1. Foreword
The safeguarding of children, young people and adults who are at risk is a fundamental obligation for everyone who works in the NHS and its partner agencies. Safeguarding children and adults at risk of abuse or neglect must be kept constantly under review. The NHS takes its safeguarding responsibilities seriously – that is why we regularly review our guidance so it is as up to date as possible, based on the very best practice across the NHS and beyond. This is the 4th edition of the NHS England Safeguarding accountability and assurance framework (SAAF). We have developed this edition in partnership with experts, patients, people with lived experience and many more. It builds on its predecessor by strengthening the NHS commitment to promote the safety, protection and welfare of children, young people and adults.
2023 has seen significant changes across our healthcare system with the imbedding of integrated care systems, integrated care partnerships, provider collaboratives, primary care networks, and local maternity and neonatal systems, and new legislation which will impact how we all safeguard people and populations.
As we write this 2024 SAAF, we are also considering the implementation of the Children’s Social Care Reforms and the Working together to safeguard children 2023 revised legislation for multi-agency safeguarding arrangements.
As we move forward with new ways of working on how we safeguard, the focus will be on local level support and professional practice. This means the SAAF will iterate and need to be further developed.
I would like to take this opportunity to thank all those who have contributed to the development of the revised SAAF, and all who work with passion and professionalism to safeguard the health and wellbeing of our most at risk people.
The NHS is there for people in so many ways and in so many settings. This means that it has a unique opportunity, and a special responsibility, to help those at risk.
This edition of the SAAF is an important benchmark of how we in the NHS deliver that.
Dame Ruth May
Chief Nursing Officer, England
2. Introduction/purpose
This Safeguarding accountability and assurance framework set outs the safeguarding roles and responsibilities of all individuals working in providers of NHS-funded care settings and NHS commissioning organisations. It aims to:
- identify and clarify how relationships between health and other systems work at both strategic and operational levels to safeguard children, young people and adults under the care of the NHS at risk of abuse or neglect
- clearly set out the legal framework for safeguarding children and adults as it relates to the various NHS organisations, in order to support them in discharging their statutory duties and requirements to safeguard children and adults
- outline principles, attitudes, expectations, and ways of working that recognise safeguarding is everybody’s responsibility, and that the safety and wellbeing of those in vulnerable circumstances are at the forefront of our business
- outline the ways in which NHS England Regional and National teams support integrated care boards (ICBs) accountability and leadership at local level, fostering effective place-based partnerships
- identify clear arrangements and processes to be used to support evidence-based practice and provide assurance at all levels, including NHS England Board, that safeguarding arrangements are in place and are effective
- promote equality by ensuring that health inequalities are addressed and are at the heart of NHS England, ICB and provider values
This framework aims to provide guidance and minimum standards but should not be seen as constraining the development of effective local safeguarding practice and arrangements, in line with the underlying legal duties.
The responsibilities for safeguarding form part of the statutory functions for each organisation and its executive board must therefore ensure effective discharge within agreed baseline funding.
Throughout the development of this document, we have:
- given due regard to the need to eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it
- given regard to the need to reduce inequalities between patients in access to and the experience of and outcomes from healthcare services
3. Safeguarding context, legislation and mandatory reporting
Safeguarding is firmly embedded within the core duties and statutory responsibilities of all organisations across the NHS and health system. However, there is a distinction between providers’ responsibilities to provide safe and high-quality care, and commissioners’ responsibilities to assure themselves of the safety and effectiveness of the services they have commissioned.
Responsibilities for safeguarding are enshrined in international and national legislation. Safeguarding for both children and adults has transformed in recent years with the introduction of new legislation, creating duties and responsibilities which need to be incorporated into the widening scope of NHS safeguarding practice.
Regardless of the developing context, all health organisations are required to adhere to the following arrangements and legislation:
Legislation for all
- The Crime and Disorder Act 1998
- Female Genital Mutilation Act 2003
- Sexual Offences Act 2003
- Mental Capacity Act 2005
- UN Convention on the Rights of Persons with Disabilities 2006
- Mental Health Act 2007
- Children and Families Act 2014
- Modern Slavery Act 2015
- Serious Crime Act 2015
- Mental Capacity (Amendment) Act 2019
- NHS Constitution and Values (updated Jan 2021)
- Domestic Abuse Act 2021
- Serious Violence Duty 2023
- Prevent Duty 2023
Safeguarding children and young people
- United Nations Convention on the Rights of the Child 1989
- Children Act 1989 and Children Act 2004
- Promoting the Health of Looked After Children Statutory Guidance 2015
- Children and Social Work Act 2017
- Working Together to Safeguarding Children 2023
- Children Social Care Reforms
- Safeguarding Children and Young People: Roles and Competencies for Healthcare Staff 2019
- Looked After Children: Roles and Competencies of healthcare staff 2020
Safeguarding adults
- European Convention on Human Rights
- The Care Act 2014
- Care and Support Statutory Guidance- Section 14 Safeguarding
- Adult Safeguarding: Roles and Competencies for Health Care Staff 2018
It remains the responsibility of every NHS funded organisation, and each individual healthcare professional working in the NHS, to ensure that the principles and duties of safeguarding children and adults are holistically, consistently and conscientiously applied. The wellbeing of those children and adults is at the heart of what we do.
