Summary
The new NHS Oversight Framework 2025/26 describes a consistent and transparent approach to assessing integrated care boards (ICBs) and NHS trusts and foundation trusts, ensuring public accountability for performance and providing a foundation for how NHS England works with systems and providers to support improvement. It has been developed with the engagement and contributions from the NHS leadership and staff, representative bodies and think tanks, including through two public consultations. They said that NHS England’s approach to oversight and performance improvement needs to be consistent and our interactions coherent.
This 1-year framework sets out how NHS England will assess providers and ICBs, alongside a range of agreed metrics, promoting improvement while helping us identify quickly where organisations need support.
The framework will be reviewed in 2026/27 to incorporate work to implement the ICB operating model and to take account of the ambitions and priorities in the 10 Year Health Plan.
The framework is supported by a focused set of national priorities, including those set out in the planning guidance for 2025/26, aiming to strengthen local autonomy. These are presented alongside wider contextual metrics that reflect medium-term goals in areas such as inequalities and outcomes. The contextual metrics do not constitute part of the score but will inform how NHS England responds to segmentation.
The NHS priorities and operational planning guidance 2025/26 made it clear that achieving a financial reset this year is a priority. The NHS must live within the budget it is allocated, reduce waste and increase productivity to deliver growth against demand. It set the expectation that every ICB and provider must deliver a balanced net system financial position in collaboration with its system partners. NHS England will identify organisations that are not performing and take quick action. Our approach to assessment will mean that unless providers are delivering a surplus or breakeven position, their segmentation will be limited to no better than 3.
Our improvement approach will be based on the results of our assessment and tailored to the support providers in each delivery segment need. Discussions about performance will be led by colleagues at NHS England who are experienced in addressing delivery challenges, with a focus on offering informed evidence and practical guidance that is grounded in a deep understanding of the operational challenges faced.
Our assessment will be the starting point for how we work with organisations throughout the year and will help us determine how we can support them to improve. We will do this by considering an organisation’s segment score, as set out in this framework, and leadership capability.
The framework outlines the circumstances in which providers can obtain increased freedoms. It also describes how we will determine whether a provider’s performance falls below an acceptable standard and/or has governance concerns that may lead NHS England to use our regulatory powers to step in and secure improvement. NHS England’s approach to the use of enforcement powers is set out in the NHS enforcement guidance.
We will not be segmenting ICBs in 2025/6, as this will be a year of significant change for ICBs as they transform in line with the Model ICB Blueprint to focus on strategic commissioning and implement plans to meet the running cost reductions. Support for ICBs this year will focus on the safe implementation of their plans. ICBs that are currently in the Recovery Support Programme will continue in this programme and will be assessed against their current improvement trajectory to agree a transition plan. This will be the equivalent to segment 5.
We will report ICB performance against the full suite of oversight metrics, but we will not issue a comparative rating. ICBs will still be assessed through a statutory annual assessment, which reviews how well each ICB is performing its statutory duties. Where there are performance or governance concerns, NHS England will step in and we may use our regulatory powers to secure improvement. We will introduce the segmentation approach for ICBs in 2026/27.
Performance assessment
Roles and responsibilities
We recognise that streamlining the NHS operating model will be an important step in laying the foundations for the delivery of the 10 Year Health Plan. We need a less duplicative, leaner and simpler way of working, where every part of the NHS is clear on its purpose, what it is accountable for and to whom. The clarified roles and responsibilities for ICBs, providers and NHS England are set out below.
