Equality and health inequalities statement
Promoting equality and addressing health inequalities are at the heart of NHS England’s values. Throughout the development of the policies and processes cited in this document, we have:
- Given due regard to the need to eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it; and
- Given regard to the need to reduce inequalities between patients in access to, and outcomes from healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities.
About this document
This guidance, issued under the NHS provider licence, sets clear expectations of collaboration by NHS trusts and foundation trusts and the governance characteristics that trusts must have in place to support this.
Key points
- The success of individual NHS trusts and foundation trusts will increasingly be judged against their contribution to the objectives of the integrated care system, in addition to their existing duties to deliver safe, effective care and effective use of resources.
- This guidance sets expectations of providers in terms of collaboration in respect of three key areas – engaging consistently in shared planning and decision-making, consistently take collective responsibility with partners for delivery of high quality and sustainable services across various footprints including system and place, and consistently taking responsibility for delivery of agreed system improvements and decisions.
- Five characteristics of governance arrangements that providers must have in place to support effective collaboration are detailed.
Action required
- NHS trust and foundation trust boards must ensure that their organisations have in place the governance arrangements to support effective collaboration.
Other guidance and resources
- Integrated care systems: design framework
- Working together at scale: guidance on provider collaboratives
- The wider suite of Integrated care systems: guidance
1. Introduction
This guidance is issued under the NHS provider licence and applies to NHS trusts and foundation trusts and NHS-controlled providers, collectively referred to in this document as providers [NHS trusts and foundation trusts are expected to comply with the NHS provider licence, including the governance licence condition FT4 under which this guidance is issued. They must also comply with their underlying statutory duties, recognising that there are differences between the duties of NHS trusts and of foundation trusts. In addition, GC5 of the licence obliges providers subject to the licence to have regard to guidance issued under the licence. The NHS-controlled provider licence condition was introduced in early 2018; please refer to the relevant guidance.
Independents providers (Ips) will have certain statutory responsibilities that are different from those of both NHS trusts and foundation trusts; however, the content of this guidance may also be relevant to certain IPs such as those providing commissioner requested services and/or systemically important services at scale]. Provider boards must consider this guidance and ensure that their organisations have in place the governance arrangements to support effective collaboration. The guidance will also be of interest to governors of NHS foundation trusts and others engaged with the governance of providers.
The Health and Care Act 2022 has removed legal barriers to collaboration and integrated care, making it easier for providers to use their knowledge and experience to take on greater responsibility for service planning and putting integrated care systems (ICSs) on a statutory footing through establishing for each ICS:
- An integrated care partnership (ICP), a statutory joint committee of the integrated care board (ICB) and the upper tier local authorities in the ICS, that brings together organisations and representatives concerned with improving the care, health and wellbeing of the population. Each partnership has been established by the NHS and local government as equal partners and has a duty to develop an integrated care strategy proposing how the NHS and local government should exercise their functions to integrate health and care and address the needs of the population identified in the local Joint Strategic Needs Assessment(s).
- An ICB, which brings the NHS together locally, to improve population health and care; its unitary board allocates NHS budget and commissions services, and – having regard to the ICP’s integrated care strategy – produces a five-year joint plan for health services and annual capital plan agreed and created with its partner NHS trusts and foundation trusts.
The ICP and ICB, together with other key elements of the new arrangements including place-based partnerships and provider collaboratives, bring together all partners within an ICS.
This guidance sets a clear expectation that providers collaborate with partners to agree shared objectives through ICPs and collaborate on delivery of the five-year joint plan and annual capital plan through system and place-based arrangements, and provider collaboratives.
The guidance also forms the basis of how we will oversee providers’ performance, with respect to collaboration and the governance needed to support it, under the NHS Oversight Framework. In section 3 of this guidance we explain how this will work in practice.
We will determine the degree and effectiveness of the collaboration through discussion with leaders of an ICB, drawing on a range of information including Care Quality Commission reviews of how effectively systems are working together. See section 3 for further details.
