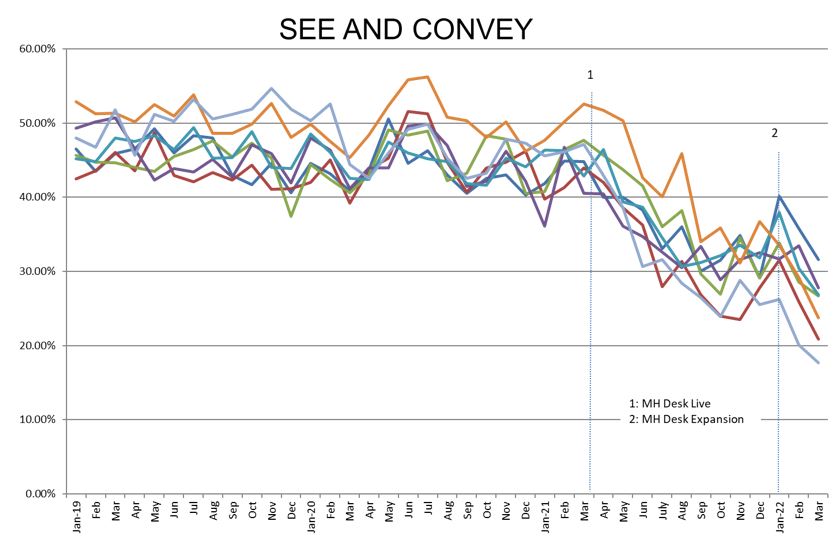
Graph description:
Each of the lines on the graph represents a different phone line that links into SWAST and BNSSG’s ambulance dispatch pathway, and the impact of the mental health desk going live is again universal across all entry points into the EOC, in terms of reducing the number of ambulance conveyances to A&E.
Potential national impact if all areas integrate mental health and ambulance services
The impact of joint ambulance and mental health services:
- Where mental health professionals from local services are embedded in 999 and providing a joint on-scene response in ambulance services, conveyance to A&E is reducing by around 30% and more people are having their needs met over the phone or conveyed to more appropriate services.
- The table below shows the potential national impact if all areas were to implement these models nationally, based on areas with these services in place.
- As part of the Long Term Plan, it is already expected that by 2023/24 all systems have funded plans for:
- Mental health professionals embedded in emergency operation centres.
- A joint mental health and ambulance on-scene response (supported by capital funding).
- A mental health training programme for ambulance staff.
Ambulance and mental health initiative incident outcome estimation
Please note: this is hypothetical data only and based on scaling up current initiatives. It covers mental health demand only, which is estimated to be around 4-5% of total incident demand for ambulance services.
| Ambulance only model | Joint ambulance and mental health model |
| 51% to ED | 20% to ED |
| 5% to non-ED | 12% to non-ED |
| 32% see and treat | 51% see and treat |
| 12.5% hear and treat | 17% hear and treat |
Additional ways systems can add mental health capacity into ambulance services over winter (while recruiting into EOC)
The following actions are recommended to support ambulance services over winter months:
- Deploying multidisciplinary mental health professionals to support 999 mental health demand across all ages (either co-located or remotely from 999 call centres) over winter months. See a list of actions for deployment below.
- Daily ambulance, crisis team and police virtual ‘huddles’ to review CAT3-5 mental health stack and jointly decide an approach, for example crisis resolution and home treatment referral, signposting to voluntary and community sector (VCS) or other community services, closing cases and so on.
- A resourced ‘professionals’ line within crisis teams to advise on 999 triage and ambulance on-scene response (including a section 136 Mental Health Act priority line).
- IIncrease local communications (among public and emergency services) to ensure people are aware of local 24/7 urgent mental health helplines, crisis alternatives and other community services.
- All areas must profile and regularly update 24/7 urgent mental health helplines and other crisis services on their local directory of service (DOS).
- Mental health, ambulance, police and other professionals to conduct joint safety planning and case reviews for frequent callers and complex patients, to better support ambulance services to safely manage risk.
- Convert existing vehicles into additional joint response vehicles, with the capability to undertake ‘hear and treat’ when not responding on scene.
Deploying multidisciplinary mental health professionals to support 999 mental health demand
Actions to ensure ambulance services deploy mental health professionals in emergency operations centres include:
- direct recruitment of mental health professionals into ambulance control rooms.
- rotational schemes in collaboration with local mental health trusts and services.
- cross-service re-deployment of mental health professionals where this a suitable and appropriate option, for example those unable to work face to face.
- extended or altered rota cover, for example where areas only have 12 hours covered, but understanding that resourcing may be planned around mental health demand.
- 999 control room remote access into mental health advice, for example a local clinical advice service or resourced crisis line.
Optimising flow through mental health inpatient settings
We advise all adult and older adult acute mental health settings to take the following steps to help inpatients receive the best support through the available services.
Launch system challenge on discharge from mental health settings
NHS England is launching a national discharge challenge for mental health. This follows the recent success of the 100-day discharge challenge in the acute sector, which resulted in reduced delayed discharges relating to hospital processes. The challenge will be led by integrated care boards, to ensure system accountability and support from multi-agency partners. The scope and approach being taken will be communicated shortly, underpinned by the following overarching aims:
- Fewer people with a long length of stay in acute mental health inpatient care (greater than 60 or 90 days for adults and older adults respectively).
