This a practical guide for hospital tobacco dependence teams (TDTs) and hospital pharmacy teams on how to refer patients at discharge into the community pharmacy NHS Smoking Cessation Service (SCS). The guide should be read in conjunction with the community pharmacy advanced service specification.
If you are a community pharmacist intending to provide the service, please read this guidance to help understand the referral process and patient experience when they access the SCS. For the rest of the community pharmacy team, this document provides practical guidance that should help you in the successful provision of the SCS.
The NHS long term plan focuses on the importance of preventing avoidable illness and more active management of the health of the population. Treating tobacco dependence is specifically identified as a key service that can improve the prevention of avoidable illness. It suggests that existing tobacco dependency services can be redesigned to better support patients who are looking to quit smoking as well as those affected by second-hand smoke.
Smoking-related illness puts a considerable strain on NHS resources. In 2015/16 474,000 hospital admissions and 79,000 deaths were caused by smoking.
It is estimated that smoking has cost the NHS in England £2.6 billion per year.
Tobacco dependency services currently exist in primary care, and community and mental health care services. The NHS long term plan also commits to providing NHS-funded tobacco treatment to all patients admitted to hospital and pregnant women by 2023/24.
This service builds on the successful findings of the Pharmacy Integration Fund community pharmacy NHS Smoking Cessation Transfer of Care (SCTC) pilot and aims to create capacity in primary care with a service commissioned through community pharmacy that supports the transfer of care following hospital discharge.
Part A – for both NHS trust tobacco dependency and NHS trust pharmacy teams
The following sections cover:
- an overview of the community pharmacy NHS Smoking Cessation Service
- getting started
- how to provide the service.
It is important that all staff involved in treating patients for tobacco dependency in hospital have read and are familiar with the content of Part A.
Aims of the service
The SCS will provide a care pathway for patients who wish to continue their tobacco dependence treatment in community pharmacy after discharge from hospital.
Community pharmacy has a proven track record of delivering successful tobacco dependency services and this pathway will improve access to this support in primary care.
Providing a bridge between primary and secondary care will reduce smoking-related harm by helping people to stop smoking, reduce the risk of harm to friends, family and the wider community from second-hand smoke by reducing levels of smoking, and promote healthy behaviours in people using the service.
This collaborative approach will improve working relationships between primary and secondary care providers and reduce morbidity and mortality from smoking, and reduce health inequalities associated with higher rates of smoking.
Service description
Inpatients who start a stop smoking attempt in hospital will be able to be referred to a community pharmacy to continue their stop smoking journey once they are discharged.
People can choose the community pharmacy to which they wish to be referred.
A pharmacist will meet with the person stopping smoking or carry out consultations over the phone to discuss their quit progress for up to 12 weeks. They will review the nicotine replacement therapy (NRT) prescribed by the hospital team and make any necessary adjustments to support the continued quit attempt and provide ongoing supplies free of charge as required.
Where appropriate, people will be referred from hospital to community pharmacy using an electronic referral system. This will be determined by the hospital pharmacy discharge process and may vary between hospitals.
Inclusion criteria
- people aged 18 years and older who have started treatment for tobacco dependence in hospital and have chosen to continue their treatment in community pharmacy after discharge
- this service does not exclude women who are pregnant or people who suffer from non-complex mental health problems, although local arrangements may already be in place to direct such people to these alternative services.
Exclusion criteria
- people who are unable to give consent to participate
- people who choose not to use community pharmacy to continue their tobacco dependency programme after discharge
- children and adolescents under the age of 18 years
- people with complex mental health problems. These people will be encouraged by the hospital smoking team to receive follow-up care from specialist tobacco dependency advisors in the community
- people who have completed a 12-week tobacco dependency programme prior to discharge (as a result of an extended duration in hospital as an inpatient).
The model of care
Hospital trusts will identify people who are smokers, provide a pre-quit assessment and start treatment. With consent, patients will be offered referral to a participating community pharmacy. The referral will be made using an electronic system following or in preparation for discharge from hospital. The patient will choose the community pharmacy to which they wish to be referred.