1.1 What is governance?
Governance is the means by which provider boards direct and control their organisations so that decision-making is effective, risk is managed and the right outcomes are delivered. In the NHS these outcomes include ensuring the delivery of safe and effective services in a caring and compassionate environment, while collaborating effectively with partners. The Health and Care Act 2022 requires providers to have regard to the effect of their decisions on the triple aim duty of better health and wellbeing for everyone, better quality of health services for all and sustainable use of NHS resources. Effective participation within system and place-based partnerships, and provider collaboratives will be necessary.
A separate framework has been issued that sets out the competencies and behaviours expected by individuals holding board responsibilities as part of effective NHS boards. Details of competency frameworks published to date can be found at the leadership academy.
1.2 Why we have issued this guidance
Better health, improved care quality (for further insight please see NHS England » National Guidance on Quality Risk Response and Escalation in Integrated Care Systems) and a reduction in health inequalities (for further information, see Core20PLUS5, an NHS England approach to support the reduction of health inequalities at both national and system level. The approach defines a target population cohort – the ‘Core20PLUS’ – and identifies ‘5’ focus clinical areas requiring accelerated improvement) for populations across England will be delivered by providers working collaboratively as part of system and place-based partnerships and provider collaboratives, and the wider health and care system in England.
Effective collaboration requires system-minded leadership (These ambitions are set out in more detail in the people promise and NHS Long Term Plan – workforce – recognising that trusts and other health and care organisations together are the system – and strong working relationships between partners to develop shared objectives and ensure their delivery. This must be underpinned by organisational and individual behaviours that create the right environment for collaborative change. Providers can put in place governance arrangements to help ensure that these essential ingredients are in place and are used to deliver system improvements.
We have issued this guidance to set clear expectations of how providers should work and collaborate with partners via system and place-based partnerships, and provider collaboratives, and the governance arrangements that must be in place to support this, to comply with the governance conditions of the NHS provider licence.
The guidance builds on and supports the ambitions and commitments set out in:
- Integrated care systems: design framework
- Working together at scale: guidance on provider collaboratives
- The wider suite of Integrated care systems: guidance
- NHS Long Term Plan
2. How we expect providers to collaborate with system partners
2.1 Building on response to and recovery from COVID-19
The health and care system’s response to, and ongoing recovery from, the COVID-19 pandemic highlights the power of collaboration. Providers worked together and with other partners at pace to respond to the health crisis and they continue to do so to recover performance. Collaborative working to maximise the use of system resources – such as through mutual aid (we refer to mutual aid in the broad sense. We are not referring to mutual aid within the NHS COVID-19 vaccination programme for which there is a specific national policy) – enabled an effective response to the needs of patients, service users and the public, which could not have been achieved by providers working alone.
2.2 Expectations of provider collaboration
Providers have an active and strong leadership role to play in system and place-based partnerships, provider collaboratives, and the wider health and care system in England, collaborating with both NHS partners and others such as local authorities to transform care and manage system performance. ICSs exist to achieve four aims:
- improve outcomes in population health and healthcare
- tackle inequalities in outcomes, experience and access
- enhance productivity and value for money
- help the NHS support broader social and economic development.
In addition to their existing duties to deliver safe, effective care and effective use of resources, the success of individual NHS trusts and foundation trusts will increasingly be judged against their contribution to the objectives of the ICS (Integrated care systems: design framework, p30.).
In this section we set expectations of providers in terms of collaboration in respect of three key areas and give illustrative (non-exhaustive) minimum behaviours. At the heart of effective collaboration is the expectation that providers will work effectively on all issues, including those that may be contentious for the organisation and system partners, rather than focusing only on those issues for which there is already a clear way forward or which are perceived to benefit their organisation. Appropriate priority will need to be given to reducing health inequalities and ensuring equitable access to services. We recognise that providers are working in different local contexts and their priorities will therefore vary. The three key areas are:
1. Providers will engage consistently in shared planning and decision-making – participating consistently and constructively with partners in system and place-based partnerships and provider collaboratives (this may include place-based partnerships, provider collaboratives or other clinical networks.), and ensuring open sharing of information and appropriate delegations are in place to develop shared plans and priorities and reach shared decisions.
