Foreword
People experience life-changing moments within NHS services every day. They may be undergoing challenging treatment, receiving difficult news or reaching their final hours of life. While people turn to the NHS for issues with their health, we know that supporting their pastoral, spiritual and religious needs is integral to their overall care. Access to this support, through our NHS chaplaincy services, plays an important role in delivering personalised care and reinforces our core values of respect, dignity and compassion.
Our chaplaincy services also provide a vital source of support for our staff which we saw especially during the height of the COVID-19 pandemic. I’d like to offer my own personal thanks to our chaplaincy colleagues for supporting patients, their families and our staff in unpredictable and extremely challenging circumstances.
In the NHS Long Term Plan, we committed to delivering more personalised care to our patients and ensuring that we listen to their choices, values and preferences. This new guidance makes an important contribution to that process, and I thoroughly recommend it to everyone who is involved the delivery of pastoral, spiritual and religious care within the NHS.
This guidance has been developed with the input of people from a wide range of faith and belief groups and backgrounds. I want personally to thank all those involved and all the people who continue to work with us in our shared goal of providing high quality and inclusive chaplaincy services within the NHS.
Dame Ruth May, Chief Nursing Officer for England.
Chaplaincy is a vital part of NHS care – for patients, for their families and carers, and for NHS staff. Chaplaincy services should be offered fairly and equally to everyone without discrimination.
A note on language
The terms ‘chaplaincy’ and ‘chaplain’ are used in these guidelines to reflect the profession, which is known as Healthcare Chaplaincy, and the existing main healthcare chaplaincy bodies in England, as listed in Appendix 2.
The term ‘chaplaincy’ is used in these guidelines to refer to the pastoral, spiritual and/or religious care and support that the NHS is expected to offer to all its users. For some, this has the connotation of the Christian tradition on which it was at one time based: however, by using this term in these guidelines we intend it to encompass care and support available to individuals of all religions and beliefs.
For clarity, where reference is made in these guidelines to ‘all religions and beliefs’, this encompasses non-religious beliefs and the absence of a religion or belief.
Those who practise chaplaincy are described in these guidelines as ‘chaplains’. Again, this is intended to refer to individuals who provide pastoral care, whether or not with a spiritual or religious dimension.
While the terms above have been adopted in these guidelines, NHS organisations should use the terminology that they feel will best be understood in their local contexts, provided that due consideration is given to inclusivity and equality. A glossary of terms can be found in Appendix 2.
Introduction
“The NHS provides a comprehensive service, available to all irrespective… of religion or belief”
“We value every person – whether patient, their families or carers, or staff – as an individual, respect their aspirations and commitments in life, and seek to understand their priorities, needs, abilities and limits.”
“Respect, dignity, compassion and care should be at the core of how patients and staff are treated not only because that is the right thing to do but because patient safety, experience and outcomes are all improved when staff are valued, empowered and supported.”
“We ensure that compassion is central to the care we provide and respond with humanity and kindness to each person’s pain, distress, anxiety or need. We search for the things we can do, however small, to give comfort and relieve suffering. We find time for patients, their families and carers, as well as those we work alongside. We do not wait to be asked, because we care.”
“We are compassionate and inclusive
We do not tolerate any form of discrimination, bullying or violence.
We are open and inclusive.
We make the NHS a place where we all feel we belong.”
To fulfil the commitment in the NHS Constitution to value every person, it is important that the NHS not only cares for people’s physical and mental health but also supports them with any spiritual, pastoral or religious needs they may have in relation to their care.
Patients may view their condition or illness in the context of how they view other aspects of their life, which may not be explained adequately through a biopsychosocial approach alone. The human elements of compassion, hope and understanding, and the relationship between carer and cared for can be a crucial element of the healing process.
In relation to those who work in the NHS, the NHS People Plan commits to practical actions that employers and systems should take, focusing on:
- looking after our people– with quality health and wellbeing support for everyone
- belonging in the NHS – with a particular focus on tackling the discrimination that some staff face
- new ways of working and delivering care – making effective use of the full range of our people’s skills and experience
- growing for the future – how we recruit and keep our people, and welcome back colleagues who want to return.
Providing resources for people in the NHS to receive pastoral, spiritual and religious care plays a part in this.
In this guide, we use the term ‘chaplaincy’ to describe pastoral, spiritual and/or religious care available to all, irrespective of religion or belief. NHS clinicians and others involved in caring for NHS patients may provide an element of such care, but the specialist role has traditionally been described as ‘chaplain’ and that is the term widely adopted internationally, both within and outside healthcare. In the NHS context, chaplaincy care should be available to everyone – without discrimination on grounds of age, disability, race, sex, sexual orientation, gender identity, or any other protected characteristic – and the term is understood to be inclusive of all religions and beliefs.
The purpose of these guidelines is to set out for NHS managers of chaplaincy services in England guidance on how to run and manage a safe, effective and inclusive chaplaincy service, with some examples of how NHS bodies across the country are operating such services. The guidelines are not intended to describe how chaplains should perform their duties. This edition replaces the last guidelines published in 2015, reflecting changes in society and the NHS since then. This edition is also written recognising the importance of chaplaincy services in the NHS during the COVID-19 pandemic, when chaplaincy support played an important part in supporting patients, families, carers and staff at a time of severe stress and trauma.
1.1 The role of chaplains
Chaplains promote pastoral, spiritual and religious wellbeing through skilled compassionate person-centred care for patients, their families and their carers, NHS staff, volunteers and students. Chaplains take an empathetic and reflexive approach, listening to each person’s unique story, and respecting what matters and is meaningful to the individual. This approach enables the pastoral, spiritual and religious needs of the individual to be understood and addressed.
Chaplains, with the appropriate authorisation, may perform rituals consistent with the individual’s religion or belief, such as those associated with birth, marriage or death. Chaplaincy services should be managed and run in such a way so as to enable such ceremonies or rituals to be performed by someone who shares the religion or belief of the person for whom they are being performed. They may also facilitate and lead collective ritual such as acts of remembrance and celebration.
