Background
The Education and Training Tariffs: tariff guidance and prices for the 2023 to 2024 financial year is a guidance document which is intended to provide further information in support of the education and training (ET) tariff payment process. This includes:
- details about the introduction of the ET tariff payment mechanism,
- confirmation of NHS England’s continued responsibilities for ET tariff development,
- powers and requirements with regards to the application of the ET tariffs in 2023 to 2024,
- further information relating to the ET tariffs for 2023 to 2024, including prices and scope and links to further guidance which support and supplement the information contained in the tariff guidance document.
It should also be noted that as of 1 April 2023, Health Education England (HEE) will be merging with NHS England to create the new NHS England. As this guidance applies to the 2023/24 financial year, references are made to NHS England rather than HEE. Email addresses with the domain hee.nhs.uk will remain active until they are replaced by equivalent NHS England addresses. All email addresses and website links will still apply. Any changes to contact information of websites will be confirmed in the next version of this guidance.
The clinical tariff payment is a payment which is intended to provide a contribution to the funding of placement coordination and practice-based learning (this can be defined as a setting where trainees learn clinical skills and gain experience towards their placement hours) for all eligible clinical professions. The funding is provided for clinical education and training and should be used to support all professions for which it has been allocated and it is funded by the Department of Health and Social Care (DHSC).
NHS England is responsible for administering the tariff payments to placement providers in line with the tariff guidance document, which has been published annually by DHSC on the Government website.
Alongside NHS England’s role in administering tariff payments to placement providers, from April 2021, NHS England assumed responsibility for tariff development, including production and publication of this tariff guidance document.
As part of these responsibilities, NHS England continue to be required to present tariff proposals annually to DHSC for sign-off and ministerial approval. This approach to developing the placement tariffs does not impact on the existing powers and requirements for the tariffs set out in legislation (see paragraph 2.6 of the tariff guidance for further information).
Clinical tariff
The Department of Health and Social Care (DHSC) have accepted recommendations from NHS England that have resulted in an increase to the funding available to placement providers in 2023/24 for the delivery of placement activity covered by the scope of the clinical tariff (see eligibility below).
Table 1 below provides confirmation of the prices that will be applied to activity from 1 April 2023. The price has been uplifted for 2023 to 2024 from 1 April 2023 to reflect inflation within the outcomes of the spending review settlement. The April increase reflects feedback from stakeholders around the need to increase the current funding and has been achieved through redistribution of funding from the wider tariff quantum, primarily through a reduction to the funding of undergraduate medical placements.
Please note when reviewing table 1 that the figures presented are the payment per full time equivalent (FTE) and not the payment per student. For the purposes of this funding an FTE is defined as 40.8 weeks of placement, including 37.5 hours per week. Therefore, to achieve the full payment a provider would need to deliver 1,530 hours of placement activity. See the example in the Accessing clinical tariff for your organisation section for details on how to calculate payments and payment (£) per hour for tariff.
Table 1: ET tariff prices for 2023 to 2024
|
Type of placement |
(Revised) Tariff for placement activity in 2023 to 2024 |
|
Clinical |
£5,343 + Market Forces Factor (MFF) per full time equivalent (FTE) |
Visibility of clinical tariff funding
NHS England have worked with several teams within providers who have accessed the clinical tariff (formally Non-Medical Education Tariff or NMET) to support the development and quality of clinical student placements and they are keen to share their experiences and learning from this process. It is important that funding is spent accordingly, as funding for the clinical tariff is limited to a specific amount as it is an annual contribution to the funding of placement coordination and practice-based learning for all eligible clinical professions. Hence it is fundamental that the clinical tariff funding is value for money and spent appropriately in supporting the development of high-quality placements.
NHS England is aware that accessibility and transparency around funding can be challenging for healthcare professionals and education providers to navigate, however, NHS England aims to address this by providing clear and concise information as well as case studies on the process of accessing the clinical tariff, understanding the flow of funding and where this sits within the organisation. Also, given the increase in funding, it is of great importance that there is clarity, transparency, and parity of access for all professions to access the clinical tariff if they wish to.
NHS England provides funding to placement providers via the clinical tariff payments to:
- ensure that those providers are reimbursed consistently for the training placements that they deliver
- contribute to the delivery of placements that are high quality and ensure that learners develop the skills and knowledge they require to meet their respective professional competencies.
Clinical tariff eligibility criteria
The Education and Training Tariffs: tariff guidance and prices for the 2023 to 2024 financial year, including the clinical tariff, is set by the Department of Health and Social Care (DHSC) with NHS England overseeing the Education and Training (ET) tariff payment process and all other related ET responsibilities.
