Summary
This interim policy statement sets out the criteria for perinatal post-mortem investigation of fetal and neonatal deaths in England and Wales.
The new interim access policy and the histopathological examination of placenta guidance aim to support greater standardisation in access to perinatal post-mortem investigations and placental examinations, and the prioritisation of available perinatal pathology capacity.
This policy updates and replaces the previous interim clinical policy statement Perinatal post-mortem investigation of fetal and neonatal deaths (England, Scotland and Wales) published on the 27 October 2022. This policy has been revised in the context of the Royal College of Pathologist (RCPath) Guidelines (G108, G143, G160) published June 2024. The new RCPath guidelines cover the spectrum of post-mortem clinical scenarios that present to perinatal pathologists and the range of post-mortem options available to pathologist. Clinicians are encouraged to read this policy alongside the RCPath guidelines.
Links and updates to other policies and documents
This policy relates to the following guidance, practices and specification:
Replaces:
The interim clinical policy statement Perinatal post-mortem investigation of fetal and neonatal deaths (England, Scotland and Wales) published on the 27 October 2022.
Links to:
Royal College of Pathologists:
- G160: Guideline on autopsy practice: Third trimester antepartum and intrapartum stillbirth
- G161 Guidelines on autopsy practice: Fetal autopsy of 2nd trimester fetal loss (excluding termination of pregnancy for congenital anomaly)
- G193 Guidelines on autopsy practice: Fetal autopsy after termination of pregnancy or fetal loss associated with congenital anomaly
- G108: Tissue Pathway for histopathological examination of the placenta
- G143: Guidelines on staffing and workload for paediatric and perinatal pathology departments
National Institute for Health and Care Research (NIHR):
Human Tissue Authority (HTA):
(England only) NHS England Commissioning Service Specification: Perinatal Pathology
Plain language summary
About perinatal autopsy services
Perinatal post-mortem examination (also called an autopsy) refers to a specialist medical examination that is completed following the death of a fetus or baby. Post-mortem examination traditionally refers to a collection of investigations including: external examination, examination of all of the internal organs (usually via two or more cuts into the body), examining small samples of tissue under a microscope, and a range of imaging techniques as appropriate, medical photographs and other tests such as genetic investigations. Tests may also be done for infection and other possible causes of death or complications. The placenta where relevant will also be examined.
Post-mortem examination can be carried out from 12 to 40 weeks gestation and after birth. For the purposes of this policy statement, this period is referred to as the perinatal period and relates to post-mortem examinations performed for fetuses and babies who were aged up to 28 days old when they died.
The role of the autopsy is twofold; firstly, the pathologist reviews the clinical and postmortem examination findings to suggest how (where possible) a fetus or baby died. Perinatal autopsy is also used to identify diseases that may have implications for future pregnancies (including genetic diseases).
Bereaved parents want to know why their baby died. Post-mortem investigations offer a possibility of answers, even if it is to rule things out. The post-mortem can be an important part of a parent’s path through their grief and may inform decisions about another pregnancy. Parents will often feel protective and strongly connected to their baby. Therefore, it is vital that this is acknowledged and parents’ wishes are held at the heart of perinatal post-mortem services. Liaison between the parents, referring clinician, consultant perinatal pathologist and wider clinical team will take place to determine the most appropriate investigation(s)*. In some cases, postmortem will not provide a cause of death.
* Where parents have consented to a full post-mortem, the pathologist should consider the parents’ request, but if they determine to safely undertake fewer or less extensive investigations, then the reasons will be documented within the post-mortem report. See Perinatal post-mortem investigative pathway.
Perinatal post-mortem examination (outside of HM Coronial system) can only be performed if informed consent has been given, typically by the mother. This consent sets the limits for the investigations after death. Fetal tissue is considered in law to be the tissue of the mother and therefore tissue from the living. In cases where the fetus has survived outside of the womb, consent can be obtained from either the mother or the maternal partner if they are married, in a civil partnership or with declared parental responsibility.
