ICBs and their partner trusts have a duty to prepare a plan setting out how they propose to exercise their functions in the next five years (the ‘Joint Forward Plan’ (JFP)).
We expect that ICBs and trusts will wish to perform a limited refresh of existing plans before the beginning of the new financial year given the anticipated publication of the 10 year health plan in the Spring of 2025 and a multi-year financial settlement for the public sector as part of the Spending Review 2025.
We will work with systems to develop a shared set of expectations and timetable for a subsequent more extensive revision of JFPs aligned to wider reform of nationally co-ordinated NHS planning processes. This will include a shift from single to multi-year operational and financial planning.
View the guidance on developing joint capital resource use plans 2025/26
Updates between versions will be documented in the table below and highlighted in yellow.
| Version | Date | Changes |
|---|---|---|
| V1.0 | 22 December 2023 | Initial Version |
| V1.1 | 20 March 2024 | Updates: Clarified dates for preparing and publishing 2024/25 Joint Forward Plans |
1. Introduction
This updated guidance for 2024/25 supports integrated care boards (ICBs) and their partner NHS trusts and foundation trusts (referred to collectively in this guidance as partner trusts) to further develop and/or revise the joint forward plans (JFPs) they first published earlier this year.
The National Health Service Act 2006 (as amended by the Health and Care Act 2022) requires ICBs and their partner trusts[1] to prepare a plan setting out how they propose to exercise their functions in the next five years. These should be reviewed and/or revised before the start of each financial year.
Systems continue to have the same flexibility to determine their JFP’s scope and how it is developed and structured. For the majority of ICBs, revised plans are likely to reflect a continuation of the priorities set out in the previous year’s JFP (dependent on the detail previously included). The annual review is an opportunity to update plans based on updated assumptions or priorities, including those set out in the 2024/25 priorities and operational planning guidance) and address the last year of the five-year look ahead.
This guidance summarises the specific statutory requirements that plans must meet. It should be read alongside the 2024/25 priorities and operational planning guidance. Specific JFP supporting resources are available on the FutureNHS collaboration platform (registration/log in is required)
1.1 Action required of ICBs and their partner trusts
ICBs and their partner trusts are required to prepare a JFP before the start of each financial year, setting out how they intend to exercise their functions in the next five years. To provide the opportunity to reflect the 2024/25 priorities and operational planning guidance, once published, NHS England is setting 30 June 2024 as the date for ICBs to publish and share their JFPs with us, their integrated care partnerships and health and wellbeing boards.
If there are significant revisions to the initial JFP, ICBs and their partner trusts must consult with those for whom the ICB has core responsibility[2] and anyone else they consider appropriate. This should include the integrated care partnership (ICP) and NHS England (with respect to the commissioning functions that have been and will be delegated to ICBs). A draft of the revised JFP should be shared with the relevant ICP and NHS England; see section 4.1.
ICBs and their partner trusts must involve relevant health and wellbeing boards (HWBs) in revising the JFP. This includes sharing a draft with each relevant HWB, and consulting relevant HWBs on whether the JFP takes proper account of each relevant joint local health and wellbeing strategy (JLHWS); see section 4.1.
ICBs and their partner trusts should then agree processes for finalising and signing off the revised JFP. The final version must be published in an accessible format on the ICB website.
ICBs and their partner trusts should expect to be held to account for delivery of the JFP – including by their population, patients and their carers or representatives – and through the ICP, Healthwatch and the local authorities’ health overview and scrutiny committees.
1.2 Purpose of the joint forward plan
JFPs should set out how the ICB will meet its population’s health needs. As a minimum, it should describe how the ICB and its partner trusts intend to arrange and/or provide NHS services to meet the physical and mental health needs of their population. This should include the delivery of universal NHS commitments,[3] address ICSs’ four core purposes and meet legal requirements.[4]
Legal responsibility for developing the JFP lies with the ICB and its partner trusts. However, we encourage systems to use the JFP to set out a shared delivery plan for the ICP integrated care strategy[5] and the JLHWS developed by local authorities and their partner ICBs,[6] that is supported by the whole system, including local authorities and voluntary, community and social enterprise partners.