Local authorities have a general duty under section 17 of the Children Act 1989 to safeguard and promote the welfare of children within their area who are in need.
Section 47 of the Children Act 1989 creates a specific duty for local authorities to make enquiries to determine whether a child is or is likely to suffer significant harm, and what action to take to safeguard and promote a child’s welfare. NHS bodies have a duty to assist the local authority with those enquiries, where reasonable to do so.
In supporting local authorities to safeguard children in their local area, section 11 of the Children Act 2004 creates an additional statutory duty for NHS bodies to ensure that they discharge their functions having regard to the need to safeguard and promote the welfare of children. This includes providers commissioned by NHS bodies to deliver services on its behalf.
It is important to recognise that healthcare has a statutory assurance role for child safeguarding which is not the case for adult safeguarding.
Local authorities have a specific duty under section 42 of the Care Act 2014 to make, or cause to be made, enquiries to identify whether an adult in their area is experiencing, or at risk of, abuse or neglect to determine what action should be taken and by whom to protect the individual.
The local authority also has specific responsibilities under the Mental Capacity Act 2005 in the day-to-day operation of the Deprivation of Liberty Safeguards. Section 6 of the Care Act 2014 places a specific duty on NHS bodies to co-operate with the local authority in its enquiries.
That said, the NHS takes a leading role in the following safeguarding programmes which predominately impact adults: female genital mutilation (FGM), domestic abuse, prevent, domestic homicide reviews, modern slavery and human trafficking (MSHT).
Every NHS-funded organisation needs to ensure sufficient safeguarding leadership capacity is in place for them to fulfil their statutory duties. They should regularly review their arrangements to assure themselves that they are working effectively to the Safeguarding Commissioning Assurance Toolkit (Safeguarding-CAT).
Organisations need to co-operate and work together within new demographic footprints to seek common solutions to the changing context of safeguarding, and developing a structural landscape needed to deliver the NHS Operating Plan and NHS Operating Framework.
4. Roles of national, regional and local safeguarding
The national safeguarding team and Regional Safeguarding Leads (RSLs), known as NHS Safeguarding, will work to improve safeguarding practices across the NHS to produce positive health outcomes for victims and survivors of abuse and exploitation, within all communities.
Each NHS England region will continue to operate a bespoke safeguarding assurance function and structure which aligns to the NHS England operating framework.
The regions will review safeguarding governance processes for integrated care systems (ICSs) and partnerships. This will allow each region to support improvement through their safeguarding commissioning assurance governance processes, whilst ensuring the following key objectives are met (see below):
- the implementation of effective safeguarding assurance arrangements via schedule 32 of the NHS Standard Contract, our SAAF, the Safeguarding-CAT and the NHS Safeguarding Case Review Tracker. This will include:
- Child Protection-Information Sharing (CP-IS) systems
- NHS contribution to local safeguarding partnerships
- Prevent
- MSHT
- FGM
- domestic abuse guidance
- serious violence duty for ICBs
- Liberty Protection Safeguards guidance (when launched)
- ensure direct commissioning, specialised commissioning and health in the justice systems are also meeting SAAF requirements at national, regional and local levels
- learn lessons from cases where children or adults die or are seriously harmed under the care of the NHS which is party to any statutory death reviews with safeguarding recommendations, to ensure the learning is effectively disseminated across the NHS
- all parties within NHS Safeguarding will provide safeguarding advice, role modelling leadership across the NHS underpinned by contemporaneous evidence-based methodologies such as contextual safeguarding; trauma informed practice and strength-based approaches to safeguarding interventions
4.1 The regional safeguarding team
The regional safeguarding team will underpin the NHS England operating framework via their regional safeguarding work plans, as below:
|
Operating framework for NHS England regions |
How will it be delivered? Workplan/delivery plan functions |
|
Act as the main voice to ICSs and the primary interaction between NHS England and systems |
Liaison with the ICBs/ICSs via: · chief nurses/deputies · designated professionals · named practitioners · regional safeguarding maternity/midwifery leads · regional counter terrorism group · violence reduction units · community safety partnerships |
|
Translate national strategy and policy to fit local circumstances, ensuring local health inequalities and priorities are addressed |
