Introduction
This report expands on the research into how we can learn from patients’ experiences relating to patient safety. It is recommended you read our summary report prior to reading this full report.
NHS stakeholder views
This section sets out what NHS staff told us in user research sessions.
Pain points, challenges and benefits of increasing collection of patient perspectives
Summary
Pain points
- Patient safety feedback is not all kept in one place.
- Complaints often include information about things that should have been recorded as safety events.
- Patients do not know where to go to record safety events.
Benefits
- Richer data with information on new topics.
- Authentic account direct from the patient.
- More engagement with the patient, in turn reducing complaints.
- Systemic or cultural issues could be identified.
Pain points
NHS staff
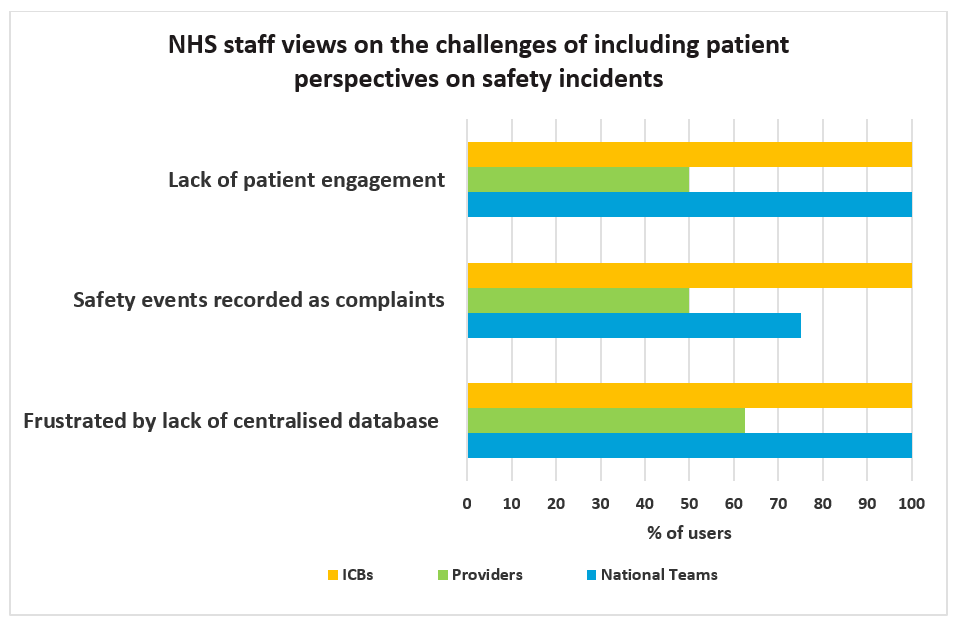
These were the top 3 difficulties identified by the NHS staff we spoke to:
- Lack of engagement – patients are not actively engaged with when carrying out investigations.
- Complaint vs safety event – patients identify something going wrong rather than a distinction between safety and a complaint, leading to safety events being recorded as complaints.
- No centralised database – data comes in from several different routes and is not easily accessible in one place for analysis.
National team
Lack of incident recordings from primary care: In primary care settings, investigations often only occur once a patient makes a complaint. If the patient does not raise a complaint, then there is no record of the event. This means that only 1% of incident data comes from primary care providers. For incidents that are escalated, patients are not involved in the process, and they do not see any of the findings. This is likely to lead to further complaints and escalation.
Complaints are analysed separately: There is no consistency in the way in which complaints are captured. The data produced through the complaints process does not have to be captured in any form of output, and how trusts use this data is down to their capacity and resources. There is no defined process to identify learning from complaints within NHS England. Furthermore, stakeholders do not engage with data produced through the complaints process. This is problematic as information provided through the complaint’s avenue may contain safety incident data. Complaints and safety data are separate and there is no requirement for the two teams to communicate with one another.
Recording mechanisms are underutilised by patients: Patients do not know about available patient safety reporting services, leading to their underutilisation. Most of the reports that national teams receive have been written by clinicians rather than patients, leading to the loss of vital details. Patients’ mental models is also of something going wrong rather than there being a distinction between a safety event and a complaint specifically.
Data quality is affected by additional information: Findings are disseminated across providers but with no feedback loop between departments, which makes it difficult to receive all relevant information needed to carry out analysis. Furthermore, there may be excess information around the data and clinicians use different terminology, which may be difficult to interpret. Healthcare professionals may also copy and paste medical records into the incident recordings, which does not add value and obscures what they are reporting. This issue is exacerbated as many of the questions currently asked are not helpful to national teams.
Lack of capacity to analyse all feedback: National teams do not have capacity to do exploratory research and a lot of the analysis is reactive rather than proactive, leading them to feel as though they are ‘on the backfoot’. There is a lack of a feedback loop between departments makes it difficult to receive all relevant information.
The people we interviewed who work in national teams said:
- “A lot of stuff that we see that comes through as a complaint looks like it should have been reported as an incident but hasn’t been.”
- “In some trusts they [patient safety and complaints teams] will have worked very, very separately as two different teams.”
Providers
Complaints contain clinical aspects: Incidents may be missed and only identified when a complaint that contains clinical aspects has been raised. This is problematic as patients often use the complaints process to record safety events as other avenues are not as clearly signposted. Complaints may also contain a large amount of additional information, and this can make identifying and following up on clinical aspects difficult. Frustration surrounding the complaints process may also lead to additional complaints being raised by patients as they seek results.
Data is disseminated across the service: Providers do not get sight of all feedback data as it is not all recorded in one place. In particular, Friends and Family Test (FFT) data is kept separate and not integrated with other forms of feedback. This is problematic as the data from the FFT may indicate a problem that is developing and may be overlooked as a result. Direct feedback provided by matrons is also not tracked and therefore cannot be analysed. Finally, PALS feedback is also not fed into one place as providers have different systems for accessing this feedback.
Under resourcing: Providers are under resourced and therefore they batch low to no harm incidents for analysis by theme. This may potentially lead to important information being missed and not analysed in great depth.
Data quality is impacted: Data may not be validated before it is uploaded into the LFPSE, raising concerns about the quality of the information provided. Furthermore, a lot of non-clinical information can be included in complaints, and this is not relevant to safety learning. Staff also fill out complaints on the patient’s behalf which can lead to the authentic account of the patient being lost. This may lead to incidents being graded incorrectly leading to them being incorrectly analysed. There are also fears surrounding the duplication of data when patients move wards or hospitals.
The people we interviewed who work in providers said:
- “I mean we’re in a blame culture, aren’t we at the moment and the people are very unhappy.”
- “We are finding that people are copying and pasting from medical records, so they are pages long.”
Key challenges
Overall, the key challenges identified by staff were:
- Resources constrain the ability of teams to review high quantities of data as teams reviewing incidents and recordings are often small. By increasing the number of recordings, this may result in potential areas of interest and learning opportunities being overlooked.
- There are concerns surrounding the volume of information provided by patients as they may provide information that potentially does not benefit learning. This can lead to issues being missed as they get lost within the details.
- There is potential for duplicated data as patients may record events that have already been noted by clinicians and therefore risks the frequency of events being over exaggerated.
- There are constraints on sharing data between organisations and departments, which can mean that vital information is missed, and we do not receive the full picture from the data provided.
- Transparency – Who is going to oversee this data and where will the responsibility lie for reviewing, managing and responding to it? There would need to be guidelines on which types of information should go to trusts and which should be used for national learning.
- Providers are keen to rectify issues before an official incident is recorded. Some issues that could be used for learning purposes will be rectified informally and not noted.
- Organisations are concerned that having a good recording culture will reflect poorly on them, as they may have unusually high incident rates. Trusts still tend to compare themselves based on number of incidents reported, not the reporting culture that a higher rate may reflect.
Potential benefits
NHS staff
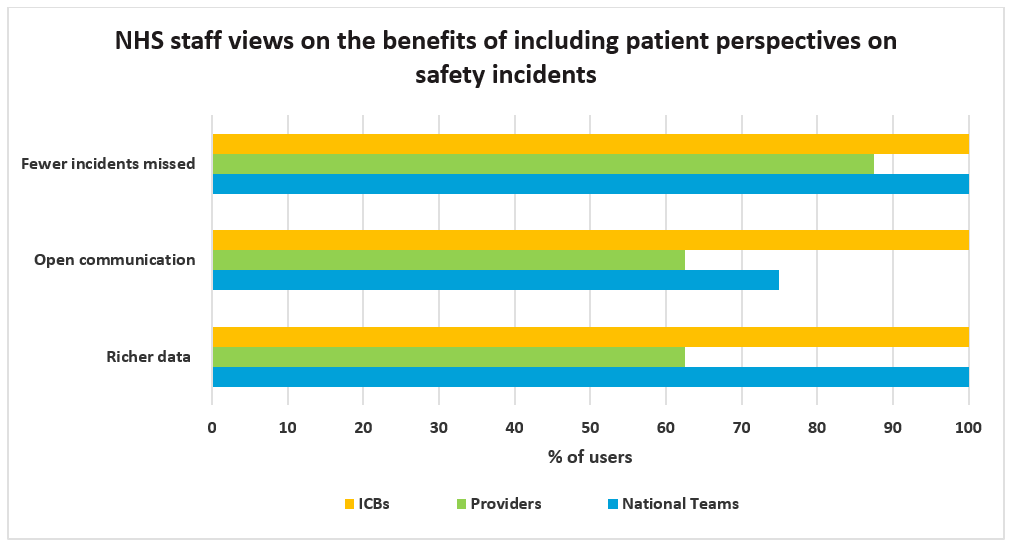
These were the top 3 benefits identified by the NHS staff we spoke to:
- Fewer incidents missed – Gaining direct feedback from patients would likely result in fewer safety incidents being mislabelled as complaints.
