1. Foreword
Since the publication of Professor Sir Mike Richards’ independent report ‘Diagnostics; Recovery and Renewal’ and the need to bring diagnostic waits back to pre-Covid levels, diagnostics transformation has become a priority that has received significant government investment.
This offers us a unique opportunity to shape physiological science (PS) services so that they can deliver to future needs and circumstances. PS networks have a critical role to play in making this transformation a reality.
Networks and alliances bring together teams working in specific areas of healthcare to help facilitate delivery of high quality, efficient and patient-centred services.
Clinical networks have demonstrated that they can improve patient outcomes and care processes and by working together can achieve successful service improvement and transformation. We have seen this in other areas related to cardiology, cancer, respiratory networks, and diagnostic networks such as pathology and imaging.
We know that PS services have had a low profile and been poorly understood and resourced for decades, in part due to the multiple disciplines that contribute to PS. The important role they play in supporting patients and clinicians in the diagnosis, assessment, and treatment of health issues across the whole life span cannot be underestimated.
With the recommendations from the independent review of diagnostic services, the need to recover from Covid and reduce waiting times for diagnosis and disease management, it is essential that PS services, acute and community providers trusts leaders, integrated care boards (ICBs) come together as a network along with patients and other experts within regions to help transform these services.
They will play a key role in elective recovery, ensuring high quality accredited PS services, so that people can access the right PS tests, at the right time, performed by the right person.
The establishment of PS networks will help drive the reorganisation and transformation of services at regional and local level. They will enable greater connectivity between individual services, driving standardisation, improving quality, supporting training and career progression and, create opportunities for shared learning between and across individual groups and services.
Dr Martin Allen, National Specialty Adviser for Physiological Science, NHS England.
2. Introduction
Physiological sciences play an essential role in supporting patients and clinicians in the diagnosis, assessment and treatment of health issues across the whole life span.
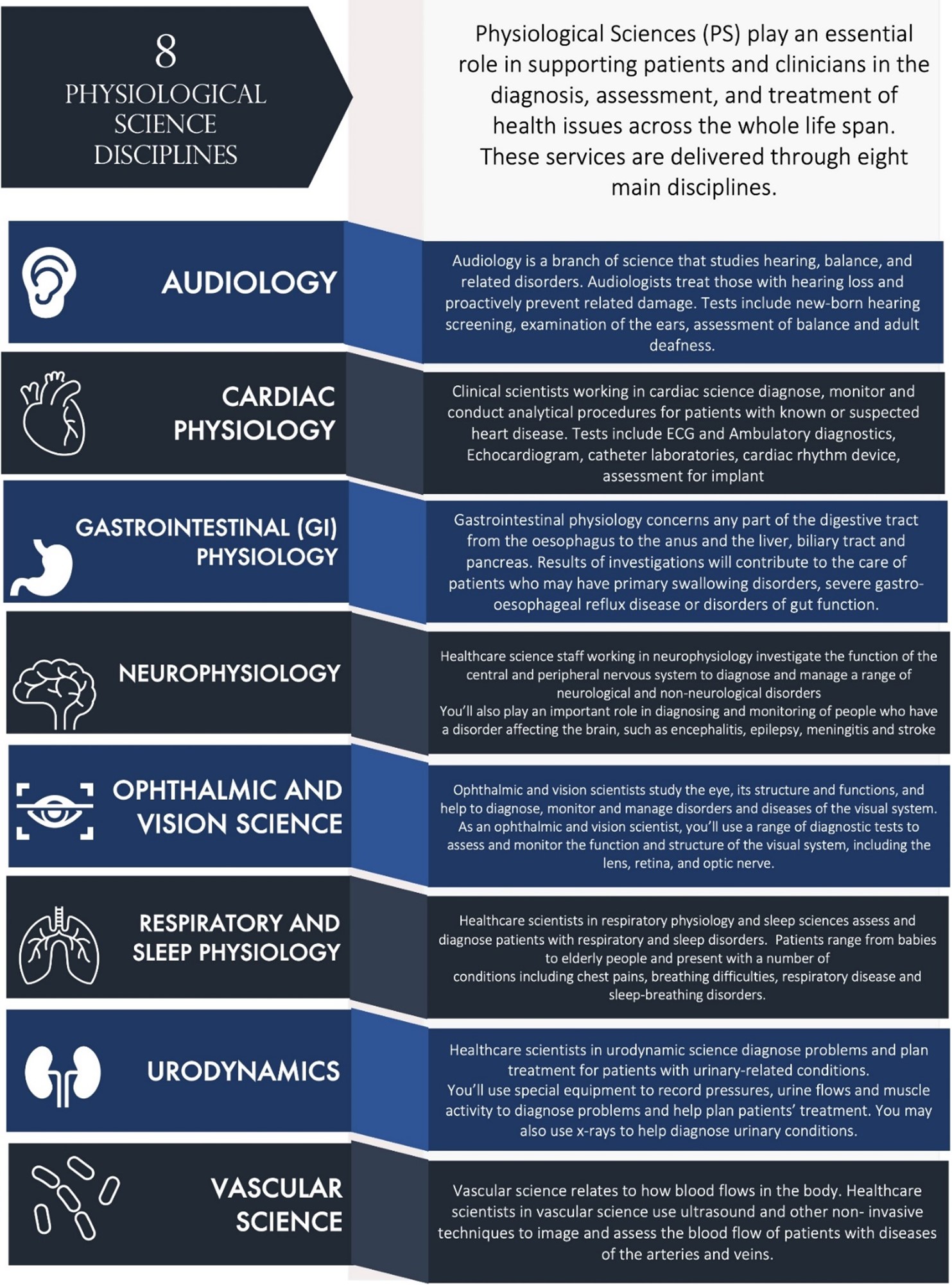
These services (summarised in figure 1 below) are delivered through eight main disciplines: audiology; cardiac physiology; gastrointestinal (GI) physiology; neurophysiology; ophthalmic and vision science; respiratory and sleep physiology; urodynamics; vascular science.
Across all these disciplines, PS enables diagnosis, assessment and monitoring as well as the delivery of therapeutic interventions. These services provide information on the extent of disease or disability and the provision and/or response to therapeutic interventions.