Chaplains are often involved in the initial response to crisis situations and major incidents because of their pastoral skills. They provide support for people in distressing or traumatic situations when they are often at their most vulnerable such as pregnancy loss, sudden infant death, psychosis, self-harm, diagnosis of life-threatening conditions, and end of life care. Chaplains also provide support to NHS staff, students and volunteers involved in these situations and contribute to staff wellbeing and resilience initiatives such as meditation sessions and Schwartz Rounds.
Chaplains in the NHS often also contribute to the wider organisation and health and care system. They may sit on multidisciplinary care teams, management and leadership groups, ethics committees and EDI groups. Chaplains contribute to and lead training on pastoral, spiritual and religious care; they provide clinical supervision; contribute to safeguarding and the welfare of children and young people; conduct audits, service evaluations and research; and help plan for and provide support in emergencies or major health incidents. They may also sit on bodies such as Health and Wellbeing Boards; they may be members of charitable bodies and collaborate with other professionals in community settings and with chaplaincies in other sectors. Chaplains also connect with faith groups and belief communities which can help the organisation understand local needs and create opportunities to improve services and address health inequalities.
Note: Examples are included in these guidelines of how NHS bodies across the country are currently operating chaplaincy services. We recognise different approaches may be appropriate in different circumstances to best suit the populations being served.
2. Overarching principles
2.1 Equality, diversity and inclusion
NHS Organisations have a legal obligation to comply with the public sector equality duty both as employers and when providing services to the public. This requires NHS organisations to have due regard to the need to eliminate unlawful discrimination, harassment and victimisation, to advance equality of opportunity and to foster good relations between people who share a protected characteristic and those who do not. All care, including chaplaincy, should be made available equally and without discrimination to all patients, families and carers, and staff, regardless of any protected characteristic an individual may have (such as religion or belief).
Chaplaincy services should be based on the needs expressed by service users, not just service providers. NHS managers should play a key role in advancing the equality of opportunity and inclusivity of underrepresented groups in these services. Patients from a diverse range of backgrounds and those sharing protected characteristics, and those who do not, should be included in drawing up local policy and shaping the provision of services.
While chaplains are expected to support people of all religions and beliefs, chaplains from a particular religion or belief group may also deliver religious or belief-specific care for service users who seek their support. For example, a Catholic chaplain who may be appointed following an open recruitment process may provide Catholic liturgical services to patients, families and carers, and staff. Care for people who share the chaplain’s particular religion or belief cannot be the exclusive focus of their work, but nor must chaplains be expected to perform rituals or ceremonies from religions or traditions which are not their own or to give advice counter to their own beliefs. Chaplaincy services should be managed, resourced, and run in such a way to ensure that the service can be offered and provided to all, irrespective of individual chaplains’ religions or beliefs.
Some people understand ‘chaplain’ as a term linked to religion and particularly the Christian tradition. To avoid confusion, the addition of a prefix to denote the individual chaplain’s religion or belief system – such as Humanist chaplain, Jewish chaplain or Muslim chaplain – can be helpful.
In some cases there may be grounds for a post holder to have a particular protected characteristic under the Equality Act. In law, this is known as an ‘occupational requirement’ which may be a particular religion or philosophical belief, and this must be justified and proportionate to achieving a legitimate aim. An Equality Impact Assessment must be conducted before an occupational requirement can be determined.
2.2 Leadership
Each chaplaincy service should have a designated manager – sometimes referred to as lead chaplain, head of department or chaplaincy manager. This person is responsible for the delivery of a safe, effective and high-quality service that is well integrated within clinical services as set out in these guidelines.
It is recommended that an NHS organisation Board level champion is appointed to support the designated manager and act as an advocate of chaplaincy services at the Board. They would need to understand NHS chaplaincy but need not be a chaplain. The champion should have access to data and feedback on the service to support regular reviews of the service’s effectiveness, quality, accessibility and staffing.
As a person-centred service, it is recommended that chaplaincy be managed alongside other similar clinical services: this will often mean within an organisation’s Clinical Services, Nursing, Allied Health Professionals or Patient Experience Directorate or grouping. Given the role that chaplains play in supporting staff, it is also good practice for chaplains to work with HR departments to advance health and wellbeing.
2.3 Coordination and team working
To ensure that chaplaincy is integral to the holistic response to patient needs, it is good practice for chaplains to be included in Multidisciplinary Teams (MDTs) and other relevant provider meetings and forums. Some specialties, such as Palliative Care, specify the inclusion of chaplains in their MDTs.
It is good practice for chaplains to work as part of a chaplaincy team rather than as lone individuals and time and resource should be available for ongoing team development. Effective teamwork and compassionate leadership is particularly important for chaplains as it helps build the necessary safety, trust and mutual support to sustain them in their emotionally demanding role.
Chaplaincy should develop close working relationships with key departments such as bereavement services, given their frequent involvement with end-of-life care and their support of people who are bereaved. Chaplains can support patients with their funeral plans, and they can have a key role in funerals arranged by the NHS organisation. In these cases, for example in circumstances where there are no family or friends able or willing to make the funeral arrangements, appropriate consideration should be given to the religion or belief of the deceased patient where this is known.
Chaplains should work with Equality, Diversity and Inclusion (EDI) leads to ensure their services are open and inclusive. In particular, EDI leads can support chaplains to communicate the breadth and potential impact of their services. This should encourage uptake by all, irrespective of religion or belief, using language that is readily understood by both patients and staff and respectful to all.
2.4 Code of Conduct
To provide safe and effective care, chaplains must follow all relevant organisational policies for their place of employment and complete any relevant mandatory training for their organisation.
The UK Board of Healthcare Chaplaincy (UKBHC) operates a voluntary register, which is accredited by the Professional Standards Authority: registrants are required to meet the standards for competence, professional and ethical behaviour that are set out in its Code. NHS organisations should expect all chaplains, whether UKBHC registered or not, to abide by that Code.
For avoidance of doubt, NHS policies on Disclosure and Barring must be followed in relation to chaplains and chaplaincy volunteers, who may work closely from time to time with potentially vulnerable adults and children. Chaplains should also adhere to safeguarding policy within their organisation and undergo relevant training. The lead chaplain has a duty to ensure that the staff and volunteers in the service follow safe practice.