1.3 Relationship with NHS planning
ICBs and their partner trusts will continue to separately submit specific operational and financial information to NHS England as part of the nationally co-ordinated NHS planning process. NHS England will continue to work with systems to avoid duplication and ensure alignment between NHS planning submissions and the public facing JFP.
2. Principles
Three principles – describing the JFP’s nature and function – were co-developed for 2023/24 with ICBs, trusts and national organisations representing local authorities and other system partners. These principles, as outlined in Box 1, continue to apply.
Box 1: JFP principles
Principle 1: Fully aligned with the wider system partnership’s ambitions.
Principle 2: Supporting subsidiarity by building on existing local strategies and plans as well as reflecting the universal NHS commitments.
Principle 3: Delivery focused, including specific objectives, trajectories and milestones as appropriate.
3. Legislative requirements
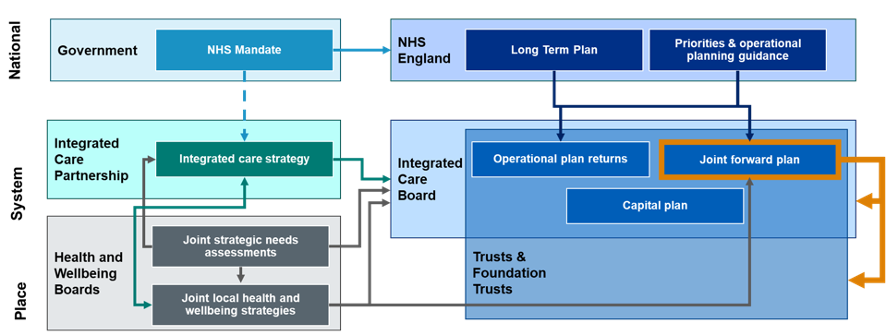
Statute describes the purpose of the JFP, the NHS mandate, the integrated care strategy, JLHWSs, joint strategic needs assessments (JSNAs) and system capital plans. For the relationship between the various requirements, see
Appendix 1.Appendix 2, Table 1 describes each statutory requirement the JFP must meet.
4. Developing and updating the JFP
4.1 Consultation
Systems will have engaged local partners in the development of their initial JFP,[7] including:
- the ICP (ensuring this also provides the perspective of social care providers)[8]
- primary care providers[9]
- local authorities and each relevant HWB
- other ICBs in respect of providers whose operating boundary spans multiple ICSs
- provider collaboratives, clinical networks and other alliances
- the voluntary, community and social enterprise sector
- people and communities that will be affected by specific parts of the proposed plan, or who are likely to have a significant interest in any of its objectives, in accordance with the requirement to consult described below.
Where an ICB and its partner trusts are revising an existing plan in a way they consider to be significant (see section 4.2 for revision of plans), there is a statutory duty to consult:
- people for whom the ICB has core responsibility: ie those registered with a GP practice associated with the ICB or unregistered patients who usually reside in the ICB’s area (as described in the ICB constitution)
- anyone else they consider it appropriate to consult, eg specific organisations with an interest in the plan or whose views it would be useful to obtain, and out-of-area patients who receive treatment funded by the ICB.
The approach should be determined by the ICB and its partner trusts but could involve working with people to understand how services can better meet local needs, developing priorities for change and gathering feedback on the revised JFPs.
As JFPs will build on and reflect existing JSNAs, JLHWSs and NHS operational delivery plans, we do not anticipate their development will require full formal public consultation, unless a significant reconfiguration or major service change is proposed.[10]
Previous local patient and public engagement exercises and subsequent action should inform the JFP. The ICB and its partners will need to consider how this is managed to maximise the benefits from engagement and fulfil these statutory duties efficiently.
For consistency and to avoid duplication of effort, we recommend ICBs and their partner trusts develop a standard approach to consulting on the JFP.
In developing the JFP, ICBs and their partner trusts should consider other relevant duties: eg seeking the views of underserved groups (such as inclusion health groups and vulnerable populations) as part of the duty to reduce inequalities. They must also show they have discharged their legal duty under the Public Sector Equality Duty (s.149, Equality Act 2010).
ICBs and their partner trusts must include in their JFP a summary of the views expressed by anyone they have a duty to consult and explain how they have taken them into account.
Further guidance on public engagement and consultation for ICBs is on the NHS England website.