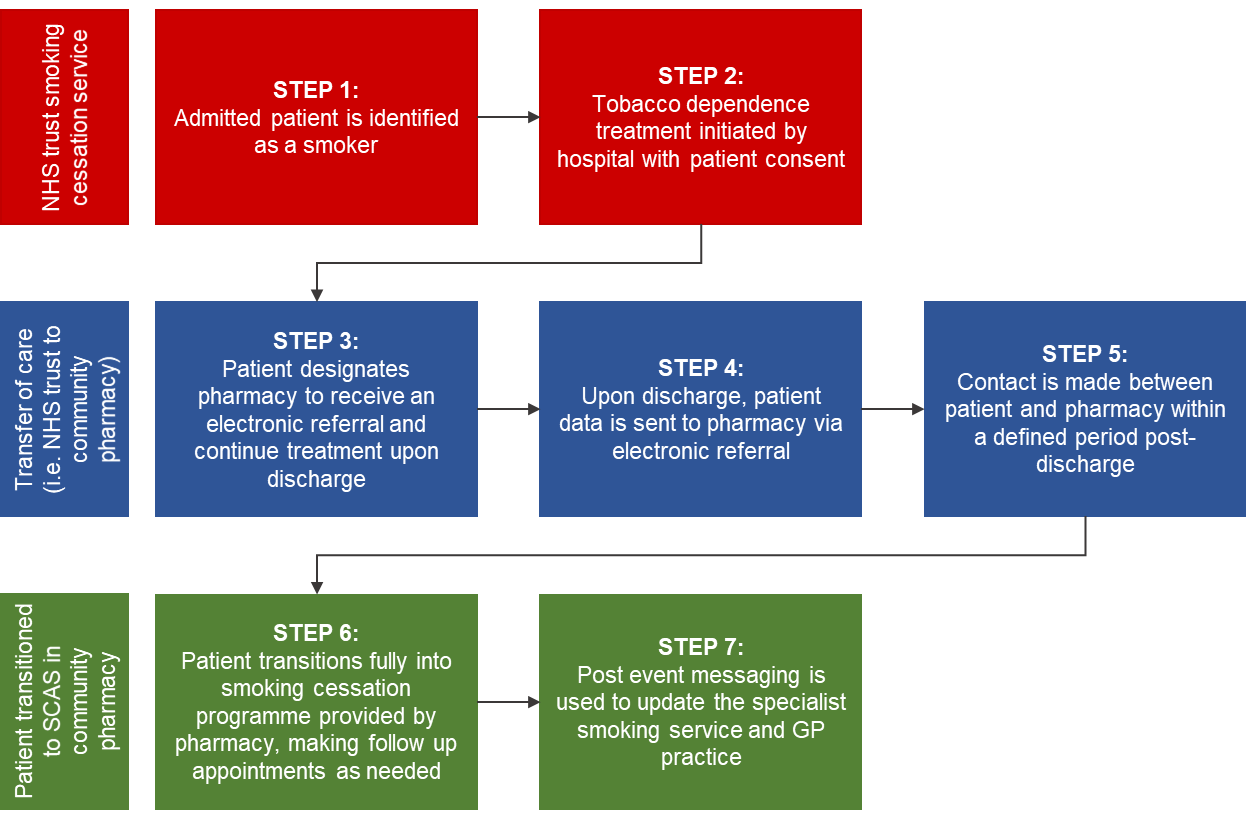
The referral notice will include a description of the items, quantities supplied to support tobacco dependency and a quit date where established (see Appendix B). The community pharmacy will complete step 5, 6 and 7 as described in Figure 1.
Figure 1: The community pharmacy SCS model of care
Figure 1 accessible text:
NHS trusts smoking cessation service:
- Step1: Admitted patient is identified as a smoker.
- Step 2: Tobacco dependence treatment initiated by hospital with patient consent.
Transfer of care (ie NHS trust to community pharmacy)
- Step 3: patient designates pharmacy to receive an electronic referral and continue treatment upon discharge.