Integrated care boards (ICBs):
- provide system leadership for population health, setting evidence-based and long-term population health strategy and working as healthcare payers to deliver this, maximising the value that can be created from the available resources
- this includes holding their partners in the integrated care system (ICS) to account using the system levers that bind them together, such as joint system plans, partnership agreements, joint committees and collaboratives
- through effective strategic commissioning, invest in, purchase and evaluate the range of services and pathways required to ensure access to high quality care, to improve outcomes and to reduce inequalities within their footprint
- this includes monitoring provider performance against their contractual obligations for the services purchased as part of the ICB’s population health strategy
- strategically align funding and resources with long-term population health outcomes and manage clinical and financial risks
Providers (NHS trusts and foundation trusts):
- deliver high quality (safe, effective and positive patient experience) and efficient care
- comply with the requirements of the NHS provider licence
NHS England:
- oversee overall delivery, performance and improvement of both ICBs and providers (a statutory responsibility
- conduct an ICB performance assessment each financial year
- determine how to support and drive improvement in each organisation, including where necessary the use of enforcement powers
Overview
NHS England will use the performance assessment process to measure delivery against an agreed set of metrics. This will determine the segment score for each provider and identify where improvement is required. NHS England’s improvement response will be based on the segmentation score alongside consideration of the organisation’s leadership and governance (provider capability) to ensure that it is tailored and nuanced, balancing performance improvement and management. We plan to finalise our approach to the assessment of provider capability and issue guidance during Q2. It is our intention is to align our approach with that of the Care Quality Commission (CQC).
Drawing on the 4 purposes of an ICS (improving population health and healthcare; tackling inequalities in outcomes, experience and access; enhancing productivity and value for money; and supporting social and economic development), the performance assessment process measures each provider’s delivery on key metrics across 6 domains, as set out in Table 1. Each domain has a range of appropriate metrics for each type of organisation (acute, mental health, community and ambulance trusts).
For this transitional year, a focused set of metrics, which reflect the 2025/26 NHS priorities and operational planning guidance, will contribute to the segment score for an organisation. While not scored and rated as part of our segmentation approach, we have identified a longer list of contextual metrics that sit largely in the areas of population health, primary prevention and health inequalities. The performance data on contextual metrics will be available for boards to consider, aligned with the Insightful Board approach (as described in the Insightful provider board guidance) and we will consider this in our oversight response. Annex A identifies those metrics that will be scored and those that are contextual.
Table 1: Scoring and non-scoring domains of the framework
| Domains and sub-domains |
| Access to services – elective care – cancer care – urgent and emergency care – mental health care |
| Effectiveness and experience of care |
| Patient safety |
| People and workforce |
| Finance and productivity |
| Improving health and reducing inequality (non-scoring) – improving population health – primary prevention – inequalities |
Where providers are part of a provider collaborative or group model, they will be measured as a trust and not as a wider group. The effectiveness with which providers are collaborating and supporting system working will form part of the provider capability assessment.
Integrated care boards
For ICBs, a set of metrics and system considerations have been selected to reflect the NHS priorities and operational planning guidance, system performance and longer-term strategic priorities. However, ICBs will not be segmented this year, given the significant changes they are undertaking during this year. This means these metrics will not be scored to inform segmentation, but they will be reported as contextual information to be used in strategic planning and improvement conversations. Although ICBs will not be segmented, their leadership capability will be assessed through our annual assessment of ICBs, which reviews how well each ICB is performing its statutory duties.
Primary care providers
Primary care providers, primary care networks and other non-trust providers or partnerships, such as provider collaboratives, will not be allocated their own segments. However, we will continue to keep under review our arrangements for accountability of primary care providers as we move towards the planned shift to neighbourhood health.
Independent providers
For independent providers of NHS services, ICBs will be expected to continue to ensure quality and performance through contractual levers and escalate concerns to NHS England regions. We will continue to oversee and assure certain independent providers under the Independent Providers Risk Assessment Framework (IPRAF) and NHS-controlled providers under either the IPRAF or this framework.
