Executive summary and action required
NHS England and integrated care boards (ICBs) have a legal duty to have due regard to the need to reduce inequalities between persons with respect to their ability to access health services and the outcomes achieved by the provision of health services. This paper outlines the progress and impact of NHS England’s Healthcare Inequalities Improvement Programme and the NHS Race and Health Observatory in 2024/25 and plans for the current period of change and transition across the NHS.
The Board is asked to:
- Note that this report concludes Professor Bola Owolabi CBE’s tenure as Director of the NHS England Healthcare Inequalities Improvement Programme and the programme now welcomes the appointment of Dr. Dianne Addei as SRO.
- Note the progress of the Healthcare Inequalities Improvement Programme during 24/25, notably further embedding the overall strategic framework via the Core20PLUS5 approach, progressing delivery against the five strategic priorities, maintaining a robust delivery network, ensuring each frontline organisation has a clear plan to address inequalities, against which it is starting to deliver.
- Endorse the development of our respective work including a strong focus on measurable progress in reducing health inequalities with metrics, indicators, data and evidence, particularly as we begin to support implementation of the health inequalities ambitions in the government’s 10 Year Health Plan.
- Note the work of, and progress made by, the NHS Race and Health Observatory in identifying and tackling ethnic and racial inequalities in health and healthcare – including its partnership work with NHS England.
- Endorse the Observatory’s strategic approach for 2025-27, including the expansion of its work programme to include workforce equality (including race and other protected characteristics), and its role in supporting implementation of the 10 Year Health Plan in the period beyond its current contract
Background and context
1. The NHS continues to have a crucial role to play in reducing healthcare inequalities as well as addressing the ‘biggest killers’ for the most underserved population groups. It can do this by tackling inequalities in access to, experiences of, and outcomes from, healthcare delivery – healthcare inequalities.
2. We also play a vital role in supporting the government’s Health Mission and twin aims of halving the healthy life expectancy gap between the richest and poorest regions in England and boosting economic growth:
3. The NHS Race and Health Observatory has, in this past period, made significant progress in making evidence on inequalities relevant to change-makers and decision-makers; in championing new approaches to community participation, working internationally to develop and spread good practice; and in supporting the implementation of effective interventions – working in partnership with providers, patients, and the public.
4. The Observatory has worked closely with ministers, policymakers and communities to support the development of the 10 Year Health Plan and is specifically delivering a work programme that supports implementation of the Plan, including the delivery in areas such as vaccination uptake and supporting the revision of the Mental Health Act. It also continues its international work with the US CDC as part of the UK-US government agreement and is also involved in the planned UK-Brazil government agreement, that also includes tackling racial inequalities in healthcare.
Key programme achievements in 2024/25
5. The NHS England Healthcare Inequalities Improvement Programme has an important role in implementing the health inequalities ambitions in the government’s 10 Year Health Plan, putting policy into practice. It does this through setting direction on healthcare inequalities for the healthcare system; evidence and data led action to facilitate healthcare inequalities improvement; and targeted implementation support for systems.
Setting direction
6. We have informed relevant national guidance and developed national resources to guide system action on addressing inequalities including:
- The Director of the National Healthcare Inequalities Improvement Programme was tasked by the Secretary of State (SoS) for Health & Social Care to Co-Chair vision workstream 4 of the Ten-Year Health Plan: ” I am treated fairly and inclusively, irrespective of who I am”. The Co-Chairs’ report was submitted in December 2024. We also received and responded to multiple policy commissions to provide ministerial advice for the Ten-Year Health Plan.
- Ensuring that healthcare inequalities featured strongly in the Elective Recovery Reform Plan. We are now working with the Elective Programme team to support delivery of the specific health inequalities commitments set out in the Plan.
- We have developed a community languages and translation improvement framework for action and delivered a launch webinar in June 2025. The Framework is designed to support the provision of consistent, high-quality community language translation and interpreting services by the NHS to people with limited English proficiency.
- The Patient Safety Healthcare Inequalities Reduction Framework has been published, setting out principles to reduce patient safety healthcare inequalities in the NHS.
- Health inequalities objectives remain in NHS priorities and operational planning guidance for 25/26.
- We successfully ran and concluded an open market procurement exercise for a host organisation for the NHS Race and Health Observatory.
- We have responded to multiple committee briefing requests including: health inequalities and CVD; older people; dental inequalities; and the Health and Social Care Committee evidence session on inequalities in black maternal health.