In the UK, perinatal pathology protocols are published by the RCPath and their implementation overseen by the United Kingdom Accreditation Service (UKAS) as per ISO standard 15189. In England, Northern Ireland and Wales, autopsy facilities and procedures must be covered by appropriate licencing issued in line with the Human Tissue Act (HTA) 2004, and consent procedures must be compliant with the relevant HTA Code of Practice. The Human Tissue Regulations 2007 cover England, Northern Ireland, Wales and Scotland.
Epidemiology and needs assessment
Extended perinatal mortality in the UK has reduced by 20% over seven years, from 6.04 per 1,000 total births in 2013 to 4.85 per 1,000 total births in 2020, equivalent to approximately 820 fewer deaths in 2020 (MBRRACE-UK, 2022). Stillbirth rates in the UK have reduced by 21%, from 4.20 per 1,000 total births in 2013 to 3.33 per 1,000 total births in 2020, representing approximately 605 fewer stillbirths in 2020 (MBRRACE-UK, 2022).
Across the four UK nations the lowest stillbirth rate is 2020 was in England (3.29 per 1,000 total births) whilst the lowest rate of neonatal mortality was in Scotland (1.47 per 1,000 lives births) (MBRACCE-UK, 2022). Neonatal mortality in the UK has reduced by 17% from 1.84 per 1,000 live births in 2013 to 1.53 deaths per 1,000 live births in 2020, representing approximately 215 fewer neonatal deaths in 2020 and an increased rate of reduction. (MBRRACE-UK, 2022).
In 2020, parents were offered a post-mortem for 98% of stillborn babies but only 86% of neonatal deaths in 2020 (MBRACCE-UK 2022). Where a post-mortem examination was offered, consent was given for half of stillbirths (53%) and one-third of neonatal deaths (34%) (MBRACCE-UK, 2022).
Policy criteria
Perinatal pathological examination will be commissioned in England, Scotland and Wales in line with the following criteria:
Inclusion criteria
- Fetus is of 12-23 completed weeks gestation OR
- Stillbirth from any cause > 24 weeks gestation; OR
- Fetal anomaly without a unifying diagnosis (including suspected skeletal dysplasia); OR
- Referral from specialist fetal medicine team; OR
- Intra partum death (if not referred to His Majesty’s (HM) Coroner); OR
- Neonatal death (if not referred to HM Coroner)
Exclusion criteria
- Fetal gestation < 12 weeks
- Clinically documented abruption at delivery (if day 10 falls on a weekend then the approval can be sought on the last working day before the weekend)
- All antenatally diagnosed aneuploidy (e.g., Known T13/18/21 monosomy X/22q deletion)
- Uncomplicated anomaly where the unifying clinical and/or genetic diagnosis has been definitively determined (e.g., uncomplicated neural tube defect) and post-mortem examination is unlikely to yield any further useful information
- Cases where the only clinical question is determination of sex
- Cases which require cytogenetic sampling only
The need for a perinatal pathological examination in exceptional scenarios can be considered by the responsible pathologist as per the inclusion criteria. The extent of the examination should be determined by the ceiling of consent provided by the parents and the clinical judgement of the responsible pathologist, guided by the ultimate goal of the likelihood of identification of significant findings.
When NHS England Mutual Aid arrangements for access to full postmortem have been attempted but it has proven not possible to implement such aid, then from day 10 (from date of death), the Exceptional Circumstances Protocol for perinatal pathology can be followed (appendix a).