Provide support, leadership and guidance on the development of NHS Safeguarding policies and procedures for safeguarding |
|
Agree ‘local strategic priorities’ with individual ICSs |
Use and monitor the allocated funding to develop safeguarding practice and expertise within the region, in line with nationally agreed priorities |
|
Provide oversight to ICBs and agree oversight arrangements for place-based systems and organisations |
Be the conduit for the evolving assurance of ICBs via: · the NHS Safeguarding heat maps · the multi-agency safeguarding arrangements · child death overview process · joint targeted area inspections · thematic reports from the National Child Safeguarding Review Panel · safeguarding adults boards (SABs) · chair networks |
|
Develop leadership within ICBs and providers |
Establish regional safeguarding networks, clinical groups and communities of practice as agreed within the region Ensure all NHS providers and system leaders are engaged in arrangements for safeguarding babies, children, young people, and adults |
|
Within national frameworks, determine the ‘how’ of delivery to achieve outcomes and expectations to reflect local populations, workforce, service structures and digital capabilities |
Provide support to safeguarding improvements in the integrated care partnership (ICP) space Delivered via regional safeguarding governance architecture, relationships and one-to-ones and communications |
|
Develop mechanisms for systematically collating and sharing good practice and lessons learnt |
Adopt a lead RSL function with the NHS Safeguarding statutory functions providing leadership, support and guidance to the National Safeguarding team Support systems in making improvements via the application of learning lessons from statutory reviews |
|
Manage regional level relationships including regional government |
Provide oversight and safeguarding intensive support as part of any ICB or provider being in the Recovery Support Programme, where this is identified as a key risk Delivered as directed via regional directors, regional chief nursing officers and system quality review groups (see regional safeguarding and quality governance architecture) |
|
Provide support to ICSs to enable delivery |
Collaborate with ICBs to escalate significant risks and issues which may have system-wide impact and require national resolution, to include learning from incidents such as: · child safeguarding practice reviews · domestic homicide reviews · safeguarding adult reviews · other local and regional safeguarding reviews |
4.2 NHS national safeguarding team
The national safeguarding team will underpin the NHS England Operating Framework via our NHS Safeguarding workplan, as below:
|
Operational framework |
How will it be achieved |
|
Sets direction |
Via contract schedule 32 and SAAF |
|
Allocates resources |
Via budgeting, commissioning and ICB offer, and via regional management teams |
|
Ensures accountability through the National Safeguarding Steering Group (NSSG), the forum that provides assurance to the Executive Quality Group, quality committees and the NHS England Board |
Via SAAF, ICB self-assessment heat maps and Safeguarding-CAT using the NHS Safeguarding Integrated Data Dashboard NSSG leads the assurance of the NHS safeguarding system and offers strategic leadership for safeguarding and quality improvement across NHS England and the health economy |
|
Supports and develops people |
Via safeguarding clinical networks, learning together events, rapid reads and FutureNHS |
|
Mobilises expert networks |
Via safeguarding clinical networks and clinical reference groups |
|
Bring together expert knowledge to support service improvement |
Via national safeguarding clinical networks and the NHS Safeguarding reflective practice framework |
|
Support delivery of improved outcomes and provide benchmarks for services |
Via the NHS Safeguarding Integrated Data Dashboard |
|
Enable the spread of best practice |
Via NHS Safeguarding rapid reads and our NHS Safeguarding Strategic Community of Practice |
|
Manage relationships across national and professional bodies |
Via liaising with XGov (regarding impact assessments) and royal colleges (standards and competencies) |
|
Enable and support the development of systems and ICBs |
Via the NHS Safeguarding Strategic Community of Practice |
|
Enables improvement |
Via safeguarding clinical networks and learning together events |
|
Delivers services |
Via our NHS Safeguarding workplan |
|
Drives transformation |
Via lead RSL matrix, RSLs meetings, National Safeguarding Collaborative, NHS Safeguarding reflective practice framework and the regional chief nurses and regional directors |
4.3 The ICB safeguarding system
Following several years of locally led development, and based on the recommendations of NHS England, the government and the Department of Health and Social Care (DHSC) has put ICBs and ICPs on a statutory footing. DHSC are responsible for guidance regarding ICPs.