- Having supported the development of proposals to the Treasury to fund the health and growth accelerator sites, we continue to hardwire healthcare inequalities improvement into the delivery and evaluation of this work contributing to the government’s economic growth mission.
Evidence and data led improvement
7. We are committed to delivering a data led approach to programme delivery, monitoring the impact of interventions on healthcare inequalities through data and evaluation. We have:
- Agreed and developed metrics for measuring healthcare inequalities for the 5 key Core20PUS5 clinical programmes for adults which will be available to track via the NHS England Performance Oversight Dashboard (POD) and reported regularly to execs. This will allow us to demonstrate measurable improvements and understand geographic variation in deprivation and ethnicity-based inequalities in access and outcomes for our clinical priority areas. Work to develop healthcare inequalities metrics across the Core20PLUS5 areas for children and young people (CYP), and further metrics for adults (including disaggregation of urgent and emergency care and elective data), has progressed, navigating ongoing resource constraints.
- Embedded 6 health inequalities contextual (non-scored) metrics in the NHS Oversight Framework for 2025/26 (appendix 1).
- We have finalised a plan for improving the quality of ethnicity data in health datasets with outputs. We have worked with the Chief Data Architect’s office to support the publication of guidance to support the uptake of modernised 2021 Census codes for new data products, in line with Government Statistical Service guidance, and are working in collaboration with the Transformation Directorate to support the development of a single point of collection for ethnicity data.
- We have delivered the first year of the longitudinal evaluation of the Core20PLUS5 approach with The Strategy Unit, including scoping interviews and report, workforce survey with IPSOS Mori, and 13 in-depth qualitative case studies with ICBs. Initial scoping report themes can be found in appendix 2.
Implementation support
8. We are enhancing system capability to address healthcare inequalities through strategic partnerships, learning networks for change and products tools and resources to solve common problems. This includes:
- Significant investment to improve access to urgent care, patient experience, and outcomes for people with Sickle Cell Disorder (PwSCD), we have improved provision of digital care plans for all PwSCD, enabling delivery of personalised care; provided training programmes on a national platform and launching the ACT NOW campaign.
- Making gene-editing therapy available on the NHS for people living with the most severe forms of SCD and Thalassemia Major, working with NHS England’s Complex Medicines Negotiation team, NICE and stakeholders including the Sickle Cell Society. This is a first in Europe. Blood transfusions for the patient group are being made safer by the implementation of a blood genotyping programme which will allow the detection of previously undetectable anti-bodies which could cause complications. Gene therapy Exa-gel is to be made available for persons both with sickle cell, and thalassaemia.
- Supporting the launch of the Coastal Navigators Network prospectus a collaboration between NHS England and six coastal Integrated Care Boards—brings together learning, data, and innovation showcasing scalable interventions that tackle the root causes of poor health and economic exclusion.
- Ongoing Health Innovation Network delivery of the Innovation for Healthcare Inequalities Programme (InHIP) with an impact and learning report published in December 2024, ensuring the newest NICE approved innovations reach underserved population groups.
- Delivery of a series of Health literacy webinars, and the launch of the Making Every Contact Count (MECC) ‘how to guide’.
- Working in partnership with OHID to support development and testing of a self-assessment Inclusion Health tool, to support implementation of our Inclusion Health Framework.
- A report developed by Pathway and part funded by NHS England was published in June 2025, offering recommendations to local health systems and national bodies on further action required on inclusion health.
- We supported development of the Good Things Foundation digital trusts and beliefs report and supporting leaflet.
- We have facilitated a series of networks for change, for example, during the year we launched the alumni programme for the Core20PLUS Ambassadors and Cohort 3 of the programme involved 680 ambassadors; the Core20PLUS Connectors programme involved every ICS across the lifespan of the programme; the Core20PLUS Collaborative hosted the Director General of the Ten-Year Health Plan in a deliberative session.
- We have continued to collaborate with HM Prison and Probation Service (HMPPS) to fill the current gap in evidence, raise awareness of health risks, improve health literacy, improve uptake of health services and provide resources to enable regions to effectively support people in non-custodial community settings, an inclusion health group. Recent examples include scoping of a Probation Health Needs Assessment and Core20PLUS5 probation animation and QR coded posters.
NHS Race and Health Observatory
9. Since the Board’s last deep dive into its work, the Observatory has continued to be an active delivery partner, it has:
- Continued to be a source of evidenced intervention and implementation for the NHS, DHSC and parliament, with evidence quoted extensively by the Health and Social Care Select Committee in the interrogation of the 10 Year Plan and included in the DHSCs evidence gathering on the benefits of improving patient experience.