- Open communication – Communicating more openly and providing a simple mechanism for patients to do so would reduce frustration and subsequent complaints stemming from miscommunication.
- Richer data – The data provided would have more detail and would highlight additional areas of potential learning.
National teams
Cultural issues – These types of issues are not currently widely addressed. However, through the patient’s perspective it may be possible to identify and learn from such concerns, creating a new form of analysis that can produce richer data for national learning purposes. While this data might be seen as subjective, if there are numerous reports around the same concern, this could indicate an issue that would not otherwise be picked up.
Direct recording – Recordings that are made directly by patients provide the most authentic account of their experience, in ways that have not been seen before. This will also lead to a greater understanding of the psychological impacts on patients.
Consumable data – Learning from the patient’s perspective will help provide consumable data, such as case studies. Doctors can relate to this data more as they can identify how their own patients could be impacted.
Complaints vs event recording – More data would be captured through event recordings as information provided through the complaints process potentially contains clinical information and may otherwise be missed. This provides the capacity to look at smaller emerging trends.
Increased opportunities for analysis including machine learning capabilities – Adding the patient’s perspective will create more data to drive data analytics and machine learning driven insights helping to detect safety issues quicker and more systematically.
The people we interviewed who work in national teams said:
- “By including their voices, it would enhance their intelligence and allow them to triangulate on issues surrounding safety culture and how they are responding.”
- “The individual patient is the one common denominator across all their care experiences, making them a natural source for information across healthcare professionals, services and care.”
- “Complaints data can act like early warning signs and can be a great indicator for service monitoring and organisational learning.”
- “A real authentic patient voice is so valuable as it provides an authentic account of events, and it is the only way we can deal with the problem and highlight the stress upon the system.”
- “You gain a more detailed account of events when it comes to a patient’s perspective, and you get an idea of the emotional impact on the individual as well as their relatives. This is missed when recorded by a third party.”
Providers
Enhanced data – Including the patient’s voice would enhance the providers’ intelligence, allowing them to triangulate on issues surrounding safety culture and improve their response to these types of concerns. This feedback would help create richer data that could improve safety locally.
Authentic data – A more detailed account of an event is provided when it comes from a patient’s perspective as it is not rewritten by third parties. This means no potentially vital detail is lost; for example, the emotional impact on the individual or their relatives.
Fewer complaints – Speaking to the patient and engaging with them proactively can help ensure that the patient feels heard and can therefore help to reduce the risk of the complaints process being triggered.
Reminds clinicians of the value – Better reporting mechanisms can help clinicians better empathise with their patients beyond the clinical perspective and understand the emotional impact that safety events can have on patients.
The people we interviewed who work in providers said:
- “We can get this response right for our patient and learn the lesson that we need to do.”
- “If we can bring patient stories in…hopefully it can bring them [doctors and nurses] closer to our patients.”
- “I think it would be critical intelligence.”
- “Really hearing their story and seeing their emotions absolutely helps to understand.”
- “When we’ve been open and transparent with the patients it’s actually stopped them making a formal complaint as well.”
NHS stakeholder user needs
Summary
The top 3 needs identified by NHS staff were:
- No duplication – Data needs to be provided once; duplication could exaggerate the prevalence of an issue.
- Cultural shift – Recording needs to be seen as beneficial and not harmful so that people are encouraged to record.
- Data quality – Only the most relevant data is needed so that information key to learning is not overlooked.
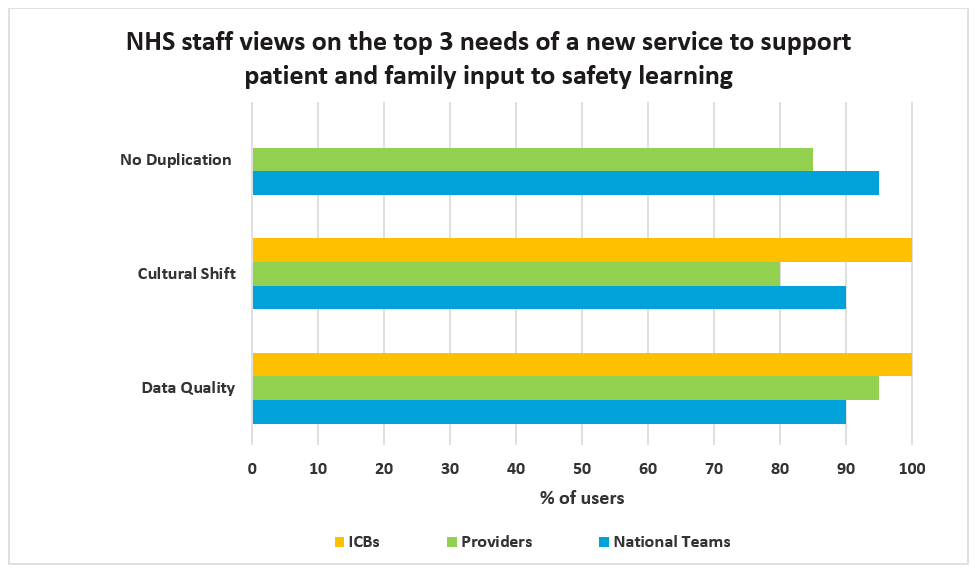
N.B, ‘No duplication’ was not included for ICBs as was not expressed during interviews.
National teams
National teams need:
- Sight of all information that could be relevant even if it has not been selected for review in more detail, so that they do not miss any potential safety issues, even low to no harm events.
- Incident recordings to be viewed as beneficial and not a threat to the trust or individuals, so that issues are not under-recorded.
- Users to understand what information is required to ensure they only receive priority information.
- Users to understand that the service will not be able to guarantee a response or to rectify every individual issue.
- Only the relevant information to a case; including data that does not add value as can make the identification of issues difficult.
- Data not to be duplicated so that they do not review the same data more than once.
People from the national teams said:
- “We don’t want incident reporting to be used as a threat.”
- “There’s just miscommunication, misunderstanding, false expectations, all of that.”
Providers
Providers need:
- Data to be authentic and transparent so that the correct information is recorded.
- Patient’s to be engaged throughout the process to prevent complaints being made due to miscommunication.
- The option for patient recordings to be given anonymously, to ensure that patients who may be afraid of any consequences can do so without fear.
- Patients to understand how the data they provide will be used nationally/locally so that patient safety events are handled in a satisfactory way for patients.
- Only the most relevant information so that they do not receive a lot of excess detail.
- Data not to be duplicated so that they do not review the same information more than once.
People we spoke to within providers said:
- “When we’ve been open and transparent with the patients it’s stopped them making a formal complaint.”
- “Really hearing their story and seeing their emotions absolutely helps to understand.”
Patients’, service users’ and families’ views
This section first sets out what patients, families and carers told us in the user research sessions, and then what we were told through a survey.
Summary
Pain points
- Lack of acknowledgment/response.
- No clear signposting of where patients need to go.
- Lack of active engagement with patients throughout the process.
- Patients fear their care will be affected if they raise a concern.
Needs
- The process needs to be accessible for all.
- There needs to be clear signposting telling patients where to go.
- There needs to be engagement with the patient.
- Patients need to know what will happen with this information.
Patient motivations
- The most frequent motivation mentioned by patients was a desire to prevent similar events from occurring to others in the future.
- Patients are often motivated to record an event to improve the quality of the care they are receiving.
- A desire to ensure that NHS England learns from patient feedback was also mentioned.
Barriers to recording
Fear – Most patients expressed that they would be fearful of their care being impacted by any complaints/concerns that they raise.
Time – Several patients, particularly those who have actively engaged in the recording process previously, stated that the time-consuming nature of raising concerns would deter them.
Futility – Some patients stated that they felt that raising a concern was futile, as they would not be listened to, and nothing would come of their recordings.
Pain points
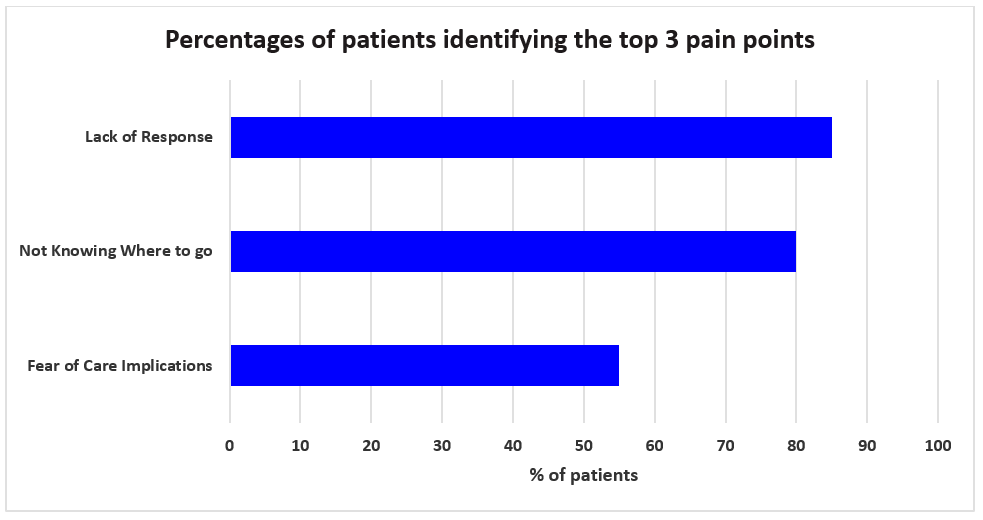
Lack of response – If patients do not receive a response after they raise a concern, they feel they are not being heard.