Segmentation approach
Figure 1: Process for determining a segment
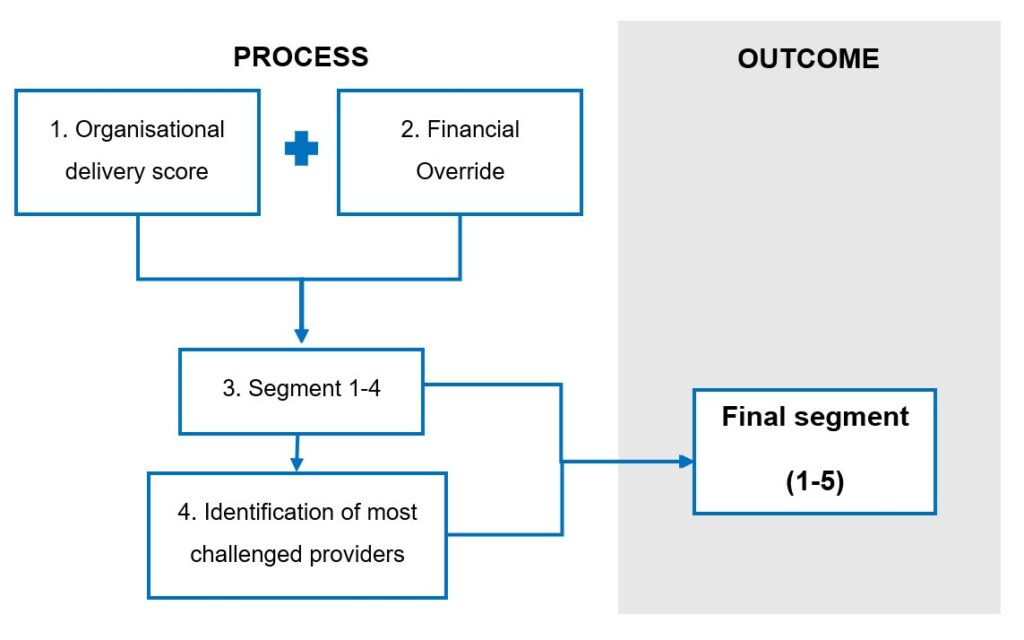
Step 1 – Organisational delivery score
Each provider will receive an individual organisational delivery score derived from its performance against the metrics listed in Annex A.
Each metric has an individual set of scoring rules and based on these, a provider will receive a score between 1 and 4 for each metric.
To calculate the overall organisational delivery score, the individual metric scores are averaged according to the number of metrics the organisation will be measured against. The scores are then benchmarked against those for the rest of the country and divided into 4. These quartiles are numbered 1 to 4 with the highest performance scoring quartile numbered 1 and these numbers become each organisation’s overall organisational delivery score.
Further detail on the scoring approach is given in the separate methodology manual. The specific scoring regime for each metric will be detailed in a separate technical document that we will publish when we release initial segments in July.
Step 2 – Financial override
As part of the scoring methodology an override relating to organisational, not system-wide, financial performance will be applied. The override means all organisations in deficit or in receipt of deficit support will be limited to an organisational delivery score of no greater than 3.
Step 3 – Segmentation
Based on the process described above, we will place every provider into a segment. This indicates its level of delivery from 1 (high performing) to 4 (low performing) and informs its support or intervention needs. Entry into segment 5 will be reserved for the most challenged organisations that require the most support to improve. See Table 2 for descriptions of the 5 segments.
Step 4 – Allocation to segment 5
To establish which providers will be allocated to segment 5, we will review the outputs of both segmentation and capability assessments. Those providers rated low for both performance and capability will be considered for entry into the Provider Improvement Programme (PIP), which replaces the Recovery Support Programme (RSP), and is the support for the most challenged providers. All providers in the PIP will be placed in segment 5. Providers already in the RSP will be placed in segment 5 when the initial segments for 2025/26 are published in July 2025. For providers currently undergoing a diagnostic as part of the planning process, the outcome of the diagnostic will inform their potential entry into the PIP and segment 5.
In exceptional circumstances, where NHS England has identified concerns about a provider’s capability such as failures of governance, it may be necessary, regardless of the provider’s existing segment, to review whether it should be placed in segment 5 and the PIP. This is to ensure it is allocated the appropriate support and intervention. This review will be agreed with the appropriate NHS England committee.
Finalisation of segments
Once NHS England has approved the final segmentation decision, this will be officially communicated to each organisation and published on NHS England’s website.
Segmentation data will be reviewed at least quarterly as part of a review meeting and segments may be updated at any time based on emerging information.
