Introduction
This document outlines the integrated urgent care (IUC) key performance indicators (KPIs) which commissioners must apply in relation to the service. It is for use by local commissioners, providers and NHS England.
It must be read in conjunction with the Integrated urgent care aggregate data collection specification (2023/24) which provides each of the metrics used in the KPIs, and the current Integrated urgent care service specification which provides additional detail.
This document seeks to clarify which organisations need to report against the KPIs listed and provides guidance to both commissioners and service providers on compliance.
In addition to these KPIs, NHS England will be monitoring other sources of operational information related to urgent and emergency care, including data linking NHS 111 calls and activity data, to ensure providers are maximising patient compliance with advice from NHS 111.
IUC services are regulated by the Care Quality Commission (CQC). The CQC approach when reviewing services is to consider:
- is it safe?
- is it effective?
- is it caring?
- is it responsive?
- is it well-led?
The KPIs and standards described in this document will contribute to the information the CQC uses when conducting service reviews.
A note on definitions
Throughout this document the term ‘provider’ is used to mean any organisation providing IUC services under an NHS Standard Contract (or legacy contract if an NHS Standard Contract is not yet in use), or a general medical services (GMS)/ personal medical services (PMS)/ alternative provider medical services (APMS) contract.
This may be:
- a provider organisation with whom an NHS commissioner has a contract to provide IUC services
- a GMS or PMS practice that chooses not to transfer responsibility for the provision of IUC services and either provides the service itself or sub-contracts the service to another provider
IUC services include:
- the assessment and management of patients by telephone who have called NHS 111
- activity generated by NHS 111 Online as described in the IUC Aggregate Data Collection (ADC)
- the face-to-face management of patients in any treatment centre (dealing with urgent care), the patient’s residence or other location if required
Results of the IUC KPIs should be considered in context of how local services are delivered.
Measurement of IUC
In October 2016 NHS England introduced a set of KPIs for IUC. These indicators built on the existing out-of-hours national quality requirements (NQRs), revising the way certain elements were measured and introduced new KPIs reflecting the development of the IUC model.
A revised set of KPIs were introduced in April 2021 following a review, with further amendments made in 2023.
During 2024, NHS England ran 3 KPI feedback sessions with key stakeholders to revisit these indicators, and concluded there was a need to simplify the collection and update these measures, resulting in a review of the existing KPIs.
That process has resulted in a refinement of the KPIs, with implementation required from April 2025.
IUC is provided by a variety of organisations; this includes ambulance services, private companies, not-for-profit organisations and other NHS organisations.
IUC is not limited to the provision of care at certain times or in a particular place.
The KPIs apply to parts or the whole of the patient journey and data needs to be compiled to allow them to be measured, managed and reported irrespective of any organisational boundaries.
Providers will need to co-operate so that this is achieved, even when they operate under separate contracts.
Commissioners have a key role to play in enabling the flow of data between provider organisations in order to supply the full set of data items required.
The KPIs are whole system measures and do not aim to focus on particular provider types unless stated. Commissioners can define additional local KPIs as required to monitor the service they receive in relation to their IUC contracts.
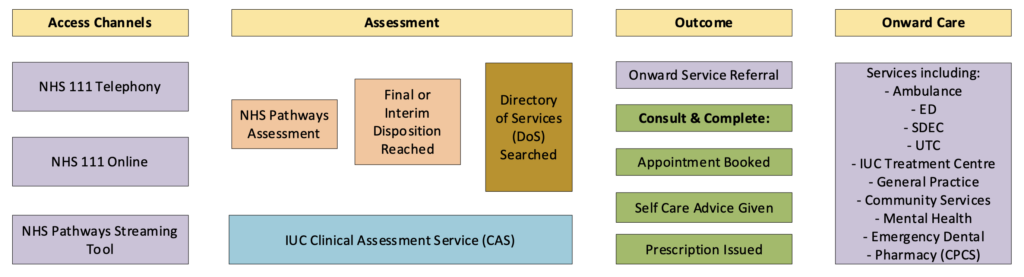
Figure 1: IUC patient journey. Different steps in this journey may be provided by different organisations.
The IUC KPIs
This section contains the KPIs to measure the performance of the IUC service. These KPIs will be published on a monthly basis.