- Step 4: Upon discharge, patient data is sent to pharmacy via electronic referral.
- Step 5: Contact is made between patient and pharmacy within a defined period post-discharge.
Patient transitioned to SCAS in community pharmacy
- Step 6: Patient transitions fully into smoking cessation programme provided by pharmacy, making follow up appointments as needed.
- Step 7: Post event messaging is used to update the specialist smoking service and GP practice.
While in hospital
During the process of admission to hospital, the smoking status of the patient will be captured and if identified as a smoker the tobacco dependency team (TDT) will be notified via the hospital clinical system.
It is expected that a patient identified as a smoker will be contacted by the TDT within 48 hours of admission to carry out a pre-quit assessment with an offer of tobacco dependence treatment and support.
A patient accepting treatment and support during their hospital stay should then be offered referral to a community-based service of their choice. It may be preferable for the patient to continue their tobacco dependence treatment and support from a community pharmacy providing the SCS. The accessibility of and familiarity with community pharmacy have been shown in the pilot areas to be important factors in making that choice.
Making a referral
The referral sent to the community pharmacy must include the minimum dataset described in Appendix B.
This referral will be made by the TDT. In some cases the referral process may be undertaken by the hospital pharmacy team on behalf of the TDT with the expectation that the referral will be made on the day of discharge (or very soon after). The patient will receive up to 14 days’ supply of NRT on discharge from hospital. This is to enable the individual to bridge the potential gap in smoking support during transfer to community pharmacy.
Following discharge into the NHS Smoking Cessation Service (SCS)
Following receipt of the referral, community pharmacy staff will contact the patient within five working days to confirm an appointment. The community pharmacy will attempt to contact the patient at least three times (the last of which must be on the fifth working day following receipt of referral) before closing the referral if the patient does not respond.
The pharmacy should give people who wish to decline further support after referral or do not wish to stop smoking at this time details of alternative tobacco dependency services for use should they wish to seek support in the future. Where disclosed by the patient, the reason for not continuing should be captured in the clinical record for the service before the referral is closed.
The community pharmacy should notify the NHS trust TDT when patients who are referred either are not contactable or decline the service when contacted and the referral is closed.
The quit date where established will be communicated to the community pharmacy as part of the referral dataset (Appendix B). This may be the date the patient has engaged with the service in hospital or date of discharge.
People who wish to continue their tobacco dependency programme will be offered behavioural support appropriate to their needs. The pharmacy will also supply a maximum of two weeks’ NRT at a time with no charge to the patient. The course length may not exceed 12 weeks of treatment from the defined quit date. This may include NRT supplied to the patient while in hospital and at the point of discharge.
People who have completed their 12-week tobacco dependency programme during an extended stay in hospital but are at risk of relapse should be given details of alternative community-based stop smoking services that can support their continued treatment. These patients should not be referred to the SCS.
The SCS includes the ongoing provision of both behavioural support and the supply of NRT. There is no ‘supply only’ option as part of this service.
At each consultation self-reported abstinence is checked, where possible, using carbon monoxide (CO) monitoring. A successful quit attempt is defined as a CO test reading of less than 10 parts per million (ppm) four weeks after the quit date. This does not imply that treatment should stop at four weeks (NICE 2018, Stop smoking interventions and services).
If a CO test cannot be carried out due to the consultation being remote or being declined by the patient, this will be noted by the pharmacist along with the self-reported smoking status.
If a patient does not continue with the service up to their four-week planned review, the pharmacy should seek to re-engage them and continue the service.
Ongoing support will be provided for individuals who succeed with their four-week quit attempt for up to 12 weeks from their quit date.
Getting started with the service
Notification of readiness to make referrals into the NHS Smoking Cessation Service (SCS)
It is important that NHS trusts preparing to implement their TDT service to include referrals to community pharmacy through the SCS notify the SCS National Implementation Support team by emailing mlcsu.scs@nhs.net and contact their local pharmaceutical committee (LPC) so that the service is introduced in a co-ordinated way.