The SAAF governance processes will replicate ICB guidance and the ICB executive chief nurse will be accountable for the statutory commissioning assurance functions of NHS Safeguarding as per the agreed timelines with the regional chief nurse. These programmes will include:
- CP-IS
- Child death overview process
- FGM
- Prevent
- Working together to safeguard children
- MSHT
- Domestic abuse
- duty to collaborate to prevent serious violence
- mandatory reports of child sexual abuse
The core principles of the executive accountability, including protecting the welfare and paramountcy of every child, will be sustained via the NHS SAAF.
While place directors can delegate responsibility for implementation of safeguarding practice across all ages, executive accountability for safeguarding cannot be delegated. The ICB will also have accountability for prevention and strategic workforce planning.
The ICB executive chief nurse is likely to oversee place-based partnership structures of clinical leads to collaborate with local safeguarding partnerships and SABs. These partnerships need to be preventative:
- violence reduction units
- community safety partnerships
- lived experience victim and survivor advocacy services
- sustainable peer support community assets
- police and crime commissioners
- education leads
We recommend that ICB safeguarding workforce plans should take into account the children, looked after children and adults safeguarding competencies and standards:
- Safeguarding Children and Young People: Roles and Competencies for Healthcare Staff | Royal College of Nursing (rcn.org.uk)
- Looked After Children: Roles and Competencies of Healthcare Staff | Royal College of Nursing (rcn.org.uk)
- Adult Safeguarding: Roles and Competencies for Health Care Staff | Royal College of Nursing (rcn.org.uk)
ICBs are also required to act as statutory safeguarding partners (section 16E of the Children Act 2004), working together with local authorities and the police to ensure that their functions are exercised for the purpose of safeguarding and promoting the welfare of children in the area.
This requires an annual report to be prepared and published, setting out what arrangements the safeguarding partners have made and how effective they have been.
4.3.1 Section 11 audits
Section 11 of the Children Act 2004 creates a specific statutory duty for NHS bodies to ensure that they discharge their functions having regard to the need to safeguard and promote the welfare of children. This includes providers commissioned by NHS bodies to deliver services on its behalf.
To monitor this, it is necessary for regular audits to be completed to ensure compliance. NHS England has replaced the variation of local section 11 audits from local authorities with our Safeguarding-CAT, the SAAF and the NHS Standard Contract Schedule 32. ICBs should collaborate with their local authorities to understand the specific local section 11 audit.
4.4 NHS, health and care providers
All health providers, including provider collaboratives, are required under statute and regulation to have effective arrangements in place to safeguard and promote the welfare of children and adults at risk of harm and abuse in every service that they deliver.
Providers must demonstrate that safeguarding is embedded at every level in their organisation, with effective governance processes evident. Providers must assure themselves, the regulators, and their commissioners that safeguarding arrangements are robust and are working. These arrangements include:
- the contractual requirements as laid out in Schedule 32 of the NHS Standard Contract
- identification of a named nurse, named doctor and named midwife (if the organisation provides maternity services) for safeguarding children
- identification of a named nurse and named doctor for children in care
- identification of a named lead for adult safeguarding and a Mental Capacity Act (MCA) lead – this role should include the management of adult safeguarding allegations against staff
- this could be a named professional from any relevant professional background
- safe recruitment practices and arrangements for dealing with allegations against staff
- provision of an executive lead for safeguarding children, adults at risk and Prevent
- an annual report for safeguarding children, adults and children in care to be submitted to the trust board
- a suite of safeguarding policies and procedures that support local multi-agency safeguarding procedures
- effective training of all staff commensurate with their role and in accordance with the intercollegiate safeguarding competencies
- safeguarding must be included in induction programmes for all staff and volunteers
- providing effective safeguarding supervision arrangements for staff, commensurate to their role and function (including for named professionals)
- developing an organisational culture where all staff are aware of their personal responsibilities for safeguarding and information sharing
- developing and promoting a learning culture to ensure continuous improvement
- policies, arrangements and records, to ensure consent to care and treatment is obtained in line with legislation and guidance
It is worth noting that provider accountabilities and responsibilities need to be considered in conjunction with professional accountabilities to the professional regulators.
5. Disclosure and barring service
The Disclosure and Barring Service (DBS) is responsible for administering the government’s statutory scheme to help employers make safer recruitment decisions.
There are different levels of checks that disclose a range of different information contained within the Police National Computer and local police force information.
To help decide which level of check is needed for different roles, the DBS provide guidance specifically for NHS roles: Role eligibility for DBS Checks | NHS Employers
About us – Disclosure and Barring Service – GOV.UK (www.gov.uk)
6. Fit and proper persons tests
There are 2 ‘fit and proper’ persons tests that are separated within the health and social care regulations:
- Regulation 19 – which outlines the requirements for the fit and proper persons test for persons employed
- Regulation 5 – which outlines the requirements for directors to be fit and proper persons
7. Duty of candour
Safeguarding requires openness, advocacy, transparency and trust. The publication of the Francis Inquiry report recommended that a statutory duty should be introduced for healthcare providers to be open with people when things go wrong; this duty is regulated by the Care Quality Commission (CQC).
