Foreword
Every year, NHS providers produce approximately 156,000 tonnes of clinical waste that is either sent to high temperature incineration (HTI) or for alternative treatment (AT), which is equivalent to over 400 loaded jumbo jets of waste. This has a significant environmental impact and is associated with high running costs and carbon emissions.
Therefore, as one of the largest producers of waste in the country, it is vital that the NHS disposes it in a safe, efficient and sustainable manner, and we are only creating waste when absolutely necessary.
This clinical waste strategy has been created to support NHS providers in making the necessary step change in waste management practices. It is part of a suite of documents including the HTM 07-01 and the NHS waste planning tool, developed to help set the direction, trajectory, and speed of change necessary to reach the NHS target of net zero for direct carbon emissions by 2040, and net zero for indirect carbon emissions by 2045, and to ensure the NHS is using its resources effectively.
The best waste management practices reduce waste, improve compliance, and can lead to significant cost savings from lower waste volumes. They also have a significant part to play in minimising harm to the environment and increasing resource utilisation. This all leads to a reduction in carbon generated from waste and saving taxpayers money.
This strategy also encourages the use of innovation to increase NHS waste management resilience, improved data use to help guide decision making, and improved staff engagement and training to improve compliance and seek out carbon reduction opportunities in the system.
In our journey to reduce waste to an absolute minimum, there will be many opportunities to review the materials we use and to find ways of re-using, remanufacturing, or recycling, thus turning them into valuable resources for future use.
Most importantly, by implementing this strategy over the next 10 years, we estimate that the NHS can save approximately £11 million every year in recurrent revenue costs and we can reduce our carbon emissions from waste by approximately 30% – equivalent to removing 2 million road miles a year.
I encourage all NHS providers to embrace and adopt this strategy and embed the steps from the action plan as part of their daily waste management practices.
Simon Corben, Director of Estates and Head of Profession, NHS England.
1. Executive summary
It is a legal requirement for NHS providers to comply with waste legislation and regulations. Doing so ensures that waste is minimised, treated, and disposed of in a safe way that minimises environmental harm and thus protects patients, staff, the NHS, and the wider community.
This clinical waste strategy aims to improve waste management practices amongst NHS trusts, NHS foundation trusts and primary care (referred to collectively as ‘providers’ unless specified individually) to make them more efficient and sustainable in order to save on cost, improve hospital function, and reduce the impact on the environment in line with NHS net zero carbon commitments. This will be achieved through fostering improvement in six key areas of focus: data, workforce, compliance, commercial, infrastructure and sustainability. This strategy details the planned key activities and key performance indicators for progress in each of these areas and provides a background for why they are important.
This is a rolling 10 year strategy, with annual reviews and implementation plans for one and three years ahead. The strategy primarily covers the management plans for clinical and offensive waste from NHS providers in England. However, in reference to sustainability and net zero carbon objectives, the strategy is relevant to all waste types produced by NHS services.
- We estimate that implementing this strategy save the NHS up to £11 million in recurrent revenue costs (15% of current expenditure, based on Estates Return Information Collection (ERIC) figures 2020/21), 29,540 tonnes a year of whole-life CO2e (around 30% of the CO2 from this area) and an estimated 2 million road miles a year.
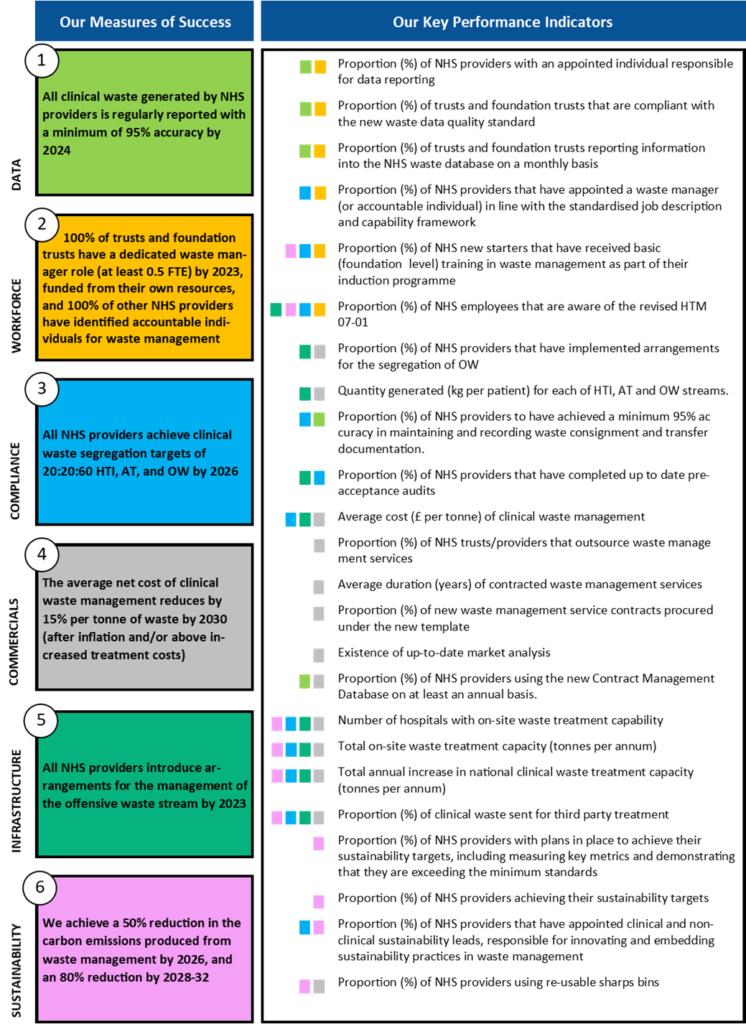
Figure 1 summarises the key areas of priority, intervention, and measurement set out to deliver on the six key areas of focus in this strategy. It is followed by figure 2, an indicative timeline of target dates for the strategy’s measures of success.