In accordance with NHS policies for record keeping, chaplains should keep clear and accurate records relevant to their practice, which not only supports safe and effective care, but also helps ensure continuity of care and MDT coordination, while providing evidence of their practice and decisions. Records, in whatever form they are kept, should be subject to audit against quality standards.
2.5 Quality assurance
Chaplaincy services should be subject to relevant quality assurance measures and governance processes to ensure effectiveness and safety. This should include methods of service evaluation and audit, the analysis of activity, learning from incidents and risk management. (see also Section 9 on Measurement and Evaluation)
As part of a learning culture it is good practice for managers to seek feedback on the work of chaplains and volunteers. It is recommended that managers/lead chaplains make occasional follow-up visits to patients, families, carers or staff who have received a visit from a chaplain or volunteer to seek their feedback and ask chaplains’ colleagues for any observations about the chaplain or the service. This can inform the appraisal process.
It is expected that chaplaincy will be included in Quality and Improvement committee reviews, for example to help shape the organisation’s work on patient safety, patient experience and effective patient care.
2.6 Information governance
In order to contribute to holistic patient care, chaplains require relevant information to carry out their duties. The chaplaincy department is subject to the same information governance (IG) considerations as apply elsewhere in the organisation. The organisation’s IG policy should cover the processing of data relating to a person’s spiritual, pastoral and religious care, as well as their physical and mental health.
Chaplains, including those on honorary contracts (see section 4.5), must complete regular training in IG and confidentiality, in a similar way to all other organisational employees, and a record must be kept of all training undertaken. Chaplaincy volunteers should also receive training on IG and confidentiality.
You can find more about IG and Chaplaincy on the NHS England website.
3. Staffing
Chaplaincy staffing requirements will vary from organisation to organisation and should be based on the principles of effective workforce planning. In so doing, managers should take account of the profile and needs of service users (including out-patients), working patterns (including any requirement to maintain round the clock or out-of-hours services), the job plans of staff, the overall functions and objectives of the department, and service user and staff outcomes. Planning should also ensure that the composition and focus of the team gives due regard to the religions and beliefs represented in the patient population.
Unless there is a demonstrable ‘occupational requirement’ (see chapter 4 on Recruitment), NHS organisations must not set out to recruit chaplains of a particular religion or belief: chaplaincy must be provided as an inclusive service.
It is good practice to allocate management/professional leadership time for the lead chaplain, and supervising chaplains based on the number of whole-time equivalent chaplains in the team, depending on circumstances in each provider organisation and recognising that small teams may require an increased allocation in order to meet organisational expectations. In particular, certain settings, such as palliative and end of life care, mental health services, community and specialist paediatric care, and primary and community care, may call for a different level of staffing and specific skills and experience relating to the complexity of needs in these disciplines – see chapter 10.
The chaplaincy team may comprise not only paid staff but also chaplains who have an honorary contract, and volunteers. It is often the case that organisations choose to have arrangements with volunteers from minority faith communities or other beliefs with relatively low local representation to support chaplaincy staff to meet the needs of all service users. Visiting ministers of religion or pastoral carers from belief groups specifically requested by patients do not generally form part of the team.
In planning the proportion of time chaplains have for the variety of activities required in their role, allowance should be made for chaplains to fulfil a range of tasks besides supporting people with their pastoral, spiritual and/or religious needs.
These include but are not limited to:
- Attending MDTs
- Liaising with health and social care staff to coordinate patient care
- Liaising with funeral directors and the bereaved and conducting funerals
- Supervising and training staff, volunteers and students on placement
- Providing training on pastoral, spiritual and religious care to healthcare professionals
- Managing the service
- Conducting research, audits and service evaluations
- Organising memorials
- Contributing to structured worship
- Providing on-call out-of-hours services
- Representing chaplaincy on Trust meetings and committees
- Travel between sites
- Supporting preparedness for and engaging with major incidents
- Undertaking continuing professional development (CPD)
- Giving and/or receiving supervision and engaging in reflective practice
3.1 Out-of-hours provision
Chaplaincy services should be made available outside of normal working hours by paid healthcare chaplains in organisations where urgent out-of-hours support is often requested (i.e. on average at least once a week). Out-of-hours use should be reviewed from time to time, to ensure that the service continues to be required, and consideration should take account of the size and location of sites. The on-call system should follow relevant local and national on-call guidance, terms and conditions and chaplains providing on-call should have sufficient training and experience to fulfil this duty. Where a 24/7 service is provided consideration must be made of the staffing needed to ensure that it is sustainable and that chaplains are not unduly burdened. Healthcare professionals should alert chaplains in advance when they believe that their services may be required out of hours.
It is good practice to aim for chaplains to reach patients within one hour when called in an emergency. When called, the on-call chaplain should assess the needs of the patient and provide the necessary care and support where they are able to do so. In situations where the patient has particular care and support needs as a result of their religion or beliefs that the on-call chaplain is unable to provide the on-call chaplain should where possible involve another chaplain who is able to provide that care and support. Alternatively, it may be possible to set up partnerships or service level agreements with local groups or communities to support an inclusive and equitable service according to service needs.
4. Recruitment
Chaplains may work either in paid roles or under contract but unpaid (honorary). This chapter considers recruitment of paid staff and honorary chaplains – see chapter 6 for volunteers.
Recruitment of paid chaplains and honorary chaplains (see section 4.5) should follow established good practice for NHS recruitment and should be in line with equality legislation. As for all NHS recruitment, employers must carry out pre-employment checks set out in NHS Employers’ Employment Standards.
Before any recruitment is undertaken, a full Equality Impact Assessment (EIA) should be completed to understand whether a post needs to be restricted. There is generally no need or justification for job descriptions and person specifications to specify that the post holder should be of a certain religion or beliefs, as chaplaincy services should be available to all irrespective of religion or belief. However, after completing a thorough Equality Impact Assessment, it may be decided that someone from a specific religion or belief group is required to do the job (known as an ‘occupational requirement’). Appropriate advice on the recruitment process should be obtained in such a situation and appointees should nevertheless meet the relevant capabilities and competences for the post.