Contact details can be found on the Future NHS smoking cessation page (this page requires a log in).
National implementation support is in place to connect NHS trusts and community pharmacy to maximise the opportunities to support smokers at discharge through the SCS.
It is important that NHS trusts preparing to implement their TDT service to include referrals to community pharmacy through the SCS notify the SCS National Implementation Support team by emailing mlcsu.scs@nhs.net and contact their local pharmaceutical committee (LPC) so that the service is introduced in a co-ordinated way.
Contact details can be found on the Future NHS smoking cessation page (this page requires a log in).
National implementation support is in place to connect NHS trusts and community pharmacy to maximise the opportunities to support smokers at discharge through the SCS.
What do I need to do to get ready to refer patients into the SCS?
It is important that you start by familiarising yourself with the service as this will provide you with a complete overview of what providing the service entails.
You will need to consider the following:
- contact the SCS National Implementation Support team (who will have previously been in contact with the NHS trust). To contact the SCS National Implementation Support team, please email mlcsu.scs@nhs.net
- familiarise yourself with the existing locally agreed smoking cessation pathways
- collaboration with colleagues including community pharmacy contractors via the LPC and locally commissioned community-based services
- use of an existing referral management system or introduction of a referral management system to enable referral to SCS
- any additional training needs for the hospital TDT to support the referral process.
How do I know which pharmacies offer SCS?
The SCS National Implementation Support Team will provide a regularly updated list of community pharmacies in your area that are registered to receive referrals into SCS.
Details of registered pharmacies will also be available via the Future NHS smoking cessation page.
What equipment will be used in the community pharmacy?
Community pharmacies will be using CO monitoring equipment to support quit attempts (specification for this equipment is detailed in the SCS service specification).
How do I manage referrals into SCS?
You will need to have access to a digital referral platform, which will send the required dataset to community pharmacies.
The NHS trust may choose to add the SCS to an existing referral management system or introduce a standalone referral management system.
The expected minimum digital requirement is an NHSmail to a community pharmacy NHSmail shared mailbox to ensure a secure electronic message can be sent. Details of NHSmail addresses for participating pharmacies will be provided by the SCS National Implementation Support Team or where agreed locally via the LPC.
How do I know if a referral has been successful?
If using NHSmail a read receipt option is available and can be requested. If the referral is made using a digital platform, this should provide a ‘receipt’ or ‘acknowledgement’ when the referral message is received.
The community pharmacy teams will regularly check for any referrals and, depending on the system used, may be actively alerted to them.
As part of business as usual processes the community pharmacy team will regularly check the pharmacy NHSmail shared mailbox.
Requirements for service provision
Full details of the requirements that pharmacies registered for the service must meet before and while they provide the SCS are provided in the service specification.
Important points for the hospital TDT to note include:
- The service must be provided by a pharmacist meeting the training requirements, and community pharmacy contractors must ensure relevant members of the pharmacy team, including locums and relief pharmacists, have access to and know how to use the electronic referral system, NHSmail and the NHS Summary Care Record (SCR), and can provide the service competently.
- Consultations with the patient must take place in the pharmacy consultation room or can be carried out remotely if the patient and the pharmacist agree this is suitable.
- Pharmacists should be aware of locally commissioned smoking cessation services to enable signposting.
- The service must not be used to divert or attempt to change the patient’s use of their usual community pharmacy.
Service availability
Tobacco dependency support services should be available to patients throughout their stay in hospital and referrals requested to be made to a community pharmacy should be made by either the trust’s TDT (or an alternative referral manager) or the trust’s pharmacy team as determined clinically appropriate by the trust. NHS trust processes will determine when referrals are made. Ideally this will be at the earliest appropriate opportunity prior to or after discharge.
Community pharmacy teams should be offering this service during their core opening hours. After the referral the pharmacy will agree with the patient the date and time of their first appointment and then subsequent appointments.
Please refer to your local pathway for details of pharmacies offering the service (Future NHS Smoking Cessation Page).