Further detail on the data, context, and research informing the actions and targets in this document can be found in the appendices to the NHS Clinical Waste Strategy.
Figure 1: Summary of relationships between areas of intervention and measurement detailed in the NHS Clinical Waste Strategy.
The image is a table showing how the themes, areas, strategic priorities, key activities and KPIs, and measures of success relate to each other.
There are three main themes: Productivity, Resilience and Net Zero Carbon. 6 areas come under these themes. In productivity, there is data, workforce and compliance. In resilience, there is commercials and infrastructure, and in net zero carbon, there is sustainability. Each of the 6 areas have an associated strategic priority and measure of success. The table also indicates that there is a selection of key activities and key performance indicators relating to each strategic priority and measure of success. These are not individually detailed in the table.
1. Data:
Strategic priority: Use better data (Utilise comprehensive, consistent data from across all NHS organisations/ICSs to drive decision-making and proactive risk management)
Measure of success: All clinical waste generated by NHS providers is regularly reported with a minimum of 95% accuracy by 2024.
2. Workforce:
Strategic priority: Invest in a skilled workforce (Invest in developing a skilled and diverse waste management workforce with appropriate support and defined career paths).
Measure of success: 100% of NHS trusts and foundation trusts have a dedicated waste manager role (at least 0.5 FTE) by 2023, funded from their own resources, and 100% of other NHS providers have identified accountable individuals for waste management.
3. Compliance:
Strategic priority: Improve our ability to comply (Ensure all NHS staff understand and adhere to compliance requirements)
Measure of success: NHS providers achieve clinical waste segregation targets of 20:20:60 HTI (High temperature incineration) AT (alternative treatment) and OW (offensive waste) by 2026.
4. Commercial
Strategic priority: Establish a commercial model that delivers better value (support the standardisation of contracting arrangement and develop a commercial model which encourages health market conditions).
Measure of success: The average net cost of clinical waste management reduces by 15% per tonne of waste by 2030 (after inflation and/or above increased treatment costs)
5. Infrastructure
Strategic priority: Develop resilient infrastructure that meets future demand (invest in clinical waste infrastructure to increase capacity and regional resilience and support sustainable waste processing practices)
Measure of puccess: All NHS providers introduce arrangements for the management of the offensive waste stream by 2023.
6. Sustainability
Strategic priority: Improve our use of resources and reduce carbon impact (proactively work to reduce harmful emissions, improve local air quality, and achieve the 2045 net zero carbon target).
Measure of success: We achieve a 50% reduction in the carbon emissions produced from waste management by 2026, and an 80% reduction by 2028-32.
Figure 2: Measures of success by target date (indicative timings only).
This figure is a chronological timeline of the NHS Clinical Waste Strategy measures of success and their target dates, spanning from 2023 to 2030. The measures of success are colour-coded to show which area they relate to. (data (light green), workforce (orange), compliance (blue), infrastructure (dark green), commercials (grey) and sustainability (pink).
- 2023: 100% of NHS trusts and foundation trusts have dedicated waste managers (at least 0.5 FTE) with accountable individuals for waste management identified across all providers. (Area: Workforce)
- 2023: All NHS providers introduce arrangements for the management of the offensive waste stream. (Area: Infrastructure)
- 2024: All clinical waste generated by NHS providers is regularly reported with a minimum of 95% accuracy (Area: Data)
- 2026: 50% reduction in carbon emissions produced from waste management in NHS organisations (leads onto 80% reduction in carbon emissions by 2028) (Area: Sustainability)
- 2026: All NHS providers achieve clinical waste segregation targets of 20:20:60 HTI (high temperature incineration), AT (alternative treatment), and OW (offensive waste) (Area: Compliance)
- 2030: The average net cost of clinical waste management reduces by 15% per tonne of waste (Area: Commercials)
2. Overview: The NHS and clinical waste
What is clinical waste?
Clinical waste is defined under the Controlled waste regulations (issued under the Environmental Protection Act) as follows:
- Waste containing viable micro-organisms or their toxins which are known or reliably believed to cause disease in humans or other living organisms.
- Waste which contains or is contaminated with a medicine that contains a biologically active pharmaceutical agent.
- Sharp waste, or a body fluid or other biological material (including human and animal tissue) containing or contaminated with a dangerous substance as defined by EC No 1271/2008 (The Classification, Labelling, and Packaging Regulation).
Not all waste created as a result of delivering clinical services is ‘clinical’ waste. A cardboard box from disposable gloves packaging, for example, would be recyclable waste. Further details on waste classification and the application of clinical waste treatment technologies are included in Health technical memorandum (HTM) 07-01: Safe and sustainable waste management for health and social care.