Table A1: Summary list of KPIs
| KPI | Title | Standard |
| 1 | Proportion of calls abandoned | ≤3% |
| 2 | Average speed to answer calls | ≤20 seconds |
| 3 | 95th centile call answer time | ≤120 seconds |
| 4 | Proportion of call-backs assessed by a clinician in agreed timeframe | ≥90% |
| 5 | Proportion of calls initially given a category 3 or 4 ambulance disposition that receive remote clinical intervention | ≥95% |
| 6 | Proportion of calls initially given an ETC disposition OR category 3 or 4 ambulance disposition that receive remote clinical intervention | ≥80% |
| 7 | Proportion of callers allocated the first service type offered by directory of services | ≥80% |
Appendix A: description and definitions of the key performance indicators
KPI 1: Proportion of calls abandoned
- ADC ref: B02 / (A03+B02)
- Frequency: monthly
- Assesses: NHS 111 call-receiving organisation
|
Rationale |
Abandoned calls represent an unquantifiable clinical risk since, by definition, the needs of the caller are not established. | |||
|
Numerator | B02 Number of calls abandoned | |||
|
Denominator | a) A03 Number of calls answered b) B02 Number of calls abandoned | |||
|
Source |
Management Information System | |||
|
Standard |
≤3% | |||
KPI 2: Average speed to answer calls
- ADC ref: B06 / A03
- Frequency: monthly
- Assesses: NHS 111 call-receiving organisation
| Rationale | The length of time before a call is answered is an important contributor to the overall patient experience. Prolonged delays in call answer time result in increasing rates of calls abandoned which generates clinical risk. | |||
| Numerator | B06 Total time to call answer | |||
| Denominator | A03 Number of answered calls | |||
| Source | Management Information System | |||
| Standard | ≤20 seconds | |||
KPI 3: 95th centile call answer time
- ADC ref: B07
- Frequency: monthly
- Assesses: NHS 111 call-receiving organisation
|
Rationale |
The length of time before a call is answered is an important contributor to the overall patient experience. Prolonged delays in call answer time result in increasing rates of calls abandoned which generates clinical risk. | |||
Data item | B07 95th centile call answer time | |||
|
Source |
Management Information System | |||
|
Standard |
≤120 seconds | |||
KPI 4: Proportion of calls assess by a clinician in agreed timeframe
- ADC ref: (D14+H20+D23+H22) / (D13+H19+D22+H21)
- Frequency: monthly
- Assesses: NHS 111 call-receiving organisations / CAS
| Rationale | Patients should be assessed within a reasonable time, therefore, time to call back (where this is required) should be monitored. | ||||
| Numerator | a) D14 Number of callers who needed to speak to a clinician or Clinical Advisor within 20 minutes (immediately), who were warm transferred or received a call back within 20 minutes. b) D23 Number of callers who needed to speak to a clinician or Clinical Advisor within a timeframe over 20 minutes, who were warm transferred or received a call back within the specified timeframe. c) H20 Number of NHS 111 Online contacts where person was offered and accepted a call back and needed to speak to a clinician or Clinical Advisor within 20 minutes (immediately), who received a call back within 20 minutes. d) H22 Number of NHS 111 Online contacts where person was offered and accepted a call back and needed to speak to a clinician or Clinical Advisor within a timeframe over 20 minutes, received a call back within the specified timeframe. | ||||
| Denominator | a) D13 Number of callers who needed to speak to a clinician or Clinical Advisor within 20 minutes (immediately). b) D22 Number of callers who needed to speak to a clinician or Clinical Advisor within a timeframe over 20 minutes. c) H19 Number of NHS 111 Online contacts where person was offered and accepted a call back and needed to speak to a clinician or Clinical Advisor within 20 minutes (immediately). d) H21 Number of NHS 111 Online contacts where person was offered and accepted a call back and needed to speak to a clinician or Clinical Advisor within a timeframe over 20 minutes. | ||||
| Source | Management Information System | ||||
| Standard | ≥90% | ||||
KPI 5: Proportion of calls initially given a category 3 or 4 ambulance disposition that receive remote clinical intervention
- ADC ref: E20 / E19
- Frequency: monthly
- Assesses: system
| Rationale | Activity needs to assure the appropriateness of ambulance dispositions. | |||
| Numerator | E20 Number of calls initially given a category 3 or 4 ambulance disposition that receive remote clinical intervention | |||
| Denominator | E19 Number of calls initially given a category 3 or 4 ambulance disposition | |||
| Source | Management Information System | |||
| Standards | ≥95% | |||
KPI 6: Proportion of calls initially given an ETC OR Category 3 or 4 disposition that receive remote clinical intervention
- ADC ref: (E27+E20) / (E26+E19)
- Frequency: monthly
- Assesses: system
| Rationale | Activity needs to assure the appropriateness of ETC dispositions. | ||||
| Numerator | a) E27 Number of calls initially given an ETC disposition that receive remote clinical intervention b) E20 Number of calls initially given a category 3 or 4 ambulance disposition that receive remote clinical intervention | ||||
| Denominator | a) E26 Number of calls initially given an ETC disposition b) E19 Number of calls initially given a category 3 or 4 ambulance disposition | ||||
| Source | Management Information System | ||||
| Standards | ≥80% | ||||
KPI 7: Proportion of callers allocated the first service type offered by directory of services
- ADC ref: F03 / F01
- Frequency: monthly
- Assesses: system
| Rationale | IUC effectiveness is dependent on commissioning of adequate urgent care services and their inclusion in the Directory of Service (DoS) so that patient choice is respected. | ||||
| Numerator | F03 Calls where the caller is allocated the first service type offered by DoS | ||||
| Denominator | F01 Calls where the Directory of Services is opened | ||||
| Source | Management Information system | ||||
| Standard | ≥80% | ||||
Appendix B: related data
Aside from the KPIs and the rest of the monthly collection, commissioners and NHS England will need other management information for various purposes.
Workforce data
Providers will be expected to share workforce planning and capacity information with the central IUC team in order to manage service demand. Details around this will be provided separately.
Patient experience data
An NHS 111 Patient Experience Survey is collected by providers every 6 months in October and April.
Following a review in 2021, a revised version of the survey was introduced from April 2022 and remains in place.
Further details about the survey are available here: Statistics » Integrated Urgent Care
Publication reference: PRN01964