Not knowing where to go – Knowing where to go is not obvious and avenues are not clearly signposted, leaving patients feeling the only option is to record an issue on the ward in person.
Fear of care implications – Concerns that their care will be affected prevents patients from recording any issues.
Patient concerns
The patient’s authentic account is lost as they are rewritten by staff, and they are not engaged with throughout the process. It is a passive experience and this can be distressing for patients.
Reputational management is often prioritised over reaching out to the patient and learning about their experience. The language used to engage with patients is often corporate and makes patients feel they are being managed.
Lack of response frustrates patients and escalates the situation as they feel that their concerns are being “sent into the ether”, leading patients to feel as though no one is interested in their concerns and that recording concerns is futile. There is no communication about what will be done with the information they provide.
Patients do not know where to go or who to speak to regarding their concerns. The only avenue that they are aware of is the complaints process.
Fear of being treated differently after raising a concern: “You are dependent on them, especially if you require long-term care, which can be distressing.”
The length of the experience; it can take several years to find any kind of resolution. This can be incredibly difficult for people who suffer from long-term health conditions and do not have the capacity to attend all the meetings or follow-up on their safety concerns.
Patients do not feel heard and feel that they are overlooked throughout the process.
Patients do not always want to cause a fuss and can feel that they are an inconvenience if they raise a safety concern.
User needs
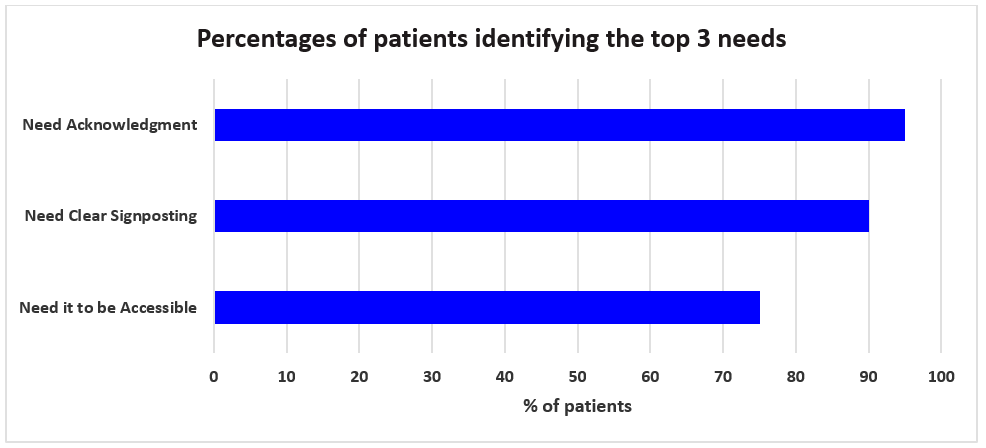
The top 3 needs identified by patients, families and carers were:
- Accessibility – Patients need to be able to access a service that works for them and does not exclude them based on their capabilities.
- Clear signposting – Clear signposting of the correct avenues for recording is needed, as currently not all avenues are well-known.
- Acknowledgement – Patients need confirmation from those receiving their complaint that it will be looked into and not ignored, and with this know that recording it is worth their time.
Patients need:
- Someone who is non-biased and independent from their care to review their concerns so that their care is not impacted.
- To be able to immediately raise a concern so that it can be addressed in a timely manner.
- To know where to go so that they do not have to spend considerable time trying to find out what to do.
- To trust in the process and be engaged with regularly so that they know it was not a waste of their time to report.
- To understand what constitutes a safety incident so that it is clear to them when they should raise a concern.
- In person help to record their concerns as they cannot always access online services without assistance.
- Feedback so that they know their concerns have gone to the right people and not disappeared into the void.
- To be able to provide their own perspective so that their experiences are accurately reflected.
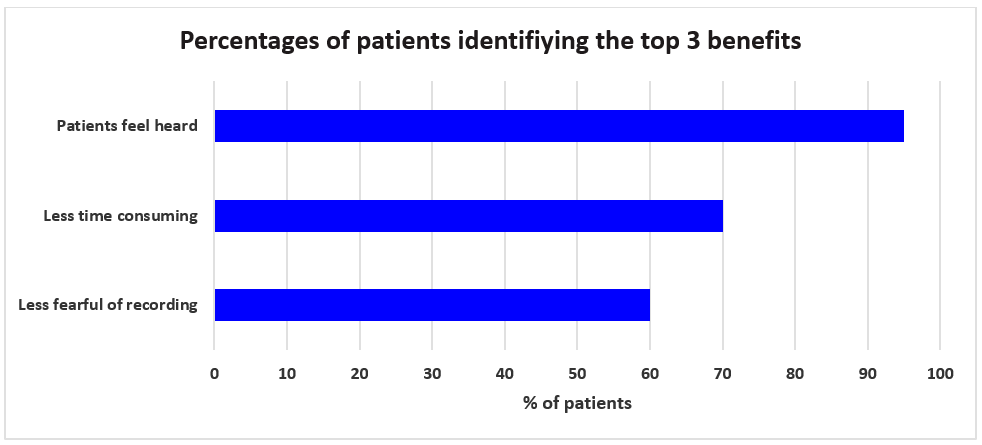
Benefits
The top 3 benefits of research identified by patients, families and carers were:
- Patients feel heard – Through providing their perspective, patients feel that they are actively being engaged with and therefore less likely to feel overlooked.
- Less fearful of recording – By creating a culture that encourages recording, this will help to stop patients from feeling fearful that recording their concerns will impact their care.
- Less time consuming – Providing an online service for patients would create a quicker, more streamlined service that is more visible to patients and thus easier to find.
Preferences for recording their experiences of safety events
- In-person and online – Most patients stated that they would be happy to use an online service but, if they were recording a “serious concern”, they would like this to be alongside in person contact.
- Online service – Most patients stated that they would be comfortable using an online service and would prefer this for its ease and flexibility. They would search for the trust’s page and look for the information there.
- Recording safety events vs complaints – The most frequently mentioned recording method was complaints as it is the most obvious avenue to patients; however, they said using this avenue felt “combative”.
- Social media – All interviewed patients stated that they would not want to use social media to record safety events or concerns.
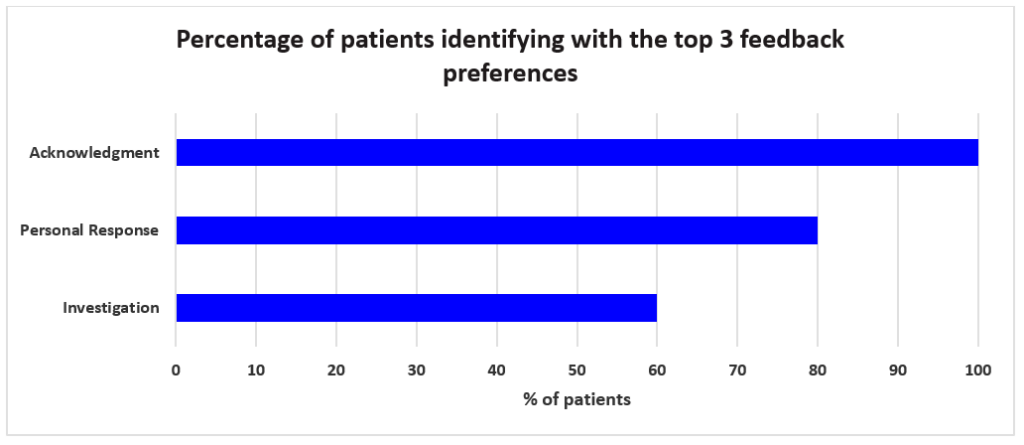
Patient feedback preferences
The top 3 preferences were:
- Acknowledgment – 100% of patients specified that they would expect at least an acknowledgment that their concern has been received.
- Personal response – 80% stated that they would expect a personal response outlining what would be done with the information they have provided.
- Investigation – 60% stated that they would expect an investigation into all the concerns they raise.
Survey responses
Around 100 members of the public volunteered to be interviewed for user research, but we were only resourced to schedule around 20 sessions. The remaining 80 people were sent a survey to capture their views. The survey was written using plain English and reviewed by members of the NHS Citizen Advisory Group.
The survey results were extracted on Monday 25 September. The survey will remain open for several more weeks and be circulated to a wider audience. Any data received after 25 September will be used in an Alpha phase to validate previous findings.
30 people had responded by 25 September. Several of the questions were multi-select, so some totals exceed 30.