Clinical waste is categorised according to its hazardous properties and associated treatment and disposal requirements. Waste that poses the highest risk to the environment or human health needs to be treated using high-temperature methods such as incineration (HTI). Waste which poses a lower risk, even if derived from patients with known infections, can be treated using alternative treatment (AT) methods such as sterilisation.
Clinical waste is different to offensive waste. Offensive waste (OW) has no hazardous properties and can be treated or disposed of in a similar manner to municipal waste, which may include conventional energy from waste (EfW) treatment.
Given the infrastructure and energy that is needed for HTI and AT, treating clinical waste has a higher cost, and produces more carbon than offensive waste.
NHS waste volume growth rate
A growth rate of 3% per annum has been applied to waste arising for the foreseeable future (this correlates with waste growth pre-COVID-19 pandemic). As a result, the total clinical waste treated through HTI and AT, combined with OW, is expected to increase from approximately 149,000 tonnes in 2019/20 to an estimated 200,000 tonnes in 2029/30. This assumption will be reviewed as accuracy and detail in data reporting continue to improve.
This growth assumption does not account for the impact of increased waste generation from COVID-19. We have seen changes in how waste is classified and segregated in response to the pandemic. NHS England has reported that clinical waste generation requiring AT disposal rose from 1.5kg per bed per day to 4.5kg per bed per day for a non COVID-19 bed and 10.5kg per bed per day for a COVID-19 bed. These findings have been supported by a separate study carried out by the Department of Health and Social Care (DHSC) during the pandemic. The short, medium, and long-term impacts of COVID-19 on the classification of clinical waste and overall waste generation are currently unclear and will be reviewed once a more reliable baseline dataset is available.
Clinical waste production and net zero carbon
On average, the NHS currently produces an estimated 156,000 tonnes of clinical waste every year from secondary care (based on ERIC data 2020/21). The estimated carbon impact of this waste is approximately 100,000 tonnes of CO2e per year.
The effective, efficient, and sustainable management of clinical waste is vital to the continued function of any healthcare facility. In 2020, the NHS declared its intention to achieve net zero carbon by 2040 for its core emissions, the first healthcare provider in the world to do so. Such an ambition requires the careful review of NHS carbon emissions, and the implementation of robust plans to reduce them. It is essential that these plans include a strategy for dealing with the waste generated by NHS services.
Improving clinical waste management practices
The challenges of the COVID-19 pandemic have demonstrated the need for and ability of NHS providers to quickly adapt their waste management arrangements. Such adaptive measures remain pertinent in the face of the risks and challenges posed by climate change to the NHS and wider population.
Improved compliance in the segregation of waste types is crucial to positively transforming how waste is managed, treated, and transported to its final destination. All members of the NHS workforce, both clinical and non-clinical, have individual responsibility for managing waste sustainably. Good clinical waste management reduces cost and lessens environmental impact, whereas the poor management of clinical waste can harm the environment and threaten the ability of hospitals to function.
The NHS faces further expected increases in volumes of clinical waste and a shortfall in infrastructural capacity to treat it. Limited processing capacity on NHS sites has seen the knock-on effect of a sharp rise in costs associated with clinical waste management over the last 25 years.
By segregating waste in line with this strategy, NHS providers could reduce their HTI requirements by up to 35%, AT infrastructure requirements by up to 61% and increase OW demand by up to 229% (according to management data based on ERIC 2020/21. See appendices to the NHS clinical waste strategy, review findings – compliance). The energy demand and cost of managing OW is significantly lower than managing clinical waste using HTI and AT methods. Therefore, achieving these targets will reduce both the financial and environmental burden of NHS waste management. Based on ERIC 2020/21 data, this would mean a cost saving of more than £11 million per year (15% of total spend on clinical and offensive waste) alongside whole-life carbon savings estimated at 29,540 tonnes a year (around 30% of the CO2 from this area).
NHS clinical waste management review
During 2019 and 2020, a thorough review of NHS clinical waste management was undertaken by the national NHS Estates and Facilities team. Waste managers across secondary care were surveyed; quantitative data analysis incorporating learning from the COVID-19 pandemic was completed; and site visits took place.
The review identified three key themes to inform the priorities and actions of this strategy. These are as follows:
- Resilience: how infrastructure, capacity and cost can be managed to improve the resilience of NHS clinical waste management processes.
- Productivity: how reduced volumes of waste, and improved compliance, culture and data management can improve productivity in clinical waste management.
- Sustainability: how improved clinical waste management processes can contribute to meeting NHS net zero carbon targets and minimising negative environmental impacts.
The appendices to the NHS Clinical Waste Strategy contains an in-depth overview of the findings and outcomes of this review.
3. Objectives, priorities, activities, and measures
The key objective of this strategy is to eliminate waste, turning it into a resource.
This objective will help us to reach our net zero goals; improve efficiency, cost effectiveness, and function; and will reduce the NHS’ negative impact on the environment. Improved clinical waste management practices together with efforts to reduce total volumes of waste in the NHS are essential in ensuring we maintain a financially, socially, and environmentally responsible approach to our operations.
Directed by the three key themes of net zero carbon, resilience, and productivity, this strategy has identified six strategic priorities in the areas of data, workforce, compliance, commercial, infrastructure and sustainability intended to transform NHS waste management practices in line with our key objective.