- Developed and delivered a unique Learning and Action Network (LAN) programme with 8 ICSs to tackle inequalities in maternal and neonatal outcomes, using an anti-racism focused Quality Improvement approach. Now under evaluation, learning from the widely cited programme is informing national maternity bundles, the Health and Social Care Committee Black Maternal Health inquiry, and the Maternity Safety Ambitions Refresh, as we prepare to spread and scale the LAN learnings and interventions.
- Developed, as part of the LAN, an anti-racism focused Model for Improvement Quality Improvement approach, as well as adapted the MUSIQ (Model for Understanding Success in Quality) tool using an anti-racism lens.
- Developed resources to improve detection of jaundice in newborn babies and worked with NHS England to roll-out birthing simulators and manikins in different skin tones across all maternity units in England.
- Published work exploring the role of trust in determining Black, Asian, and minority ethnic communities’ access to and experiences of primary care. This has led to discussions with the Secretary of State and the implementation of a programme to rebuild trust with communities, improve access to healthcare and increase productivity.
- Signed a groundbreaking partnership agreement with NICE to de-bias clinical guidance across five identified areas, and to ensure the development of any new clinical guidelines to not have bias embedded within them.
- Formed a new partnership with NHS England, working with the Chief Scientific Officer for England, to tackle the disparities faced by ethnic minority patient groups in access to, and delivery of, the NHS Genomic Medicine Service (GMS).
- Commenced work to tackle inequalities in sickle cell care, including tackling the barriers faced by children and young people living with sickle cell as they transition from NHS paediatric to adult health care providers.
- Produced resources to tackle the challenges faced by marginalised communities, including Gypsy, Roma, and Traveller communities and access mental health care, and meeting the communication needs of Jewish communities.
- Published its ‘7 Principles of Anti-Racism’ to support healthcare organisations design and deliver services in a way that actively tackles race inequity. The principles are being adopted by providers and organisations across the healthcare system, including the Care Quality Commission, and the other the major healthcare regulatory bodies. This will lead to a consistent approach to regulation and accountability for tackling inequalities across the system.
- Supported the government with community engagement on its 10 Year Health Plan consultation and on the forthcoming national cancer plan. This has included hosting roundtables, including with the Secretary of State and ministers – which have been very well-received.
- Presented evidence to the UK Covid-19 Inquiry and contributed significantly to Health and Social Care Select Committees.
- Engaged with ministers and the Secretary of State (HSC) in developing the Observatory’s strategy for 2025-27 ensuring that it supports implementation of the 10 Year Health Plan, outlining key priority areas grouped under the 3 shifts in the way healthcare is delivered: to support the creation of a more efficient, agile, and technologically enabled NHS that will deliver care closer to people and further upstream (appendix 3).
The importance of data
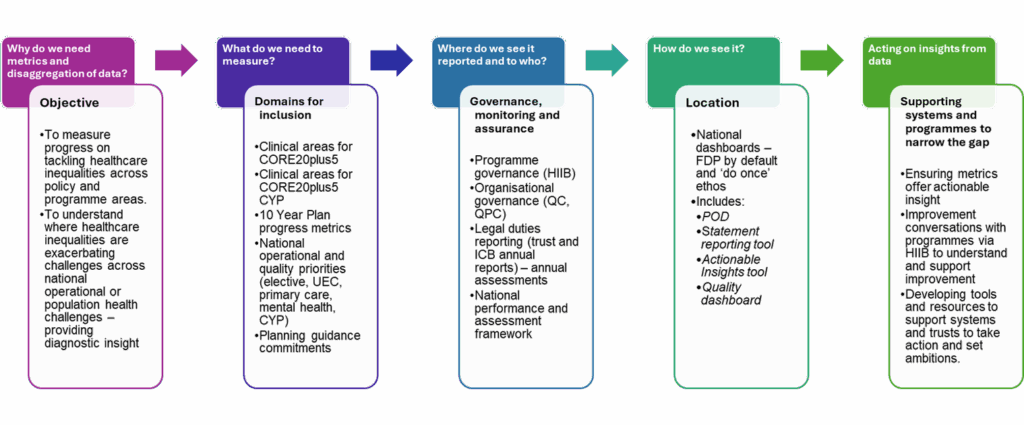
10. To move from general statements of ambition towards a tangible focus on measurable improvements, we have established a health inequalities measurement framework which we have worked to embed across key frameworks and offer a health inequalities lens on key performance, quality and population health challenges.