NHS England’s role
NHS England will continue to support ICBs and their partner trusts to develop and revise JFPs. We will review and comment on updated draft JFPs, and we recommend this is done in parallel with the review by HWBs (see below). This is not a formal assurance process but an opportunity to support ICBs and their partner trusts to develop their plans.
ICBs are accountable to NHS England for the delivery of their statutory functions, including arranging for the provision of services to meet the physical and mental health needs of their populations. The JFP, and delivery against its priorities, will form part of the evidence that NHS England considers in undertaking its performance assessment of ICBs.
Role of health and wellbeing boards
In preparing or revising their JFPs, ICBs and their partner trusts are subject to a general legal duty to involve each HWB whose area coincides with that of the ICB, wholly or in part. The plan itself must describe how the ICB proposes to implement relevant JLHWSs.[11]
ICBs and their partner trusts must send a draft of the JFP to each relevant HWB when further developing or undertaking significant revisions or updates. They must consult those HWBs on whether the draft takes proper account of each JLHWS published by the HWB that relates to any part of the period to which the JFP relates. A HWB must respond with its opinion and may also send that opinion to NHS England, telling the ICB and its partner trusts it has done so (unless it informed them in advance that it was planning to do so).[12]
If an ICB and its partner trusts subsequently revise the JFP, the updated version should be sent to each relevant HWB, and the consultation process described above repeated.
The JFP must include a statement of the final opinion of each HWB consulted.
Available support
Supporting resources providing further content recommendations are available.
NHS England regional teams can offer support and advice and should be engaged early.
Please direct any technical queries to england.nhs-planning@nhs.net.
Appendix 1: Legislative framework – further detail
Figure 1 shows the statutory framework relating to the JFP. Please note, it does not show interaction with wider system partners.
Figure 1: Relationship of the JFP with other strategies and plans[13]
NHS mandate
The government’s mandate to NHS England sets out its objectives, revenue and capital resource limits. This informs guidance from NHS England on priorities and planning requirements.
The JFP will address objectives in the government mandate regarding the ambitions in the NHS Long Term Plan and NHS planning guidance. It will also deliver on the integrated care strategy, which must take account of the mandate.
Integrated care strategy
The Department of Health and Social Care has issued guidance on the development of integrated care strategies.
The Local Government and Public Involvement in Health Act 2007, as amended by the Health and Care Act 2022, requires the ICP to produce an integrated care strategy. This should describe how the local population’s assessed needs will be met through the exercise of functions by the ICB, local authorities and NHS England. It must address integration of health and social care and should address integration with health-related services
In addition, the ICP must consider the NHS mandate in developing the integrated care strategy. As such, it should reflect both NHS priorities described in the mandate and the local population’s assessed needs.
The ICB has a statutory duty to have regard to the relevant integrated care strategy in exercising its functions. The JFP is expected to set out steps for delivering the integrated care strategy.
Capital plan
Before the start of each financial year, ICBs and their partner trusts must set out their planned capital resource use. We have published separate guidance on preparing capital plans.
The content of the JFP should be consistent with this capital plan.
ICB annual assessment
Under the terms of the Health and Care Act (2022), NHS England is required to undertake a performance assessment of each ICB in respect of each financial year and to publish a summary of these assessments. In undertaking this assessment, NHS England will consider how successfully each ICB has performed against a range of specific duties and objectives including how well the ICB has delivered against priorities set out in its Joint Forward Plan.
Joint strategic needs assessments (JSNA)
JSNAs, developed by each responsible local authority and its partner ICBs, assess needs that can be met or be affected by the responsible local authority, its partner ICBs or NHS England. These include the local community’s current and future health, care and wellbeing needs, as well as the wider determinants of health which affect those needs, to inform local decision-making and collaboration on development of JLHWSs and the integrated care strategy.
The ICB has a statutory duty to consider JSNAs when exercising any relevant functions. The JFP is expected to describe delivery plans to meet the population health needs of people in the ICB’s area.
Joint local health and wellbeing strategies
Each responsible local authority and its partner ICBs will have produced a JLHWS. This is a strategy to meet the needs identified in JSNAs and is unique to each local area. The ICP is expected to build on the JLHWS, which may be facilitated by shared membership across HWBs and the ICP
Each responsible local authority and its partner ICBs are required to consider whether JLHWSs need to be updated in response to any new or updated integrated care strategy.