These strategic priorities are each accompanied by key activities and key performance indicators (KPIs), alongside a measure of success. The relationship between the themes, priorities, activities, and measures in this clinical waste strategy are illustrated in figure 1 along with figure 2, an indicative timeline of target dates for the strategy’s measures of success. A detailed breakdown follows in section 4.
3.1 Outcomes of the strategy’s implementation
By implementing this strategy, within five years (see figure 5: Tactical roadmap, section 4.8), we can:
- Ensure 100% of NHS providers, including primary care managing agents, have fully trained waste managers.
- Improve waste segregation and compliance.
- Establish a new commercial model to help stabilise the waste management market.
- Drive NHS ownership and control over its own processing assets, with 25% of large and acute teaching hospitals owning their processing capacity thereby improving regional and national resilience.
- Deliver a 30% reduction in carbon emissions from clinical waste segregation; a 50% reduction in the carbon emissions produced from wider waste management by 2025/26, and 80% by 2028 – 2032.
- Ensure there is national support to help providers implement the strategy.
3.2 The waste hierarchy
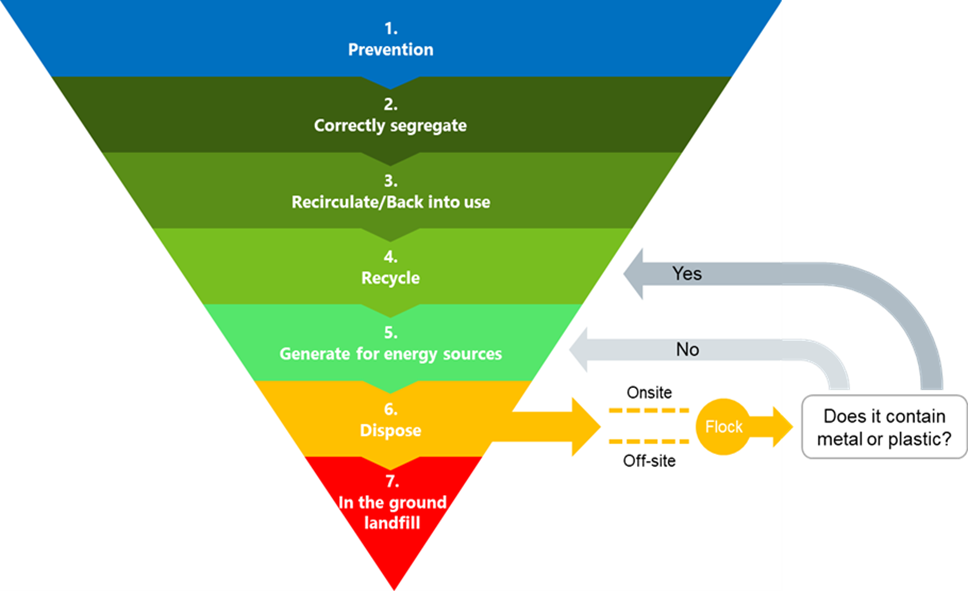
Figure 3: The waste hierarchy (adapted for clinical waste).
This image is an inverted pyramid with the widest level at the top. There are 7 levels to the hierarchy, signifying the most to the least desirable clinical waste management techniques from an environmental perspective. At the top of the hierarchy and least harmful is level 1: prevention. Level 2 is ‘correctly segregate’; level 3 ‘recirculate/back into use’, level 4 ‘recycle’, level 5 ‘generate for energy sources’ level 6 ‘dispose’ and level 7 ‘in the ground landfill’. At level 6, ‘dispose’, there is an additional arrow to ‘Flock’ which, depending on whether it contains metal or plastic can re-enter the hierarchy at level 4 (yes) or level 5 (no).
The waste hierarchy, as described by the Department for Environment, Food and Rural Affairs (Defra), ranks waste management options according to what is best for the environment. It gives top priority to preventing waste in the first place. When waste is created, it gives priority to preparing it for re-use, then recycling, then recovery, and last of all disposal (for example, landfill).
Following the waste hierarchy when making all waste management decisions in the NHS is central to good practice and to achieving the objectives of this strategy.
4. Our action plan
This section provides an explanation for each strategic priority in the six areas of data, workforce, compliance, commercials, infrastructure and workforce, detailing the review findings which constitute the rationale for each priority (covered further in the appendices to the NHS clinical waste strategy, appendix A); each associated set of key activities and key performance indicators; and a summary of the measure of success which gives a clear goal for the outcome of each priority over the next ten years. See figure 1 in section 1 for a summary of the relationships between the strategy’s themes, priorities, activities, and measures.
4.1 Data
Review theme: Productivity
Review findings: The NHS needs consistent, high-quality data to be able to make informed and proactive decisions, and to respond effectively to disaster recovery situations.
Strategic priority:
Use better data: Utilise comprehensive, consistent data from across all NHS organisations/integrated care systems (ICSs) to drive decision-making and proactive risk management.
This priority requires that all NHS providers and ICSs report consistent quantitative and qualitative data onto the newly created central Atamis platform being rolled out in 2022/23, with a minimum of 95% accuracy. This data should be collected regularly and used to drive waste-related decision-making and risk management nationally, regionally, and locally.
The immediate investment required for implementation of this strategic priority is low and will:
- Help to drive proactive data-led decision making and risk management
- Facilitate longer-term strategic planning
- Enable real-time responses to emerging issues
- Encourage organisations to be mindful of waste management and associated impacts
- Enable the analysis of data at a local, regional, and national level.