- Ensuring the participation of leaders with appropriate authority in system and place-based partnerships, and provider collaboratives to ensure shared or joined-up planning and effective decision-making arrangements, including in respect of capital plans.
- Committing sufficient resources to, and ensuring digital and data systems enable, system and place-based partnerships, and provider collaboratives to ensure shared planning and decision-making.
- Sharing sufficient information on a timely basis with partners to support shared planning and decision-making, and having regard to other sources of information such as joint strategic need assessments.
- Exploring the case for new service delivery models with partners, such as lead provider contracts, service reconfigurations, mergers or other arrangements.
- Being willing to discuss any relevant issue with partners rather than only those perceived to be in the organisation’s immediate interest.
- Sharing intelligence on quality concerns/risks, and working with partners to mitigate and manage those risks (including with appropriate risk sharing).
- Having regard to the triple aim duty of better health and wellbeing for everyone, better quality of health services for all and sustainable use of NHS resources.
2. Providers will consistently take collective responsibility with partners for delivery of services across various footprints including system and place – helping enable a shared understanding of performance, supporting arrangements for working together to manage any risks to delivery and contributing to a culture that supports continuous system improvement.
- Sharing demand and capacity information, including through system and place-based partnerships, or provider collaboratives, to allow partners to effectively manage risks to delivery of services.
- Engaging in mutual aid with other providers such as patient redirection, sharing of key workforce and sharing of scarce resources according to need.
- Seeking peer review and support in a timely manner if their organisation is at risk of failing to deliver its contribution to overall delivery of services.
- Working collaboratively with partners to improve care quality across pathways and services.
- Participating in clinical networks to raise standards of clinical practice and deliver benefits from collaborative working.
- Working with partners to deliver financial objectives in line with any system agreements of which a provider is part.
3. Providers will consistently take responsibility for delivery of improvements and decisions agreed through system and place-based partnerships, provider collaboratives or any other relevant forums – ensuring that: organisational plans are integrated with the five-year joint system plan; annual capital plan is agreed with the ICB and its partners; and that the organisation implements shared decisions and plans agreed through all relevant forums in a timely manner.
- Clearly articulating how organisational plans integrate with the ICB five-year joint plan and annual capital plan, and other shared plans for delivery of agreed improvements.
- Active participation in system quality groups to support improvement in care quality.
- Timely and effective implementation of decisions agreed through system and place-based partnerships and provider collaboratives, or any other relevant forums.
- Working to deliver the financial duties and objectives for which the provider is collectively responsible with ICB partners. This includes the duty on local resource use not exceeding a limit set by NHS England.
- Sharing with partners the risks and benefits of agreed improvements or shared decisions.
- Committing sufficient workforce and resources to deliver agreed improvements.
We give scenarios in Appendix A to indicate the ways in which providers collaborate effectively.
2.3 Characteristics of governance arrangements to support effective collaboration
Effective collaboration between providers and with a range of other partners is necessary if the NHS is to transform health and care for patients and the public, and support the delivery of integration with social care and other partners.
Collaboration needs to take place in respect of the three key areas set out above and providers must have in place governance arrangements to ensure that they are collaborating effectively. The relationship between expected outcomes, collaboration by providers and governance arrangements is summarised in the diagram below.