The ICB has a statutory duty to have regard to JLHWSs in exercising any relevant functions. The steps that the ICB proposes to take to implement any JLHWS must be described in the JFP.
Appendix 2: Legislative requirements – further detail
Table 1: Summary of legislative requirements
| Legislative requirement | Description | Implications for the JFP |
| Duty to promote integration | Each ICB must exercise its functions with a view to ensuring that health services are delivered in an integrated way and that their provision is integrated with that of health-related or social care services, where this would: improve quality of those servicesreduce inequalities in access and outcomes. | Plans should describe how ICBs will integrate health services, social care and health-related services to improve quality and reduce inequalities. This could include arrangements for: at-scale collaboration (eg provider collaboratives)partnership approaches to integrated neighbourhood teamsfunctional integration (eg non-clinical functions)service or clinical integration (eg through shared pathways, multidisciplinary teams, clinical assessment processes). This must include delivery on the integration ambitions described in the relevant integrated care strategy and joint local health and wellbeing strategies (JLHWSs). |
| Describing the health services for which the ICB proposes to make arrangements | The plan must describe the health services for which the ICB proposes to make arrangements in the exercise of its functions. | The plan should set out how the ICB will meet its population’s health needs. As a minimum, it should describe how the ICB and its partner trusts intend to arrange and/or provide NHS services to meet the physical and mental health needs of their population. |
| Duty to consider wider effect of decisions | In making decisions about the provision of healthcare, an ICB must consider the wider effects of its decisions, also known as the triple aim of: (a) health and wellbeing of the people of England (including by reducing inequalities with respect to health and wellbeing) (b) quality of healthcare services for the purposes of the NHS (including by reducing inequalities with respect to the benefits obtained by individuals from those services) and (c) sustainable and efficient use of resources by NHS bodies. | The plan should articulate how the triple aim was considered in its development. It should also describe approaches to ensure the triple aim is embedded in decision-making and evaluation processes. |
| Implementing any JLHWS | The plan must set out the steps that the ICB proposes to take to implement any JLHWSs to which it is required to have regard under section 116B(1) of the Local Government and Public Involvement in Health Act 2007. | The plan must set out steps the ICB will take to deliver on ambitions described in any relevant JLHWSs, including identified local target outcomes, approaches and priorities. |
| Financial duties | The plan must explain how the ICB intends to discharge its financial duties. | The plan must describe how the financial duties under sections 223GB to 223N of the NHS Act 2006 will be addressed. This includes ensuring that the expenditure of each ICB and its partner trusts in a financial year (taken together) does not exceed the aggregate of any sums received by them in the year, and complying with NHS England financial objectives, directions and expenditure limits. It should also set out how the efficiency and productivity of NHS services will be improved in line with the core purpose to enhance productivity and value for money. This should include the key actions the ICB will take to ensure that the collective resources of the health system are used effectively and efficiently. This could include specific plans to support the effectiveness of financial governance and controls; address unwarranted variation; strengthen understanding of the cost of whole care pathways; maximise consolidation and collaboration opportunities across corporate services; unlock efficiency through capital investment; and improve use of NHS estate. |
| Duty to improve quality of services | Each ICB must exercise its functions with a view to securing continuous improvement in: the quality of services provided to individuals for or in connection with the prevention, diagnosis or treatment of illnessoutcomes including safety and patient experience. | The plan should contain a set of quality objectives that reflect system intelligence. It should include clearly aligned metrics (on processes and outcomes) to evidence ongoing sustainable and equitable improvement. Quality priorities should go beyond performance metrics and look at outcomes and preventing ill-health and use the Core20PLUS5 approach to ensure inequalities are considered. Plans should align with the National Quality Board principles. |
| Duty to reduce inequalities | Each ICB must have regard to the need to: (a) reduce inequalities between persons with respect to their ability to access health services and (b) reduce inequalities between patients with respect to the outcomes achieved for them by the provision of health services. There is also a duty to have regard to the wider effects of decisions on inequalities. The duty to promote integration requires consideration of securing integrated provision across health, health-related and social services where this would reduce inequalities in access to services or outcomes achieved. | The plan should set out how the ICB intends to deliver on the national vision to ensure delivery of high-quality healthcare for all, through equitable access, excellent experience and optimal outcomes. ICBs must also be mindful of, and comply with, the requirements of the Public Sector Equality Duty, section 149 of the Equality Act 2010. |