The appointment process, including interviews, should be conducted by people who are appropriately qualified and consideration should be given to including a patient representative. It is recommended that an NHS manager and another healthcare professional sit on the appointment panel and at a level commensurate to the post being appointed to. It is not appropriate for a departing postholder to interview or appoint potential successors. It is also recommended that equality monitoring of recruitment data of the chaplaincy workforce is collated and reviewed in line with usual HR and recruitment practices.
The UK Board of Healthcare Chaplaincy (UKBHC) can provide professional appointment advisors to assist with the recruitment process from the outset, including sitting on an appointment panel, and their use is strongly recommended – particularly when recruiting lead chaplains.
4.1 Job descriptions and person specifications
Employers should expect chaplains to have experience as a leader in their own religion or belief, experience of spiritual and pastoral care and usually a degree or a professional qualification.
Paid chaplains are employed in the NHS under the terms and conditions of Agenda for Change (AfC), which includes national job profiles. Three chaplaincy-specific profiles have been published:
|
Profile |
AfC band |
|
Chaplain Entry Level |
5 |
|
Chaplain |
6 |
|
Chaplain Team Manager |
7 |
UKBHC sets out definitions as follows:
|
Level |
Role |
|
Chaplain Band 5 |
A practitioner with limited autonomy, who works as part of a chaplaincy team and is supervised by a chaplain Band 6 or above. |
|
Chaplain Band 6 |
An autonomous, qualified practitioner whose role is to seek out and respond to the spiritual and religious needs of individuals, their carers and staff. |
|
Lead Chaplain Band 7 (L) |
A chaplain with additional responsibilities and experience including the management of a chaplaincy team |
|
Specialist Chaplain Band 7 (H) |
A chaplain with advanced specialist knowledge, experience and expertise in a particular aspect of healthcare chaplaincy. For example: acute, mental health, paediatrics, palliative care. |
|
Consultant Lead Chaplain Band 8 |
A chaplain with management responsibility for spiritual and religious care policy and services across an NHS Trust or Health Board Area. |
Other national job profiles may apply to certain chaplaincy roles such as Professional Manager or Clinical Researcher.
It should be noted that Band 5 posts are intended for trainees and that adequate training resources, protected learning time and supervision should be available when recruiting at this level.
4.2 Advertising
Vacancies must be openly advertised. It is recommended that roles are advertised through the NHS Jobs website as this promotes equality and diversity in recruitment. Other media may also be useful to attract a wide range of applicants. Where an occupational requirement has been proven, jobs may also be advertised in specialist publications.
4.3 Evidence of suitability
Applicants should provide evidence of their knowledge, training, experience and competence to meet the requirements of the role. Employers may ask for some experience in healthcare work, which could be, for example, from hospital visiting while working as a faith leader elsewhere. Providing pastoral care for people in a faith community setting or in other areas of NHS care, however, is not on its own necessarily sufficient to demonstrate suitability.
UKBHC’s Healthcare Chaplaincy Bands and Duties Framework sets out the following qualifications for chaplains:
|
Job title |
Qualifications |
|
Chaplains (Band 5) |
Degree in healthcare chaplaincy (or equivalent) |
|
Chaplains (Band 6) |
Postgraduate certificate/diploma in healthcare chaplaincy |
|
Lead Chaplains (Band 7) |
Masters in healthcare chaplaincy and five years’ experience in healthcare chaplaincy |
|
Consultant Lead Chaplains (Band 8) |
Master’s or PhD in Healthcare Chaplaincy and minimum 3-5 years’ experience in a senior Band 7 role with demonstrable ability in quality improvement, service development, and strategic leadership.
|
While these qualifications are desirable, they are currently not a statutory requirement, and from an equalities perspective, the employer may recognise other qualifications and professional experience as equivalent: this might be a degree in psychology or sociology, for example, or training gained in other jurisdictions such as Clinical Pastoral Education programmes in the USA, Canada, Australia or New Zealand. For first appointments at Band 5 level, evidence of previous healthcare experience, e.g. as a volunteer within a healthcare chaplaincy department, is desirable.
A selection process should be based on evaluating the essential and desirable knowledge, skills, values and behaviours stated in the person specification (PS). A successful selection process may include not only questions from a panel but also clinical simulations consisting of a chaplain-patient encounter observed by those experienced in chaplaincy. The simulation may be followed by time for the candidate to give a written reflection about the chaplain-patient encounter. At Head of Chaplaincy level, the process could include a presentation to a multidisciplinary audience, stakeholder panels and written work.
While candidates must be willing and able to ensure the provision of chaplaincy services to support people of all religions and beliefs, it is expected that, prior to appointment, the employer seeks endorsement, where possible, from the religion or belief community of the desired candidate if possible. (Some belief groups, such as the Church of England and the Catholic Church, may require that candidates intending to practise as chaplains have licences or mandates from them.) A copy of the job description (JD) and person specification should be provided so that the endorsing body can have a good understanding of the duties and requirements related to the specific role for which the candidate has applied. Endorsement should state that the candidate is of good standing, is deemed safe to practise, and that the candidate has the religion or belief characteristics that they claim.
The Network for Pastoral, Spiritual and Religious Care in Health (NPSRCH) maintains a register of religion or belief groups, each of which has the ability to provide endorsements for chaplaincy candidates. Where a religion or belief group is not registered there, application should be made to the head office of the organisation concerned.
Note that endorsement on its own is not sufficient for evidence of suitability or competence for the role.
4.4 Registration
UKBHC maintains a voluntary register of chaplains accredited by the Professional Standards Authority. Registrants are required to meet the standards for competence, professional and ethical behaviour that are set out in its Code. NHS organisations should expect all chaplains, whether UKBHC registered or not, to abide by that Code.
4.5 Honorary chaplains
An honorary contract may be used for a chaplain not directly employed by the NHS organisation but who carries out authorised but unpaid chaplaincy work in a prescribed role, such as to provide religion or belief-specific duties for small patient populations or those who present infrequently. Honorary chaplains should not replace the role of a paid chaplain in a chaplaincy service but extend the core provision already in place and contracts should be issued only for fixed time periods. Honorary contracts should not be used for chaplaincy volunteers, unpaid placements or work experience opportunities.