Local delivery of these clinical services is likely to be dispersed across provider organisations with each discipline often sitting in a different directorate or care group and are not usually part of a distinct PS department or unit. Some services will be set up specifically for children and younger people, but often children will access tests and procedures in areas dealing predominantly with the adult population.
Despite their core role, PS services have traditionally had a low profile and been poorly understood, often embedded within block contract arrangements and not recognised as an integral service entity. However, it is increasingly recognised that these services form essential components of most patient pathways, impacting significantly on access, outcomes and experience of care for millions of NHS patients.
PS networks will help transform the way in which these services operate and enable improved outcomes that matter to patients. Networks will help facilitate delivery of high quality, efficient, and patient-centred care. They will play a key role in the recovery of diagnostic services and help ensure both the current and future workforce can deliver to future needs and circumstances.
Figure 1: Physiological science disciplines
Image text:
8 physiological science disciplines
Physiological Sciences (PS) play an essential role in supporting patients and clinicians in the diagnosis, assessment, and treatment of health issues across the whole life span. These services are delivered through eight main disciplines.
- AUDIOLOGY – Audiology is a branch of science that studies hearing, balance, and related disorders. Audiologists treat those with hearing loss and proactively prevent related damage. Tests include new-born hearing screening, examination of the ears, assessment of balance and adult deafness.
- CARDIAC PHYSIOLOGY – Clinical scientists working in cardiac science diagnose, monitor and conduct analytical procedures for patients with known or suspected heart disease. Tests include ECG and Ambulatory diagnostics, Echocardiogram, catheter laboratories, cardiac rhythm device, assessment for implant
- GASTROINTESTINAL (GI) PHYSIOLOGY – Gastrointestinal physiology concerns any part of the digestive tract from the oesophagus to the anus and the liver, biliary tract and pancreas. Results of investigations will contribute to the care of patients who may have primary swallowing disorders, severe gastro-oesophageal reflux disease or disorders of gut function.
- NEUROPHYSIOLOGY – Healthcare science staff working in neurophysiology investigate the function of the central and peripheral nervous system to diagnose and manage a range of neurological and non-neurological disorders. You’ll also play an important role in diagnosing and monitoring of people who have a disorder affecting the brain, such as encephalitis, epilepsy, meningitis and stroke.