To be eligible for clinical tariff funding from NHS England, a placement must meet each of the following criteria:
- Must be a recognised part of the education and training curriculum for the course and approved by the Higher Education Institute (HEI) and the relevant regulatory body, as appropriate.
- Must meet the quality standards of the regulator, the commissioner and NHS England.
- Must offer direct clinical training (including time for clinical exams and study leave) with an agreed programme, being a minimum of one week.
- Must have the appropriate clinical and mentoring support as defined by the relevant regulatory body.
- Must not be workplace shadowing or an assistantship.
- Have signed the NHS education contract.
Tariff payment and scope
The clinical tariff payment is intended to provide a contribution to the funding of placement activity for all eligible clinical professions and includes funding for international students. The list below, which mirrors the current tariff guidance, provides confirmation of the professions eligible for tariff funding:
- Clinical psychologist
- Healthcare Science Practitioner Training Programme
- Adult nurse
- Children’s nurse
- Dental hygienists/therapists
- Diagnostic radiographer
- Dietitian
- Dual qualification nursing
- Learning disabilities nurse
- Mental health nurse
- Midwifery
- Shortened midwifery courses
- Occupational therapist
- Operating department practitioner
- Orthoptist
- Orthotists/prosthetists
- Paramedics
- Pharmacist (from 1 September 2022)
- Physiotherapist
- Podiatrist
- Speech and language therapists
- Therapeutic radiographer
- Sonographers
Please note, apprenticeships are not eligible for clinical tariff funding.
Furthermore, there are a number of professions which are funded by NHS England in line with the current tariff arrangements but are not within scope. These include:
- Physician associates
- Trainee nursing associate – direct entry
In order that the placement tariffs are utilised and distributed fairly, the guidance from the DHSC states:
- Placement providers must demonstrate that any funding for clinical placements is being utilised for the delivery of such learning.
- Higher Education Institutes (HEIs) must ensure they involve the NHS placement provider budget holder in discussions on the provision of clinical placements, who must be able to identify, manage and control the costs of the placement.
- Transparency of usage of placement funding will be monitored by NHS England. It is expected that there will be regular discussion between the placement provider, HEI, and NHS England.
- All members of the tripartite agreement have access to information on arrangements governed by the agreement, and on the funding allocated to placement providers.
Collecting placement activity data – the student data collection tool
NHS Trusts
NHS England has a process for collecting placement activity data from Higher Education Institutes (HEI) and ensuring that this is accurate, before releasing funding to the placement provider. NHS England have launched a nationally standardised Student Data Collection Tool in March 2020 for the collection of degree level (and above) courses in health and care (excluding medics). The collection of this data directly informs financial payments including clinical tariff payments (often referred to as “placement tariff”) and enables NHS England to understand current and planned future student activity, and the future workforce.
Through this tool, NHS England collects data related to:
- How many students are studying; what they are studying and where
- How many students successfully complete their studies and over what time
- Student attrition on non-medical tariff supported pre-registration courses
- Students attracting salary support
- Clinical placement activity.
HEIs submit placement activity three times per year, aligned to the main student intake dates. Each submission covers a specific time and the placement activity which occurred within that timeframe, by profession, qualification and year of study identifying each relevant placement provider. Placement activity is recorded in hours as this is the tariff unit of currency.
For example, University X may report that Trust A delivered 100 hours of clinical placements for second year BSc (Hons) podiatry students between 1 November 2021 and 15 February 2022.
The data is submitted via an online platform, the student data collection tool (SDCT).
NHS England undertakes basic checks of the data. For example, ensuring a trust is correctly named or that the HEI has provided activity for all eligible programmes which it delivers. If NHS England is aware of consistent relationships between an HEI and a placement provider for specific programmes, it may check that activity is represented in the latest data set.
After these initial checks, the data is released, through the SDCT, to NHS trusts for validation. The data must be validated before a payment can be made.
Different trusts will have different sign off procedures. Some sign all placement activity off centrally through their Clinical Education Team, meaning there are a limited number of trust users on the SDCT. Others may require individual professional leads, or even individual team leaders, to confirm the activity for the students they hosted in the time. If you are unsure, contact the Education Department in your trust to check.
The trust can do one of the following:
- Agree that the data submitted by the HEI is correct
- Dispute the data by providing an alternative figure, and a rationale which supports this (for example, number of students and dates placements occurred)
If the figure is disputed, the line of data returns to the HEI for review. The HEI can either accept the revision or reject it, possibly offering an amendment to their own original figure. If an agreement cannot be reached between the HEI and the trust, NHS England will act as arbitrator.
The placement data must be validated within a set timeframe outlined for each validation window to ensure that a payment can be made to the trust.