Key activities
- Create an NHS waste data quality standard that specifies the required quality, frequency, and type of data to be centrally reported.
- Ensure that all NHS providers have an accountable individual trained with analytical skills or a data analyst that can support the analysis of waste management data and take responsibility for central reporting.
- Expand the NHS waste database to capture monthly qualitative and quantitative data on healthcare waste generation and treatment at an organisational level across all trusts. Review the tool’s suitability for use by primary care organisations.
- Set up a central process within the NHS to monitor and interrogate trust compliance with the new waste data quality standards.
- Develop and implement an annual clinical waste monitoring report to measure and monitor each of the KPIs included within the clinical waste strategy.
Key performance indicators
- Proportion (%) of NHS providers with an appointed individual responsible for data reporting.
- Proportion (%) of trusts and foundation trusts that are compliant with the new waste data quality standard.
- Proportion (%) of trusts and foundation trusts reporting information into the NHS waste database on a monthly basis.
Measure of success:
All clinical waste generated by NHS providers is regularly reported with a minimum of 95% accuracy by 2024.
4.2 Workforce
Review theme: Productivity
Review findings: Waste is better managed and allocated in trusts where there is sufficient resource, clarity around roles and responsibilities, and appropriate training for those with legal accountabilities around waste.
Strategic priority:
Invest in a skilled workforce: Invest in developing a skilled and diverse waste management workforce with appropriate support and defined career paths.
The intent of this priority is for every NHS trust and NHS foundation trust to have a dedicated, full-time waste manager with a defined career path, training, role requirements and responsibilities. All NHS primary care providers will have accountable managing agents for overseeing waste management, with access to support and training.
The benefits of this action include:
- Developing our workforce to provide the capability and resource to significantly improve the segregation of clinical waste.
- Training waste managers and accountable individuals in contract management, enabling us to address existing issues with contracting and to strategically engage with suppliers in the future.
- Improved contracting to drive better deals for the NHS and contribute towards creating a healthier national waste management market.
- Creating a defined estates and facilities management (EFM) career path and development opportunities for staff in waste management.
- Engaging the whole NHS workforce so that everyone working in the NHS understands their roles and responsibilities relating to waste management (see appendices to the NHS clinical waste strategy, appendix C).
Key activities
- Create standardised waste manager job descriptions and a competency framework that is defined centrally and implemented in all trusts and foundation trusts, with scope for career progression across ICSs.
- Develop a consistent and comprehensive overview of waste management training requirements, which is provided to all waste managers and accountable individuals.
- Centrally define the institutional responsibilities and governance accountabilities for all employees regarding waste management and develop an action plan for introducing these at all NHS providers.
- Develop a plan for incorporating basic (foundation level) waste management training into induction programmes for all NHS employees.
- Create an engagement strategy to support the roll-out of the revised HTM 07-01 across the workforce.
Key performance indicators
- Proportion (%) of NHS providers that have appointed a waste manager (or accountable individual) in line with the standardised job description and capability framework.
- Proportion (%) of NHS new starters that have received basic (foundation level) training in waste management as part of their induction programme.
- Proportion (%) of NHS employees that are aware of the revised HTM 07-01.
Measure of success:
100% of NHS trusts and foundation trusts have a dedicated waste manager role (at least 0.5 FTE) by 2023, funded from their own resources, and 100% of other NHS providers have identified accountable individuals for waste management.
4.3 Compliance
Review theme: Productivity
Review findings: There is an opportunity to improve the knowledge and skills of all NHS staff around compliance requirements and accountabilities, in order to improve adherence to correct segregation, tracking, and transportation methods for waste.
Strategic priority:
Improve our ability to comply: Ensure all NHS staff understand and adhere to compliance requirements.
This priority requires all organisations to segregate 100% of their waste correctly, and to actively measure and report on progress towards their segregation targets. Every individual working in the NHS should be aiming to ensure compliance requirements are met, and policies and procedures should be in place to enable the monitoring of waste management compliance. All NHS staff should understand their waste management responsibilities and the compliance standards required of them.
Reasons for implementing this strategic priority with the aim of upskilling the whole NHS workforce in waste management include:
- Significant financial and environmental savings from improved segregation.
- Enabling efficiencies that mean less overall waste management capacity is required to treat waste, thus reducing the need for future investment.
- Removing the risk of fines or closures due to non-compliance and reducing the risks to public health from poorly managed waste.
- This is a low cost, high impact intervention.
Key activities
- Introduce a waste segregation target of 20:20:60 (for HTI, AT and OW respectively) for all NHS providers and trusts.
- Include compliance requirements within the responsibilities, accountabilities, training, and induction programmes across the NHS workforce.
- Introduce a ‘compliance checklist’.
- Review current practices to identify barriers to correct segregation and encourage compliant behaviours.
- Work with key stakeholders to develop a live system for tracking clinical waste consignments from the point of generation through to disposal.
- Work with regulators to introduce a system that notifies the NHS centrally, and affected trusts locally, of non-compliances with the waste management value chain (e.g., waste carriers and treatment facility operators).
- Develop a plan to raise awareness of waste management compliance requirements with the boards and governing bodies of all NHS organisations, providers, and integrated care systems (ICSs).