- OPHTHALMIC AND VISION SCIENCE – Ophthalmic and vision scientists study the eye, its structure and functions, and help to diagnose, monitor and manage disorders and diseases of the visual system. As an ophthalmic and vision scientist, you’ll use a range of diagnostic tests to assess and monitor the function and structure of the visual system, including the lens, retina, and optic nerve.
- RESPIRATORY AND SLEEP PHYSIOLOGY – Healthcare scientists in respiratory physiology and sleep sciences assess and diagnose patients with respiratory and sleep disorders. Patients range from babies to elderly people and present with a number of conditions including chest pains, breathing difficulties, respiratory disease and sleep-breathing disorders.
- URODYNAMICS – You’ll use special equipment to record pressures, urine flows and muscle
activity to diagnose problems and help plan patients’ treatment. You may also use x-rays to help diagnose urinary conditions. - VASCULAR SCIENCE – Vascular science relates to how blood flows in the body. Healthcare
scientists in vascular science use ultrasound and other non-invasive techniques to image and assess the blood flow of patients with diseases of the arteries and veins.
“For too many decades the importance, contribution and expertise of this hugely important scientific workforce and the services it provides have quietly developed and nurtured cutting edge technologies, brilliant innovations, and the highest levels of care without the broader NHS understanding or knowing about it.
“PS networks and communities of practice are beginning to awake managers and strategists to the enormous potential to streamline patient pathways and modernise diagnostics in the community.
“There are many challenges to overcome. Expanding physiological diagnostics while tackling the legacies of the pandemic will take time, but there is no doubt about the wisdom of investing in PS to make the NHS ready for the next 75 years.”
Prof. Brendan Cooper B.Sc. (Hons), M.Sc., Ph.D., C.Biol, FRSB, FERS. President, Academy for Healthcare Science.
This framework provides advice and guidance on establishing a PS network as outlined in the Richards review of NHS diagnostics: ‘Recovery and Renewal’ and will enable delivery of the NHS Long Term Plan commitments on diagnostics. It is intended to provide a high-level development framework to support PS teams, service providers, regions and integrated care systems (ICSs) to come together and implement arrangements which meet local and regional circumstances and need.
The expectation is that PS networks will be developed during 2023/24 and working to a common standard by March 2024.
The framework has been developed in collaboration with PS service leads and other stakeholders across England. It sets out the expected purpose, benefits, suggested design features and key requirements for success. It also provides details of national and regional support available.
“I’m delighted to see the formation of the PS networks and the bringing together of these relatively small but important clinical and scientific services.
“They are crucial to the delivery of high-quality diagnostics, as well as supporting the assessment and treatment of a range of health conditions. Importantly, they will play a key role in driving forward transformation and improvements to the way services need to be delivered for the future.”
Professor Dame Sue Hill. Chief Scientific Officer, England.
3. Network development
The initial steps that all health communities need to take are outlined below. Regions will play a key role in the initial development stages. The steps outlined are not linear and several steps will be taken at the same time.
We would expect networks to complete most of the initial enablement steps outlined by the end of 2023-24 and operating as a network to a common standard framework by March 2024.
Initial steps in network development
Develop a common purpose and vision
- Bring stakeholders together to gain input into the purpose, priorities and how the network may operate.
- Develop terms of reference, core values and a vision that inspires collaboration across service providers of the eight PS disciplines that will enable the network to deliver on its clinical and operational objectives.
- Develop and agree the high level transformational goals of the PS network with your key stakeholders (incluidng the ICBs and NHS England), which are designed to improve patient outcomes across all PS services.
Establish the network footprint
- Undertake a mapping exrecise to identify the service configuration of each of the PS disciplines across the region alongside identification of existing networks that the PS network would need to work with.
- Agree the footprint of the PS network, ensuring that the configuration decision is suported by all ICBs involved and the NHS England region.
Establish leadership, governance and workplan
- Identify an executive sponsor of the network and appoint a senior responsible officer (SRO).
- Define the leadership roles for the networks and set out role descriptions for each role.
- Recruit to the network senior leadership team and identify leadership training needs.
- Further define the operational structure with a clear accountability framework and establish key workstreams and disciple specific groups around the priorities identifying a lead for each workstream.
- Develop the PS network first annual workplan, that covers a range of workstreams and plans for each PS discipline.