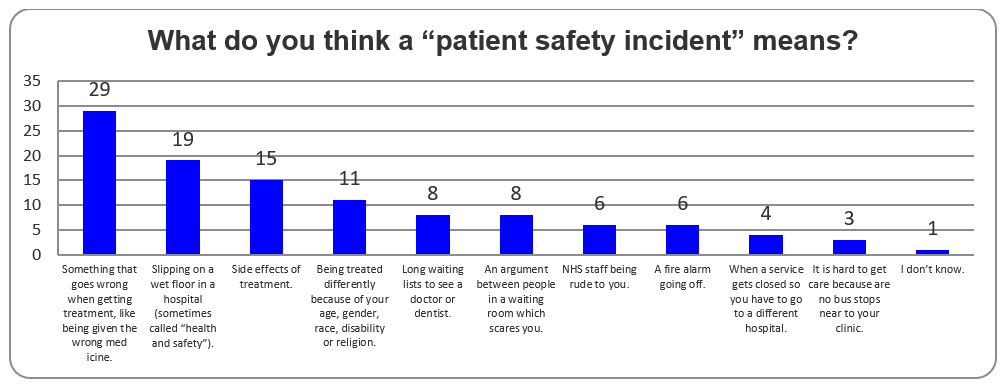
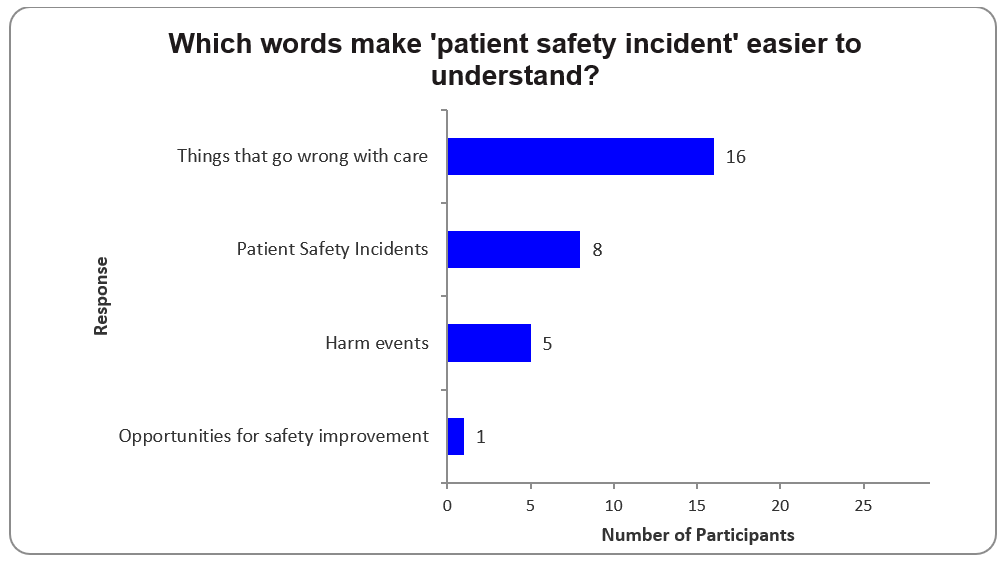
Understanding of ‘patient safety incident’ terminology
- 29 respondents correctly identified a safety incident as “something that goes wrong when getting treatment, like being given the wrong medicine”.
- However, most also identified other things that do not meet the definition of a patient safety incident, indicate that there is a lack of clarity about what does and does not “count”.
Something that goes wrong when getting treatment, like being given the wrong medicine.
Slipping on a wet floor in a hospital (sometimes called “health and safety”).
Side effects of treatment.
Being treated differently because of your age, gender, race, disability or religion.
An argument between people in a waiting room which scares you.
Long waiting lists to see a doctor or dentist.
A fire alarm going off.
NHS staff being rude to you.
When a service gets closed so you have to go to a different hospital.
It is hard to get care because are no bus stops near to your clinic.
I don’t know.
Not Answered
Terminology preferences
Feedback services
Familiarity with existing services
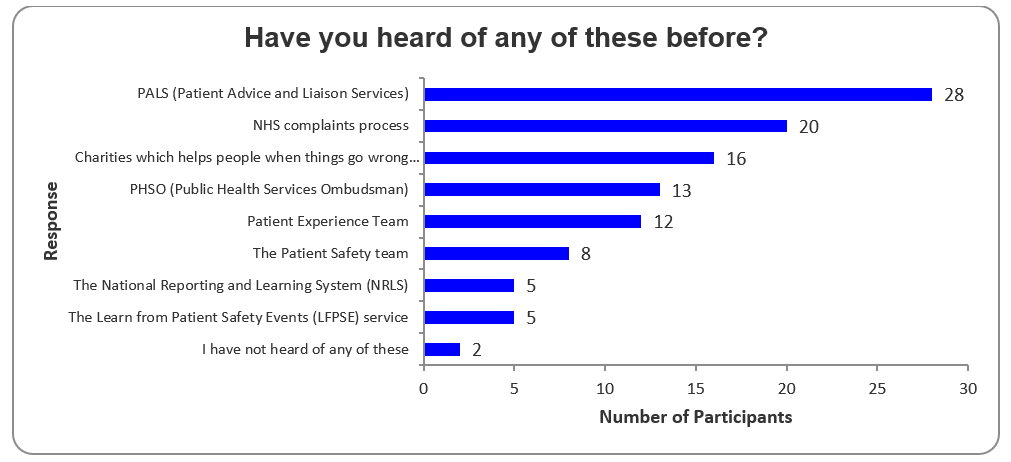
PALS (Patient Advice and Liaison Services)
NHS complaints process
Charities which helps people when things go wrong (such as the Patients Association, Healthwatch, Care Opinion)
PHSO (Public Health Services Ombudsman)
Patient Experience Team
The Patient Safety team
The National Reporting and Learning System (NRLS)
The Learn from Patient Safety Events (LFPSE) service
I have not heard of any of these
Not Answered
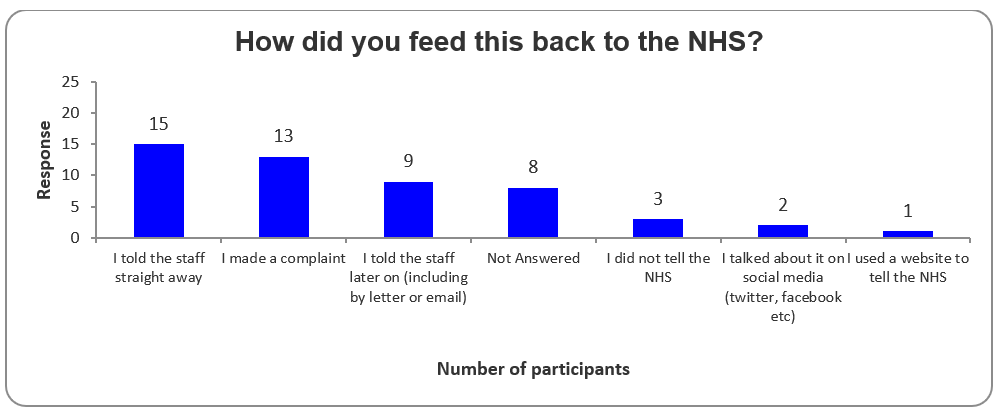
Routes used in the past
Of the 22 respondents who had raised safety concerns in the past, 15 did so by speaking directly to staff and 13 raised a complaint.
Recording preferences
- 21 respondents said they would use an online service.
- Most respondents said in the past they had spoken to staff immediately or made a complaint when recording events.
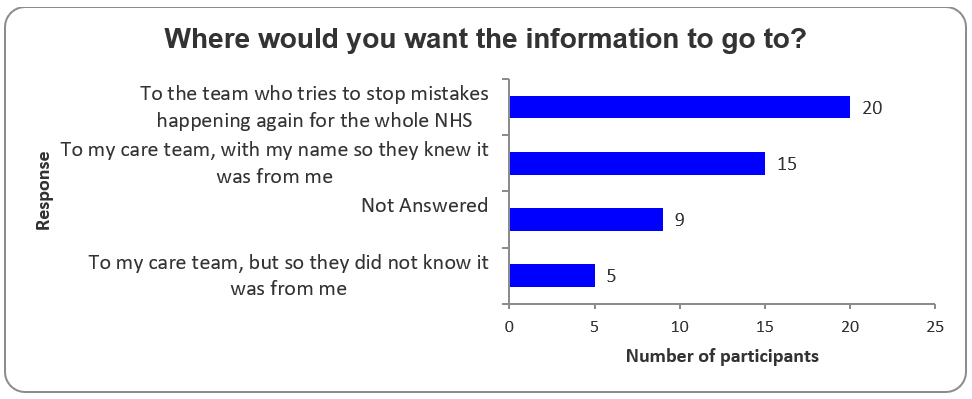
- 20 respondents stated they would want the information to go to a team that works to stops mistakes happening nationally.
Online form preferences
Of the 21 respondents who would use an online form:
- 17 wanted space to write “whatever they want”.
- 15 stated that it would be useful if questions helped them decide what information they should provide.
- 12 wanted questions with drop-down answer options to pick from.
Feedback preferences
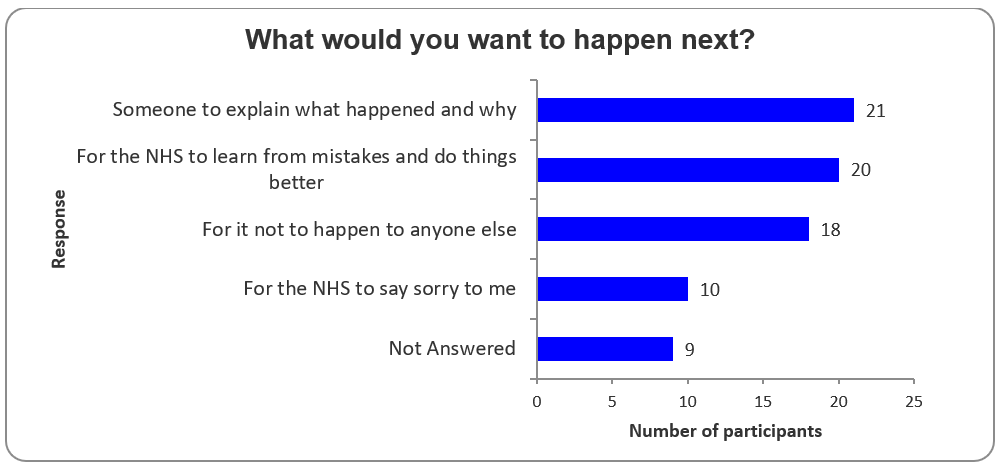
21 wanted “someone to explain what happened and why”; 20 wanted “for the NHS to learn from mistakes and do things better”; 18 wanted “for it not to happen to anyone else”; 10 wanted “the NHS to say sorry to me”, and 9 did not answer.