Opening hours for these pharmacies can be found on www.nhs.uk
Service promotion
The hospital trust will be responsible for informing patients and encouraging referrals into the SCS. The SCS National Implementation Support Team can support this by providing promotional material, eg patient leaflets and TV monitor advert cards.
This service is specifically for people referred from secondary care who choose to continue their tobacco dependence treatment in community pharmacy following discharge from hospital. It provides behavioural support and choice of NRT individual to their needs free of charge.
Patients presenting at the pharmacy without a digital referral into the SCS are not eligible for the service and should be treated in the same way as other patients who present directly at the pharmacy. It is a requirement of the SCS provider that pharmacists are aware of other locally commissioned smoking cessation services to enable signposting.
Part B – for trust-based tobacco dependency teams
This part of the guidance provides more detail specifically for trust-based TDTs looking to implement referral to community pharmacies registered for the SCS.
A regularly updated list will be available through the following routes:
- SCS National Implementation Support team (mlcsu.scs@nhs.net)
- Future NHS smoking cessation page (this page requires a log in)
- NHS England regional pharmacy contracting team.
Trusts will be able to use this national list of pharmacies, which includes postcodes to help patients choose a pharmacy. The full list of all pharmacies across England will be available to all NHS trusts to support patient choice. This may be useful when the patient lives outside the integrated care system for the hospital and wishes to receive follow-up near their home.
Each pharmacy will have a shared NHSmail email address (which must be in the following format: ODScode@nhs.net).
This email is either the back-up to the electronic referral system or the primary means of referral, depending on the NHS trust.
It is important that NHS trusts preparing to implement their TDT service to include referrals to community pharmacy through the SCS notify the SCS National Implementation Support Team by emailing mlcsu.scs@nhs.net and contact their local pharmaceutical committee (LPC) so that the service is introduced in a co-ordinated way.
Contact details can be found at: Future NHS Smoking Cessation Page.
National implementation support is in place to connect NHS trusts and community pharmacy to maximise the opportunities to support smokers at discharge through the SCS.
How should I involve my tobacco dependency team?
This service has been commissioned to add capacity and improve choice, accessibility and the support available for patients wishing to continue with their quit attempt when they are discharged from hospital.
It is always easier to provide any new service if the full team are aware of what is being introduced and know how the service will operate. You may want to consider:
- holding a briefing session for your team
- providing them with the one-page overview on how the service will work (Appendix A)
- discussing as a team how you can work collectively to make the service a success
- making sure team members are clear on the daily activity required, such as managing referrals.
How do we contact a pharmacy and how will they contact the TDT if required?
If contact is needed between the hospital TDT and the pharmacy after discharge and the referral has been sent, then the pharmacy shared NHSmail email address or the pharmacy contact telephone number should be used depending on urgency.
Contact telephone numbers are included as part of the list of registered pharmacies or can be obtained through www.nhs.uk.
In the event of a query from the pharmacy, a monitored email address for the TDT or contact number should be available as part of the local service communication arrangements.
Governance
As part of their NHS trust governance requirements, both the hospital pharmacy and TDT will be required to report any incidents related to patient safety, near misses and the referral process, or operational issues in relation to this service.
In the instance an NHS trust pharmacy team or the TDT receives a complaint about the referral to or service provided by community pharmacy, this should be reported to the local NHS England pharmacy contracting commissioning team within 24 hours. Contact details will be provided through the SCS National Implementation Support Team. Also refer to the trust’s internal policy.
For information, community pharmacies providing the SCS will be required to report any complaints about the service, untoward incidents including violence and aggression towards pharmacy staff, and customer falls to the local NHS England primary care commissioning team within 24 hours.
As detailed in the SCS service specification, the community pharmacy will record details of the consultations carried out, including NRT supplied and CO monitoring when it takes place.
Pharmacists will seek appropriate consent from patients to the data sharing, including notifications to their GP and a summary report of the outcomes of the service provision sent to the referring NHS trust. See Appendices D and E of the SCS service specification.