When developing the network workplan, we would expect the network to prioritise work around:
- Workforce and training working with professional bodies, higher education institutions and the School of Healthcare Science to address issues across the eight disciplines.
- Digital infrastructure which will unify services across a region and enable the sharing of information seamlessly.
- Demand and capacity using all available data to plan and manage capacity and demand and determine any systems or providers that need urgent support.
- Quality assurance, developing a quality framework that aligns with the current improving quality in physiological services (IQIPS) standard that allows all disciplines within a provider in the network to meet the requirements for quality and competency that allows accreditation of all PS services within a trust.
As the network matures, we would expect to the workplan also work on research and innovation working alongside professional societies, the research community, providers, and the Academic Health Science Networks (AHSNs) to identify innovations that can transform the way services can be delivered.
Networks will need to adopt a maturity model which NHS England will develop in collaboration to help guide their first three years of development.
4. A national mandate to improve physiological science services
Diagnostics is recognised as a priority in the NHS Long Term Plan. Getting diagnostic provision right is a key enabler of several of the plan’s commitments, including those on cancer, heart disease and respiratory disease, along with outpatient transformation.
Increasing diagnostic capacity can be expected to improve care outcomes for major health conditions by providing quicker access to diagnostics and therefore earlier diagnosis. It also indirectly supports broader ambitions to transform health and care services across the NHS and the target of under six week waits for diagnostics.
In the NHS Long Term Plan, Professor Sir Mike Richards was commissioned to undertake a review of NHS diagnostics capacity. The independent report, Diagnostics: Recovery and Renewal, 2020, recommended significant reform and investment in diagnostic services.
These recommendations covered:
- new service delivery models (including the separation of elective and urgent pathways)
- investment in equipment and facilities
- workforce development
- service digitisation and connectivity
- key enablers to drive and deliver the required change such as the establishment of networks.
The suite of recommendations is aimed at increasing and optimising diagnostic capacity and improving efficiency. Which in turn will reduce waiting times and diagnostic backlogs, manage the safe delivery of diagnostic provision and improve patient outcomes.
To meet the recommendations, set out in the Richard’s Review, the National Diagnostics Transformation Programme has been established and includes the Physiological Science Transformation Programme.
The Physiological Transformation Programme aims to improve outcomes that matter to patients, by enabling delivery and access to the right physiological tests at the right time performed by the right person.
Key enablers to this which the programme is focusing on include improving service level data to understand PS services, establishing PS networks and developing workforce capacity and capability. More information about the programme can be found on the Physiological Science’s FutureNHS Platform.
Below outlines what good PS services may look like in the future.
What good physiological science services may look like:
Service model
- Greater service reliance, sites connected through networks.
- Closer working between disciplines, eg cardio/respiratory.
- Services are closer to people who need them including at home and in the community.
Workforce
- Development of new roles and opportunities for progresion.
- Co-ordination of training across services through academy models.
- Greater leadership opportunities for physiologists.
Operational elements
- Services are externally accredited.
- Skilled physiologists are supported to work across organisations.
- Embedding into and working with establish networks, eg cardiac, respiratory.
Enablers
- Physiological science teams improve, innovate and learn together.
- Services are digitally connected, improving service delivery and quality.
- Greater visibility and profile of the service.
- Services are informed by the needs and experiences of people who use services.
- Services are engaged with national, regional and system agendas and have good stakeholder engagement.
5. Why networks?
PS networks are a key element to achieving our vision, improving performance and developing PS services that can meet population needs and help reduce health inequalities.
Clinical networks are often an essential ingredient for successful service improvement, and transformation. Patient-centred and population-focused, clinical networks bring together teams focussed on a specific area of healthcare, across traditional organisational boundaries, delivering benefits through multi-professional, inter-disciplinary or cross-organisational working.
Networks are considered an essential component of the drive to transform diagnostic services. Imaging and pathology networks have already been established across England, and endoscopy and PS networks are recommended in the Richards Review.
“PS networks will help connect services to improve quality, efficiency and sustainability.
“They will enable skilled staff to work and train across multiple sites, improving capacity. They will support digital innovations to bring services closer to patients, mitigate workforce shortages and reduce analytical/reporting time”
Professor Sir Mike Richards
PS networks will form a key element in the recovery and transformation of these important services across England. The development of these networks provides a unique opportunity to improve outcomes that matter to patients for a range of disease areas by improving access, service quality and the care they receive from PS services.