Perinatal post-mortem investigative pathway
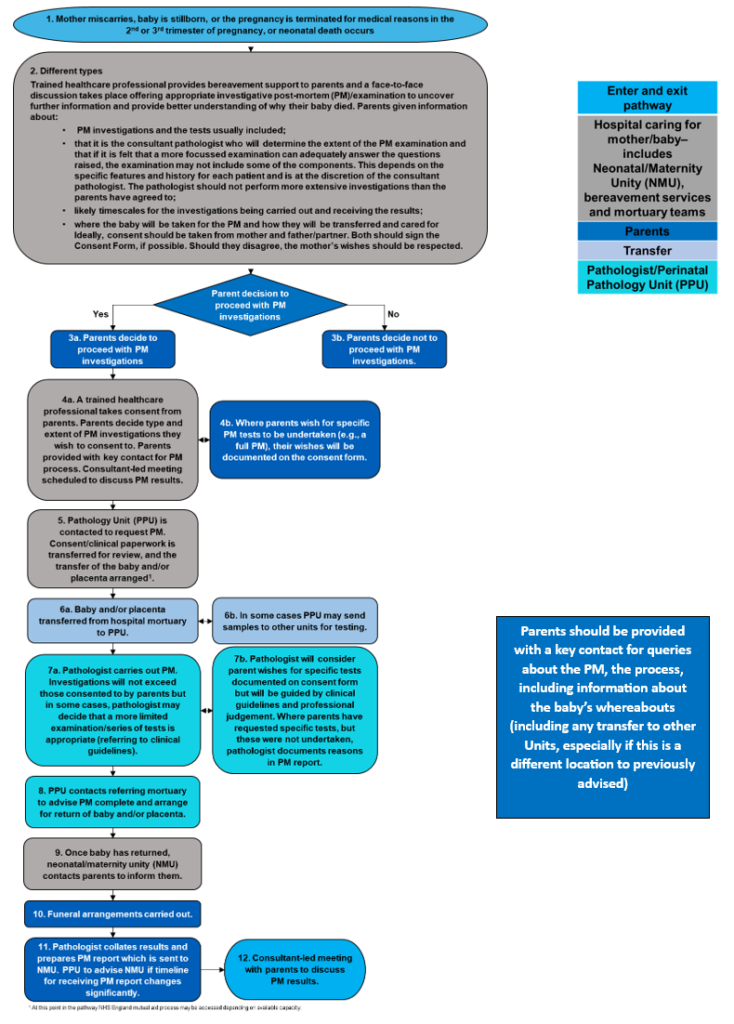
Download the Perinatal post-mortem investigative pathway in PDF format.
Audit requirements
Laboratory and mortuary services are accredited by UKAS under ISO18159. Policy audit forms an important part of the clinical governance of mortuary services and should be covered as part of accreditation at local trust/health board level. Furthermore, audits should be conducted in accordance with HTA standards and guidance (Post-mortem licensing standards and guidance).
Policy review date
This document will be reviewed when there are significant changes in clinical evidence and/or change in perinatal pathology capacity which indicate that the policy requires revision. If a review is needed due to a new evidence base then a new Preliminary Policy Proposal needs to be submitted by contacting england.CET@nhs.net.
Equality statement
Promoting equality and addressing health inequalities are at the heart of the two nation’s values. Throughout the development of the policies and processes cited in this document, we have:
- Given due regard to the need to eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it; and
- Given regard to the need to reduce inequalities between patients in access to, and outcomes from healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities.
References
Lees, C., Breeze, A., Sebire, N., Hutchinson, C. and Jessop, F., 2021. Report of the Joint Fetal Medicine & Perinatal Pathology Working Group: A Subgroup of the Specialised Womens’ CRG. Draft Report.. Specialised Women’s CRG.
Elizabeth S Draper, Ian D Gallimore, Lucy K Smith, Ruth J Matthews, Alan C Fenton, Jennifer J Kurinczuk, Peter W Smith, Bradley N Manktelow (2022). MBRRACE-UK Perinatal Mortality Surveillance Report. UK Perinatal Deaths for Births from January to December 2020. Department of Health Sciences University of Leicester.