The duty of candour is triggered by a “notifiable safety incident”, for any “unintended or unexpected incident that has occurred in respect of all service users during the provision of a regulated activity”.
A safeguarding incident might be because of a clinical procedure or practice that could have contributed to death, physical or psychological harm.
8. Information sharing
Robust information-sharing is at the heart of safe and effective safeguarding practice.
Information sharing is covered by legislation, principally the General Data Protection Act 2018 (GDPR) and the Data Protection Act 2018. This legislation introduces new elements to the data protection regime, superseding the Data Protection Act 1998.
Practitioners must have due regard to the relevant data protection principles which allow them to share personal information. The GDPR and Data Protection Act 2018 place greater significance on organisations being transparent and accountable in their use of data.
All organisations handling personal data need to have comprehensive and proportionate arrangements for collecting, storing, and sharing information. The GDPR and Data Protection Act 2018 do not prevent or limit the sharing of information for the purposes of keeping children, young people and adults safe.
There are explicit data sharing protocols for children which states that data protection law allows you to share information when required to identify children at risk of harm and to safeguard them from harm.
Data protection law does not prevent organisations from doing this. It simply helps organisations share information in a fair, proportionate and lawful way. For more information, please see a 10-step guide to sharing information to safeguard children | ICO.
9. Statutory and mandatory reviews
All NHS agencies and organisations that are asked to participate in a statutory review must do so. The input and involvement required will be discussed and agreed in the terms of reference for the review.
Broadly, this will involve evidence of contribution, meeting regularly with colleagues and attending panels or review group meetings throughout the investigative phase.
Statutory reviews are processes for learning and improvement and all health providers, including GPs, are required to provide and share information relevant to any statutory review process.
ICBs, via the designated professionals, may support panel chairs where learning and improvement has wider implications and needs co-ordinated national action, and/or where there are obstacles to full NHS participation that require a range of relationship, contractual and professional influences.
9.1 Rapid reviews
As per Working together to safeguard children 2023, the purpose of rapid reviews for serious child safeguarding cases, at both local and national level is to identify improvements to be made to safeguard and promote the welfare of children.
Serious child safeguarding cases are those in which abuse, or neglect of a child is known or suspected and the child has died or been seriously harmed.
The safeguarding partners should promptly undertake a rapid review of the case in line with any guidance published by the Child Safeguarding Practice Review Panel. The aim of this rapid review is to enable safeguarding partners to:
- gather the facts about the case, as far as they can be established at the time
- discuss whether there is any immediate action needed to ensure children’s safety and share any learning appropriately
- consider the potential for identifying improvements to safeguard and promote the welfare of children
- decide what steps they should take next, including whether or not to undertake a child safeguarding practice review
9.2 Child safeguarding practice review
The responsibility for how the system learns the lessons from serious child safeguarding incidents lies at a national level with the Child Safeguarding Practice Review Panel and at local level with the local safeguarding children’s partnerships.
A child safeguarding practice review should be considered for serious child safeguarding cases where abuse or neglect of a child is known or suspected, and a child has died or been seriously harmed. This may include cases where a child has caused serious harm to someone else.
9.3 Child death review (CDR)
The Children Act 2004 requires ICBs and local authorities (child death review partners) to make local arrangements to undertake statutory CDR processes. The CDR process relies on inter-agency co-operation and information sharing.
These arrangements should result in the establishment of a child death overview panel, or equivalent, to review the deaths of all children (under the age of 18 years), regardless of cause of death, normally resident in the relevant local authority area; and if they consider it appropriate, the deaths in that area of non-resident children.
The review should then be carried out by a child death overview panel, on behalf of CDR partners, and should be conducted in accordance with Child Death Review: Statutory and Operational Guidance 2018 and Working Together to Safeguard Children 2023.
9.4 Learning disability mortality review (LeDeR) programme
LeDeR is a service improvement programme which aims to improve care, reduce health inequalities, and prevent premature mortality of people with a learning disability and autistic people by reviewing information about the health and social care support people received.
Everyone with a learning disability aged 4 and above who dies, and every adult (aged 18 and over) with a diagnosis of autism is eligible for a LeDeR review. It aims to make improvements in the quality of health and social care for people with learning disabilities and autism, and to reduce premature deaths in this population.