Table 2: Segment descriptions
| Segment | Description |
|---|---|
| 1 | The organisation is consistently high-performing across all domains, delivering against plans. |
| 2 | The organisation has good performance across most domains. Specific issues exist. |
| 3 | The organisation and/or wider system are off-track in a range of domains or are in financial deficit. |
| 4 | The organisation is significantly off-track in a range of domains. |
| 5 | The organisation is one of the most challenged providers in the country, with low performance across a range of domains and low capability to improve. or The organisation is a challenged provider where NHS England has identified significant concerns. |
Publication of data
To support transparency, NHS England will publish a dashboard to give the public access to the data that underpins segmentation.
Each provider’s domain scores, organisational delivery score and final segmentation will be shown alongside the individual metric scores used to calculate them. Although contextual metric results for providers and ICBs, including measures of progress against reducing health inequalities, will not contribute to these scores, they will also be shown on this dashboard. An overall score will also be displayed for each provider indicating its position relative to organisations of the same type. Data related to segmentation will be updated quarterly.
In addition, once our approach to provider capability is finalised, we anticipate that the dashboard will include the provider capability ratings.
Segmentation response
Segmentation combined with consideration of NHS England’s assessment of provider capability will inform our oversight response.
Each NHS England region will co-ordinate the response to segmentation with NHS England national teams and wider system partners. We will use the segmentation scores alongside wider information to direct our oversight activities at those organisations that have lowest performance and lack the capability to improve without support.
We will base our oversight of performance improvement activities on essential principles that will be focused on the delivery of joint system plans. The frequency of review meetings with ICBs will depend on the confidence the region has in the ICB’s capability to deliver the required improvements. The system’s providers will be included in these meetings where required, for example where the ICB cannot drive the required improvement of a provider using the contractual levers it has with the provider. Further meetings to monitor in-year delivery and co-ordinate support will be scheduled as required.
We will align our improvement support offer to organisational delivery scores. For some priority areas for 2025/26 (reflected in the finance, urgent and emergency care, elective and mental health sub-domains), those providers with a relevant sub-domain score of 4 will receive the most intensive improvement support and this will be provided onsite. The offer for those with a sub-domain score of 3 will be predominantly offsite support. A universal improvement offer will be available to all organisations.
Where required, NHS England regional teams will undertake performance management activities (tiering) for providers with low performance in the priority areas of finance, urgent and emergency care, elective and mental health. In addition, a proportion will receive more intense scrutiny, and they may be supported by national programmes. Those organisations in segment 4 with an associated low provider capability may enter into the programme of support for our most challenged providers, the Provider Improvement Programme (PIP).
Example: Contract management of a provider
A provider is placed in segment 2 and has good performance across all domains including elective care. As a result, the relevant NHS England region does not plan to take any performance improvement actions.
The ICB reviews the provider’s performance against its contract for elective care services. It finds that the provider is meeting its 18-week referral to treatment target but not fully meeting its contractual requirements to treat patients with complex needs. This means that patients with complex needs are waiting significantly longer than those who do not.
The identified concern is more appropriate for the ICB to manage under its statutory responsibilities for arranging services than for intervention under NHS England oversight functions.
NHS England has no concerns about the ICB’s leadership capability, so the ICB agrees with the region that it will manage the provider’s underperformance using its contractual levers. After speaking to the provider, the ICB issues a Contract Performance Notice under General Condition 9 of the NHS Standard Contract, the condition that sets out the contract management process. The ICB and provider then hold a contract management meeting and following this they agree a remedial action plan.