Evans, M., Draper, E. and Smith, L., 2020. Impact of sociodemographic and clinical factors on offer and parental consent to postmortem following stillbirth or neonatal death: a UK population-based cohort study. Archives of Disease in Childhood – Fetal and Neonatal Edition, 105(5), pp.532-537.
Marton, T., Hargitai, B., Jessop, F., Hutchinson, C., Lees C., Johnston T., et al. 2024 Guidelines on autopsy practice: Fetal autopsy following antepartum or intrapartum death of non-malformed fetuses (G160) Royal College of Pathologists.
Marton, T., Hargitai, B., Jessop, F., Hutchinson, C., Lees C., Johnston T., et al. 2024 Guidelines on autopsy practice: Fetal autopsy of 2nd trimester fetal loss (excluding termination of pregnancy for congenital anomaly (G161) Royal College of Pathologists.
Marton, T., Hargitai, B., Jessop, F., Hutchinson, C., Lees C., Johnston T., et al. 2024 Guidelines on autopsy practice: Fetal autopsy after termination of pregnancy or fetal loss associated with congenital anomaly (G193) Royal College of Pathologists.
Appendix A – Exceptional circumstances protocol for perinatal pathology – England
To be applied when NHS England Mutual Aid arrangements have been unable to implement MA arrangements in a suitable timeframe.
Exceptional circumstances protocol for perinatal pathology
1. Introduction
- In those circumstances where it is not possible to provide a full postmortem as part of NHS England’s Mutual Aid arrangements for perinatal pathology, the Exceptional Circumstances Protocol can be activated on a case-by-case basis by NHS England. From day 10 (from date of death), the provider can seek approval through their internal hospital trust arrangements to request access to the protocol. The Trust will then notify NHS England that they have initiated the protocol and request a less invasive investigation through pre-agreed arrangements in place with other providers (and detailed within a pre-agreed Standard Operating Procedure).
- The investigations and assessments that are used as part of this protocol are consistent with standard practice and postmortem guidance relating to less invasive and external examinations. The less invasive examination may involve X-ray, other imaging modalities including CT and MRI, the use of photography, routine measurements, placental examination and genetic testing (but not internal examination). These investigations may provide sufficient clinical yield to provide bereaved parents and clinicians with a report in the absence of a postmortem 1,2,3.
Access to the protocol is assessed on a case-by-case basis and subject to clinical triageas detailed within a pre-agreed Standard Operating Procedure. Individual providers can only enact the protocol in exceptional circumstances and with the agreement of NHS England. Whilst in some cases the examinations can provide sufficient clinical yield to present bereaved parents with a report in the absence of complete/full postmortem, this will not be the case in all circumstances. The Perinatal Pathology service requesting mutual aid will inform NHS England and referrers if they are unable to provide a full/complete postmortem when a less invasive investigation has been deemed not suitable during triage. Referring services will inform parents of the situation.
The RCPath recognises that there is an accumulating body of evidence that a less-invasive approach can, in some circumstances, complement or replace dissection based post-mortem examination.
References
- Fetal autopsy of 2nd trimester fetal loss (excluding termination of pregnancy for congenital anomaly) – The Royal College of Pathologists
- Fetal autopsy following antepartum or intrapartum death of non-malformed fetuses – The Royal College of Pathologists
- Fetal autopsy after termination of pregnancy or fetal loss associated with congenital anomaly – The Royal College of Pathologists
- Lewis C, Hutchinson JC, Riddington M, Hill M, Arthurs OJ, Fisher J et al. Minimally invasive autopsy for fetuses and children based on a combination of post-mortem MRI and endoscopic examination: a feasibility study. Health Technol Assess 2019;23:1–104.
- Shelmerdine SC, Simcock IC, Hutchinson JC, Guy A, Ashworth MT, Sebire NJ et al. Postmortem microfocus computed tomography for noninvasive autopsies: experience in >250 human fetuses. Am J Obstet Gynecol 2021;224:103.
- Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong W, Olsen O et al. Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 2013;20:223–233.