Networks will also play an important role in raising the profile of healthcare sciences, especially PS within the NHS.
It is intended that networks will support the delivery and achievement of the following benefits:
1. Improving performance and outcomes for patients
- A PS network’s core purpose will be improving patient outcomes.
- This will be achieved by implementing new service models to improve access to diagnostic tests and therapy, working collectively to manage resources and service capacity for the benefit of the populations they serve.
- Quality (both QI and QA) will be central to every network’s objective. PS networks will need to work in alignment with disease specific networks such as cardiac, respiratory or neurology networks and be included in pathway re-design work.
2. Developing the PS workforce
- Workforce planning and collective co-ordination around education and training, including training capacity and leadership development, should be priority areas for all PS networks.
- Leadership development and innovating with new roles and rapidly spreading what works well will enable service transformation.
3. Digitisation and innovation
- All PS services will need to implement digital approaches, across requesting, scheduling, testing and reporting.
- They will need to ensure they are part of wider established digital programmes and will need to develop capability in the rapid evaluation and implementation of new innovations.
4. Analytically led services
- Networks will be analytically led, using data (for example the national stocktake collections) to benchmark and improve service performance and inform where additional support may be required.
What networks will actually do
We acknowledge PS networks will develop and mature at a pace specific to their region. Established ‘communities of practice’ can form a sound basis to develop towards a fully-fledged PS network.
Realising the benefits set out above will take time and will be built on developing strong relationships and collaborative ways of working.
At the Physiological Science Stakeholder Workshop held in September 2022, stakeholders informed this list of areas a network should aim to deliver on:
- Raising the profile and increasing representation of PS services and healthcare sciences at regional, system, and provider level.
- Providing leadership to support the development and collaboration of efficient pathways.
- Supporting quality management and improvement using data to understand variation and improve service delivery. Enabling improved rates of service accreditation through IQIPs.
- Co-ordinating investment in service infrastructure through the stewardship of resources including capital planning and collective procurement.
- Workforce planning including capacity and demand modelling and facilitation of staff working across NHS boundaries.
- Co-ordination of education and training resources to support workforce priorities and career progression.
- Acting as a single point of access for other networks, alliances, and CDCs where there is an interdependency.
- Supporting the facilitation of best practice across the network.
- Supporting engagement with research to ensure services continually evolve and improve.
- Co-ordinate initiatives to learn from patient experience of PS services.
6. Network success factors
In the commissioned review by the Health Foundation to better understand how networks can support healthcare improvement, they identified five core features of effective networks. These included:
- having a common purpose
- a co-operative structure
- critical mass
- collective intelligence
- community building.
A common purpose brings network members together, keeping them aligned and moving in the same direction. A network would otherwise lack sufficient focus to drive its cause forward.
Next, a network can establish a cooperative structure that allows people to work together across organisations, make decisions and pool resources. Then the network can gain momentum and achieve critical mass as it continues to expand, increasing its value for members.
Value is further enhanced by gathering collective intelligence, which accumulates as members share and learn from each other, facilitating discussion and experimentation.
Value also stems from developing a sense of community, with members benefiting from each other and building relationships that foster reciprocity and discretionary effort.
McInnes et al (2015) identified the following network model principles as key influential success factors:
- clinical and strategic leadership
- formal organisational structures and processes and solid systems in place that facilitates effective planning and communication
- network projects that systematically address patients’ health needs and are aligned to national strategic plans
- strong links to academic, professional, policy and clinical organisations
- a strong profile and credibility of the network to enable the establishment of strategic external relationships.
This is further supported by the work of Manns and Wasylak (2019) who state that successful networks have effective leadership, partnerships, and communication, are embedded within the health system, operate with adequate resources and, projects are strategically aligned.
The network should initially focus on building upon these core features to successfully form and deliver its initial strategic objectives. Careful consideration must be given to the overall structure, function and participation of its members.
7. Network configuration
To be successful the size of, and members involved in each network should make sense to patients, clinicians as well as provider and commissioning organisations.
It is for health communities to agree their network configuration with support and advice from their NHS England regions.
Initially we suggest a region undertakes a mapping exercise to identify the service configurations of each of the PS disciplines across their region, alongside identification of existing networks and disease pathways that the network would need to align with. This will inform the footprint of the PS network.