Part C – Role of hospital pharmacy teams
The role of the hospital pharmacy team to support the SCS is complementary to the role of the trust-based TDT. There should be no duplication of activity to gain agreement for referral to community pharmacy. It is therefore important that the hospital pharmacy team and TDT fully understand their roles in supporting patients who wish to continue with support to quit smoking once they are discharged.
The expectation is that hospital pharmacy teams will:
- Support the offer of community pharmacy as first option for referral.
- Confirm that the community pharmacy receiving the referral will provide the ongoing tobacco dependency support and NRT.
- Be available to provide NRT-related advice to patients enrolled in the hospital tobacco dependence programme.
- Where indicated by the hospital TDT, the hospital pharmacy team will follow-up with the patient to encourage continuation of their programme.
- Confirm patient participation in the SCS when sending information about any NRT supplied, along with any other medicines, at discharge to the patient’s preferred pharmacy for the discharge medicines service (DMS).
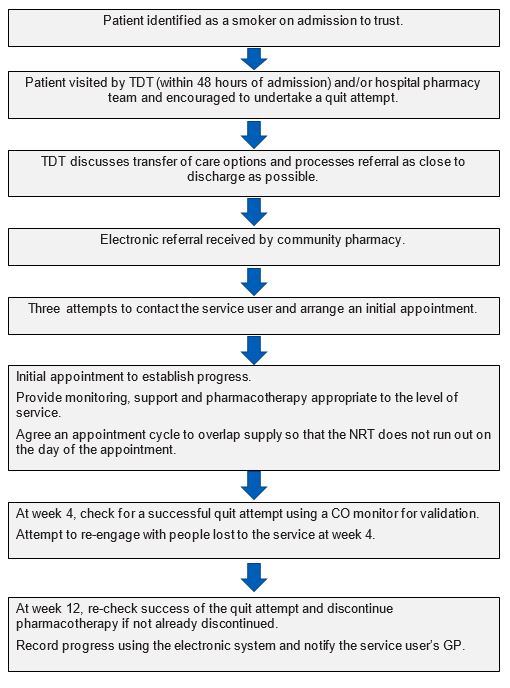
Appendix A – Service overview
- Patient identified as a smoker on admission to the trust.
- Patient visited by TDT (within 48 hours of admission) and/or hospital pharmacy team and encouraged to undertake a quit attempt.
- TDT discusses transfer of care options and processes referral as close to discharge as possible.
- Electronic referral received by community pharmacy.
- Three attempts to contact the service user and arrange an initial appointment.
- Initial appointment to establish progress. Provide monitoring, support and pharmacotherapy appropriate to the level of service. Agree an appointment cycle to overlap supply so that the NRT does not run out on the day of the appointment.
- At week 4, check for a successful quit attempt using a CO monitor for validation. Attempt to re-engage with people lost to the service at week 4.
- At week 12, re-check success of the quit attempt and discontinue pharmacotherapy if not already discontinued. Record progress using the electronic system and notify the service user’s GP.
Appendix B – Dataset for transfer from NHS trusts to pharmacies
- Name
- NHS number
- Date of birth
- Gender
- Address
- Postcode
- Telephone number(s)
- Ethnic group
- Reason for hospital admission
- Quit date
- NRT 1 supplied on discharge
- Quantity of NRT 1 (days)
- NRT 2 supplied on discharge
- Quantity of NRT 2 (days)
- GP practice identifier – where patient is registered
- Contact details of the referring tobacco dependency team
- NHS trust ODS code
- Notes including any Fagestrom score and adverse drug reaction.