| Duty to promote involvement of each patient | Each ICB must promote the involvement of patients, and their carers and representatives (if any), in decisions that relate to: (a) the prevention or diagnosis of illness in the patients or (b) their care or treatment. | The plan should describe actions to implement the Comprehensive model of personalised care, which promotes the involvement of each patient in decisions about prevention, diagnosis and their care or treatment. |
| Duty to involve the public | ICBs and partner trusts have a duty to involve people and communities in decisions about the planning, development and operation of services commissioned and provided. | The plans should describe how: the public and communities were engaged in the development of the planthe ICB and partner trusts will work together to build effective partnerships with people and communities, particularly those who face the greatest health inequalities, working with wider ICS stakeholders to achieve thisactivity at neighbourhood and place level informs decisions by the system and how public involvement legal duties are met and assured. |
| Duty to patient choice | Each ICB must act with a view to enabling patients to make choices with respect to aspects of health services provided to them. | The plan should describe how ICBs will ensure that patient choice is considered when developing and implementing commissioning plans and contracting arrangements and delivering services. The plan should also describe how legal rights are upheld and how choices available to patients are publicised and promoted. |
| Duty to obtain appropriate advice | Each ICB must obtain appropriate advice to enable it to effectively discharge its functions from persons who (taken together) have a broad range of professional expertise in: (a) the prevention, diagnosis or treatment of illness and (b) the protection or improvement of public health. | The plan should outline the ICB’s strategy for seeking any expert advice it requires, including from local authority partners and through formal governance arrangements and broader engagement. |
| Duty to promote innovation | Each ICB must promote innovation in the provision of health services (including in the arrangements made for their provision). | The plan should set out how the ICB will promote local innovation, build capability for the adoption and spread of proven innovation and work with academic health science networks and other local partners to support the identification and adoption of new products and pathways that align with population health needs and address health inequalities. |
| Duty in respect of research | Each ICB must facilitate or otherwise promote: (a) research on matters relevant to the health service and (b) the use in the health service of evidence obtained from research. | The plan must set out how ICBs intend to discharge their duty to facilitate or otherwise promote research, and the use in the health service of evidence obtained from research. This could include considering research when commissioning, encouraging existing providers to support and be involved in research delivery, recognising the research workforce in workforce planning, and supporting collaboration across local National Institute for Health and Care Research (NIHR) networks. Plans should address the research needs of the ICBs diverse communities. |
| Duty to promote education and training | Each ICB must have regard to the need to promote education and training[14] so as to assist the Secretary of State and Health Education England (HEE)[15] in the discharge of the duty under that section. | The plan should describe how the ICB will apply education and training as an essential lever of an integrated workforce plan that supports the delivery of services in the short, medium and long term. The plan should articulate the role of education and training in securing healthcare staff supply and responding to changing service models, as well as the role of trainees in service delivery. |
| Duty as to climate change | Each ICB must have regard to the need to: (a) contribute towards compliance with (i) section 1 of the Climate Change Act 2008 (UK net zero emissions target) and (ii) section 5 of the Environment Act 2021 (environmental targets) and (b) adapt to any current or predicted impacts of climate change identified in the most recent report under section 56 of the Climate Change Act 2008. | The plan should describe how the ICB and its partner trusts will deliver against the targets and actions in Delivering a ‘Net Zero’ NHS , including through aligning the JFP with existing green plans. |
| Addressing the particular needs of victims of abuse | The plan must set out any steps that the ICB proposes to take to address the particular needs of victims of abuse (including domestic and sexual abuse, whether children or adults). It must have due regard to the provisions of the Domestic Abuse Act 2021 and accompanying statutory guidance, and relevant safeguarding provisions. | This should include related health inequalities and access to, and outcomes from, services. The plan should also cover the needs of staff who are victims of abuse. This should include the use of data and lived experience to ensure the plan identifies and sets out steps for the delivery of longer-term priorities and ambitions for supporting victims, tackling perpetrators and the prevention of abuse, including through the commissioning of services. |
| Addressing the particular needs of children and young persons | The plan must set out any steps that the ICB proposes to take to address the particular needs of children and young persons under the age of 25. | This could include using data and gathering insights to ensure the plan identifies and sets steps for delivery of the longer-term priorities and ambitions for the ICBs population of children, young people and families. |
Other content
Workforce
Evidence-based, integrated, inclusive workforce plans that ensure the right workforce with the right skills is in the right place to deliver operational priorities aligned to finance and activity plans.