The ICB will escalate to the region if it does not see improvement or wider concerns develop through performance management. The region will monitor the ICB’s progress in the management of the provider and will keep our view of ICB leadership capability under review as part of our wider oversight of the ICB.Table 3: Segment support needs
| Segment | How NHS England supports | How NHS England drives improvement | How NHS England intervenes |
|---|---|---|---|
| 1 | No specific support or intervention needs are identified. All organisations will have access to NHS IMPACT, the universal NHS improvement approach. | The organisation is expected to take a leadership role in developing and sharing best practice and improvement initiatives in areas that it excels in. | NHS England’s use of its enforcement powers is not expected for organisations in this segment as they do not have intervention or support needs, but, if necessary, we will take enforcement action. |
| 2 | The organisation can diagnose and clearly explain its support needs, which are predominantly met locally. Our support on specific issues is provided where appropriate. | The organisation works with us to support the development of best practice in areas it shows high performance in and is expected to lead on its own improvement. Minimal, targeted support is aimed at improving specific areas where issues have been identified. | Due to the relatively high-performing nature of the organisation and its level of maturity, NHS England’s use of its enforcement powers will be uncommon, but we may use these where specific issues call for this approach. |
| 3 | NHS England agrees the support needs of the organisation involving the provider’s relevant ICB in the decision. To do this we take account of segmentation and capability. Support is delivered through local support offers, defined national support programmes and bespoke regional interventions. | The organisation receives increased scrutiny targeted at delivering improvement in challenged performance areas. | NHS England may apply interventions and/or require the organisation to take action in specific areas of low performance. This may involve use of our enforcement powers, particularly where performance concerns persist. |
| 4 | NHS England will consider the organisation’s challenges and support needs, taking account of segmentation and capability to inform the appropriate support or intervention. As with segment 3, support needs are prioritised through local support offers, defined national support programmes and bespoke regional interventions. | The organisation receives intense scrutiny targeted at delivering improvement in the most challenged performance areas. Recovery KPIs and trajectories are agreed and proactively monitored. | NHS England may apply interventions and/or require the organisation to take broad actions or address specific concerns related to known issues. This may involve use of our enforcement action, particularly to secure improvement or where improvement is insufficient. |
| 5 | The organisation will be subject to NHS England’s most intensive support – the Provider Improvement Programme (PIP) – to ensure it meets improvement goals. | The organisation is subject to the highest level of NHS England scrutiny and performance management to meet agreed transition criteria to leave the PIP or meet its agreed improvement plan. These demonstrate it can sustain levels of improvement. | Alongside support for the most challenged organisations, it is likely that enforcement action will be agreed through the relevant executive governance group if deemed necessary. Transition out of segment 5 requires the transition criteria to be met. |
Emerging information and capability assessments
As part of NHS England’s assessment process, we will gather insights across the assessment domains. We will collect this mix of quantitative data and qualitative information annually, in-year or by exception.
Qualitative information may be derived from:
- ICBs and providers as part of routine interactions, for example around emerging financial risks or clinical quality risks in line with the National Quality Board guidance on risk response and escalation
- reports from other regulators such as the CQC, including ICS assessments and internal and external audit reports
- the police and coroner reports
- third-party information, for example whistleblowing, 360-degree feedback, peer reviews, complaints or formal publications/assessments
NHS England will work with regulators, including the CQC, Health and Care Professions Council, General Medical Council and Nursing and Midwifery Council, through the national and regional Joint Strategic Oversight Group. This group provides a space for regulators to share intelligence and develop aligned approaches to support organisations.
We will assess the information we gather as part of the separate provider capability assessment process; we will publish our approach for this in Q2 of 2025.
Critical to the assessment approach is the early identification of emerging issues and concerns, so they can be addressed before they have a material impact or performance deteriorates further. If necessary, this could include the use of NHS England’s enforcement powers in response to emerging information outside of the segmentation process. Issues and concerns may be identified outside the quarterly review of segmentation and may not relate directly to segmentation data. Organisations should not wait for the next cycle of the assessment process to acknowledge performance, finance or quality concerns. ICBs and providers should promptly escalate all issues that are significantly affecting performance, finance or quality to their NHS England regional team.
Oversight of delegated commissioning
NHS England remains accountable for those services it has delegated responsibility for the commissioning of to ICBs. These include certain specialised services and all primary care services (primary medical care, dentistry, pharmacy and ophthalmic services) and the handling of associated complaints. NHS England will hold ICBs to account for the performance of these services in their system through delegation agreements.