Initially the network should start with a similar footprint to the seven geographical regions within NHS England.
Some regions may develop more than one network depending on the size of their services, the populations they serve and the geographical size of their region. As PS networks evolve and mature this can be reviewed as to whether further subdivisions within a region would be beneficial.
Consideration must be given to how the PS network aligns and interacts with the footprints of the other diagnostic networks i.e. pathology, imaging and endoscopy. We expect strong links to be established with training providers and academies, research networks, other diagnostic and disease specific networks and pathway re-design work.
In designing the footprint, it should be recognised that discipline specific groups will form a key part of the network structure (see 8.2). These groups may need to operate at different scales depending on the existing configuration of that discipline.
For example, cardiac and respiratory groups may best operate at a system level within the overarching network whereas neurophysiology groups may come together once across the whole network.
Caution must be given to ensure that where there are existing disease networks, duplication of effort does not occur. It is envisaged that the network should enable physiologists to better inform improvement work led through the relevant disease specific networks.
Working together to address variation in apprenticeship salaries in the South West
“The South West region has a network of system lead healthcare scientists who are connected to the NHS England regional diagnostic team, system diagnostic leads, trust lead scientists and PS teams.
“This has ensured both wide geographical and PS discipline participation at a range of regional diagnostic events on workforce, training, performance, and data collection.
“One of the many common training outputs across the region and all diagnostic disciplines has been a desire to eliminate the variation in apprenticeship salaries.
“A sub-group has been formed by the diagnostic workforce steering group to develop a consensus across the region for apprenticeship salaries, to ensure individual apprentices are paid equally for the same role from trust to trust and across networks.
“The network is using its connections to gather data for PS across trusts and departments in the region.”
Teresa Robinson, Head of Physiological Sciences, South West Region.
Midlands Echocardiology Community of Interest (CoI)
“In response to the significant challenges in echocardiology recovery a more coordinated approach in was needed to provide a platform to share best practice, highlight issues, learn from successes, and build a trusted support network.”
Approach
“Having previously co-ordinated our PS services to develop a data tool we used our subject matter expert network list to identify an echo leader from each organisation to represent on the group. The group was established with initial leadership from the Regional CSO and Midlands Diagnostic Team.
“Terms of reference have been developed and the groups meets bimonthly.”
Key benefits?
- This early co-ordination helped us identify local issues with recovery.
- Sign up to deep-dive visits to support challenged organisations.
- Sharing of best practice training examples.
- Support for projects such as staff passporting, variation in payment and digital maturity.
- Attendance at the National Echo Event with representation from several providers.
- Share data and a regional position, so that there is a wider understanding of the issues.
- Raising the profile for PS and the scientific workforce
Key learning
“While the echo CoI has been an early success in establishing a co-ordinated Midlands approach to PS services, there are lessons to be learned when developing other specialties.”
- Engagement from all providers and systems is vital to ensure all communities are appropriately represented and specific local challenges correctly described.
- To ensure engagement is maintained during this difficult period of recovery investment in a structure is necessary to provide relevant clinical leadership giving the group direction credibility and links to peer networks, and project management support to maintain the group.
- We would recommend early identification of key partners to ensure they are part of the group, ideally with sponsorship from system diagnostic leaders who can support the completion of actions and be a conduit for feedback into regional board structures.
“Our positive experience and learning will guide us when setting up PS networks more broadly.”
Next steps
“We are now in the process of maturing this network to enable sustainability; this includes securing specialised clinical leadership (requested from our cardiac network, held up due to NHS England changes) and interfacing the CoI with the cardiac network to tackle shared priorities.”
Michelle Mercer, Programme Manager, Midlands.
8. Network governance and leadership
There are many forms of clinical network, with the things that a network wants to achieve having a strong bearing on how it is led and constituted.
Experience from other programmes that have sought to establish clinical and diagnostic networks, indicates that a clear governance structure together with both executive sponsorship and network leadership is essential to a network’s effective formation and functioning. All networks will need to establish and confirm their local arrangements.
While imaging networks have, by necessity of their role, needed to determine their commercial structure, the purpose and nature of PS networks is not expected to require such commercial governance arrangements.
It is therefore recommended that, in the first instance, the focus is on instigating an overarching network governance group (e.g. network board) with an underpinning structure of workstreams and associated project groups.