Payment for clinical placements is part of the Education Contract, formally known as the Learning and Development Agreement, held between NHS England and the trust. The contract covers all funding streams between NHS England and the trust, but the financial schedules issued before an invoice can be raised break these down to specific activity streams. Within the clinical schedule, it is straightforward to identify the profession/university for which placement money relates to and the period in which the activity occurred.
Private, Independent and Voluntary Organisations (PIVO)
NHS England has different arrangements for managing placement activity for Private, Independent and Voluntary Organisations (PIVOs). This includes NHS England making placement funding available to the Education Providers who can then sub-contract on to PIVOs directly for placement activity, assuming that this provider is only supporting a relatively small number of placements or where the provider is not holder of the NHS Education Contract. Pharmacy is an example of a profession which gets funding for clinical placements via PIVO. NHS England does not expect small PIVO placement providers to undertake validation activities. It is anticipated that the Education Provider will be validating the activity agreed and will be able to evidence this, and that this will be subject to audit where required. NHS England will therefore continue to use the current local office arrangements in place for payment of placement activity by small PIVO placement providers.
It is important to note that there may be regional differences in funding for PIVO from NHS England. Please get in touch with your NHS England regional team if you require further information on this.
Simulation-based learning
Funding arrangements are in place for simulation-based learning that meets the criteria in section 4.11 through to 4.13 of the Education and Training Tariffs: tariff guidance and prices for the 2023 to 2024 financial year, for activity that constitutes placement learning hours. NHS England will not pay the clinical tariff rate for simulation activity delivered as part of the education provider’s teaching requirements.
For confirmation of activities classified as simulation, please refer to section 4.11 through to 4.13. Please note, there is no requirement for NHS England to approve the simulation hours, in line with section 4.11 through to 4.13 of the guidance.
Knowledge and Library Services
There are several requirements on Placement Providers regarding library service provision. These are set out in Schedule 1, Section 14 of the NHS Education contract. The Placement Provider is required to ensure that there is a proactive, high-quality knowledge and library service that is available to all staff and learners, whether this is hosted internally, or delivered via a managed service level agreement (SLA).
NHS England’s Guide to NHS Education funding (p. 7), highlights that education funding contributes to the costs of proactive, high-quality knowledge and library services for all learners and the workforce.
NHS England offers indicative guidance on the basis on which Placement Providers determine the proportion of funding from tariff that should flow, as a minimum, to a knowledge and library service.
The DHSC’s Education and Training Tariff document sets out an option for organisations within a local area to agree to pool a proportion of the placement fee (Section 7.7). This may assist some knowledge and library services to improve provision to clinical students on placement.
Placement providers are encouraged to engage with the local knowledge and library service manager to ensure that the service has the right resources to offer proactive, high-quality services irrespective of the setting in which clinical students and staff are based.
Accessing clinical tariff for your organisation
The clinical tariff can provide a useful resource for supporting a high-quality practice placement experience. This could be through funding provision of knowledge and library services, setting up simulation centres or by creating dedicated clinical education teams.
As you work through the process of identifying your clinical tariff, consider how you will utilise it and how you will demonstrate that this is having a beneficial impact on the placement experience.
Step 1
Speak to your education team and understand what resources and services are currently available to support clinical student placements. For example, is there a clinical student placement coordinator or a practice education facilitator to support student placements? They may be able to help provide information about your placement activity and how your organisation is supporting placements across the clinical professions.
Step 2
Understand how many clinical students your organisation supports per year. This step will be easier if all your placement activity is centralised through a team who have responsibility for clinical education. Your education team may be able to provide you with some placement activity data (this is how the clinical tariff is calculated).
DHSC have agreed a financial uplift for the clinical tariff for 2023 to 2024, which can be found in the Education and Training Tariffs: tariff guidance and prices for the 2023 to 2024 financial year. Please refer to Table 1 previously where you can find the most recently published ET Tariff prices.
Market Forces Factor (MMF) estimates the unavoidable cost differences between healthcare providers. It is used to adjust resource allocations in the NHS in proportion to these cost differences, so that patients are neither advantaged nor disadvantaged by the relative level of unavoidable costs in various parts of the country. NHS England calculate an individual MFF value for each NHS trust and foundation trust.
Where a placement provider doesn’t have an agreed MFF payment index, NHS England has calculated regional MFF indices that will support payments. For example, a central London trust will have a higher MFF rate than a trust based in Manchester.
See Annex A for the Regional MFF payment indices for 2023 – 2024.
Example of how to convert activity into money
For illustrative purposes, we have created an example based on a provider with an MFF payment index of 1.0383 undertaking 5000 hours of placement activity across the 22/23 financial year and a tariff price of £5,000.
a. As identified above, an FTE for placement funding purposes is determined as 40.8 weeks of placement activity. The first step in calculating an appropriate payment is therefore, to divide the tariff price by the number of weeks to get a payment per week.