Key performance indicators
- Proportion (%) of NHS providers that have implemented arrangements for the segregation of OW.
- Quantity generated (kg per patient) for each of HTI, AT and OW streams.
- Proportion (%) of NHS providers to have achieved a minimum 95% accuracy in maintaining and recording waste consignment and transfer documentation.
- Proportion (%) of NHS providers that have completed up to date pre-acceptance audits.
Measure of success:
All NHS providers achieve clinical waste segregation targets of 20:20:60 HTI, AT and OW by 2026.
4.4 Commercials
Review theme: Resilience
Review findings: By improving contracting arrangements and contract management capability and by supporting a health waste management market, we will improve our commercial model and the resilience of our supply chain.
Strategic priority:
Establish a commercial model that delivers better value: Support the standardisation of contracting arrangements and develop a commercial model which encourages healthy market conditions.
This priority involves supporting the restructuring of the commercial model for contracting, to help establish a healthier market.
This will be achieved by developing internal contracting expertise and templates, and by establishing a dialogue with the marketplace and external regulators.
The benefits of this include:
- Saving significant time and effort in the contracting process.
- Driving better, more consistent deals across all organisations whilst offering the ability to leverage purchasing power.
- Enabling the NHS to strategically support its suppliers (e.g., to develop their infrastructure or sustainability) and have oversight of the market.
- Limiting risk exposure from service delivery by creating healthier market conditions and improving the quality of service provided by suppliers.
Key activities
- Establish a plan to redefine the current commercial model to support the regional and ICS delivery model and help to secure a resilient marketplace.
- Support the development of a framework of standard waste service contracts that are appropriate for the key requirements for each type of NHS providers, including infrastructure and equipment provision, standard service specifications, performance framework, payment mechanism, KPIs, and contingency planning.
- Define the principles and minimum requirements for contract governance and reporting for all NHS providers, including a process for risk escalation and duty of care/compliance issues.
- Establish and maintain a standard contract management database for all NHS providers, which interfaces with procurement systems and provides transparency at a national level.
- Introduce a mechanism for monitoring the provision and capacity of clinical waste treatment, to mitigate clinical waste market price volatility and prevent disproportionate price increases.
- Maintain an up-to-date market analysis.
- Develop and implement a supplier code of conduct to ensure supply chain alliance with NHS goals and ambitions.
Key performance indicator
- Average cost (£ per tonne) of clinical waste management.
- Average duration (years) of contracted waste management services.
- Proportion (%) of new waste management service contracts procured under the new template.
- Existence of an up-to-date market analysis.
- Proportion (%) of NHS providers using the new Contract Management Database on at least an annual basis.
Measure of success:
The cost of clinical waste management is reduced by 15% by 2030 (based on ERIC data 2020/21; after inflation and/or above increased treatment costs).
4.5 Infrastructure
Review theme: Resilience
Review findings: There is an opportunity to improve waste management infrastructure to drive efficiencies, lower costs, reduce the use of incineration, and improve our resilience to unforeseen increases in waste production.
Strategic priority:
Develop resilient infrastructure that meets future demand: Invest in clinical waste infrastructure to increase capacity and regional resilience and support sustainable waste processing practices.
This priority requires in-house waste processing capability and capacity to be developed at a local, ICS and regional level. At the same time, it involves working in collaboration with suppliers and trusts and foundation trusts as they develop their infrastructure, ensuring that it is future proof both in overall capacity and sustainability.
We will work to encourage innovation, collaborating with key stakeholders including providers, suppliers, and the Environment Agency to assess the financial and operational feasibility new technologies for treating and reducing the carbon impact of wastes. See appendices to the NHS clinical waste strategy, appendix A, Review findings – infrastructure for more information.
This action will enable the NHS to:
- Have the right waste infrastructure in place, offering significant long-term benefits by lowering costs and increasing resilience.
- Reduce the environmental impact of waste management by improving processes and reducing road miles.
- Create an opportunity to integrate the infrastructure developments into the New Hospital Programme (NHP).
Key activities
- Conduct a review of regional and local waste processing capability to identify potential areas for developing additional onsite hospital capacity.
- Develop and implement a national clinical waste infrastructure plan to address the capacity gap and determine future public and private sector investment needs, incorporating regional processing resilience into HIP schemes.
- Actively promote investment in onsite treatment infrastructure at major/acute hospitals or those locations that may serve as waste treatment hubs.
- Encourage and incentivise the sharing of surplus on-site treatment capacity between trusts and foundation trusts, where this already exists.
- Carry out soft market testing with established and emerging waste treatment market players to determine scope and appetite for the development and location of new infrastructure.
Key performance indicators
- Number of hospitals with on-site waste treatment capability.
- Total on-site waste treatment capacity (tonnes per annum).
- Total annual increase in national clinical waste treatment capacity (tonnes per annum).
- Proportion (%) of clinical waste sent for third party treatment.
Measure of success:
All NHS providers introduce arrangements for the management of the offensive waste stream by 2023.
NHS organisations that do not currently segregate offensive waste will be expected to introduce bins, signage, and labelling, along with collection arrangements. This will support the achievement of the segregation targets detailed in section 4.3 compliance, in turn reducing infrastructural demand for the processing of clinical waste using AT and HTI.
4.6 Sustainability
Review theme: Resilience
Review findings: Waste management processes and arrangements should be optimised to prevent excess emissions and encourage recycling.