11. Throughout the period of rapid organisational change, data and evidence must remain a central focus to monitor impact, and to test and evidence what works and ensure that NHS England continues to fulfil legal duties with respect to healthcare inequalities.
12. There is a risk that tackling health inequalities continues to be treated as a long-term ambition rather than a priority area of performance and care quality sensitive to shorter term NHS intervention. There is a risk that the loss of specific health inequalities ambitions and specific measures will disincentivise action on health inequalities in the context of stretched financial resource, and the impact of this on our ability to measure trends and evaluate the NHS’s long-term progress towards equitable access, experience and outcomes. This ultimately increases the risk of health inequalities legal duties not being met and wider issues around patient safety, long term population health outcomes and increased demand and resource utilisation.
13. The publication of the NHS Oversight Framework 2025/26 which incorporates non-scored health inequalities metrics is an important starting point, and further action is required to plan for longer term opportunities to involve scored health inequalities metrics into future iterations of the framework for ICB segmentation and regional accountability mechanisms, in line with the health inequalities ambitions set out in the 10 Year Health Plan.
14. In June, the Observatory launched its new interactive digital platform, the Health Action Resource Platform (HARP). This pioneering platform will support healthcare providers in identifying and tackling health inequalities, including at local levels, based upon ethnicity and deprivation, through the effective use of data, evidence and examples of replicable good practice.
Planned actions for delivery in the next 3-6 months and beyond
NHS England Healthcare Inequalities Improvement Programme
15. During the next 3-6 months we are reviewing programme delivery objectives in response to the 10 Year Health Plan and aim to align our Healthcare Inequalities Strategic Framework narrative to support action on the health inequalities expectations for the NHS set out in the 10 Year Heath Plan:
Priority 1: Neighbourhood Health
a. We aim to inform the development of national guidelines and new contracts to ensure Neighbourhood Health Services systematically address inequalities across care pathways and providers.
Priority 2: Analogue to Digital
b. We plan to inform a systematic approach to addressing digital inclusion and exclusion across the NHS, through implementation of the NHS England digital inclusion framework, working alongside teams responsible for delivery of the NHS App, and Single Patient Record, including an emphasis on AI safety and quality.
c. We will focus on data quality including recording of key risk factors and characteristics, scoping delivery of the social risk assessment commitment within the Ten Year Health Plan.
d. Refine and expand development of a digital inclusion heatmap tool and develop eLearning to support digitally inclusive NHS services.
e. Develop an ethnicity recording self- assessment tool.
Priority 3: Shift from sickness to prevention
f. We will support the equitable shift from sickness to prevention through targeted action for Core20PLUS5 populations, an organisation wide strategic approach to anchor practice, and supporting action on health literacy and patient activation.
g. Support and influence the NHS contribution to the government’s health mission ambition to reduce healthy life expectancy gap between the richest and poorest regions.
Priority 4: Shifting financial resources
h. Addressing systematic disadvantage in funding formulae and allocations.
i. Informing ACRA reviews of the Carr-Hill formula, and incentives (Best practice narratives) 3-year funding allocations and medium-term planning.
j. Influencing contracts and FT regimes, multi neighbourhood providers and integrated health organisations.
k. Identifying contractual levers and influencing their delivery including health inequalities implications for strategic commissioning and new service frameworks.
Priority 5: Transforming accountability and performance
l. Ensure health inequalities considerations are reflected in the NHSE balanced scorecard and support system understanding of the contextual, non-scored health inequalities metrics set out in the NHS Oversight Framework for 2025/26.
m. Work to maintain visibility of healthcare inequalities reporting and monitoring as part of new organisational governance arrangements.
n. Review and refresh the NHSE ‘statement on information on health inequalities’ to strengthen it further as a lever for data-led improvement.
o. Commence year 2 of the longitudinal evaluation of Core20PLUS5 and finalise the qualitative report and insights.
Priority 6: Sickle Cell Programme Delivery
p. Delivery of the Sickle Cell and Thalassaemia programme, including implementation of recommendations outlined in the Infected Blood Inquiry.
q. Sickle cell disease: expand digital care plans and stand-up community accelerator sites for sickle cell disease.
r. Begin development of RSPH modules for level 2 accredited programme aimed at community leaders / lay people to develop their understanding of the principles of promoting health and wellbeing, the importance of effective communication and the impact of behaviour change
NHS Race and Health Observatory
16. In the coming period, the NHS Race and Health Observatory will continue to be a key delivery partner to the Department of Health and Social Care and NHS England – supporting the implementation of the 10 Year Health Plan by ensuring that the 3 shifts to the way healthcare is delivered benefit all communities equitably. This will include:
- Operationalise its 2025-27 strategy, including new programmes that will oversee tackling inequalities in dementia screening; improving access to perinatal mental health for ethnic minority communities; tackling the ethnicity pay and progression gap in the NHS workforce, and tackling bullying and harassment amongst staff in a way that will lead to improved workforce engagement and increased productivity.