- Fewer people remaining in hospital when they are clinically ready for discharge, resulting in improved care and experience for patients and their carers.
- Improved flow through the acute mental health pathway meaning people can be admitted close to home and in a timely way.
Use of adult social care discharge fund
As set out in a recent letter to the health and social care sector from the Minister for Care, £500 million is being made available to support hospital discharge over the winter period. Discharge from mental health inpatient settings is in scope for this funding and the letter includes further information on how this money is being allocated locally
The system challenge on discharge set out above will support effective local use of this funding.
Flow across whole inpatient pathway
Optimising inpatient flow should be considered across the whole of the pathway, including specialised inpatient provision so that the ability to move up and down the pathway is ensured according to patient need.
Partnership working and early engagement between all agencies/teams involved in someone’s care post-discharge is important to support this. The interventions which form part of the discharge challenge will also help drive improvements in flow across systems.
Additionally, to optimise flow there should be:
- sufficient step down/step up provision
- temporary enablement in-reach support package into someone’s home on their discharge from hospital
- local crisis house capacity
- temporary B&B or similar accommodation while medium-term housing solutions are found, for example for people who may have been rough sleeping or are awaiting home adaptations
- care home/accommodation placements
- home treatment team capacity.
All areas to review escalation protocols for admissions
Reviewing escalation protocols for acute mental health settings will eliminate delays to admission caused by financial sign-off processes for out-of-area placements.
- If someone becomes unwell away from where they are usually resident and they require an emergency admission to a mental health inpatient unit, this should be arranged as quickly as possible.
- It is not acceptable to delay an emergency mental health admission while determining which area has clinical responsibility for an individual. The person should be admitted to a bed where they are. If it is then clinically appropriate to then transfer the person to a setting provided by their local mental health trust, for example because they are well known to their local team, this should be arranged subsequently.
- This aligns with service condition 6 of the NHS Standard Contract, which says that a provider must accept certain referrals to their services from any commissioner, even one with which it holds no written contract. This applies to any referral or presentation for emergency treatment (where the provider can safely accept the referral).
Ensuring system control centres have adequate mental health clinical input
All integrated care boards will be setting up system control centres (SCCs) by the start of December 2022. The specification for SCCs is available here, but in summary they will ensure:
- visibility of operational pressures and risks across providers and system partners
- concerted action across the integrated care service on key systemic and emergent issues impacting patient flow, ambulance handover delays and other performance, clinical and operational challenges
- dynamic responses to emerging challenges and mutual aid
- efficient flows of information.
The minimum viable product requirements of an operational SCC include the need to have 24/7 access to a senior clinician (senior medical or senior nurse decision maker) who can lead and take responsibility for the proactive management of clinical risk and make system-level decisions to balance risk across the urgent and emergency care system. With a specific focus on mitigating clinical risks across the acute, community and mental health urgent and emergency pathway. This will require expert mental health input.
Once up and running, it is recommended that use of SCCs is built into existing mental health bed escalation protocols that all integrated care boards already have in place.
Raising the profile of 24/7 urgent mental health helplines
Areas are encouraged to raise the profile and prominence of access routes to age appropriate crisis care with all services taking the following actions:
Update directories of service (DOS)
All areas to profile 24/7 urgent mental health helplines for all ages on directory of services (DOS), in line with DoS profiling guidance issued in 2020 (on the FutureNHS platform), which describes a standardised approach to profiling, based on national mental health starter and stretch templates and existing urgent mental health 24/7 helpline services.
The DoS lead for each area will be responsible for ensuring that there is an all age 24/7 urgent NHS mental health helpline service DoS profile for each mental health crisis care support service in their region. Service demographic information key contacts can be found on FutureNHS platform.
A national ‘urgent NHS mental health helpline’ DoS service template has been developed collaboratively. The clinical profile is based on existing crisis care telephone support services and will be subject to regular reviews.
Please note: where services are already established and profiled on DoS, these should be re-named and reviewed against the *Service* template – mental health: urgent NHS mental health helpline and amended as appropriated, where this is not yet in place.
Potential benefits of updated directory of service
The 999 service should have an up to date and complete directory of service of NHS, local authority and VCS services and ideally have good relationships and understanding of the local teams and services to whom they might signpost/refer people. This will enable patient access to a range of mental health
professionals to meet different needs e.g. nurses, psychiatrists, peer support workers, other trained professional.
All areas will need to profile crisis lines onto the DoS to achieve the Long Term plan commitment to move towards NHS 111 becoming the single point of access (on the FutureNHS platform) for people experiencing mental health crisis.
Challenges and potential mitigations
- All communications should be clear that mental health patients, like all patients, should only call 999 in an emergency, and that when it is a mental health emergency, 999 is the right option.
- 999 and mental health services should work together to help people get to the right care as soon as possible.
Crisis line capacity
- Commissioners should aim to keep demand and capacity under regular review to ensure that calls do not go unanswered, or result in long waits.