Preferences for feedback usage
Next steps and considerations for Alpha
Three high-level options for a digital service to help incorporate patient and family experiences of patient safety incidents have been identified. They fulfil different levels of user need and come with varying levels of complexity and therefore cost.
Option 1: Local collection – each healthcare setting collects patient feedback in its own way
Description
- Each trust would be responsible for running its own collection methods for patient views of patient safety events. This could be done using various existing methods such as PALS and LRMS.
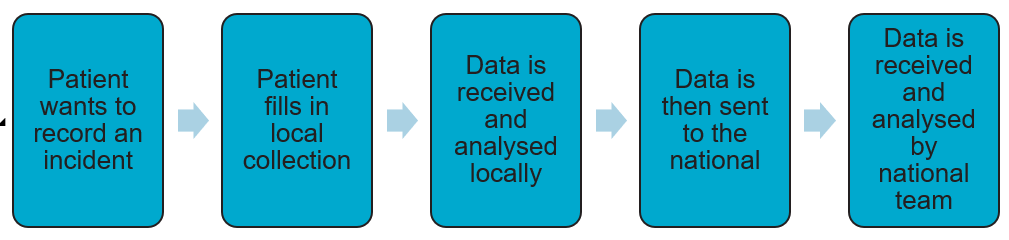
A diagram outlining the main steps in the local collection option. This is a linear process of: Patient wants to record an incident Patient fills in local collection Data is received and analysed locally Data is then sent to the national Data is received and analysed by national team
Key advantages
- Trusts have flexibility to implement processes that work best for them.
- Allows organisations to create and establish relationships with their patients for richer quality feedback.
- Provides opportunities to give patients feedback on any outcomes/investigations when incidents are reported.
Key disadvantages
- No standardised process for collecting patient feedback.
- Inconsistent quality of data.
- No control from the national team over what data is received.
- Patients may not feel comfortable recording locally.
- Likely to produce duplicated data, which could make the review processes inefficient.
LFPSE feasibility and readiness
- Patient data standard would need to be established with providers for exchange data collected from patients.
- Ability to surface data through national review tools.
Option 2: National collection – one service feeds into the national service
Description
- Patients would record safety incidents directly into a national system.
- This mirrors the legacy state using the NRLS eForm.
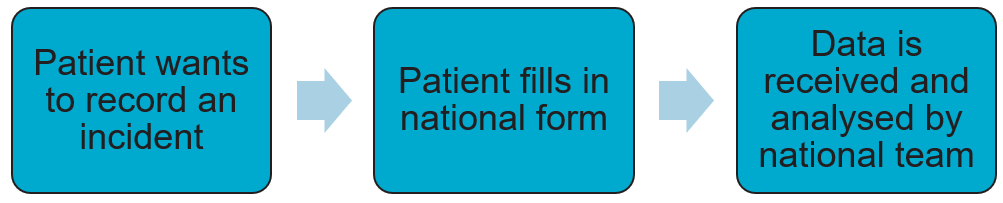
Data is then sent to the national
Data is received and analysed by national team
Key advantages
- Organisations do not have to maintain their own systems.
- One standardised process.
- Consistency across the dataset.
- National team have control over what data fields are asked for and received.
Key disadvantages
- No ability to provide patients with direct feedback on any incidents raised.
- No ability for trusts to tailor data collection to their individual needs.
- No ability for trusts to create and establish relationships with their patients for richer quality feedback.
- Likely to produce duplicated data which could make the review processes inefficient.
LFPSE feasibility and readiness
- New online data collection capability for patients to input into LFPSE.
- Ability to surface data through national review tools.
Option 3: Hybrid local-national collection approach
Description
- National team would produce a data collection method that would then be picked up by trusts.
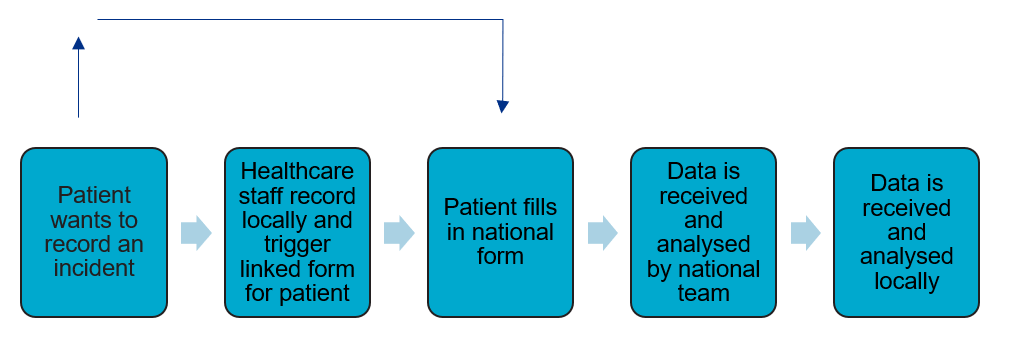
A diagram outlining the main steps in the hybrid local-national collection option. This process is mostly linear, with the main flow being: Patient wants to record an incident Healthcare staff record locally and trigger linked form for patient Patient fills in national form Data is received and analysed by national team Data is received and analysed locally But with the additional pathway of the patient going directly to the national form, if they do not want to speak to staff locally.
Key advantages
- Trusts have flexibility to implement processes that work best for them.
- Allows organisations to create and establish relationships with their patients for richer quality feedback.
- Provides opportunities to give patients feedback on any outcomes/investigations when incidents are reported.
- Organisations do not have to maintain their own systems.
- One standardised process and consistency across the dataset.
- National team have control over what data fields are asked for and received.
Key disadvantages
- More technical complexity and implementation effort, including potential patient identifiable information (PII) handling and complexity around data sharing.
LFPSE feasibility and readiness
- New online data collection capability for patients to input into LFPSE.
- Ability to create linked records for patients and healthcare professionals.
- Push/pull data retrieval mechanism for vendors including extended authentication controls.
Options assessment
This table lays out all the identified user needs, by user group, and rates the extent to which each of the above three options has the potential to meet those needs on a scale of 0 to 2.
0 means the need is not met; 1 that it is partially met; 2 that it is met.
| User need | Option 1: Local | Option 2: National | Option 3: Hybrid | |
| Patients | ||||
| I need to feel listened to so that I feel there is value in offering my feedback. | 2 | 0 | 2 | |
| I need to know my concerns are being dealt with and taken seriously so that it doesn’t happen again. | 2 | 1 | 2 | |
| I need assistance with raising my issue so that my concern can be progressed while I’m busy with long-term care. | 2 | 0 | 2 | |
| I need to be able to immediately raise a concern so that it can be addressed in a timely manner. | 2 | 2 | 2 | |
| I need to know how my information will be used so I know what to expect. | 2 | 2 | 2 | |
| I need to be able to provide my own perspective so that it accurately reflects my experience. | 2 | 2 | 2 | |
| I need someone who is without bias and independent from my care to review my concerns so that my care isn’t impacted. | 1 | 2 | 2 | |
| I need to be able to raise concerns on someone else’s behalf so that those unable to raise concerns for themselves can still be advocated for. | 2 | 2 | 2 | |
| I need to be able to quickly find where to raise a concern so that I don’t waste valuable time. | 2 | 2 | 2 | |
| I need people who are independent to review the data so that there is no bias throughout the investigation. | 1 | 2 | 2 | |
| I want to trust in the process and be engaged with regularly so that I know it wasn’t a waste of my time. | 2 | 0 | 2 | |
| I need to know where to go so that I don’t have to spend considerable time trying to find out what to do. | 2 | 2 | 2 | |
| I need clear, accessible information about how to access assistance so I know I can get help if I need it. | 2 | 2 | 2 | |
| I need in person help to record my concerns as I cannot always access online services without assistance. | 2 | 0 | 2 | |
| I need to understand what constitutes a safety incident so that it is clear to me when I should raise a concern. | 2 | 2 | 2 | |
| I need feedback so that I know my concern has gone to the right people and not disappeared into the void. | 2 | 0 | 2 | |
| I need to raise my concerns simply and quickly so that doing so doesn’t add to my stressful situation and cause me more distress. | 2 | 2 | 2 | |
| I need to know about any changes that are happening as a result of my feedback, so that I know there’s been improvements. | 2 | 0 | 2 | |
| I need an easy process; simple and quick | 2 | 2 | 2 | |
| I need the option for anonymity so that I do not fear my care could be affected. | 1 | 2 | 2 | |
| I need to write the recording myself so that I know all details that are important to me have been noted. | 2 | 2 | 2 | |
| I need to know what will happen next so that I know what to expect from the service. | 2 | 2 | 2 | |
| National teams | ||||
| I need sight of all information that could be relevant even if it has not been selected for review in more detail, so that I do not miss any potential safety issues. | 1 | 2 | 2 | |
| I need incident recording to be viewed as beneficial and not a threat to the trust or individuals, so that issues are not under-recorded. | 2 | 2 | 2 | |
| I need users to understand what information is required to ensure we only receive priority information. | 1 | 2 | 2 | |
| I need users to understand that the service will not be able to guarantee a response or rectify every individual issue. | 1 | 2 | 2 | |
| I need to have only the relevant information to a case, so that data that does not add value is not included as this can make it difficult to identify issues. | 0 | 2 | 2 | |
| I need data not to be duplicated so that we do not review the same information multiple times. | 0 | 0 | 2 | |
| I need patients to have the option to provide recordings anonymously so they can do so without fear of any consequences. | 1 | 2 | 2 | |
| Providers | ||||
| I need the data to be authentic and transparent so that the correct information is recorded. | 2 | 2 | 2 | |
| I need patients to be engaged with throughout the process to prevent complaints being made due to miscommunication. | 2 | 0 | 2 | |
| I need patients to have the option to provide recordings anonymously so they can do so without fear of any consequences. | 2 | 2 | 2 | |
| I need only the most relevant information so that we do not receive a lot of excess detail. | 1 | 2 | 2 | |
| I need patients to understand how the data they provide will be used nationally/locally so that patient safety events are handled in a satisfactory way for patients. | 2 | 2 | 2 | |
| I need data not to be duplicated so that we do not review the same information multiple times. | 1 | 0 | 2 | |
| I need sight of all data so that no potential learning is missed. | 2 | 0 | 2 | |
Recommendation
Based on this assessment, we recommend that Option 3 is taken forward for further exploration in an Alpha phase.