Where suitably experienced members of faith communities or belief groups are recruited to act as honorary chaplains, it is required that they meet the standards expected of paid chaplains in that role. It is also essential that they have an explicit agreement covering the extent of the role and its limits. They should be endorsed by their religion or belief community where possible and should receive an equivalent level of training and supervision to paid chaplains.
Recruitment of honorary chaplain posts should follow the same good practice used in the NHS (see above). If hosting an honorary chaplain employed elsewhere, NHS hosting organisations should ensure that they have the necessary assurances from the proposed honorary chaplain’s employer that the appropriate employment clearances, including identity checks, have been conducted in compliance with the NHS Employment Check standards. In cases where there is no other employer, the host organisation should ensure that all checks are undertaken to a satisfactory standard.
5. Training and support
Chaplains are expected to have received training and a suitable level of professional development and practical experience in pastoral, spiritual or religious care, typically within their religion or belief tradition, before being appointed. However, the context of working in the NHS is different in many ways and newly appointed chaplains should receive an extensive induction and be supported by an experienced practitioner to develop their confidence and capability of working in the NHS.
After appointment, employers should ensure that chaplains undertake CPD and receive regular appraisal and supervision, with their training needs identified as part of their annual appraisal. This will support chaplains to become effective in their role, work safely within the NHS and sustain the capabilities necessary to care for people at times of vulnerability, suffering and death. Job descriptions, job plans and budgeting should allow for this. Employers will also have their own mandatory training with which all staff, including chaplains, will be expected to comply.
NHS employers should offer or provide access to training in subjects allied to chaplaincy for chaplains to attend. It is recommended that this includes but is not limited to training in how the organisation works, service improvement, teamworking, communication skills, cultural competence, mental capacity, record keeping, major incidents, and palliative and end of life care. Chaplains should be made aware of opportunities to work across directorates to build a breadth of knowledge of the organisation.
5.1 Supervision
Entry level chaplains (Band 5) should receive regular management and clinical supervision and be offered opportunities for work shadowing, mentoring and reflection, during which significant aspects of their work can be discussed as a means of learning, enhancing reflexivity and developing their professional identity and capability.
Chaplains (Band 6 or above) should receive regular clinical supervision from another suitably qualified person – preferably neither within their department nor their line manager – to enable them to reflect carefully on the spiritual assessment and interventions they carry out. This recognises the burden of chaplaincy and the high level of responsibility that chaplains have towards their service users, staff and their organisation. In instances where there is no suitable supervisor within the setting or organisation then a suitable supervisor will need to be identified from outside their immediate organisation.
Good practice is for sessions to use anonymised case discussion to facilitate learning, reflective practice, managing of boundaries, avoidance of dependence and attention to safeguarding issues or general safe practice. They can be individual or group sessions and can be conducted in person or online. Both the Association for Pastoral Supervision and Education and The Institute of Pastoral Supervision & Reflective Practice set standards in this area.
5.2 Continuing professional development
Healthcare chaplains should engage in a programme of CPD, which may include attending external training/degree courses and study conferences, such as those provided for members by the College of Health Care Chaplains (CHCC) or other recognised chaplaincy bodies (see Appendix 2). Such CPD should be recorded and may enable career progression, which is to be encouraged.
Collaboration between chaplains in different healthcare settings or locations can be valuable to develop professional skills. Chaplains should be supported to attend and contribute to relevant professional networks.
In the North and Midlands, lead chaplains meet monthly and other chaplains quarterly to support each other. This includes time for peer reflection on what is working and what needs further consideration; training sessions provided by peers; and collaboration on research. Chaplains from specific faith groups but from different sectors, such as prisons and universities, meet with healthcare chaplains to develop professional practice.
5.3 Research
Research produces new knowledge and insights that can help improve practice and bring benefits to patients and those who chaplaincy supports. It is good practice therefore to encourage chaplains to develop their knowledge and skills in research including the ability to critically interpret and translate findings into practice. The UKBHC has a Research Standard to guide the conduct of research in chaplaincy.
6. Volunteers
Volunteers can add significant value to chaplaincy provision in all sorts of support roles. They should be regarded as complementary to rather than replacements for substantive posts, but it is good practice to consider the diversity of volunteers alongside those in substantive roles. As with all volunteers in the NHS, it is important that they are properly selected, recruited and trained and are subject to appropriate management and supervision. General guidance may be found in Recruiting and Managing Volunteers in NHS Providers – a practical guide.
6.1 Recruiting volunteers
Chaplaincy volunteers are often recruited on a trial basis to give them and their manager(s) a chance to see if they are suited to chaplaincy practice. It is recommended that a review is held after the first three months so that each party can determine whether there is a good fit.
A volunteer agreement should be provided to candidates recruited as volunteers, which they should read and sign.
Whilst the chaplaincy service will manage and support the day to day activities of chaplaincy volunteers, managers of chaplaincy services should link with their organisation’s Volunteer Service Manager who can advise and support with the recruitment, training and support of volunteers. It is good practice to use positive action to recruit volunteers of all religions and beliefs.
6.2 Supervision
Volunteers, who must receive an induction when they start, should be supervised by a chaplain (Band 6 or above). After appointment, they must complete relevant mandatory training, which must include equality, diversity and inclusion (EDI), safeguarding and IG training. It is expected that they attend at least one annual training event focusing on safe chaplaincy practice and they should be encouraged to engage in supervision and reflective practice appropriate to their role, which has been shown to improve service user outcomes.
7. Raising awareness and understanding
A chaplaincy service can be valuable only if patients, families, carers and staff are aware of it and understand what it offers. It is therefore important that NHS managers responsible for the chaplaincy service in their setting ensure that information about it is communicated in the right way, at the right time and in the right place.
7.1 The right way
The chaplaincy service should be described in a way that people easily understand. The phrase “It’s good to talk, so we’re here to listen”, for example, may be a good introduction on publicity material.
Chaplains (including honorary chaplains) can make their services known, for example by walking around in an acute setting and talking to patients, their families and carers. It should be made clear that the service is for everyone, whatever their belief or religion.