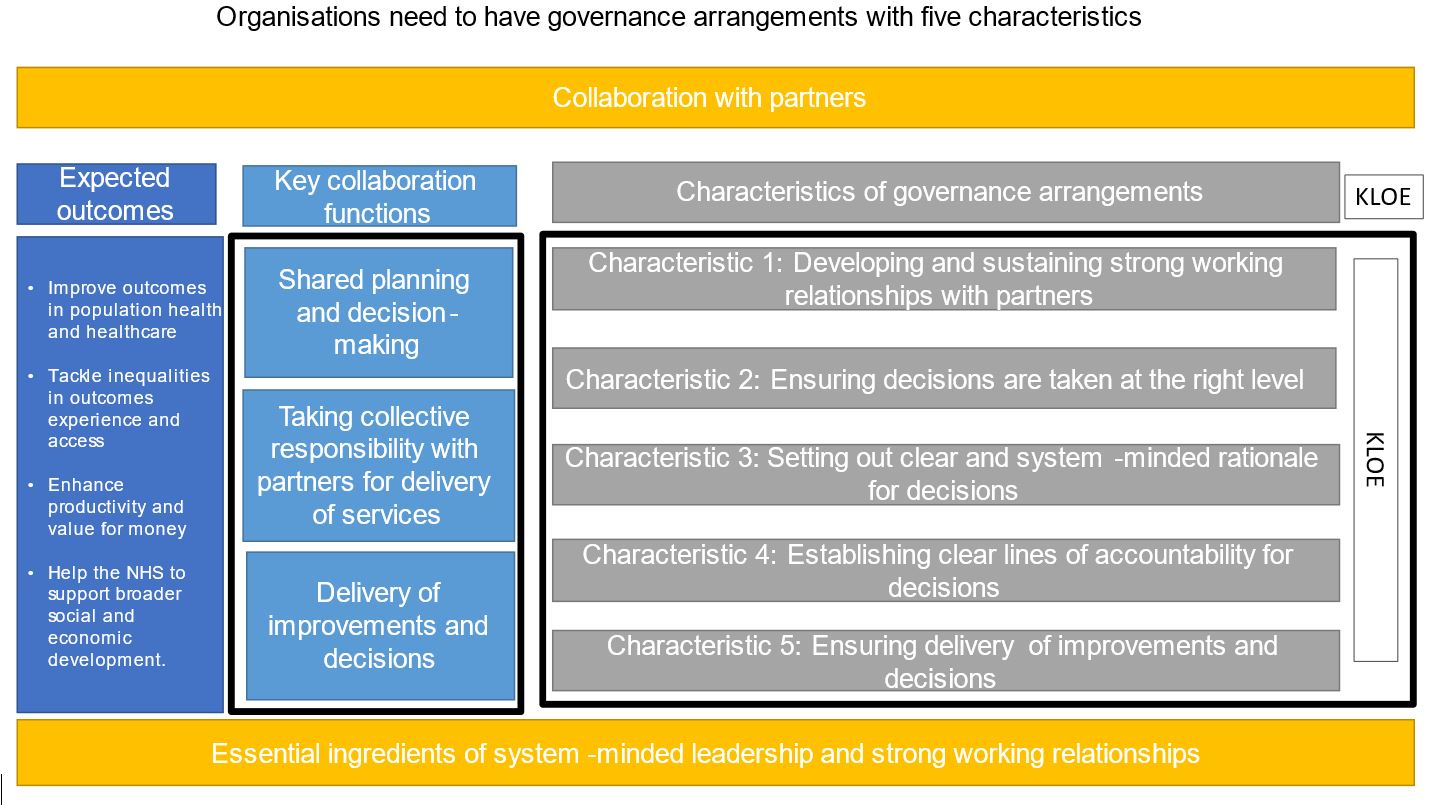
Below details five characteristics of governance arrangements to support effective collaboration; there may be others depending on particular situations. It also sets out the key lines of enquiry that, when used by NHS England in discussion with an ICB, are likely to indicate whether or not a provider is acting in line with this guidance and the underlying obligations; they are not intended to be exhaustive and should not be used as a compliance checklist (other guidance on good governance continues to apply, and providers should refer to the Code of governance for NHS provider trusts and the Well-led framework for further details. Providers will also need to have due regard to other relevant legal obligations. These include: the duty on NHS bodies to co-operate with each other and the duty on foundation trust directors to maximise benefits for the public as well as their members).
1. Developing and sustaining strong working relationships with partners: The manner of engagement must be consistently constructive and where appropriate proactive.
Key lines of enquiry:
- Do providers consistently engage with partners in a meaningful, effective and constructive way?
- Are providers contributing to building a culture of transparency, honesty, and constructive challenge where collective responsibility is taken for problems and conflicts are resolved quickly?
- Do providers communicate system vision, values and strategic goals to their staff and other stakeholders?