Key considerations for Alpha
Signposting
- Identify the most appropriate places to advertise the service, e.g. wards, GP surgeries.
- Explore where it would be appropriate to link to other existing services such as complaints.
Collection of data
- Work in Alpha should look at determining what the priority fields are to collect from patients.
- Questions will need to be written in plain English and non-clinical language, to be accessible to everyone.
- Ideally, questioning will be tailored to the incident and much shorter than for staff recording. Options such as adaptive question response techniques should be considered.
- Different channels for collecting data should be explored; during the research users had mentioned options such as SMS, online form and NHS App.
Areas for more research/prototyping and testing
- Define minimum dataset – type and depth of information that patients are willing/able to provide.
- Linking of records in LRMS and LFPSE.
- Ensure hypotheses for service design work for both primary and secondary care settings.
- Any limitation to or barriers that may be created by data sharing and consent?
- Ensure patient expectations around ‘investigation’ are understood and adequately accounted for under the new Patient Safety Incident Response Framework.
Appendices
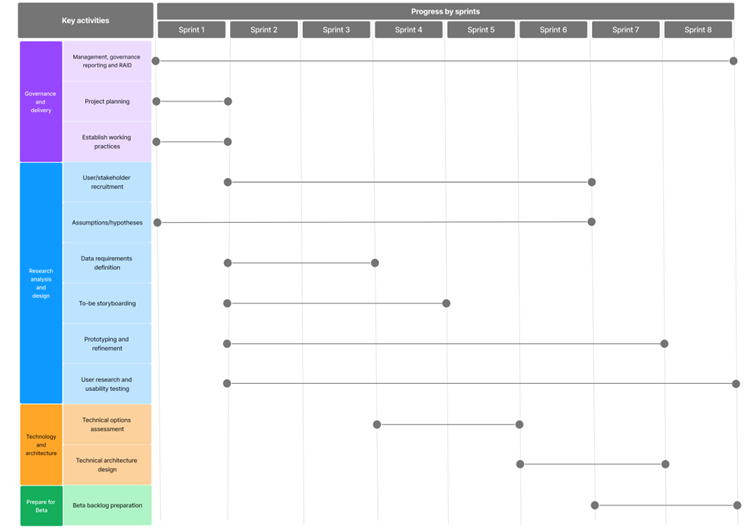
Proposed high level Alpha plan
Demographics of user research participants
Research participants were asked optionally to share demographic data about themselves.
Interviewees
| Age Range | % | Ethnicity | % | Gender | % | Disability | % |
| 35-44 | 4.8 | White | 81.0 | Female | 52.4 | No | 57.1 |
| 45-54 | 28.6 | Asian/British Asian | 4.8 | Male | 42.9 | Yes | 42.9 |
| 55-64 | 42.9 | Mixed/Multiple Ethnicities | 4.8 | Prefer not to say | 4.8 | ||
| 65 and over | 23.8 | Other inc Arab | 4.8 | ||||
| Prefer not to say | 4.8 |
Online survey
| Age Range | % | Ethnicity | % | Gender | % | Disability | % |
| 18-24 | 3.3 | White | 83.3 | Female | 70.0 | No | 46.7 |
| 25-34 | 3.3 | Asian/British Asian | 6.7 | Male | 30.0 | Yes | 50.0 |
| 35-44 | 10.0 | Mixed/Multiple Ethnicities | 6.7 | Prefer not to say | 3.3 | ||
| 45-54 | 26.7 | Prefer not to say | 3.3 | ||||
| 55-64 | 26.7 | ||||||
| 65 and over | 30.0 |
Personas
National teams
Role
Promotes high quality health and care for all and supports NHS organisations to work in partnership to deliver better outcomes for their patients and communities.
Quotes
- “That search can bring through noise or it can miss what you’re searching.” – Analysing the LFPSE for themes
- “Think it sometimes feels like we’re on the back foot a bit.”
How is patient feedback captured?
- The data is captured directly through the incident recording process i.e. the e-form and NRLS/LFPSE.
- Incident recordings are viewed through the national review tool and are analysed through deep dive search to find key terms and identify trends. This is then used to generate learning reports.
- LFPSE data is live and analysed daily by the clinical review team to highlight cases of interest for review within meetings.
Current learning process
- Analysts create reports based on requests from stakeholders, such as royal colleges and universities, looking into certain topics of interest.
- Safety event data is analysed to create learning reports which highlight cases of interest and key themes. This analysis is carried out through a free text search using agreed terms to find the most relevant data. These reports are then shared with relevant commissioners.
- NHSR uses these reports to support doctors learning. This is particularly important as doctors prefer case studies for identifying issues which could potentially impact their own work/patients.
- National teams have insight into the local level learning, as updates in guidance are fed back to them for commentary.
User needs
- I need sight of all information which could be relevant even if it is not selected to review in more detail, so that we do not miss any potential safety issues, even low to no harm events.
- I need incident recording to be viewed as beneficial and not a threat to the trust or individuals, so that issues are not under-recorded.
- I need users to understand what information is required to ensure we only receive priority information.
- I need it to be clear to users that the service will not be able to guarantee a response or be able to rectify all of their individual issues.
- I need to have only the relevant information to a case, so that excess data which does not add value is not included as this can make the identification of issues difficult.
Pain points
- Complaints are not extracted centrally, making it more likely that cultural issues are missed.
- The available capacity of providers impacts the level of detail of complaints outputs.
- The safety and complaints teams do not always interact, potentially leading to issues being overlooked.
- Complaints may include clinical data which should have been recorded as a safety incident as often a patient’s mental model is of something going wrong rather than there being a distinction between a safety event and a complaint specifically.
- Extracting learning from the incident recording can be difficult as they often include excess information especially in the patient e-form as there are several fields, many of which are free text, resulting in main points get lost.
- National learning teams’ analysis is often reactive rather than proactive.
- Patients don’t know about the services they can use to report incidents, leading to potential issues not being recorded.
- Team capacity means there are limitations on the amount of information we can analyse in depth.
Trusts
Role
A legal entity that provides health care for the NHS. This can include hospital, mental health, community, and ambulance services that treat patients and service users.
Quotes
- “We may not know that there’s been an incident, and the only time we know about it is when it comes through via a complaint.”
- “You’re constantly reaching out, there isn’t a central portal.”
How is patient feedback captured?
- Patient feedback is captured primarily through PALS (patient advice and liaison service), complaints, speaking directly to ward matrons, and incident recording. Patients are also engaged with at the end of serious harm investigations when they asked to review investigation reports.
- There is the FFT (friends and family test) which captures patient’s feedback using a form. Patient participation services will also go onto wards and have informal conversations with patients.
- MP’s, Care opinion, and Healthwatch may also email in feedback and information on behalf of patients.
Current learning process
- Generally, incidents will be reviewed based on their harm level, with serious harm incidents being investigated in the most detail. Reports are generated from these investigations which stem from incidents being raised by clinicians.
- Meetings are held fortnightly to identify possible areas of learning stemming from the reports.
- The data is analysed to look for key trends which are then reviewed to see if any learning can be identified.
- Some trusts use a patient safety panel where learnings are shared and disseminated across divisions.
- Patient stories are also used in meetings to make it more personal for the staff.
User needs
- I need the data to be authentic and transparent so that the correct information is recorded.
- I need patient’s to be engaged throughout the process to prevent complaints being made due to miscommunication.
- I need patient recordings to have the option for anonymity to ensure that patients who may be afraid of any consequences can do so without fear.
- I need only the most relevant information so that we do not receive a lot of excess detail.
- I need patients to understand what will be done with the data provided nationally/locally in order to handle patient safety events in a satisfactory way for patients.
- I need data to not be duplicated, so that we do not review the same information multiple times.
Pain points
- Often a patient’s mental model is of something going wrong rather than there being a distinction between a safety event and a complaint specifically. Incidents may therefore be missed and only identified through the complaints process.
- Data is not stored centrally making “getting sight of it difficult.