Strategic priority:
Improve our sustainable use of resources and reduce carbon impact: Proactively work to reduce harmful emissions, improve local air quality, and achieve the 2045 net zero carbon target.
This action requires all NHS providers to ensure, if not specified already, that, a net zero carbon action plan for their waste management is included as part of their Green Plans, including both the emissions they control directly, and those they can influence. This will involve the creation of an action plan to meet sustainability targets for carbon reduction and air quality improvements. The action plan should also include consideration of opportunities for innovation in providers’ waste management activities.
There are a number of benefits to trusts and patients from introducing environmental considerations into waste management practices, such as:
- Reducing the total quantity of waste needing to be managed.
- Reducing waste miles (distance waste must travel for disposal), thereby reducing fuel and energy use.
- Maximising of the use of materials and resources before they become waste.
- Minimising the quantity of packaging in the health product supply chain, thus saving on waste management costs.
- Increasing the measurement of key sustainability metrics, thus facilitating the progress of Green Plans and sustainability reporting.
- Improving NHS approach to waste management service procurement through undertaking supplier meetings which review sustainability credentials.
- Preventing harmful emissions from the waste value chain and improving air quality and associated population health outcomes.
- Enhancing engagement around sustainability issues, raising the profile of the waste manager role.
Key activities
- NHS England has developed a waste planning tool in line with this Clinical Waste Strategy for all NHS providers, which includes improved segregation, waste minimisation, and increased reuse programmes. This will lead to reductions in the road miles waste travels, increases in the use of re-usable sharps bins and plans made towards the achievement of net zero carbon from waste management.
- Design a national action plan for educating both producers of waste (across all NHS providers) and waste suppliers in sustainable waste practices.
- Work with DEFRA to re-define the guidelines and minimum standards to be used for measuring sustainability metrics.
Key performance indicators
- Proportion (%) of NHS providers with plans in place to achieve their sustainability targets, including measuring key metrics and demonstrating that they are exceeding the minimum standards.
- Proportion (%) of NHS providers achieving their sustainability targets.
- Proportion (%) of NHS providers that have appointed clinical and non-clinical sustainability leads, responsible for innovating and embedding sustainability practices in waste management.
- Proportion (%) of NHS providers using re-usable sharps bins.
Measure of success:
We achieve a 50% reduction in the carbon emissions produced from waste management by 2025/26, and an 80% reduction by 2028-32.
Increasing sustainable, environmentally friendly waste management methods and successfully reducing associated carbon emissions will demonstrate progress in effectively moving up the waste hierarchy (figure 3, section 3.2).
4.7 Monitoring progress
NHS England will review progress annually, evaluating system performance against national waste and carbon reduction targets, KPIs, and Measures of Success. Using this information, we will consider whether any changes or course corrections should be made for the following year.
Strategic reviews of the implementation of this Clinical Waste Strategy across the NHS will also be conducted by NHS England at years 3, 5, and 8. These will provide a more in-depth, holistic assessment that considers the strategy’s overall progress and assesses whether more significant interventions are necessary.
The regular central reporting of robust data and information by all NHS providers will be key to ensuring that our KPIs remain appropriate and that assessment against them is founded on reliable information. Our strategy sets out mechanisms to improve data quality. This strategy has identified 24 KPIs to monitor implementation of our Strategic Priorities and determine the likelihood of achieving our Measures of Success. Although the KPIs are divided between our Strategic Priorities, many of them contribute to more than one Measure of Success. Figure 4 illustrates the relationship between each KPI and each Measure of Success.
Figure 4: Relationship between KPIs and measures of success
The image compiles all of the Key Performance Indicators introduced by the NHS Clinical Waste Strategy and shows which out of the 6 Measure(s) of Success each relates to using a colour key.