- Continue to facilitate the convening of the major healthcare regulatory bodies to develop a collaborative and aligned approach in tackling inequalities, including those related to the NHS workforce.
- Progress our impactful programmes on developing evidence-based resources to support implementation of the forthcoming Mental Health Act, as well as work on familial hypercholesterolemia; the impact of Long-COVID on the NHS workforce, and the scale and spread of its Learning and Action Network for tackling ethnic and racial disparities in maternal and neonatal health.
- Outline and support the scale and spread of the Observatory’s Learning Action Network to tackle ethnic inequalities in maternal and neonatal outcomes.
- Support the healthcare system by continuing our work on impactful implementation of evidence-based interventions to close inequality gaps, including through the spread of the Observatory’s implementation model and development of a co-production and engagement resource.
- Support engagement and subsequent implementation of major healthcare plans and strategies, including continued evidenced input into the 10 Year Workforce Plan and the National Cancer Plan.
- Work with NHS England and the Department of Health and Social Care to further embed the Observatory as a partner in delivering the ambitions and implementation of the 10 Year Health Plan, including in the delivery of its future business planning and sustainability programme, ensuring the vital role of the Observatory beyond 2027 in the process.
Appendix 1: NHS Oversight Framework Health Inequalities Metrics
| Metric | Organisations to which the metric relates |
|---|---|
| Deprivation and ethnicity gap in pre-term births | Integrated care boards |
| Deprivation gap in early cancer diagnosis gap | Integrated care boards |
| Deprivation gap in myocardial infarction and stroke admissions | Integrated care boards |
| Percentage of annual health checks completed for patients with a learning disability or who are autistic | Integrated care boards |
| Under 18s elective waiting list growth | Acute trusts |
| Percentage of older inpatients (over 65) with >90 day length of stay | Mental health trusts |
Appendix 2: Interim themes emerging from the Core20PLUS5 longitudinal evaluation: scoping report
The table below summarises the key conclusions based on the key findings of the scoping interviews for each of the four domains. Alongside these conclusions, the table also provides recommendations for both the Department of Health and Social Care (DHSC) as well as the NHS England HiQiP team. (Excerpt from The Strategy Unit, Core20PLUS5 Evaluation Scoping Report).
This table is available upon request: england.boardsecretariat@nhs.net
Appendix 3: NHS Race and Health Observatory strategic ambitions
Appendix 4: Overview of health inequalities data ambitions
Health inequalities measurement framework
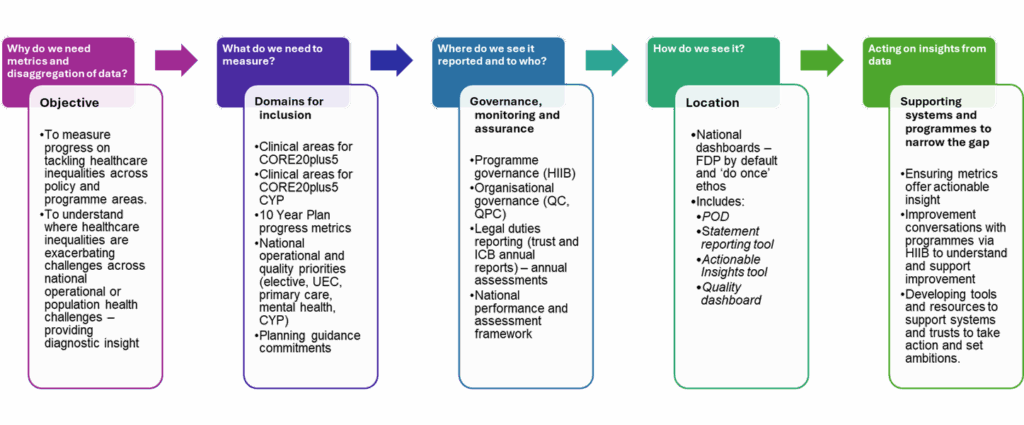
Shifting towards measurement and impact requirements