- There is a risk of duplicated data when a patient moves to a different ward.
- There is often a lot of excess information within complaints which makes identifying a potential safety event difficult.
- Smaller providers are reactive and only raise a safety event recording after a complaint has been raised.
- Direct feedback to patients which staff can provide, is not tracked and therefore can’t be learnt from.
- Patient’s perspective is filled out on their behalf by clinicians, which can lead to patients feeling unheard.
Patient: Kendall
Role
Kendall is a recipient of health care treatment. He is 32 and does not receive long term treatment but has been treated in hospital recently.
Quotes
- “There would have to be a dialogue to ensure that anything comes of it.”
- “How somebody would know where to go I don’t know.”
Patient’s recording preferences
- Kendall would likely record an incident immediately in person to whoever is involved in his care but would be comfortable recording a concern online.
- He would expect some form of acknowledgement, including information stating that it was being looked at, what the process was, and the time frame of expecting a response.
- Kendall wants to know his feedback is being used and without a response he would feel as though his input had disappeared into the void.
Understanding of incident recording
- Kendall views a patient safety event as anything which adversely affects the care and safety of patients, their families and carer.
- Kendall worries about raising smaller issues as he does not feel they would not be taken seriously by staff.
- Kendall would use the complaints process in order to record something which he felt was a patient safety event.
- When searching for the service, he would search for complaints or feedback, and he would first check the Trust’s website.
User needs
- I need the information to be reviewed independently and by people who have no interest other than improving services as I do not want it to be used to influence my treatment with bias.
- I need to be able to raise a concern immediately, so that I don’t have to carry my worries with me for long periods.
- I need receive a personal response and for everything to be looked at on a local level in some capacity.
- I need clear signposting wherever I am receiving care which tells me where to go.
- I need to know how the information will be used so that I know what to expect.
- I need to feel heard by the care team in order to build trust with them.
- I need to know what qualifies as a safety concern to ensure I’m recording to the right place.
- I need it to be simple and quick so that it is an easy process.
Pain points
- The authentic account of the Kendall’s version of events is ignored and rewritten by staff members leading to inaccuracies and misrepresentations of information, leaving Kendall feeling unheard and ignored.
- Kendall does not know who to speak to and the information is buried within trust’s websites, and not easily identifiable.
- The experience is very passive, and Kendall is not engaged with actively within the investigation process leaving them feeling frustrated.
- Kendall feels that a lack of response from recordings leads to loss of trust in the process and in turn leads to additional frustration and complaints.
- Kendall does not know of any avenues other than a formal complaint which is off-putting as Kendall is in ongoing care.
- NHS culture issues, e.g. Doctor’s attitudes, are not looked at with the same level of concern which leaves Kendall wondering why he should bother recording it.
Patient: Glen
Role
Glen is a recipient of healthcare treatment. He is 87 years old and suffers from several long-term health conditions, including a disability. He has no relatives to help him raise any concerns he may have.
Quotes
- “Need to do something where people can write in” – Rather than online.
- “I did not know where to go or what to do and felt frustrated.”
Patient’s recording preferences
- Glen would prefer to record an event in person as he does not feel as comfortable with using online services.
- He wants a response so that he knows what is going on with his concern and when he can expect to hear back.
- Glen would also like the option for an independent advocate who could support him with his concern.
- Written literature outlining how to raise a concern should be provided to Glen.
Understanding of incident recording
- Glen does not know where to go to record an event and would usually speak directly to a member of staff who might direct him to PALS.
- Glen is worried about raising a concern as he does not want it to be seen as complaining and becomes fearful of the impact this might have on his care, particularly as he engages with the same treatment teams frequently.
- He does not like to complain as he feels it is a negative process but there often aren’t any other clear avenues signposted.
User needs
- I need to know where to go so that I don’t have to spend large amounts of time trying to find out what to do.
- I need clear, accessible information about how to access PALS so that I have something to reassure me there is help.
- I need in person help as I cannot always access online services without help.
- I need to understand what constitutes a safety incident so that it is clear to me when I should raise a concern.
- I need feedback so that I know my concern has gone to the right people and not disappeared into the void.
- I need to raise my concerns simply and quickly so that it doesn’t add to my stressful situation and cause more distress.
Pain points
- Glen is already in a stressed and vulnerable position and doesn’t want to struggle to seek out the correct recording avenue.
- Glen does not know who to speak to and useful information is often buried online and therefore not easily accessible.
- Glen does not know how to get updates after he has raised an in-person concern and has left the hospital.
- Glen does not know of any avenues other than formal complaints which can be off-putting when he must receive long-term care.
- Glen feels excluded from the process unless he actively goes out and engages with the process, which is difficult when suffering from a long-term health condition.
Patient: Sharona
Role
Sharona is the 40-year-old mother and carer to a young child who requires frequent medical treatment due to a lifelong health condition.
Quotes
- “I would expect a personal response as it proves that someone has done something about it”.
- “Needs to have good signposting and good volunteer support to access the right information.”
Patient’s recording preferences
- Sharona feels comfortable using an online service to record her concerns and any issues she might have.
- Sharona would like a response to each piece of feedback to ensure that her concerns aren’t disappearing into the void.
- If it is a serious or pressing concern then Sharona would prefer to record it in person to the most immediate member of staff, and to have it instantly rectified, as well as a recording of the event being made.
- Sharona would want a response to every piece of feedback she provides so that she knows her child’s care is being improved.
Understanding of incident recording
- Sharona fears that raising a complaint is combative and may impact the care of her child when she tries to raise one, especially as she is in need of long-term care from the team.
- The option to record anonymously is important to her for smaller issues so that she is not seen as constantly complaining.
- Sharona would use the complaints process when raising a serious concern as there is no other clear avenue for her to voice her concerns.
- Sharona would look at the trust’s website and search for complaints or feedback in order to note an event.
User needs
- I need to be able to raise concerns immediately and in person as my child cannot advocate for themselves and I needs to ensure their care is not being harmed.
- I need clear signposting so that I know who to speak to and where to go when I need to raise a concern.
- I need to feel actively engaged with so I don’t feel overlooked or as though I’m not being listened to.
- I need to be able to quickly find where to raise a concern so that I don’t waste valuable time where I need to be looking after my child.
- I need people who are independent to review the data so that there is no bias throughout the investigation.
- I want to trust in the process and be engaged with regularly so that I know it wasn’t a waste of my time.
Pain points
- Sharona struggles to know who to speak to when she needs to raise a serious concern as it is not clearly outlined where she should go.
- Sharona finds that staff are often nervous to provide her with a response as they are unsure what information they can provide.
- Sharona feels as though she is not engaged with throughout the process and therefore looses faith in the process.
- Returning with her child for future treatment is difficult as she does not have confidence in the care.
- Sharona cannot easily find the service online and therefore has to spend a long period of time searching for it, which is frustrating as they are in a stressful situation.
- Sharona often does not receive a response to her concerns and therefore wonders what the point in raising a concern is.
Patient: Wendy
Role
Wendy is a 62-year-old who has been involved in a serious harm event. She has recorded the event and escalated it throughout the system all the way to their ombudsman.
Quotes
- “I think things like good sign posting sometimes, like good volunteers, support can be really helpful just to kind of access the right information.”
- “You should get a copy of what you have recorded, with a receipt so you can record it.”
Patient’s recording preferences
- Wendy would prefer a clearly defined online system which can be used with ease and quickly.
- Wendy would rather raise her concern immediately in person to a person of authority such as the head of the ward, and would like proof that is has been recorded, and to know what’s going to happen to it.
- Wendy wants feedback on how the information is being used, with updates being provided so that she is engaged with.
- Wendy wants an independent advocate to help her with the process as she may be too ill to attend some meetings.
Understanding of incident recording
- Wendy does not know where to go if she is unhappy with the response of staff on the ward.
- Wendy worries about the impact this will have on her care which she now needs to receive.
- Wendy would use the complaints process to raise an issue.
- Wendy does not want this to happen to anybody else in the future so feels obligated to report it so that learning can occur in order to prevent it in the future.
User needs
- Wendy needs more human communication which feels less corporate and impersonal so that she feels listened to.
- Wendy needs to know where to go as it is often unclear who she should speak to.
- Wendy needs a response so that she knows her concerns are being taken seriously.
- Wendy needs an independent advocate as she may be in long-term treatment and not have the time to attend all meetings.
- Wendy needs to be able to speak to someone in person as she may need it to be addressed urgently.
- Wendy needs to know how they will use the information she’s provided so she knows what to expect.
- Wendy needs her input to come from her directly and not written on her behalf so she can include all important information.
Pain points
- Wendy does not know how far to pursue it as she cannot attend all of the meetings and it is incredibly time consuming and can go on for several years, often reaching a point of futility.
- Wendy is fearful of the impact on themselves and their family: She is very dependent on them and often she can only raise it directly to the person she’s complaining about.
- Wendy finds finding who to talk to incredibly difficult, she does not know who to approach and as there is an inability to identify who to speak to.
- Wendy feels everything happens in silos, meaning nothing gets passed along.
- Wendy’s experience is very passive and she is not actively engaged with, often feeling marginalised and ignored.
- Wendy feels the NHS is more concerned with reputational management than just speaking to the patient and their family, instead using corporate communications.