It does this by:
- delivering local service improvement, learning from LeDeR reviews about good quality care and areas requiring improvement
- driving local service improvements based on themes emerging from LeDeR reviews at a regional and national level
- influencing national service improvements via actions that respond to themes commonly arising from analysis of LeDeR reviews
Local ICBs are responsible for ensuring that LeDeR reviews are completed for their local area and also, and very importantly, that actions are implemented to improve the quality of services for people with a learning disability and autistic people to reduce health inequalities and premature mortality.
Further to LeDeR, LeDeR reviews are done for people with learning disabilities over the age of 18 years.
Deaths relating to under 18 years old are now to be reported under Child Death Review.
- Learning from lives and deaths – People with a learning disability and autistic people (LeDeR) policy 2021
- LeDer Learning from Lives and Deaths
9.5 Domestic homicide reviews (DHRs)
A DHR convened by the local community safety partnership is a multi-agency review of the circumstances in which the death of a person aged 16 or over has, or appears to have, resulted from violence, abuse or neglect by a person to whom they were related or with whom they were, or had been, in an intimate personal relationship, or a member of the same household as themselves.
From April 2024, ICBs will be accountable to ensure lessons learned from any DHR are cascaded across the health system, and any commissioning/contractual sanctions with specific providers are implemented and learning is imbedded.
9.6 Safeguarding adults reviews (SARs)
SARs are required under the Care Act and convened by an SAB when an adult has died from, or experienced, serious abuse or neglect, and there is reasonable cause for concern about how agencies and service providers worked together to safeguard the person, as per the Safeguarding adults review quality markers.
From April 2024, ICBs will be accountable to ensure lessons learned from any SAR are cascaded across the health system and any commissioning/contractual sanctions with specific providers are implemented, as part of local inter-agency safeguarding agreements.
9.7 Other reviews
Mental health homicide reviews, multi-agency public protection arrangements and learning disability mortality reviews are carried out under separate arrangements but may, depending upon the circumstances, need to link to a safeguarding statutory review.
Such reviews may run parallel to local authority safeguarding inquiries and serious incident investigations.
10. Parallel investigations
At times, the safeguarding of children and/or adults in a health setting may feature in a wider multi-agency statutory review commissioned for other purposes: for example, a DHR or a mental health investigation. In these circumstances, a separate safeguarding practice review may be deemed appropriate.
Therefore, NHS organisations should be prepared to share information and co-operate with the parallel practice review panel. Duplication of effort should be avoided where possible with each review informing the parallel process.
System leaders need to be aware of the new patient safety incident response framework (also known as PSIRF) which may also be activated due to other incident management processes.
11. Allegations against staff involving child abuse – local authority designated officer (LADO)
Working together to safeguard children 2023 stipulates that information must be shared with the local authority designated officer (LADO) where it is considered that a member of health staff poses a risk to children or might have committed a criminal offence against one or more children.
12. Allegations against staff involving abuse or neglect – adults
The Care Act (2014) defines people in positions of trust (PiPoT) as “people who work in paid or unpaid capacity, including celebrities and people undertaking charitable duties with adults with care and support needs” (see Statutory Guidance 14.120 to 14.132).
It is a requirement of the Care Act 2014 Statutory Guidance that SABs should establish and agree a framework and process for any organisation to respond to allegations against “anyone who works, (in either a paid or an unpaid capacity) with adults with care and support needs”.
Where there is an allegation that a member of staff in an ICB or primary care services has abused or neglected an adult in their personal life, the designated professional for safeguarding adults in the ICB should be informed and HR due processes followed.