Special consideration should be given to the provision of information about chaplaincy in different languages and formats. For example, by providing easy-read or pictorial information for people with poor literacy or a learning disability.
It should be made clear that staff, patients, families and carers may self-refer to a chaplaincy service. Clinical staff should also be trained how to introduce and describe the service to patients, families or carers and how to refer them.
The chaplaincy service should make people aware that in addition to providing chaplaincy care and support services, they are there to support people to practise and express their religion or beliefs while in hospital, including observing religious festivals/dates, with adjustments made as necessary to ensure they can participate. For example, if a patient is unable to attend a ceremony usually performed in a place of worship, it is expected that the chaplaincy service make it possible for it to be conducted in the healthcare setting if feasible. Similarly, the service should support patients who wish to fast for religious reasons where this would not compromise their physical care.
The provision of chapels, prayer rooms, quiet rooms and other spaces should be made known to service users and staff. If only one area is designated for service user and staff use, it should be described in inclusive terms, for example ‘room for reflection’ or ‘quiet room’, to avoid suggesting that it is for use only by people of particular religious or other beliefs. An additional space designated for multi-faith use, if required, may be described as such.
7.2 The right time
Service users should be made aware of a chaplaincy service when appropriate: this may be on admission as an in-patient, but may be at other times, such as when booking surgery or following the breaking of bad news, for example.
It is strongly recommended that all staff be made aware of the service as part of their induction and be reminded about it from time to time – especially if major incidents occur or if, for example, there is an unexpected staff death.
Clinical and other relevant staff should be trained in relevant screening and know how to refer to the chaplaincy service at all times. It is good practice to note consent as part of any record of referral kept.
It is good practice for the chaplaincy department to keep managers and staff informed about a calendar of religious and belief festivals.
7.3 The right place
It is good practice for information or publicity about a chaplaincy service to be made available online and offline in places where patients, families, carers and staff are likely to see it. Formats may include posters, leaflets, ‘tent cards’, references in newsletters, blogs or social media, videos and pages on the organisation’s website. Organisations are encouraged to develop versions in languages other than English suitable to their patient population.
An app to enable chaplaincy services to be accessed from a mobile phone has been developed by Bradford Teaching Hospitals NHS Foundation Trust, and the Trust welcomes enquiries about it via SPaRCteam@bthft.nhs.uk.
8. Facilities
8.1 Office space
Chaplains require office space, phones and networked computers, and these should always be provided. Administrative support and data should also be provided where relevant. Chaplains must have access when necessary to confidential working space, such as an office, where they can offer one-to-one support to carers, friends and families and staff.
8.2 Chapels, prayer rooms, multi-faith spaces and quiet rooms
To meet human rights and equalities requirements, it is good practice to provide suitable and fully accessible spaces for individual and collective religious or belief practices and observances, and spaces for spiritual refuge, contemplation, meditation and reflection. It is advised that these rooms be located close to clinical practice areas so that patients and staff can attend without difficulty.
The design and provision of spaces should give due regard to the diversity of religions and belief needs in the population served, such as provision of ablution facilities. Some organisations make available holy books or guidance examples for prayer and reflection. Rooms should contain storage or screens for religious artefacts and facilities, so that they can be reset for others after use.
Spaces that are shared by different belief groups or faith communities need to feel useable and welcome to all whilst being able to meet specific needs at certain points in the day or times of the year (e.g. Muslim prayer times). Facilities therefore should be managed to ensure that respectful cooperation among all users can be achieved and the faith communities and belief groups should be consulted and involved. For example, retrofitted chapels may not be appropriate as quiet rooms for use by people with non-religious beliefs or people of certain faiths. In this case, a separate space may be required and designated as a ‘quiet room’, ‘sanctuary’ or ‘room for reflection’.
9. Measurement and evaluation
It is strongly recommended that NHS organisations evaluate the chaplaincy service in a similar way to other clinical disciplines and to report on this in their annual report and quality accounts. Regular reviews by those managing Chaplaincy services, as well as others that may champion the service, can also be used to make planning decisions about the scope of the service, resourcing, workforce and facilities.
Quantitative measures (e.g. referrals, numbers and type of interactions by chaplains, lengths of contacts, response times) have a part to play and should be collected and reported. Qualitative information on user experience/ outcomes is also important to help assess the impact of the service and to guide its development.
Bradford Teaching Hospitals NHS Foundation Trust keeps records of incidence, location and nature of interactions which yield quantitative data. Qualitative data is recorded (as case studies, reflective accounts, feedback from families, survey responses, intervention summaries, etc.) in order to analyse expressions of need and range of responses. Data is used for service review, to measure impact, to monitor inequalities, trends and performance, to review staffing and volunteering, to allocate resources and to support research activities.
University Hospitals of Leicester NHS Trust produces an Annual Report in which it records a wide range of quantitative data. It also builds a picture of the activities of the chaplaincy department by including items such as:
- training delivered by chaplains to staff, communities and volunteers
- testimonials from patients and staff
- events held e.g. Eid, Christmas and Diwali celebrations and memorial services
- resources created e.g. MP3 versions of prayer for use on wards
- training, development and research undertaken by members of the department
- a list of staff members’ wider responsibilities
It is strongly recommended that feedback on the chaplaincy service is sought from patients, families and carers, and staff. Organisations may wish to include questions about it in patient and staff surveys, such as the Friends and Family Test, provided they have the means to analyse the results.
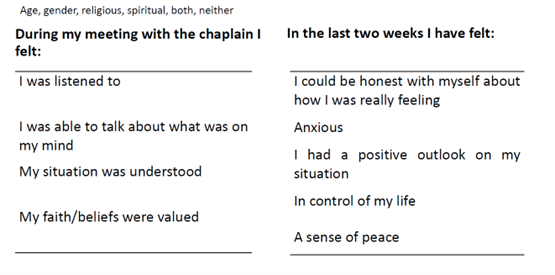
The Scottish Patient Reported Outcome Measures (PROMs) is a measure that has been used successfully to assess the impact of chaplaincy interventions.