£5,000 ÷ 40.8 weeks = £122.55
b. Once we have calculated the payment per week of £122.55, we are then able to calculate the payment per hour, which is calculated by dividing the weekly rate by 37.5 hours.
£122.55 ÷ 37.5 hours = £3.27
c. The hourly rate should then be applied to the total number of hours of placement activity.
5,000 hours x £3.27 = £16,350
d. The final stage is to apply the MFF payment index to the total funding.
£16,350 x 1.0383 (Midlands MFF rate) = £16,976
The total funding that this activity will generate is therefore £16,976.
Step 3
Speak with your finance lead or budget accountant to ask them to help you to understand the current situation. For example, is the clinical tariff money already paid in to your local or departmental budget? How is the clinical tariff broken down per professional group? What proportion of tariff flows through to the knowledge and library service?
Utilising clinical tariff – case studies
West London NHS Trust
Helen Lycett, Associate Director for Allied Health Professions (AHP)
Situation
West London NHS Trust is an integrated provider of community and mental health services, with a broad range of in-patient and out–patient services. There are approximately 300 AHPs working across all clinical pathways.
The Associate Director for AHPs commenced in post in January 2016 and made it an immediate priority to ensure that there was a strong culture of supporting pre-registration clinical placements for AHP students within the Trust. Central to supporting the development of this culture was the placement tariff that the Trust receives for the placements it facilitates.
The placement tariff is paid by NHS England to placement providers and supports them with being able to provide a high-quality learning experience. It aims to ensure However, from discussion with colleagues regionally and nationally we know that, for many AHPs the placement tariff goes unidentified within providers and the opportunity for using it to support practice placements is lost.
Who is involved?
The Associate Director for AHPs worked with the Director of Nursing and Directorate Accountant over several months to identify where the placement tariff for AHPs was and introduced a mechanism to ensure that going forward this money was filtered into a central budget so that it could be clearly identified for use to support the delivery of AHP practice placements. In doing so this also increased the governance and accountability of these funds and ensured the Trust was more easily able to report back to NHS England on the activity the money is being used to support.
Action taken
In the first 12 months of having access to the placement tariff the Associate Director for AHPs used the funds to create a Darzi Fellow role who led a project to improve the quantity and quality of AHP practice placements across the Trust. They developed a range of systems and structures to ensure that the oversight of practice placements across the organisation was greatly improved and that the experience of AHP students having a placement in the Trust was positive and rewarding. In 12 months, they increased practice placements in the Trust by 50% and in doing so provided proof of concept that having a centralised role (funded by placement tariff) could have a significant impact on the culture of supporting AHP students within the Trust.
Outcomes
After this the placement tariff was used to create an AHP education lead post that worked directly to the Associate Director for AHPs. This was on a 0.3 WTE basis originally and so given their limited capacity they focussed largely on supporting the practice placement agenda within the Trust. Over time they were able to increase placement capacity sufficiently to increase the hours of the role, eventually to full time. In 2020 the Associate Director for AHPs successfully secured funds for an additional AHP education lead on a 12-month fixed term basis, but this was with a specific objective of increasing AHP placements to the place where the placement tariff would be able to fully fund the two AHP education lead posts on a substantive basis. Within 8 months of having these two posts in place that objective had been reached and the posts were made permanent in December 2021.
This success was driven by robust use of data, which demonstrated the impact that the roles were having on AHP placements, and this is key to anyone wishing to replicate what was achieved in West London NHS Trust. But ultimately, this was predicated on being able to access and make use of the placement tariff. This money provided a vital foundation for demonstrating the benefit of a dedicated resource to support practice placements. During this time both AHP education leads have won awards for their work and the Trust is now recognised as an exemplar of best practice for AHP practice learning.
Top 3 tips
- Work closely with your Trusts finance team to identify where the placement tariff sits.
- Create the case for centralising the placement tariff within the budget of the trust’s Chief AHP or similar.
- Use data to evidence the impact of utilising the placement tariff, to help build the case for additional resource.
Croydon University Hospital, NHS Foundation trust
Sindhu Sivagnanasithiyar – Project Manager for Midwifery Student Clinical Expansion, South West London Integrated Care Board (SWL ICB)
Margaret Nakigudde – Maternity Programme Manager, (SWL ICB)
Situation
As part of the on-going work to increase the midwifery workforce, SWL ICB have been working with NHS England as part of the Maternity workforce transformation strategy, to enable and support the expansion in midwifery training placements.