13. The regulation of safeguarding
CQC regulates compliance of the SAAF across healthcare – CQC safeguarding statement:
- working with other inspectorates such as Ofsted, HMI Probation, HMI Constabulary, HMI Prisons, and NHS England to review how health, education, police, probation and prison services work in partnership to help and protect people from harm
- working with local partners such as local Healthwatch, local authorities, the police and ICBs to share information about safeguarding people using services
Professional registrants must refer to their professional regulatory body:
- Safeguarding statement – GMC (gmc-uk.org)
- Our safeguarding policy – The Nursing and Midwifery Council (nmc.org.uk)
- Professional standards authority safeguarding policy
- Guidance on child protection and vulnerable adults (gdc-uk.org)
- other professional regulators will have safeguarding policies imbedded into their membership webpage
14. The safeguarding governance across the NHS pathway of the National Safeguarding Steering Group (NSSG)
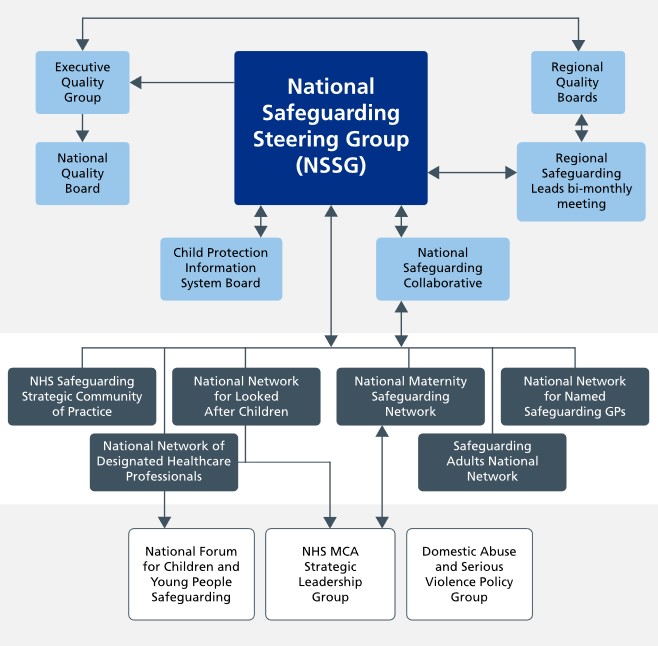
NHS England’s safeguarding role is discharged through the Chief Nursing Officer (CNO) for England, who has a national safeguarding leadership role. The CNO is the lead board executive director for safeguarding and has several forums through which assurance and oversight is sought.
The system-wide NSSG co-ordinates these forums and gains assurance on behalf of the CNO. These groups and the governance arrangements are set out below.
The NSSG is chaired by the Deputy Chief Nursing Officer for England – Professional and System Leadership, for NHS England and leads the assurance of the NHS safeguarding system and offers strategic leadership for safeguarding and quality improvement across NHS England and the health economy
NSSG achieves this through working with a range of temporary and permanent subgroups and clinical reference groups that focus on key issues using a risk-based approach.
Membership of the NSSG includes representation from the national safeguarding team, regional safeguarding system leadership, internal directorates, national safeguarding clinical networks and safeguarding partners such as the royal colleges and Office of Health Improvement and Disparities.
Figure 1: Safeguarding governance into and out of the National Safeguarding Steering Board
Click here to read a detailed description of figure 1
The image shows a flowchart related to the National Safeguarding Steering Group (NSSG).
Here is a description of the flowchart:
At the top centre is a blue box labelled “National Safeguarding Steering Group (NSSG)”.
Directly above the National Safeguarding Steering Group box, there are two boxes:
On the left “Executive Quality Group”
On the right “Regional Quality Boards”
Below the National Safeguarding Steering Group box, there are four boxes:
On the left: “Child Protection Information System Board”
Second from the left: “National Safeguarding Adults Board”
Second from the right: “National Maternity Safeguarding Network”
On the right: “National Network for Named Safeguarding GPs”
Below these four boxes, there are additional boxes connected to them:
From “Child Protection Information System Board”: “NHS Safeguarding Strategic Community of Practice”
From “National Safeguarding Adults Board”: National Network for Looked After Children” “
From “National Maternity Safeguarding Network”: “National Network of Designated Healthcare Professionals”
From “National Network for Named Safeguarding GPs”: “Safeguarding Adults National Network”
At the bottom, there are three boxes connected to the boxes above.
On the left “National Forum for Children and Young People Safeguarding”
In the middle “NHS MCA Strategic Leadership Group”
On the right “Domestic Abuse and Serious Violence Policy Group”
The NSSG has been reporting to the Executive Quality Group since August 2023 using the NHS overseeing quality matrix below, from the NHS England ICB Quality Reporting 2023. This supports oversight and alignment of NHS Safeguarding through NHS England’s Quality Governance framework.
14.1 NHS Overseeing quality matrix
As an organisation, NHS England must work with regulators to ensure there is a coherent system of quality oversight and regulation in place; one that is focused on improvement and enables warning signs, risks and concerns to be mitigated and managed as close to the point of care as possible.
NHS England has formal accountability for oversight of ICBs and NHS providers and will work with ICBs to support system management of quality.