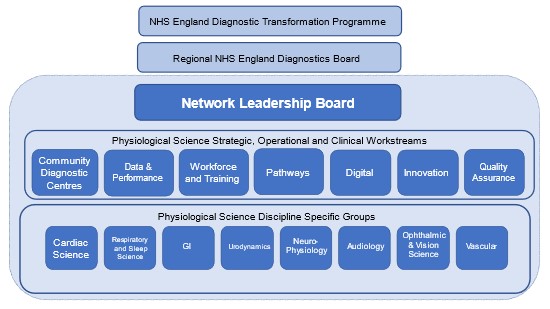
We have provided a suggested structure in appendix 1.
The other fundamental aspect of network governance arrangements will be agreements with each individual service provider about their involvement in and responsibilities to the network. This is likely to require memorandum of understanding to clearly set out respective roles and responsibilities.
Each network will need to agree reporting, escalation, and accountability arrangements in accordance with their local contexts and this will need to include alignments to system diagnostic programmes.
The central role of executive sponsorship and network leadership will be fundamental to PS networks. To manage the transformation of PS services, networks must have dedicated clinical leadership.
Operational management support is also important to work alongside clinical leads. These leaders must be given sufficient time and support to do their job effectively. Leading a network is a very different proposition to leading a PS service and must be an attractive proposition for potential network leaders.
Support and development of network leaders will be offered by NHS England. As networks develop, opportunities for network leaders to come together to share learning and access peer support will be essential.
8.1 The network workplan
Once the network is established it will be expected to develop and agree with the constituent ICBs an annual workplan which outlines the transformational goals which are aligned to national and canal priorities.
Individual workplans for key areas such as digital, workforce along with workplans for each discipline specific group will be expected to be developed by the workstream leads and agreed with the network board. In the early stages of the network, it may be the case that the network agrees to prioritise key areas.
As the network matures it is expected that there will be workplans for each priority outlined. The experience and views of people who use PS services should inform the network workplan. They should be involved in shaping the workplans through active engagement and working alongside physiologists to develop solutions that improve services.
8.2 Discipline-specific groups and operational and clinical workstreams
We expect networks to establish workstreams focussing on their highest priority areas in the first instance which cover issues related to all PS services. For example these might include:
- workforce and training
- pathways
- digital
- innovation
- quality assurance.
We would then expect discipline specific groups covering each of the eight disciplines.
The workplans for PS networks should seek to align or compliment those of existing disease specific networks and not duplicate work. Local agreement should be sought with these groups on the key areas the PS network should lead.
For example, specific to respiratory physiology, the PS network will lead work on standardising procedures and access for pulmonary function testing. A Cancer Alliance may also be doing work on the lung cancer pathway and the Targeted Lung Health Checks programme. We would expect a respiratory clinical scientist from the PS network to be involved in the work around diagnostics that support these pathways and programmes with the cancer alliance.
Another example specific to ophthalmic and vision science (OVS), the PS network OVS lead will work on standardising procedures that support diabetic eye screening, they would work with diabetes networks in their region to ensure their efforts on the Rightcare pathway and diabetes prevention programme is aligned for patients needing access to these assessments.
Working together to address variation in apprenticeship salaries in the South West
“The South West region physiological sciences network has discipline-specific groups connected to existing regional clinical networks, working together on common areas.
“For example, the regional cardiac network, cardiac science teams and NHS England diagnostic team are working together as a region on the national Echo improvement actions and have set up joint task and finish groups on DMO1, clinical triage, workforce and digital.”
Teresa Robinson, Head of Physiological Sciences, South West Region.
Deciding the footprint of discipline-specific groups will be determined by the size of the services and the most effective way to work. For example, smaller discipline groups such as neurophysiology or vascular science may be better working at a network level rather than an ICS level. There may also be the case for merging some groups with other regions such as with gastrointestinal physiology.
9. Roles and responsibilities
PS networks provide a central vehicle to transform services to enable delivery and access to the right physiological tests at the right time performed by the right person which will improve outcomes that matter to patients. However, for these networks to be successful, everyone needs to play their part. It is important that networks include the voices of people who use diagnostic services in their work.
Clinicians and professionals have responsibility for:
- actively and positively engaging in their network with the purpose of achieving quality and sustainable service provision, across whole systems of care, and reducing inequalities in care
- proving expert clinical advice taking into account views of professional bodies.