As part of the four-year strategy there is commitment to increase training placements between 2019/20 and 2023/24 by 25 percent, over four years. NHS England will increase midwifery starts in England by 3650 annually achieved by the end of 2023, with the first 650 places from 2019/20 and up to 1,000 places for a period of three years thereafter.
As part of the midwifery student clinical placement expansion project, which commenced in September 2022, SWL ICB carried out a scoping process across the South-West London Local Maternity and Neonatal System (LMNS). We recognised that the full-time equivalent education and training tariff has increased twice in the 2022-23 financial year, once in April with an inflationary uplift and then more significantly for the new academic year in September as NHS England seeks to narrow the funding gap between clinical professions and undergraduate medical students.
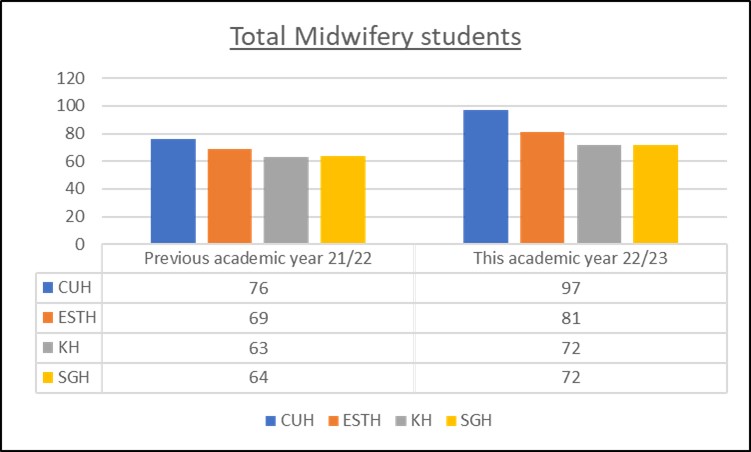
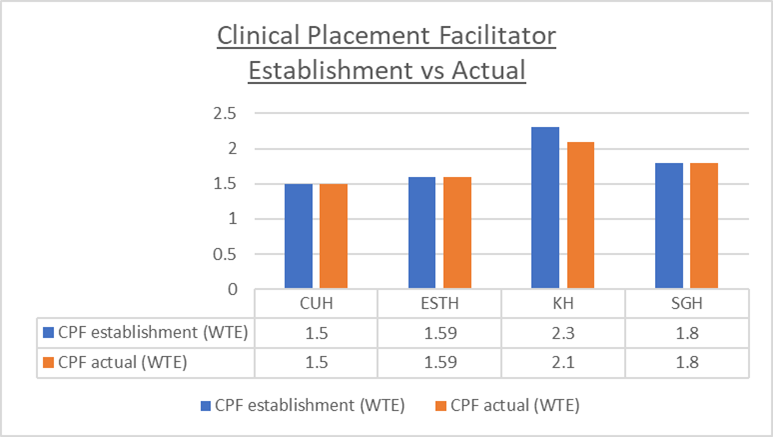
A gap analysis was carried out as part of the project and identified that while all trusts have seen an increase in students, clinical practice facilitator (CPF) support is required accordingly with this increase (depicted below in both figures 1 and 2).
Figure 1: total midwifery students
Academic year 21/22
- Croydon University Hospital: 76
- Epsom and St Helier Hospital: 69
- Kingston Hospital: 63
- St Georges Hospital: 64
Academic year 22/23
- Croydon University Hospital: 97
- Epsom and St Helier Hospital: 81
- Kingston Hospital: 72
- St Georges Hospital: 72
Figure 2: clinical placement faciliatory establishment versus actual
| CPF establishment (WTE) | CPF actual (WTE) |
|
| Croydon University Hospital | 1.5 | 1.5 |
| Epsom and St Helier Hospital | 1.59 | 1.59 |
| Kingston Hospital | 2.3 | 2.1 |
| St Georges Hospital | 1.8 | 1.8 |
Who is involved?
-
- South-West London Integrated Care System (SWL ICS) project manager for midwifery student clinical expansion
- Croydon University Hospital (CUH) head of nursing for practice development and education
- Croydon University Hospital (CUH) director of midwifery
- NHS England senior strategic programmes, planning and performance manager
- South West London Integrated Care System (SWL ICS) maternity programme manager
- South West London Integrated Care System (SWL ICS) head of maternity
- Acknowledgement: Kingston University for introducing NHS England senior strategic programmes, planning and performance manager to SWL ICS project manager for midwifery student clinical expansion.
Action taken
- Scoping process – in December 2022, while carrying out a survey questionnaire and reviewing student feedback, it was evident students value the support of CPFs. The vacancy rate within the maternity department at Croydon University Hospital (CUH) was 23%. As a result, CPFs were covering staff sickness or staff shortage and students have provided feedback that support is not always available, which affects student experience.