2. Ensuring decisions are taken at the right level: Decisions should be taken at the most appropriate level (eg ICP, ICB, place-based partnership, provider collaborative, provider board).
Key lines of enquiry:
- Do providers actively participate in all relevant and appropriate planning and decision-making forums? This may include system and place-based partnerships or provider collaboratives.
- Are decisions taken at the most appropriate level given the nature of the issue and are providers working with partners, including NHS bodies, local government and primary care, and engaging staff, patients and the wider public as necessary?
- Do providers engage with all relevant organisations and stakeholders on decisions that might affect them?
3. Setting out clear and system-minded rationale for decisions: There should be clear consideration and articulation of why decisions have been made, having regard to the triple aim duty of better health and wellbeing for everyone, better quality of health services for all, and sustainable use of NHS resources.
Key lines of enquiry:
- Are providers collaborating to develop the business case for any proposed system improvements, through a structured planning process, and working with patients, workforce and external partners?
- Do providers support an open and constructive dialogue regarding any risks or concerns?
- Has an equalities and health inequalities impact assessment been conducted where appropriate to inform decision-making?
- Have decisions been made with regard to the triple aim duty to support better health and wellbeing for everyone, better quality of health services for all and sustainable use of NHS resources, giving particular attention to reducing health inequalities between communities within the population?
- Are providers actively building business intelligence capacity to enable a single shared view of local challenges, performance and progress against delivery?
4. Establishing clear lines of accountability for decisions: There must be clear lines of accountability for decisions, taking into account providers’ legal responsibilities and internal governance.
Key lines of enquiry:
- Have providers established clear reporting lines and accountabilities, with timely and effective oversight of their involvement in system and place-based partnerships, and provider collaboratives?
- Do providers empower system, place-based and at scale provider decision-making by appropriately delegating responsibility?
- Are there appropriate governance mechanisms within the organisation and joint working arrangements with partners, such as dispute resolution or escalation mechanisms, in place and are they well understood and effective?
- Are providers’ strategic plans integrated with the ICB’s five-year joint plan and annual capital plan, and the plans of place-based partnerships and provider collaboratives?
- Are providers actively involved in co-producing and driving programmes and plans?
5. Ensuring delivery of improvements and decisions: There must be adequate systems and processes to ensure providers follow through on shared decisions so that system and place level improvements are delivered for the benefit of patients and the public.
Key lines of enquiry:
- Are providers committed to enabling the successful delivery of plans, including a willingness to share any risks or benefits that arise from collaboration?
- Do providers proactively and openly share high-quality information as appropriate to support planning and/or implementation of improvements for the benefit of patients?
- Do providers commit adequate resources and staff to participate in system planning and delivery, such as taking up system leadership roles, embedding or seconding staff to partner organisations, or contributing to funding a joint project management office?
- Have providers put in place detailed delivery plans for their own organisations and agreed actions against which progress is regularly monitored, to enable them to identify and manage any risks or challenges that arise?
3. How NHS England will apply this guidance
We anticipate that providers will want to continue to work to realise the benefits that collaboration brings by actively working with partners through ICPs and ICBs, place-based partnerships, provider collaboratives and any other relevant forums. We further understand that providers will want to access the full range of support available from NHS England as they seek to collaborate with one another and work effectively with other health and care organisations.
By setting clear expectations of providers in terms of collaboration and what it means for governance arrangements, this guidance contributes to the way we will oversee providers’ collaboration under the NHS Oversight Framework. We recognise that providers are working in different local contexts and their priorities will therefore vary.
We expect that where system partners are concerned about the effectiveness of or commitment to collaboration, they will seek to resolve this informally with the relevant provider in the first instance.
We would anticipate that leaders of ICBs and any other relevant forums would step in informally when required to facilitate resolution and then, if necessary, that any formal dispute resolution procedures would be followed. This could include inviting a third party to mediate or drawing on support from NHS England.