9.1 Complaints
If a member of the public has a concern about a chaplain or the chaplaincy service, they should follow the NHS patient complaints procedure and in the first instance raise the matter locally using the organisation’s standard complaints or whistleblowing process. Staff should follow the provider’s complaints procedure.
Complaints against chaplains registered with UKBHC should be reported to that body.
Any upheld complaints should be reported to the endorsing religion or belief group of the individual concerned and any other relevant professional bodies, which will have their own codes of conduct and processes to follow.
9.2 Regulation
The Care Quality Commission (CQC) notes that everyone has the right to expect person-centred care that meets their needs and preferences, and to be treated equally with dignity and respect. It is committed to regulating to advance equality and protect people’s Human Rights.
CQC checks whether “staff understand and respect the personal, cultural, social and religious needs of people and how these may relate to care needs, and … take these into account in the way they deliver services.” It also assesses whether “people [are] given appropriate and timely support and information to cope emotionally with their care, treatment or condition”. The CQC Inspection Framework for End of Life Care requires inspectors to check how services provide psychological, social and spiritual support to patients at the end of life. NHS organisations should have robust and well-implemented chaplaincy policies and procedures, against which the CQC can evaluate service provision.
The NHS Standard Contract states that providers must take account of the spiritual, religious, pastoral and cultural needs of service users and that NHS Trusts and NHS Foundation Trusts must have regard to these NHS chaplaincy guidelines.
10. Specialist settings
All chaplains work in complex contexts, but the complexity and specialist skills required vary depending on context. Certain settings may require additional considerations in relation to the provision of chaplaincy services. As well as specialist training and skills to support people in these settings, this may affect the recommended ratio of chaplaincy staff to service users – see Appendix 1.
10.1 Specialist palliative and end of life care
‘One chance to get it right’, the independent report published by DHSC on how health and care organisations should care for people in the last days of their life, contains priorities for care of the dying person. These include:
- “An individual plan of care, which includes food and drink, symptom control and psychological, social and spiritual support, is agreed, coordinated and delivered with compassion.”
- “The dying person, and those identified as important to them, are involved in decisions about treatment and care to the extent that the dying person wants.”
- “The needs of families and others identified as important to the dying person are actively explored, respected and met as far as possible.”
The role of chaplains is identified in relation to all of these as part of the MDT.
The report also notes:
- “When specialist spiritual/religious support is identified as required, health and care staff must ensure that the dying person, and those important to them, have ready access to information about the available chaplaincy and/or spiritual care provision.”
- “The chaplains must have information about local faith leaders to enable, where requested by the person, referral to church or faith community leaders.”
- “Staff must find out from the dying person, their family and those important to them, the details of any cultural or religious-specific requirements, including what constitutes respectful treatment of the body after death.”
In designing or reviewing a chaplaincy service in a palliative care setting, accurate information about patients’ religious or non-religious beliefs, as well as their pastoral and spiritual needs, should be considered carefully.
Job planning should take into account a chaplaincy department’s commitment to out-patient, day therapy and community services including domiciliary settings. Chaplains will be regularly involved in supporting patients’ families pre-bereavement and in many instances will play a significant role in bereavement care, including in the arrangements for patients’ funerals and the organisation and conduct of memorial services and related events.
The Association of Hospice and Palliative Care Chaplains (AHPCC) seeks to identify and promote good practice in providing chaplaincy at the end of life and provides study conferences for chaplains working in a palliative care environment. It is not required that NHS organisations employ a dedicated specialist palliative chaplain, but all chaplains should be skilled in this area whatever the context of their work or their organisation. Chaplains must, however, be able to call on a network of chaplaincy volunteers or local faith or belief groups to serve the needs of patients with specific beliefs so that appropriate customs at the end of life can be observed and respected
It is good practice for hospice chaplains to follow these NHS guidelines, even though they may be funded partly by the NHS and partly by independent hospice charities.
10.2 Mental health services
Service users in mental health often want help to make sense of what’s happening to them and why. People can struggle with their identity and their purpose and sometimes need support and guidance with managing difficulties in relationships and with guilt from past or current actions and events. Social problems such as housing difficulties, poverty and isolation are not uncommon as well as emotional difficulties or needs. It is therefore important for chaplains in mental health to be skilled in pastoral care and counselling and to be adaptive in response to their users’ broader welfare needs. Chaplains can address service users’ pastoral, spiritual or religious concerns, and often reduce a sense of isolation, increase resilience and play a part in their recovery. They can also support families and carers.
Most mental health chaplaincy work can be undertaken without requiring a specific religious or belief background from the chaplain, but people with mental illness often express a wish to receive care from a chaplain of their own religion or belief system or gender, and it is good practice to make provision for this.
Chaplains working in mental health settings often have long-term relationships with service users, given the ongoing care needs for people with enduring mental health conditions and the potential for readmission to an in-patient unit following a relapse. The relationship the service user has with the chaplain is often built up and founded on trust over many years, leading potentially to a distinctive dimension to mental health chaplaincy. Whilst some service users will still require more episodic care interventions, to ensure consistency of care for those needing longer term interventions, it is good practice for NHS organisations with long-term mental health service users to employ their own mental health chaplains who ensure a personalised care approach is taken.
Many service users, including those detained or treated under the Mental Health Act, may not trust the institution responsible for their care and can be wary of their prescribed medication and their care team in general. They may, however, regard chaplains as ‘allies’ who will not ‘impose’ treatment on them. Consequently, chaplains must exercise skill in how they conduct themselves as part of a multidisciplinary team.
For chaplains working in Children and Adolescent Mental Health Services (CAMHS), the considerations that apply to paediatric care (see 10.3) may also apply. Similarly for Children and Young People (CYP) moving between CYP and Adult Mental Health (AMH) services, the principles of transition may need to be considered.
In all engagements with service users, chaplains must recognise the vulnerability and inherent risk of the people they work alongside, including their increased risk of experiencing abuse or harm from others. Chaplains in mental health require training in working with people who may also present a risk of harming themselves or others and who may be susceptible to suicidal ideation. Since chaplains can often find themselves working alone when seeing service users in the community, managers should ensure they recognise the need for vigilance as well as maintaining professional boundaries.