14.1.1 Quality management system (NQB guidance)
|
Routine: · ICB/place with providers. · Within providers and across pathways. · Routine quality monitoring, assurance and improvement. · Identifying early warning signs. · Responding to risks. Enhanced: · ICB/place with NHS England regional support as required. · Responding to system concerns and risks. · Regional support to improve quality and outcomes. Intensive: · NHS England and other regulators, with ICB. · Responding to very serious/complex quality concerns and risks. · Either reduce risks of or address actual quality failings. · Typically regionally led. |
14.1.2 Tools and approaches
|
NHS oversight framework: · The NHS oversight framework sets out how NHS England will identify where ICBs and/or NHS providers may benefit from, or require, support. · The framework provides an objective basis for decisions about when and how NHS England will intervene. · Quality of care is a key area for consideration when NHS England is making these decisions. NHS provider licence (for NHS trusts and hard to replace independent providers): · Incorporates quality governance requirements. Intensive support and NHS Long Term Plan programme support: · For most challenged providers, ICBs and hard to replace independent providers, including quality-related subject matter expertise (for example, quality governance, pharmacy and medicines). Enforcement action: · Last resort. |
14.1.3 Shared working principles
|
· Proactively monitor and follow up on early warning signs and feedback from staff and people drawing on services. · Establish ways of working, responsibilities and accountability across tools and frameworks – must be coherence across with clear understanding of responsibilities, thresholds for escalation, escalation routes and need for joint working. · Share intelligence in a timely way about the quality of care across all system partners, particularly feedback from staff and people drawing on services. · Agree responsibilities, accountabilities and governance routes. Accountability framework can be used. · Co-design and co-ordinate improvement support. Ensure inclusion of quality measures in improvement plans and a supportive conversation wherever possible. · Monitor and mitigate future risks. Share agreement on most appropriate forum used to monitor implementation of actions (for example, Quality Improvement Group or oversight group). Engage relevant colleagues in ongoing discussions. |
14. 2 The national safeguarding networks
14.2.1 National Network of Designated Healthcare Professionals (NNDHP)
The system advisory group for all matters child safeguarding.
Designated professionals are experts and strategic leaders for safeguarding. As such they are a vital source of safeguarding advice and expertise for all relevant agencies and other organisations, particularly:
- health commissioners
- ICBs
- the local authority
- NHS England
- other health professionals in provider organisations
- system quality groups
- regulators
- the safeguarding children partnership arrangements
- corporate parenting boards
- SABs
- community safety partnerships
- the health and wellbeing board
The designated professional for children in care will offer support and advice to the board member responsible for adult and children safeguarding and ensure the regular provision of training to staff and board of the ICB.
14.2.2 Safeguarding Adults National Network (SANN)
The inclusive community of practice group for all matters adult safeguarding.
The adult safeguarding designated professional will:
- offer support and advice to the board member responsible for adult safeguarding and ensure the regular provision of training to staff and board of the ICB
- provide a health advisory role to the local SAB via the ICB member (through attendance, advice and support in connection with SAB functions)
- take a lead for health in working with the SAB on safeguarding adult reviews, and to take forward any learning for the health economy
14.2.3 National Maternity Safeguarding Network
The safeguarding group for anyone linked to perinatal and maternity safeguarding.
14.2.4 National Network of Named GPs
The forum of named safeguarding GPs.
A role description specific to named GPs is found within the RCGP/NSPCC Safeguarding Children Toolkit 2014 and a competency framework is set out in Guidance and Competences for the Provision of Services Using Practitioners with Special Interests (PwSIs) Safeguarding Children and Young People.
ICBs must have access to the services of a named GP for adult safeguarding to ensure that primary care services can meet their obligations to both adults and children and support contextualised safeguarding. The Adult Safeguarding: Roles and Competencies for Health Care Staff sets out the competencies for the named GP.
14.2.5 National Safeguarding Collaborative
The forum of all safeguarding leaders whose members care for NHS patients.
14.2.6 NHS Safeguarding Strategic Community of Practice
The Strategic Community of Practice has been established to help ICBs understand and implement their executive accountabilities for the SAAF programmes.
15. Conclusion
The safeguarding of children, young people and adults who are at risk is a fundamental obligation for everyone who works in the NHS and its partner agencies. Safeguarding children and adults at risk of abuse or neglect must be kept constantly under review. While there are some similarities, the safeguarding of children and adults are distinct and separate entities which need different approaches. Each person requires a unique safeguarding approach by the professional based on their circumstances and needs.
Fundamentally, every NHS organisation, and every individual healthcare professional working in the NHS, must ensure that the principles and duties of safeguarding adults and children are holistically, consistently and conscientiously applied: the needs of these at risk citizens and communities must be at the heart of everything the NHS does.
Partnership working is essential, and it is vital that local practitioners continue to develop relationships and work closely with colleagues across their local safeguarding system. This will help to develop ways of working that are collaborative, encourage constructive challenge, and enable learning in a sustainable and co-ordinated way.
The NHS is continuing to look at how it can improve safeguarding for all, including for those most at risk, such as pregnant women, those at risk of domestic abuse and many others and in this we are committed to learning from best practice and experiences from the across the NHS.
Publication reference: PRN01172