- Request for ICS support – following consultation with the South-West London Directors of Midwifery and Clinical Placement Facilitators (CPFs) across the sector, the SWL Integrated Board has agreed to support and prioritise the identification of the midwifery student tariff at trust level, and transparently allocate underspend funding resources on the midwifery workforce and future service provisions.
- The SWL ICB project manager for midwifery student clinical expansion and SWL ICB maternity programme manager initiated discussions with the NHS England senior strategic programmes, planning and performance manager to gain an understanding of student placement tariff and how this could be used to support student expansion and experience. Roundtable discussion – following this, and with permission of the Director of Midwifery in CUH, there was engagement and collaboration with the Head of Nursing and finance team. This encouraged and facilitated conversations identifying and ringfencing midwifery student tariff.
Outcomes
We have been successful in securing funding for a 1-year fixed term contract for a Band 7 clinical placement facilitator (CPF) 1.0 WTE for the midwifery services at CUH, in response to a survey which was undertaken with students reporting that CPF(s) improve the student placement experience. SWL LMNS will obtain further student experience feedback via The National Education and Training Survey (NETS) and student midwifery attrition data from the CUH CPF team and provide quarterly reports to the London Midwifery Placement Assurance Group. This will help ensure the funding is used to support the student placement experience (which is a factor in improving student retention and growing the nursing workforce) as well as increase the organisation’s credibility for responding to the student experience survey (“you said, we did”) by increasing the number of CPFs available. This will also be reviewed and discussed in the next SWL bi-monthly directors of midwifery meeting for forward planning and sustainability of the post beyond the end of this project, and for the following financial year.
Top 3 tips
- Work closely with Directors of Midwifery, the maternity education team and NHS England to support a better understanding of how student placement tariff is received and used in the trust.
- Showcase the work done for shared learning and future ringfencing of student midwifery tariff.
- The tariff return is completed correctly through good collaborative relationships with HEIs and in conjunction with CPFs or those directly supporting students to ensure entitled funds are granted. Collaboration and engagement with the ICB can help prioritise identification of funding.
Great Ormond Street Hospital, NHS Foundation Trust
Vicki Smith, Lead for AHP Education
Situation
The Great Ormond Street Hospital (GOSH) Chief AHP post commenced in 2018 and this was instrumental in determining the strategic vision for AHPs working at GOSH. One of the key priority areas outlined in the strategy was Education and Training and this was further supported by the Director of Education. Historically the Trust had funded an AHP educator post. This was originally on a 0.2 WTE basis which was increased by additional funding from the GOSH Learning Academy to a 0.5 WTE role in March 2020.
Who is involved?
Engagement and collaboration with Chief AHP, AHP Leads, and our finance team allowed us to identify and locate the AHP student tariff and have open and honest discussions regarding the best use of this money.
Action taken
It was recognised at the start of the pandemic that more educational leadership was required to support the AHP placement expansion program, and the Trust funded an Education Lead on a 0.2 WTE basis to oversee this work. This coincided with a successful bid and funding from Health Education England for an additional 1.0 WTE educator post to lead our Clinical Placement Expansion Programme (CPEP) which further expanded the team.
The CPEP funding was crucial for building capacity and capability within the AHP education team to support and lead AHP placements. Within this work the team scoped barriers to placement expansion, streamlined placement processes, and implemented new ways of working. This allowed GOSH to increase AHP placements by 20% in 2020/2021. This work was carried out in collaboration with local clinical educators and service leads through both Placement Working Group and AHP Education Working Group, respectively. Identifying key challenges and concerns was instrumental in developing a strategy to overcome some of the obstacles to increasing placement capacity whilst ensuring the expansion work was sustainable and high quality of education was maintained.
Outcomes
The tariff is now held centrally which ensures this money can be effectively used to support student placements and ensures GOSH can demonstrate accountability for these funds. The CPEP was a huge success and highlighted the success of a centralised AHP educator to support practice learning. Agreement was made to use the tariff money to continue to fund the central educator and this post is currently in the process of being converted to a substantive role. We were also successful in securing further CPEP funding 21/2022 and this has been used to appoint another central educator with the aim of increasing placement capacity by almost 50% for the year 2021/2022. We are also streamlining our induction processes, delivering educator workshops, and developing modules to support students while on paediatric placements. We plan to use our tariff to ensure the sustainability of this post and placement expansion.