Given these complexities, chaplains working in mental health settings need time not only for preparation in their service user and possibly family engagement but also for ‘decompression’. Supervision separate from line management should always be put in place. Volunteers in these settings should also be given additional support and be in receipt of pastoral supervision on a regular basis. Job plans and descriptions should consider not only the time needed for preparation and supervision, but also allow for the extra time needed to visit patients or service users in the community (see Appendix 1).
Given that chaplains in mental health often have a wide overview of services because of their visits across its different settings, they can often provide useful insights at Board level.
Note: Only chaplains who are qualified counsellors or therapists are permitted to conduct counselling/therapy. If qualified counselling or therapy is needed, chaplains who are not qualified in this way should make an onward referral to the appropriate service. Any decisions for therapy should be discussed with the treating MDT to ensure clear roles and responsibilities and avoid overlap or confusion in interventions the person is receiving.
10.3 Specialist paediatric care
Specialist paediatric care can be found in specialist hospitals, acute wards, residential units in Children and Adolescent Mental Health Services (CAMHS), community provision and hospices. Meeting the spiritual needs of younger people and children requires highly skilled care – some children may be too young to have a firm belief framework of their own and chaplains should also be cognisant that children and young people might have a different religion or belief from their parents or guardians, sometimes they may not feel able to share this in the presence of family/ guardians. Chaplains working in specialist paediatric units require enhanced training tailored to this context and taking account of ethical and safeguarding considerations as well as issues of capacity and consent.
It is recommended that chaplains working with children and young people have a good understanding of child development, family systems and family dynamics and social factors, to allow them to interpret the wishes of the service user and the views of their family/ care givers and friends in relation to religion, belief and spirituality. The age of the patients means that sustained support to the family may also be needed. When supporting children or young people in Mental Health settings it is important to work with the network around the child or young person.
Engaging with the spiritual needs of children and young people requires highly skilled and imaginative care, sometimes involving forms of play as an intervention. It is important to have skills to engage with both verbal and non-verbal children/young people across the developmental age range.
A PGC in Paediatric and Maternity Chaplaincy is available from the Centre for Paediatric Spiritual Care at Birmingham Children’s Hospital through Newman University. Accredited modules at level four and level seven in spiritual care and paediatric chaplaincy-related topics are available at Staffordshire University.
Volunteers will need to be suitable and comfortable to work with young people, including those with life-limiting conditions and their families/care givers.
10.4 Primary and community care
Chaplaincy in primary and community care is relatively less well developed but there are examples of good practice. In Coventry & Warwickshire for example, a chaplaincy-led project was established to tackle self-harm in the community.
As well as providing support to patients – including people with mental health conditions being cared for in the community – and their families and carers, chaplains in primary and community care can also play an important role in supporting staff.
Some GP practices provide a chaplaincy service, but this is a relatively recent development and one that is encouraged. If such a service is introduced, it is recommended that particular effort is put into making staff and patients aware of it and how to access it.
The Association of Chaplaincy in General Practice (ACGP) facilitates the setting up of this service within General Practices and provides advice on training and professional support. There are also examples of good practice in Scotland – for example at NHS Tayside.
Primary and community care services are encouraged to explore the possibilities for providing chaplaincy remotely, using videoconferencing and other forms of new technology. It is envisaged that this may enable isolated patients and service users who are part of smaller religious or belief communities to be supported and valued. Nevertheless, it should be remembered that some people may be unable to use or access the technology, so it will not necessarily be suitable for everyone.
10.5 Ambulance trusts
The provision of chaplaincy in ambulance trusts differs across the country, with varying access routes and levels of staffing in place to support patients, staff and volunteers. Some ambulance trusts have agreements with local hospital trusts to access their chaplaincy services. Since the COVID-19 pandemic, a number of ambulance trusts have reviewed their approach to chaplaincy services and as a result are undertaking pilots as a renewed commitment to providing pastoral, spiritual and religious care to front-line staff.
Appendix 1 – Healthcare chaplaincy bodies
The main healthcare chaplaincy bodies in England offer further guidance on good practice. A list is provided below.
- Association of Chaplaincy in General Practice
- Association of Hospice and Palliative Care Chaplains
- Association for Pastoral Supervision and Education
- College of Health Care Chaplains
- The Institute of Pastoral Supervision and Reflective Practice
- Network for Pastoral, Spiritual and Religious Care in Health
- Non-Religious Pastoral Support Network
- UK Board of Healthcare Chaplaincy
Appendix 2 – Glossary
| ACGP | Association of Chaplaincy in General Practice |
AfC | Agenda for Change |
| AHPCC | |
| Belief | Includes non-religious belief |
| CAMHS | Children and Adolescent Mental Health Services |
| Chaplain | An individual who provides pastoral care, whether or not with a spiritual or religious dimension |
| Chaplaincy |
Inclusive of pastoral, spiritual and/or religious care |
|
CHCC | |
| CPD | Continuing professional development |
|
CQC | |
|
DHSC | Department of Health and Social Care |
| EIA | Equality Impact Assessment |
| E&D | Equality and diversity |
| EDI | Equality, diversity and inclusion |
|
Faith | Religion |
|
FTE | Full-time equivalent |
|
Honorary | Unpaid |
|
IG | Information governance |
|
Inclusive | Encompassing all religions and beliefs and without discrimination on grounds of any protected characteristic |
|
JD | Job description |
|
MDT | Multidisciplinary Team |
|
NICU | New-born Intensive Care Unit |
|
NPSRCH | Network for Pastoral, Spiritual and Religious Care in Health |
|
PICU | Psychiatric Intensive Care Unit |
|
PROM | Patient Reported Outcome Measure |
|
Protected characteristics
| Age, disability, race, sex, sexual orientation, gender identity, religion or belief, marriage/civil partnership, pregnancy and maternity |
|
PS | Person specification |
|
PSED | Public Sector Equality Duty |
|
Schwartz rounds | A forum where all staff (clinical and non-clinical) can come together regularly to discuss the emotional and social aspects of working in healthcare |
|
UKBHC |
Publication reference: PR1073