- If a call is not answered by a receiving service, mechanisms should be in place to route the call back to the ‘core’ NHS 111 service.
Increasing local communications
Integrated care systems should seek to increase local comms to ensure more people are aware of mental health support available locally, including when to access all age urgent mental health helpline numbers (promoted via the NHS.UK service finder).
It is important to get people of all ages accessing the right support for their needs as not everyone will require access to urgent mental health services, such as crisis lines and community crisis services.
Engagement with patient advisory groups and media commentary suggests low levels of awareness of the crisis line offers across the country and what crisis lines can and cannot deliver.
A ‘traffic light’ system has been developed by NHS England to help people choose the right support this winter, including when to access 24/7 NHS urgent mental health helplines.
The following graphic can be downloaded in PDF format. There is also an editable version available to download in PowerPoint format for providers and to customise with local service details. Remember to include contact details for local debt services to support people with cost-of-living crisis.
The graphic has been created for systems and services to inform people of the different mental health care options that are available to them and signpost them to the right support It covers getting tips for wellbeing on the Every Mind Matters platform, to calling an NHS urgent mental health helpline in a crisis.
Image text:
1. Looking after yourself: There are little things you can do to look after your mental health. The Every Mind Matters online platform gives you free expert advice and practical tips to help you look after your well-being.
2. Talking Therapy: If you feel stressed, anxious or depressed, you might struggle with work, life or relationships. NHS talking therapies, also known as IAPT, can help. Search nhs.uk/talk
3. Crisis: If you or another person is experiencing a mental health crisis, you can call your local NHS urgent mental health helpline for 24/7 advice and support.
If someone’s life is at risk or they cannot be kept safe, call 999 or go to A&E
Supporting children and young people
An integration framework to support children and young people with mental health needs within acute paediatric settings
We have developed a framework for improving integration between children and young people’s mental health services and acute environments in conjunction with NHS England colleagues and the Royal Colleges.
Additional resources are on our FutureNHS platform page.
The framework currently includes:
- Key principles to underpin joint working.
- System working considerations.
- An aspirational pathway.
- Examples of innovative practice.
- Sign posting to training, including a new online learning platform to enable staff to improve their knowledge, skills and confidence when caring for children and young people with mental health needs, autism or learning disabilities.
Children and young people crisis telephone training
Health Education England has commissioned children and young people crisis telephone training to support crisis mental healthcare staff. This training programme will equip the workforce with the skills, knowledge, and confidence to be able to respond effectively to the needs of children and young people, and their parents and carers, presenting in mental health crisis via the telephone.
Training is scheduled to commence in January 2023. Details on how to access this training offer will be cascaded via Health Education England and NHS England regional teams in December 2022.
Resources and best practice
All-age urgent and emergency care pathway pressures dashboard – a collection of key metrics to monitor and identify any pressures in the pathway.
Acute care case studies – a collection of case studies on reducing delayed discharges, improving staffing mix and reducing inappropriate OAPs.
Crisis alternative case studies – a collection of good practice examples of crisis services, as alternatives to inpatient admission.
Acute mental health dashboard – this dashboard provides reports from the Mental Health Services Data Set relating to: admissions, length of stay, discharge and contacts post-discharge (including 72 hour follow-ups).
Urgent and emergency care mental health dashboard – this dashboard provides reports from the Mental Health Services Data Set (MHSDS) relating to: referrals to crisis and liaison teams, response times and clinical response priority.
Draft acute mental health inpatient guidance – draft guidance for adult and older adult acute inpatient mental health services. This supports systems to meet the ambitions for acute mental health care set out in the NHS Long Term Plan and Mental Health Implementation Plan around improving the therapeutic offer in hospital, reducing length of stay and eliminating out of area placements.
Oliver McGowan mandatory training on learning disability and autism – an e-learning module available for all staff to improve general awareness of the support autistic people or people with a learning disability may need.
Sensory-friendly resource pack – this pack is intended to support the delivery of NHS Long Term Plan commitments for autistic people and the further prevention of mental health crisis in children, young people and adults who are autistic (with or without an additional learning disability).
Breathing Space (debt respite scheme) – information on the government scheme which provides temporary protection from creditors while people receive debt advice and make a plan.
Every Mind Matters – access to advice and practical tips to help people look after their mental wellbeing.
Annex A – ambulance mental health
All systems must invest Long Term Plan funding to embed mental health clinicians into 999 control centres to reduce avoidable conveyance to A&E.
Long Term Plan deliverables for mental health and ambulance
The Long Term Plan Implementation Plan called for integrated care boards to invest £49 million from Mental Health Investment Standard growth in 2022/23 to fund:
- Mental health professionals, ideally rotating in from local mental health services, to be integrated into ambulance trusts to improve telephone triage and support as well as on-scene response.
- A national programme to increase mental health training and education of ambulance staff.
- Capital funding for dedicated mental health response vehicles to increase capacity to respond in a more timely manner, in a more suitable vehicle.
A mental health ambulance vehicle spec has been developed with patients, clinicians and fleet experts and vehicles will be procured this year to go on the road from 2023/2024.