4.8 Our tactical roadmap
Figure 5: 10-year tactical roadmap for outcomes and objectives of the clinical waste strategy.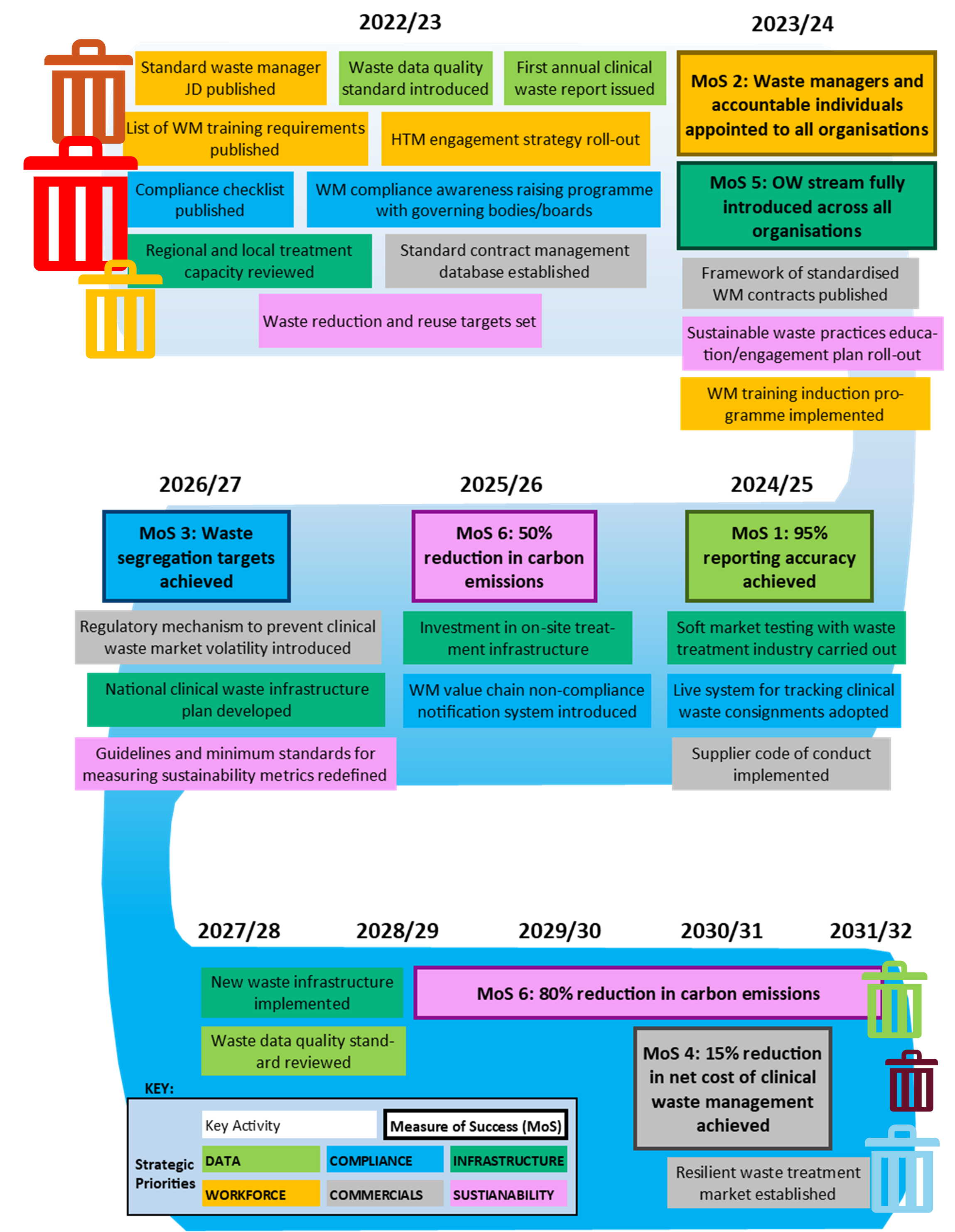
The image is a road map diagram starting in year 22/23 and ending in 2030/31, containing key activities proposed in NHS Clinical Waste Strategy in chronological order of their target achievement dates. The map also includes the six measures of success from the clinical waste strategy. The measures and actions are colour coded to represent which of the 6 themes of the strategy they relate to (data (light green), workforce (orange), compliance (blue), infrastructure (dark green), commercials (grey) and sustainability (pink).
2022/23
Workforce:
- Standard waste manager JD published
- List of waste manager training requirements published
- HTM Engagement strategy roll-out
Compliance:
- Compliance checklist published
- Waste manager compliance awareness raising programme with governing bodies/boards
Data:
- Waste data quality standard introduced
- First annual clinical waste report issued
Commercials:
- Standard contract management database established
Sustainability:
- Waste reduction and reuse targets set
Infrastructure
- Regional and local treatment capacity reviewed
2023/24
Workforce:
- Measure of Success 2: Waste managers and accountable individuals appointed to all organisations
Infrastructure:
- Measure of Success 5: Offensive waste stream fully introduced across all organisations
Commercials:
- Framework of standardised waste management contracts published
Sustainability:
- Sustainable waste practices education/engagement plan roll-out
Workforce:
- Wate manager training induction programme implemented
2024/25
Data:
- Measure of success 1: 95% reporting accuracy achieved
Infrastructure:
Soft market testing with waste treatment industry carried out
Compliance:
- Live system for tracking clinical waste consignments adopted
Commercials:
- Supplier code of conduct implemented
2025/26
Sustainability:
- Measure of Success 6: 50% reduction in carbon emissions
Infrastructure:
- Investment in on-site treatment infrastructure
Compliance:
- Waste Manager value chain non-compliance notification system introduced
2026/27
Compliance:
- Measure of success 3: Waste segregation targets achieved
Commercials:
- Regulatory mechanism to prevent clinical waste market volatility introduced
Infrastructure:
- National clinical waste infrastructure plan developed
Sustainability:
- Guidelines and minimum standards for measuring sustainability metrics redefined
2027/28
Infrastructure:
- New waste infrastructure implemented
Data:
- Waste data quality standard reviewed
2028 – 2032
Sustainability:
- Measure of success 6: 80% reduction in carbon emissions
2030/31
Commercials:
- Measure of success 4: 15% reduction in net cost of clinical waste management achieved
- Resilient waste management market established
Acknowledgements
NHS England’s Clinical Waste Strategy has been developed using staff surveys; quantitative data analysis incorporating learning from the COVID-19 pandemic; work with colleagues across the four nations, the Department for Environment, Food and Rural Affairs (Defra) and the Environment Agency; and engagement with subject matter experts. Our market insights are informed by work commissioned by the Department of Health and Social Care and the Cabinet Office. We would like to thank everyone who has taken the time to help us in its creation.
Publication number: PR2159