ICBs will be key to delivery of the Long Term Workforce Plan.
Performance
Specific performance ambitions with trajectories and milestones that align with NHS operational plan submissions and pay due regard to the ambitions of the NHS Long Term Plan, as appropriate.
Digital/data
Steps to increase digital maturity and ensure a core level of infrastructure, digitisation and skills.
These actions should contribute to meeting the ambition of a digitised, interoperable and connected health and care system as a key enabler to deliver more effective, integrated care.
This could include reducing digital inequity and inequalities and supporting net zero objectives.
Estates
Steps to create stronger, greener, smarter, better, fairer health and care infrastructure together with efficient use of resources and capital to deliver them.
This should align with and be incorporated within forthcoming ICS infrastructure strategies.
Procurement/ supply chain
Plans to deliver procurement to maximise efficiency and ensure aggregation of spend, demonstrating delivery of best value.
This could include governance and development of supporting technology and data infrastructure to align or ensure interoperability with procurement systems throughout the ICS.
Population health management
The approach to supporting implementation of more preventative and personalised care models driven through data and analytical techniques such as population segmentation and financial demand modelling.
This could include developing approaches to:
- better understand and anticipate population needs and outcomes (including health inequalities)
- using population health management approaches to understand future demand and financial risk
- support redesign of integrated service models based on the needs of different groups
- putting in place the underpinning infrastructure and capability to support these approaches
System development
How the system organises itself and develops to support delivery. This could include:
- governance
- role of place
- role of provider collaboratives
- clinical and care professional leadership
- leadership and system organisational development
Supporting wider social and economic development
How the ICB and NHS providers will support the development and delivery of local strategies to influence the social, environmental and economic factors that impact on health and wellbeing.
This could include their role as strategic partners to local authorities and others within their system, as well as their direct contribution as planners, commissioners and providers of health services and as anchor institutions within their communities.
References
- The ICBs partner NHS trusts and foundation trusts are named in its constitution.
- People who are registered with a GP practice associated with the ICB, or unregistered patients who usually reside in the ICB’s area (as described in the ICB constitution).
- For the purposes of this guidance, universal NHS commitments are those described in the annual NHS priorities and operational planning guidance and NHS Long Term Plan.
- This includes the National Health Service Act 2006 and the requirements of the Public Sector Equality Duty, section 149 of the Equality Act 2010.
- Further details are provided in Guidance on the Preparation of Integrated Care Strategies (Department of Health and Social Care, 2023)
- Which may be through HWBs.
- This relates to the general duty of ICBs to involve the public (s14Z45 of the NHS Act 2006), the duty of NHS trusts to involve the public (s242 of the NHS Act 2006) and the ICB duty to consult with the public and other relevant persons when developing the JFP (s14Z54 of the NHS Act 2006).
- See guidance on adult social care principles for ICPs; this advises on how ICPs and adult social care providers should work together.
- This includes the full breadth of primary care services, including general practice, community pharmacy, optometry and dental services.
- See also Cabinet Office guidance on consultation principles and Local authority health scrutiny guidance (which provides guidance on service reconfigurations and scrutiny by health overview and scrutiny committees).
- A joint local health and wellbeing strategy (JLHWS) is defined as a strategy under section 116A of the Local Government and Public Involvement in Health Act 2007, as amended by the Health and Care Act 2022.
- We may discuss this opinion with the ICB and its partner NHS trusts and foundation trusts.
- In some systems, HWBs’ geography is coterminous (or nearly coterminous) with the system footprint and therefore the relationships may be different.
- This duty relates specifically to persons mentioned in section 1F(1) National Health Service Act 2006. They are “persons who are employed, or who are considering becoming employed, in an activity which involves or is connected with the provision of services as part of the health service in England”.
- HEE merged with NHS England in April 2023.