Nivi Behari (AHP Educator, CPEP Lead)
“The clinical tariff helped us to understand the challenges we face in delivering student placements and collaboratively figure out how we not only increase the number of students we take but also improve quality of students’ experiences.” #OneAHPTeam
Philippa Wright (Chief AHP)
“The clinical tariff has enabled the AHP workforce at GOSH to sustain the workstreams developed through earlier funding. The results are clear as our student numbers have significantly increased, and we know this will now be sustainable into the future owing to investment in specific leadership for student placements.”
Top 3 tips
- Work closely with service leads and local clinical educators to driving forward a change in the way tariff is used and placements are delivered.
- Showcase the work done and support local teams to demonstrate the worth of a central education team.
- Work closely with your Chief AHP to identify and drive strategic and priority areas.
Leeds and York Partnership Foundation Trust
Caroline Frascina, Practice Learning and Development lead for AHPs and Psychology
Situation
Leeds and York Partnership Foundation Trust is the main provider of specialist mental health and learning disability services in Leeds. We also provide specialist services across York, the Yorkshire and Humber region, and some highly specialised national services.
Our Education Tariff journey started approximately seven years ago when two temporary posts were created. These roles consisted of a Nurse and AHP ‘Service Improvement Lead for Practice Education’. These were temporary posts for 12 months with the aim of:
- Reviewing capacity: Gaining sight on the number of practice educators and placement capacity across the Trust
- Review of roles and responsibilities: including educators, educational leads (who oversee practice education in their services) and managers
- Develop a clear process for practice education across the Trust including improving the consistency and quality of educator training, quality placement monitoring and improving networks with local HEIs.
As part of these posts, we established a clear view of who are educators were across the Trust and what level of educator training they had received and a named ‘educational lead’ for each service area – both of which understood their roles in education. We also continued to support regular Educational Lead forums and a yearly away day so that these individuals could access continued support and development of their roles.
In addition, we needed to demonstrate the ongoing benefit of having these posts within the Trust via a business case. Luckily, we were able to make this case and the posts were made permanent. Initially though these were not funded by the education tariff.
Who is involved?
A short time after the posts were made permanent, the Trust employed a new Executive Director of Nursing, Professions and Quality. She came with awareness that other Trusts had accessed education tariff and that this would be a sustainable way to fund these posts and further develop the team, with the goal of continuing to improve learner experience and increasing placement capacity.
Action taken
The Executive Director of Nursing, Professions and Quality initiated discussions with finance to gain sight of the Education Tariff and how this could be used to fund the posts.
The education tariff in Leeds and York Partnership Foundation Trust has been used to fund numerous posts including Nursing, AHP and Psychology Practice Learning and Development Leads. These roles not only look at practice education, but part of these roles also oversee our other learners such as preceptees.
Outcomes
Some of the benefits of accessing the Education Tariff have included:
- Placement capacity and quality: Despite covid-19, for AHP’s, only 16% of placements were cancelled and this was mainly due to university cancellations rather than the placement setting.
- Innovative placement developments including collaborative placements across organisational boundaries, 2:1 model regularly employed, addition of project, leadership, and virtual placements.
- Improved awareness and culture towards students across the organisation: Education is everyone’s business.
- Positive relationships with the local HEIs which supports collaboration.
- Attracting learners to working in the organisation once qualified.
Top 3 tips
- Collaboration between nursing and AHPs – working together with the same goal of accessing and using the Education tariff to support learners in our Trust.
- Identify key influential stakeholders. The Director of Nursing, Professions and Quality was a key individual in gaining access to Education Tariff.
- Communicate the benefit of gaining access to tariff. Clearly demonstrate the benefit to learners if the Education Tariff can be access and utilised effectively.
Buckinghamshire New University (BNU)
Margaret Rioga, Associate Professor – Head of Practice Learning
Situation
The BNU School of Nursing and Midwifery in partnership with Central and Northwest London NHS Foundation Trust (CNWL) and West London NHS Foundation Trust (WL) agreed to a trial of an online placement model called the Peer Enhance E-Placement (PEEP) (Taylor, 2020). PEEP is an online placement model which allows students to continue with learning to achieve their practice outcomes in line with professional body requirements and supports progression on programmes of learning. The PEEP model is facilitated via an online learning platform (VLE such as Blackboard) and is structured with a timetable underpinned by strong peer learning and online learning pedagogy (Salmon, 2011).
The aim of this project was to introduce innovative new ways of providing practice learning and to increase capacity. PEEP had been used for training Allied Health Professions (AHPs) prior to this project, but this is the first time it has been used for nursing. As part of the project, it was agreed by the PEEP Steering Group to share the tariff between the trusts and universities involved.
Who is involved?
The project was led by BNU and in partnership with Central and Northwest London NHS Foundation Trust (CNWL) and West London NHS Foundation Trust (WL).