Oversight of delegated functions will form part of NHS England’s wider oversight of ICBs. In particular, NHS England will use the ICB annual assessment to judge whether delegated commissioning activities and associated complaints handling are being carried out appropriately. This may involve the in-year monitoring of additional data in relation to delegated services.
Incentives and consequences
NHS England is committed to supporting providers and ICBs to drive improvement and deliver high quality care for all. We want to see high-performing systems across the country and to embed earned autonomy and incentives into the operating framework. There has already been progress: fewer national priorities in the planning guidance increases local flexibility in decision-making.
NHS England will work closely with those providers that are high performing, as reflected by their segment and their leadership capability, to draw on their expertise in shaping and driving national policy and to test new models of care.
NHS England will also introduce greater performance incentives in 2025/26 and these will be reviewed for 2026/27 as we implement the 10 Year Health Plan. For example, to incentivise revenue performance, the 2025/26 capital planning guidance proposes that high-performing providers and ICBs that demonstrate effective governance, strong financial management and operational resilience will receive some freedoms and flexibility, including a partial release of revenue surpluses for capital expenditure. As set out in the Elective Reform Plan, we also intend to introduce capital incentives for improvements in elective performance.
Furthermore, to hold senior leaders to account for their performance in delivering high quality care and managing finances, in line with the NHS very senior managers pay framework, very senior managers of organisations in segment 5 (noting the ICBs in the RSP will be treated as such) will not be eligible for the annual pay award, unless exempt.
Enforcement
NHS England’s oversight of ICBs and providers may involve the use of our regulatory powers to take enforcement action, in line with the NHS enforcement guidance, against a provider if it has breached its licence or we suspect it has.
NHS England has a range of statutory powers to address serious issues at providers. While the NHS Oversight Framework is the operational tool through which NHS England will identify providers that require support or intervention, where our assessment and monitoring highlight serious concern with performance, quality or other areas and, after further enquiries or investigation, we are satisfied that the relevant statutory thresholds are met, we may use our enforcement powers to address the concern, according to the level of concern and in accordance with the NHS enforcement guidance. We do not expect to use of our enforcement powers for organisations in segment 1 as they do not have intervention or support needs. However, if necessary (for example, if a serious leadership or governance concern emerges), we can still take enforcement action for organisations in this segment and their segment may be reviewed.
Where providers fail to comply with their obligations under their provider licence (or are reasonably suspected of failing), NHS England may use powers including:
- Provider undertakings – can be used where NHS England has reasonable grounds to suspect that a provider has failed to meet the conditions of its NHS provider licence. We may agree to accept legally binding undertakings to secure progress where providers are capable of resolving performance issues themselves.
- Provider discretionary requirements – can be imposed to require the remedy of a breach of an NHS provider licence where NHS England is satisfied that a breach has occurred. We may consider imposing discretionary requirements based on a range of considerations to ensure that progress is made, including where we do not have confidence the provider is taking sufficient action to resolve performance issues.
NHS England has powers in relation to NHS trusts that we may use in appropriate cases to effect executive leadership change, and the power to remove chairs and non-executive directors. For NHS foundation trusts, NHS England can also impose additional licence conditions relating to governance, breach of which may then lead to leadership change.
NHS England may consider using our powers of direction or additional licence conditions in more serious cases of governance failure.
More information can be found in the NHS enforcement guidance, including how NHS England chooses which powers to use and when, the factors we consider when enacting them and how we ensure consistency in approach.
Annex A: Delivery metrics
The assessment process measures each provider’s delivery across 6 domains, as set out in Table 1 of the framework. Each domain has a range of appropriate metrics for each type of organisation (ICB, acute, mental health, community and ambulance trusts); these are set out in the tables below. For this transitional year, the scoring metrics (in bold) reflect the 2025/26 NHS priorities and operational planning guidance. The other contextual metrics will not influence the segmentation score.
Table A1: Access domain metrics
These metrics relate to the national objectives set out in the 2025/26 NHS priorities and operational planning guidance and other commitments relating to the NHS Constitution. All metrics are scored (denoted in bold) other than 2 mental healthcare and 2 primary care contextual metrics which do not form part of the segment score.