ICBs have responsibility for:
- agreeing the geographical footprint of the network
- establishing executive sponsorship for the network
- appointing, supporting, and resourcing network clinical leadership and operational management support
- agreeing the governance structure including reporting, escalation and accountability arrangements in accordance with the local context
- approving the network’s transformation plan, to reflect local and national priorities
- assuring progress on the establishment, development, and operation of the network
- ICBs, as system leaders, will play a key role in brokering positive relationships and solutions across provider organisations as needed
- ICBs also have responsibility for commissioning best practice accredited PS service provision.
Provider organisations have a responsibility for:
- agreeing their services will be fully engaged and participants within the network
- enabling senior provider representation on the network board
- engaging in improvement activities and supporting PS staff and healthcare science staff to provide expertise and input into workstreams.
NHS England (which now includes the organisation which was Health Education England) has responsibility for:
- supporting ICBs in determining the geographical boundaries of their networks
- supporting ICBs in deploying national funding (when available), for diagnostic networks, to best effect
- providing a range of additional support to health communities in enabling the effective development and operation of their PS network including:
- developing a network toolkit, which will be regularly updated and will contain sample documents, such as model job descriptions for network roles, best practice examples of governance structures, template terms of reference for network governance groups; the toolkit will also include an outline service specification for best practice ERCP services
- data insights – benchmarked data is already available via the Model Health System; this will be supplemented with further data intelligence and dashboards as part of the national PS data collection work.
- dedicated and bespoke support visits, delivered jointly with colleagues across the regions and the national specialty advisor for PS
- links to established networks that are available to provide advice and potentially some limited support for those who are starting out
- a network of networks:
- the national PS Transformation Programme will bring network leads together from across England at regular intervals enabling the sharing of best practice and peer support
- it will provide a virtual space on FutureNHS to enable networks to share learning.
- ensuring effective high quality training to the PS workforce through the work of regional education deans.
10. National support from NHS England
The National Physiological Science Transformation Programme at NHS England will provide support and guidance to assist networks with their work. This may take the form of national events to share best practice and information, an online space on NHS Futures for networks to share updates and discuss their work including the sharing of resources and toolkits to aid planning and delivery of transformation activities. This support offer is summarised in appendix 2.
Appendix 1: Proposed network design
Network leadership board
- Chair of board and SRO
- Independent patient/public member
- Regional chief scientific officer
- Network manager
- Integrated care board representation
- Network clinical lead
- Clinical lead for each discipline
- Provider organisation representation
Key engagements
- Trust lead healthcare scientists: A route to align network priorities across all organisations and ensure networks play a role in supporting improvement.
- Integrated care boards: A route to align network priorities with system priorities ad to ensure a role in supporting plans to access those priorities.
- Existing clinical networks: An opportunity to ensure diagnostic services that support different clinical specialisms ad pathways are aligned.
- Academic health science networks: An opportunity to source areas of innovation to transform care for patients and ways of working.
- Professional bodies: Engagement with key subject matter experts to deliver best practice and quality assurance.
- Trust chief operating officers: An opportunity to engage at a trust level on the delivery of physiological science services.
Appendix 2: National support offer
|
A network toolkit The toolkit will be regularly updated and will contain sample documents e.g. model job descriptions for network roles; best practice examples of governance structures; template terms of reference for network governance groups, etc. |
|
Data insights Benchmarked data is already available via the Model Health System. Further data intelligence and dashboards will be provided following the annual data collections. |
|
Leadership programme A national clinical and managerial leadership programme is likely to be needed once key posts have been appointed to. This will be commissioned in conjunction with network leads to ensure relevance and value add. |
Physiological Science Networks: National Support Offer |
Digital transformation The importance of both digital connectivity and digital innovations is well recognised. Physiological sciences will feature in a national diagnostics digital strategy. |
|
A network of networks The National Physiological Science Transformation Programme will bring network leads together, from across England, to enable the sharing of best practice, peer support and providing a safe space to problem solve common challenges. |
|
Tailored support visits Dedicated and bespoke support visits delivered jointly from colleagues across GIRFT Lead, National Specialty Advisor for Physiological Sciences and the regional Diagnostics team.
|
Publication reference: PRN00088