The relationship between the organisations precedes this project, given that CNWL & WL are placement partners of Buckinghamshire New University.
Action taken
As part of the PEEP Steering Group, a decision was made to split the tariff payment 50/50 between the universities and the trusts. This was then agreed via a memorandum of understanding between the trusts and the university, which outlined the terms of the agreement: that the tariff would be shared, how they would all work as partners, and what the expectations were.
The trusts provided practice assessors so that the project would meet the Nursing and Midwifery Standards for Student Supervision and Assessment (SSSA) requirements. In turn, the university were required to hire experts by experience (people with lived experience of a mental health diagnosis or caring for someone with a mental health diagnosis) to act and play roles in the simulations throughout the six-week placement. This is to ensure the experience is as close to reality as possible.
The 50/50 tariff split which was agreed upon as part of the memorandum of understanding, addressed the percentage of the division. But dividing the money would still have to be managed practically. This was achieved in the following way: the university received the initial tariff payment, and then raised a purchase order with the trust. Finally, the university distributed 50% of the funding to the trust.
The university used the tariff to cover the cost of delivering a successful PEEP placement experience. The tariff was used to cover the costs of the simulation labs and equipment, PEEP training for team, as well as payments for the experts by experience who had to commit to the full 6 weeks of delivery. It was also used to release lecturers from teaching to be replaced by associate lecturers which led to a higher quality and more educative experience for learners.
Outcomes
The clinical tariff was successfully shared between the organisations. This was made possible by the effective governance and procedures followed in identifying, agreeing to share, and subsequently releasing the tariff.
The programme evaluation revealed that sharing tariff to provide PEEP training is a successful collaborative use of tariff.
Students who undertook the placement reported learning a lot of new skills and feeling more confident about going out into practice. Action learning sets also allowed them to develop wider skills. If the university and trusts had not shared tariff in this innovative and collaborative way, it would have been challenging to offer this educative experience for students.
The PEEP project is now in phase 2 – which entails taking the project wider throughout Northwest London.
Top 3 tips
- It is essential to have a memorandum of understanding which outlines how tariff will be shared along with roles & expectations. It’s critical to have those conversations and to get agreements in place.
- Practice assessors in trusts are so busy that it can be challenging to ensure you have enough of them who can come in and support with the programme. It’s important to plan this in advance. The university are also looking at employing their own pool of practice assessors.
- It’s important for universities to recognise that tariff can be used in different and more innovative ways. It is important to stay open to other potential innovative uses of tariff in the future.
Further feedback from clinical tariff users
- “It was useful to see interdisciplinary team working in a live setting and how important communication and the delegation of roles can influence the scenario and discuss what you do when you’re initially stumped during the first 30 seconds”. (Anonymous)
- “It was good to work with people with different skills and approaches to situations. I was able to see how the nursing role is different to the doctor’s role and how they both come together to help manage the patient’s condition”. (Anonymous)
More information
If you have any questions regarding this document, please email: england.wte.frp@nhs.net
Collaborators
With thanks to NHS England London and in particular the following colleagues below for their support in producing this document.
-
- Chloe Keith-Jopp, AHP Workforce Transformation Lead, NHS England, London
-
- David Marston, Senior Strategic Programmes, Planning and Performance Manager, NHS England, London
-
- Laura Leadsford, AHP Lead, NHS England, London
-
- Helen Lycett, Associate Director for AHPs, West London NHS Trust
-
- Paula Breeze, National AHP Clinical Fellow, NHS England
-
- Nhung Doan, Funding Strategy Officer, NHS England
-
- Michael Sanderson, Project Manager, NHS England
-
- Jenny Ekstrom, Deputy Head of Clinical Education Transformation, NHS England London
-
- Caroline Ward, Workforce Transformation Lead (Clinical), NHS England, London
-
- Jacqueline Robinson-Rouse, Capital Nurse Clinical Lead Pre and Post Registration Development & Retention, NHS England, London
Further thanks to the Clinical Tariff Working Group who have provided valuable contributions in supporting a national version of this document showcasing how the clinical tariff can be accessed across all clinical professions.
To note, if you would like us to include a case study of how your organisation has utilised clinical tariff and the benefits for you, please email: england.wte.frp@nhs.net
Annex A: regional market forces factor (MFF) payment indices for 2023 – 2024
|
Region |
MFF indices for 2023 – 24 |
|---|---|
|
London |
1.15860 |
|
East of England |
1.07468 |
|
Midlands |
1.03510 |
|
North East and Yorkshire |
1.02511 |
|
North West |
1.03414 |
|
South East |
1.07399 |
|
South West |
1.03706 |
|
National |
1.0618 |
Publication reference: PRN00527