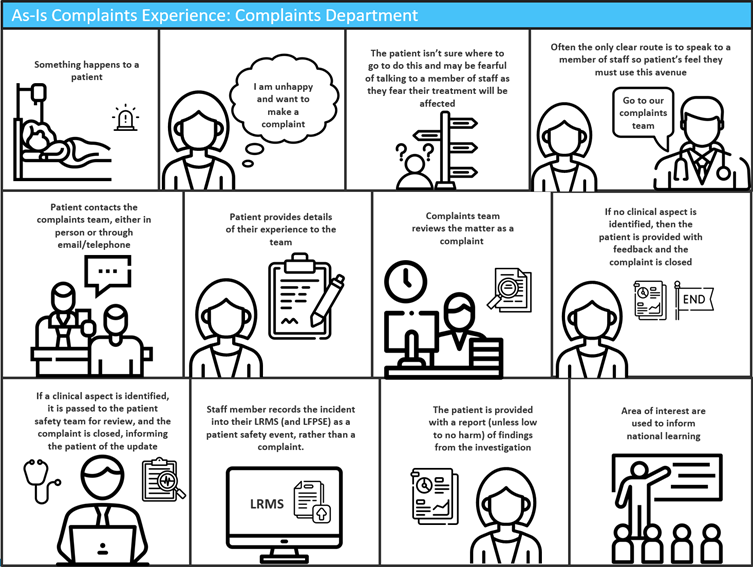
User journey map: Current process
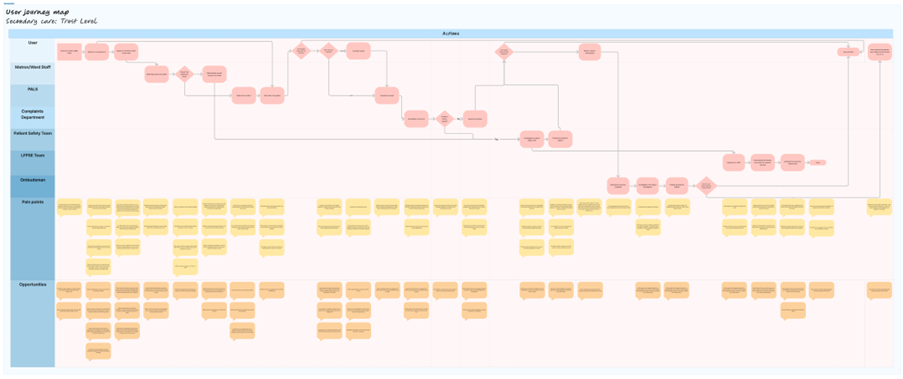
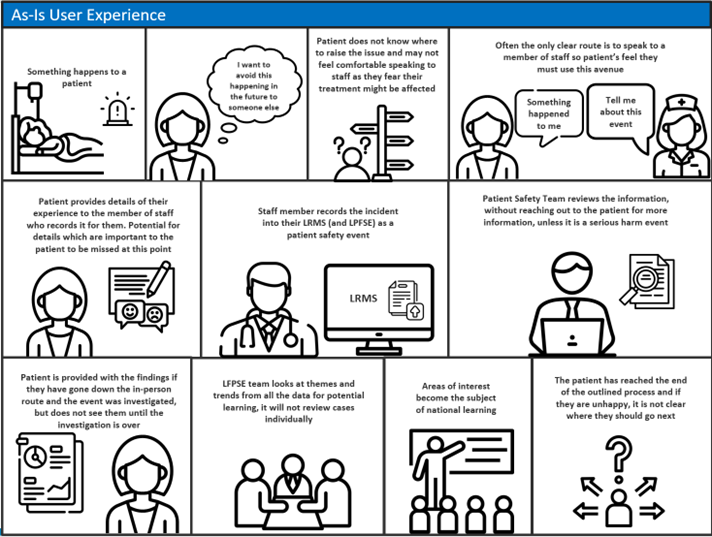
User journey: Current experience
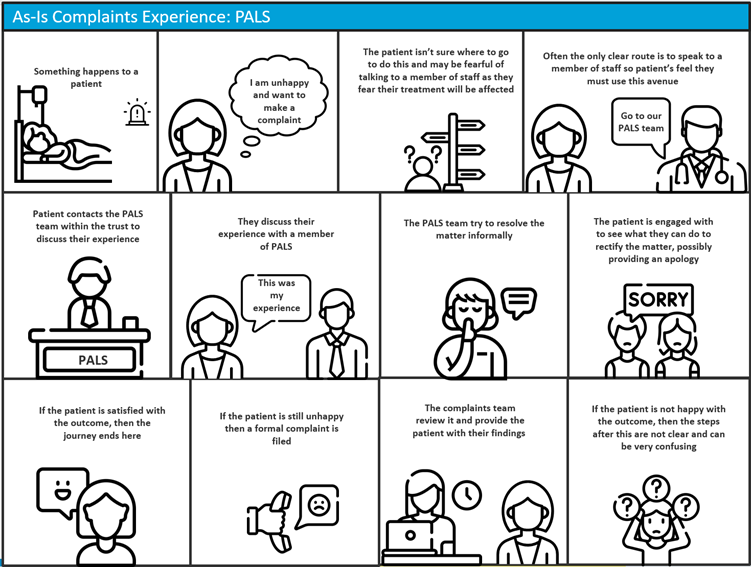
User journey: Current PALS route
User journey: Current complaints route
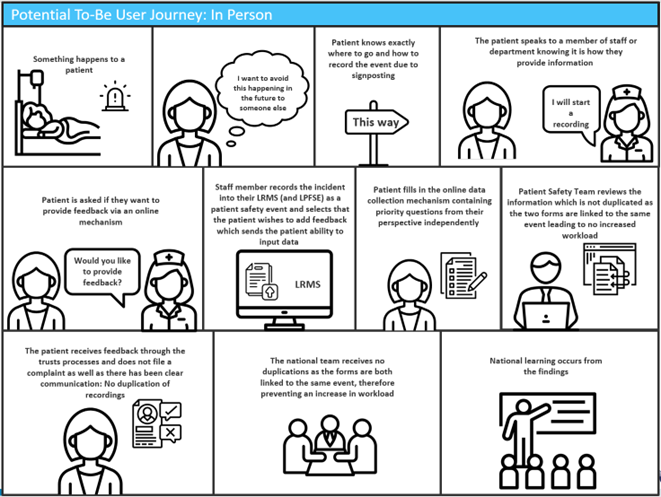
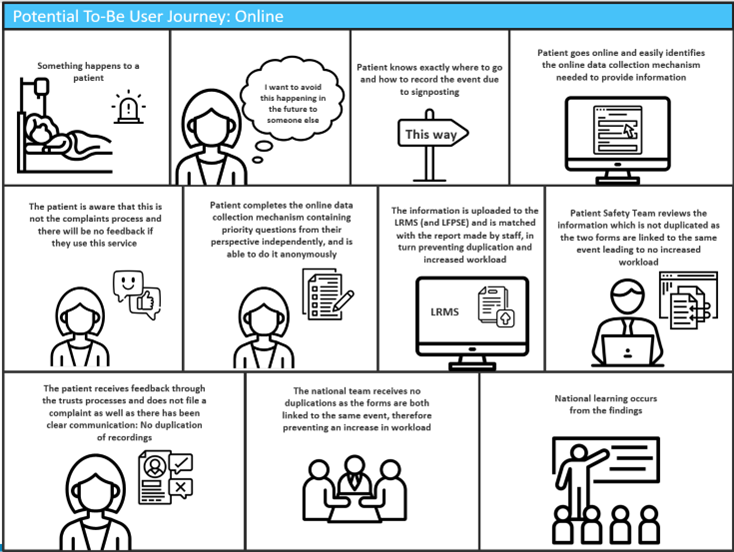
User Journey map: Potential future process
In-Person
Online
Glossary
| eForm | A website where you can fill in details online |
| FFT | Friends and Family Test: a survey given to patients after they have used NHS services, to find out about their experiences. |
| ICBs | Integrated Care Boards – NHS organisations in charge of developing a plan for meeting the health needs of the population, managing the NHS budget (money) and arranging health services. Each one looks after a different area of the country. |
| LFPSE | The Learn from Patient Safety Events service – a new system to collect information about things that sometimes go wrong in healthcare, to help the whole NHS learn from them and do things better. |
| LRMS | Local Risk Management Systems – computer systems used in hospitals to collect information about problems. They also sometimes hold other information, like complaints, staff details, and action plans. |
| NHS | The National Health Service |
| NHSE | NHS England. The part of the NHS which is in charge of the money, planning, and organising of the National Health Service in England |
| NRLS | The National Reporting and Learning System – the old system the NHS has used for around 20 years to collect information about things that go wrong. It is being replaced by LFPSE. |
| PALS | Patient Advice and Liaison Services. PALS offers confidential advice, support and information on health-related matters. They provide a point of contact for patients, their families and their carers. |
| Patient Safety | The science of understanding how and why things go wrong in healthcare, and how the NHS can work to stop them happening. |
| Patient Safety Event | Something that has happened in healthcare to make patients more or less safe, which we can learn from. This can be things that have gone wrong, things that might go wrong in the future, or things that have gone really well. |
| Patient Safety Incident | Something that has gone wrong in healthcare that could have or did make a patient more unwell. |
| Providers | NHS organisations that provide care to patients and service users. This includes hospitals, GP practices, dentists, pharmacies, and other kinds of healthcare. |
| Trusts | An NHS organisation providing care services for a specific area of the country. This might be a hospital, an ambulance service, or community services. One trust sometimes contains more than one healthcare provider or provider type. |
| UR | User Research – the process of talking to people who might want to use a certain service, to understand their views, experiences, needs and ideas., |
Publications reference: PRN00858