Elective care
| Metric | Organisations to which the metric relates |
|---|---|
| Annual change in the size of the waiting list | Integrated care boards (contextual) |
| Percentage of cases where a patient is waiting 18 weeks or less for elective treatment (absolute performance and performance compared to plan) | Acute trusts |
| Percentage of cases where a patient is waiting more than 52 weeks for elective treatment | Acute trusts |
| Percentage of patients waiting over 52-weeks for community services | Community trusts |
Cancer
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of patients with cancer diagnosed or ruled out within 28 days of an urgent referral | Acute trusts |
| Percentage of patients treated for cancer within 62 days of referral | Acute trusts |
| Percentage of all cancers diagnosed at stage 1 or 2 | Integrated care boards (contextual) |
Urgent and emergency care
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of emergency department attendances admitted, transferred or discharged within 4 hours | Acute trusts |
| Percentage of emergency department attendances spending over 12 hours in the department | Acute trusts |
| Average Category 2 ambulance response time | Ambulance trusts |
Mental health care
| Metric | Organisations to which the metric relates |
|---|---|
| Annual change in number of children and young people accessing NHS-funded MH services | Mental health trusts |
| Community mental health access rate | Mental health trusts |
| Percentage of people with suspected autism waiting more than 13 weeks for contact | Mental health trusts |
Primary care
| Metric | Organisations to which the metric relates |
|---|---|
| Growth in number of urgent dental appointments provided versus target | Integrated care boards (contextual) |
| Percentage of patients to describe booking a general practice appointment as easy | Integrated care boards (contextual) |
Table A2: Effectiveness and experience of care domain metrics
These metrics relate to the role of NHS bodies to continuously improve the quality of care patients receive. Most metrics are scored (bold), but some are non-scoring contextual metrics and therefore do not contribute to the overall domain and segment score.
| Metric | Organisations to which the metric relates |
|---|---|
| Summary Hospital Level Mortality Indicator | Acute trusts |
| Acute bed days per 100,000 people | Integrated care boards (contextual) |
| Change in the number of inpatients who are autistic or have a learning disability | Integrated care boards (contextual) |
| Average number of days from discharge ready date and actual discharge date | Integrated care boards (contextual) and acute trusts |
| Percentage of continuing healthcare referrals completed in 28 days | Integrated care boards (contextual) |
| Readmission rate band | Acute, community and mental health trusts |
| Percentage of mental health bed days that are out of area | Integrated care boards (contextual) |
| CQC inpatient survey satisfaction rate | Acute trusts |
| National maternity survey score | Acute trusts |
| Percentage of inpatients with >60 day length of stay | Mental health trusts |
| Urgent community response 2-hour performance | Community trusts |
| Community mental health survey satisfaction rate | Mental health trusts |
| Percentage of ambulance patients conveyed to emergency departments | Ambulance trusts |
| NHS staff survey – advocacy score | Ambulance trusts |
Primary care
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of patients who receive all 8 diabetes care processes | Integrated care boards (contextual) |
| Percentage of patients with GP recorded CVD who have their cholesterol levels managed to NICE guidance | Integrated care boards (contextual) |
| Percentage of hypertension patients treated to target | Integrated care boards (contextual) |
| Percentage of patients with a preferred general practice professional reporting they were able to get an appointment with that professional | Integrated care boards (contextual) |
Table A3: Patient safety domain metrics
These metrics relate to how organisations ensure that patients are kept safe, a core element of high-quality care. Most are scored (bold), but some are non-scoring contextual metrics.