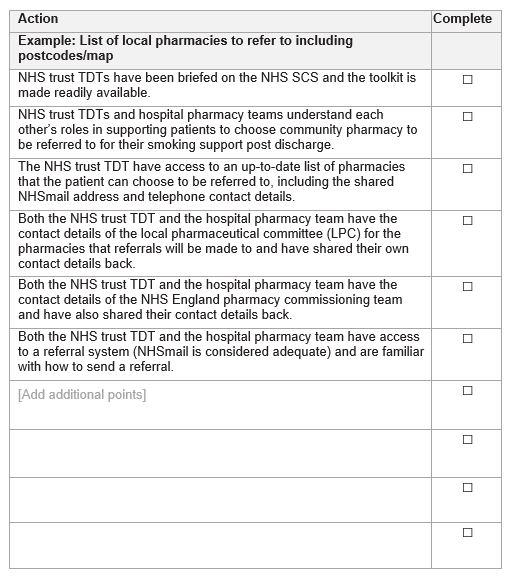
Appendix C – Implementation checklist for NHS trusts
Download the above checklist as a word document.
Appendix D – Patient flow
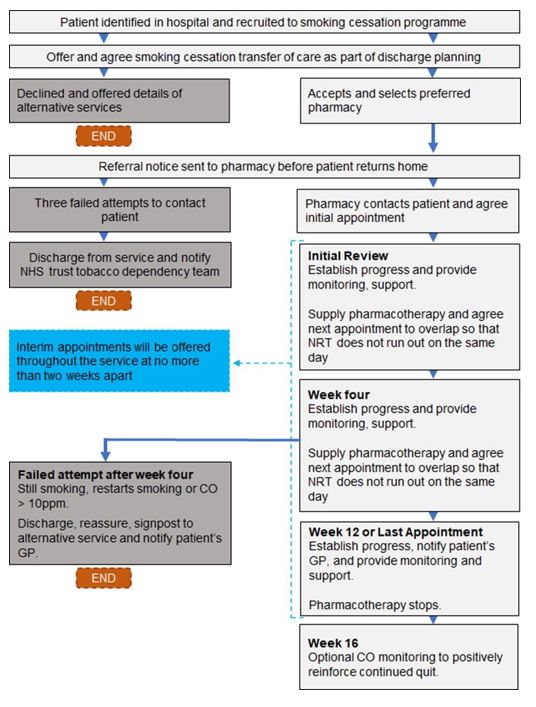
Accessible text:
- Patient identified as a smoker on admission to the trust.
- Patient visited by TDT (within 48 hours of admission) and/or hospital pharmacy team and encouraged to undertake a quit attempt.
- TDT discusses transfer of care options and processes referral as close to discharge as possible.
- Electronic referral received by community pharmacy.
- Three attempts to contact the service user and arrange an initial appointment.
- Initial appointment to establish progress. Provide monitoring, support and pharmacotherapy appropriate to the level of service. Agree an appointment cycle to overlap supply so that the NRT does not run out on the day of the appointment.
- At week 4, check for a successful quit attempt using a CO monitor for validation. Attempt to re-engage with people lost to the service at week 4.
- At week 12, re-check success of the quit attempt and discontinue pharmacotherapy if not already discontinued. Record progress using the electronic system and notify the service user’s GP.
Appendix E – Dataset to be shared with the NHS trust tobacco dependency team
PRIVATE & CONFIDENTIAL
Tobacco Dependency Team Pharmacy Name
NHS Trust Name Practitioner Name
NHS Trust Address Direct Line
NHS Trust Postcode Email
Our Ref: Insert
Date: Today’s Date
Dear Tobacco Dependency Team
RE: Pt name, Pt Address Date of Birth
Hospital Number
Ptname was identified as a smoker and was offered behavioural support and stop smoking medication whilst an inpatient at the XXXX Hospital.
Upon discharge Ptname was referred to this Pharmacy for ongoing support with their quit attempt.
Please update your records with the following: (select the applicable response)
- Ptname advised that they did not want to participate in the service/did not want to stop smoking at this stage.
- Ptname was not contactable/did not attend their appointment.
- Ptname has been supplied Nicotine Replacement Therapy (NRT) to support their quit attempt.
- Ptname has recorded a successful 4 week quit attempt.
- Ptname has recorded a successful 12 week quit attempt.
Ptname has been successful / unsuccessful with their quit attempt and discharged from the service.
Download the above template as a word document.
Publications approval number: PR1704