Where appropriate, and in discussion with leaders of an ICB, we may intervene to resolve situations where poor governance means that a provider appears to be failing to collaborate in line with this guidance or its governance obligations in the NHS provider licence. We will then consider whether there is cause to look into the matter further and to assess whether the circumstances might merit formal regulatory action, drawing on the above key lines of enquiry and a range of information to form a rounded view on a case-by-case basis.
Appendix A: Scenarios illustrating ways in which providers can collaborate effectively
Scenario 1: Effective collaboration to plan and shape system improvements
Developing new service delivery models, such as networked clinical services, built on effective collaboration between partners, can contribute to better health and improved care quality, and reduce health inequalities.
Such collaboration may require a provider within a system, place-based partnership or provider collaborative to make substantial changes to some of its services with implications for its income and other related services it delivers.
There is a risk that organisations might be slow to address such issues, which may be contentious, and that such issues are considered too difficult to pursue. Collaboration, supported by effective governance arrangements within trusts, can be used to mitigate this.
- Leaders of providers proactively develop effective working relationships with partners across the relevant system and place-based partnerships, or provider collaborative as they seek to identify opportunities for system improvements (eg the work of systems quality groups).
- Providers openly share with partners information and data needed to explore contentious issues and construct a sound case for change which articulates a shared understanding of the benefits of a service development to patients and the public.
- Providers take full account of relevant clinical input (eg from clinical networks and clinical senates) in building a case for change, to understand the benefits and the interdependency of any other clinical activity that there might be for each provider.
- Providers work together to appropriately mitigate any service or financial risks for an individual provider and maintain the quality of care provided to the population and patients. This may include providers working with relevant regulatory bodies to understand the impact that the new service development may have on an individual organisation’s performance.
- Throughout the process providers have regard to the triple aim duty of better health and wellbeing for everyone, better quality of health services for all individuals and sustainable use of NHS resources.
Scenario 2: Effective collaboration to collectively manage performance
The NHS’s response to the COVID-19 pandemic, eg through mutual aid and the flexible use of NHS people, showed the power of effective collaboration to identify and manage risks to service delivery.
Providers want to maintain this level of collaboration and not to move back to a narrower organisational focus. Collaboration supported by effective governance arrangements for a trust can be used to achieve this.
- Leaders of providers ensure that working relationships are fostered at a range of levels across organisations, as opposed to only at the most senior level, to ensure close alignment of managerial teams and clinical teams in different provider organisations.
- Providers generate a shared understanding of performance and the delivery of services at system or place through developing shared business intelligence capacity to enable a common view of performance, risks and progress against set service objectives.
- Providers collaborate via agreed decision-making forums for the objectives being considered. They have a shared and agreed understanding with partners of which decision-making body is appropriate and boards have ensured that appropriate delegations are in place.
- Providers are open about risks and concerns, and engage with partners in a constructive manner to mitigate and address any issues. This is supported by establishing clear reporting lines and accountabilities flowing from any joint working arrangement into the governance arrangements of the individual trust, and having a clear and agreed process for participating in the resolution and escalation of issues that are shared and understood by all participants.
Scenario 3 Delivery of agreed improvements and decisions
Providers recognise that there is risk that discussions in shared forums may not result in timely delivery of system improvements. Collaboration supported by effective governance arrangements can be used to mitigate this.
- Leaders of providers develop a clear vision of the role the organisation plays in system and place-based partnerships, and provider collaboratives, and in achieving shared priorities, and this is communicated to workforce and stakeholders.
- Providers ensure that their annual plans are fully integrated with the ICB five-year joint plan, which partner trusts must agree, and with provider collaborative plans, and actively engage in co-producing and driving shared programmes of work and committing the necessary resources to ensure delivery.
- Providers boards put in place appropriate delegations to their representatives in all relevant forums, to ensure that decisions can be put into effect in a timely manner by the provider board.
- Providers work with their partners to understand and resolve any conflicts of commercial interest presented by system improvements and decisions, and reflect the resolution in any risk share agreements.
- Provider boards seek assurance that their organisation is implementing in a timely manner agreed improvements and decisions taken within ICBs, place-based partnerships, provider collaboratives or any other relevant forums.
Publication reference: PR2075