| Metric | Organisations to which the metric relates |
|---|---|
| NHS Staff Survey – raising concerns sub-score | All organisations (contextual only for ICBs) |
| CQC safe inspection score (if awarded within the preceding 2 years) | All trusts |
| Rates of Healthcare Associated Infection (MRSA, C-Difficile and E-Coli) | Acute trusts |
| Number of neonatal deaths and stillbirths per 1,000 total births | Integrated care boards (contextual) |
| Rate of restrictive interventions use | Mental health trusts |
| Percentage of patients in crisis to receive face-to-face contact within 24 hours | Mental health trusts |
| Percentage of inpatients acquiring a new pressure ulcer | Acute trusts (contextual) |
Primary care
| Metric | Organisations to which the metric relates |
|---|---|
| Percentage of children (aged 0 – 9) prescribed antibiotics in the last 12 months | Integrated care boards (contextual) |
Table A4: People and workforce domain metrics
These metrics relate to how NHS organisations ensure the wellbeing of those who provide and support care. These are a mix of scored (bold) and contextual metrics.
| Metric | Organisations to which the metric relates |
|---|---|
| Sickness absence rate | All trusts (contextual only for ICBs) |
| NHS staff survey engagement theme score | All trusts (contextual only for ICBs) |
| NHS staff survey education and training theme score | Integrated care boards (contextual) |
| National Education and Training Survey overall satisfaction score | All trusts (contextual) |
Primary care
| Metric | Organisations to which the metric relates |
|---|---|
| GP leaver rate | Integrated care boards (contextual) |
Table A5: Finance and productivity domain metrics
These metrics will be used to judge individual organisational financial delivery. They all contribute to trust segmentation but are contextual for ICBs.
Finance
| Metric | Organisations to which the metric relates |
|---|---|
| Planned surplus/deficit | All organisations (contextual only for ICBs) |
| Variance year-to-date to financial plan | All organisations (contextual only for ICBs) |
Productivity
| Metric | Organisations to which the metric relates |
|---|---|
| Implied productivity level | Integrated care boards (contextual only) and acute trusts |
| Relative difference in costs | Mental health, community and ambulance trusts |
Table A6: Improving health and reducing inequality domain metrics
These metrics relate to longer-term priorities aimed at improving population health and reducing inequalities. They are all non-scoring contextual metrics and therefore do not contribute to the overall domain and segment score.
Improving population health
| Metric | Organisations to which the metric relates |
|---|---|
| Average number of years people live in healthy life | Integrated care boards |
| Percentage of patients receiving talking therapies who achieve reliable recovery | Mental health trusts |
Primary prevention
| Metric | Organisations to which the metric relates |
|---|---|
| Cervical, breast and bowel cancer screening rates | Integrated care boards |
| Percentage of pregnant women who quit smoking | Integrated care boards |
| Percentage of inpatients referred to in-house tobacco treatment services who make a supported attempt to quit stop smoking | Acute and community trusts |
| Percentage of patients supported by obesity programmes | Integrated care boards |
| MMR vaccine uptake rate | Integrated care boards |
| Percentage of people waiting over 6 weeks for a diagnostic procedure or test | Acute trusts |
Inequalities
| Metric | Organisations to which the metric relates |
|---|---|
| Deprivation and ethnicity gap in pre-term births | Integrated care boards |
| Deprivation gap in early cancer diagnosis gap | Integrated care boards |
| Deprivation gap in myocardial infarction and stroke admissions | Integrated care boards |
| Percentage of annual health checks completed for patients with a learning disability or who are autistic | Integrated care boards |
| Under 18s elective waiting list growth | Acute trusts |
| Percentage of older inpatients (over 65) with >90 day length of stay | Mental health trusts |
Table A7: System performance for ICBs
These metrics relate to tests applied at a whole system level for ICBs. They are contextual metrics and not applied in 2025/26.
| National priority | Test |
|---|---|
| Urgent and emergency care | Has the system been in the lowest quartile for 4 hour UEC performance for each of the last three months? |
| Elective care | Has the system been in the lowest quartile for 18-week performance for each month of the last quarter? |
| Cancer care | Has the system been in the lowest quartile for 62-day performance for each month of the last quarter? |
| Primary care | Is the system in the lowest quartile for overall primary care patient satisfaction? |
| Mental health | Is the system’s proportion of annual physical health checks for those with severe mental illness completed in the last year below 60%? |
| Finance | Is the system projecting an annual deficit of over 2.5% or a deficit below 2.5% that is over 1% off plan? |
Publication reference: PRN02028

