Update from Sir Jim Mackey, CEO, NHS England
Introduction
Welcome to the first edition of The Month, a new publication taking a more in-depth look at key priorities for us all.
There’s a lot happening between now and the end of summer that will impact on the challenges we all face.
In particular, the 3-year Spending Review is to be published today (11 June) and the 10 Year Health Plan is working its way across government.
But there’s a lot we can be getting on with ahead of that.
The new team have been working on a 100-day plan since the beginning of the financial year – essentially working through how we re-set a whole range of stuff to support you to be able to more effectively drive change locally.
I wanted to share the plan with you so that you can think about how the changes that are coming might support you and your teams to do even more locally in the future.
You’ll also have seen the new Urgent and emergency care plan.
As Sarah-Jane Marsh says below, this is not just a urgent and emergency care (UEC) and secondary care challenge.
This is a challenge for us all, wherever we work.
All of this is, of course, linked to elective recovery, and Mark Cubbon sets out some more detail on the validation sprints and incentives below.
We’re adapting to new ways of working in real time and I’m grateful to all of you out there who have taken the time to work with the new team as we shift to a new – and very different – operating model.
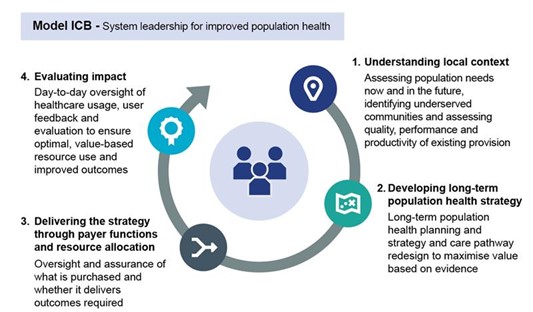
Some of the early work on the model integrated care board (ICB) has helped to set the bar for how we deliver change in the future and I look forward to continuing to work closely with many of you as we radically redesign ways of working to support you to be able to do more for your patients and your teams.
And finally, Penny and I look forward to meeting colleagues at NHS ConfedExpo this week.
The 100 day plan
We need to rebuild public trust in the NHS, restore confidence across government in how we manage our finances, and speed up the recovery of our services. Meeting this challenge means changing the way we work. Here’s how we plan to do it.
Working together better
At the heart of our 100-day plan is a reset in how we work together — across systems, regions, and the centre. We’re setting out clear roles and responsibilities, in an effort to build a new operating model – and more importantly, culture – built on trust and accountability, and creating the environment for improvement and innovation to thrive.
Our work on the Model ICB has been shaped with input from colleagues across systems and providers — those who know best what’s needed to drive real change. This collaborative approach will be our standard from now on.
Focusing on what matters most
As we change how we work, we also need to shift our focus—starting with the quality of care patients receive. We’re reviewing quality programmes across NHS England, the Department of Health and Social Care (DHSC), and the Care Quality Commission (CQC) to agree on a core set of indicators around safety, effectiveness, and patient experience. This will help us take a more joined-up, focused approach to improving care in ways that actually make a difference to patients.
We’re also simplifying how we measure performance — replacing 77 delivery metrics with a smaller, more targeted set of goals that everyone can rally behind.
Looking ahead to the next spending review, we want to move from annual to a three-year planning cycle. This will help us take a more strategic view of how we improve both operational and financial performance. This also means changing how we think about money — focusing on how we use our resources, and resetting our approach to productivity, linking efficiency directly to better outcomes for patients.
The upcoming 10 Year Health Plan will help reignite ambition across the NHS. But in the short term, delivering a better standard of urgent and emergency care this winter, and speeding up waits for elective care, will show we’re serious about change.
The new Urgent and emergency care plan sets higher expectations for leaders, and we’ll align our improvement efforts to support those ready to go further — helping the NHS regain its confidence and reputation as a high-performing, ambitious system.
Demonstrating urgency and accountability
The latest British Attitudes Survey shows public confidence in the NHS is at a record low. That’s a clear signal: we need to act — and fast. By this summer, we’re committed to delivering on the 12 key priorities below, with some already underway.
| Priority | Objectives |
|---|---|
| 1. Conclude the 2025/26 planning round | – finalise 2025/26 plans, stabilising finances and operations – align planning decisions with the Spending Review – reset approach across the NHS to drive accountability, develop local solutions and encourage ambition |
| 2. Medium-term planning and financial regime | – develop a medium-term plan approach that aligns with the 10 Year Health Plan – secure a new financial regime that guarantees sustainability and alignment with government objectives |
| 3. Oversight framework | – strengthen assurance and oversight functions while minimising duplication – balance local autonomy with clear accountability, using scheduled reviews to stay on track – combine existing improvement programmes into a single approach |
| 4. Quality refresh | – embed a stronger quality narrative throughout the NHS, informed by Dash Reviews – integrate quality metrics into the broader oversight and performance approach |
| 5. Productivity | – align NHS England’s productivity approach with government priorities – define metrics measuring efficiency gains that translate into improved outcomes – identify key work areas underpinning productivity in the NHS, covering estates, finance, improvement and workforce |
| 6. Winter preparedness | – ensure robust winter preparedness in line with the UEC Plan – improve patient flow and reduce waiting times, working closely with social care |
| 7. Capital investment model | – introduce an off–balance sheet capital investment mechanism – modernise estates and technology infrastructure, supporting the 10 Year Health Plan |
| 8. Digital, data and technology | – undertake a rapid review of current digital, data and technology (DDaT) programmes to maximise return on investment – ensure alignment with NHS priorities and the 10 Year Health Plan |
| 9. ICB cost reduction | – clarify roles of ICBs, through a ‘model ICB’ approach, and support rapid transition – demonstrate progress in merging or reorganising ICBs |
| 10. Integration programme | – coordinate the overarching integration programme – set out a clear NHS England – DHSC operating model and consider arm’s length bodies in the potential transfer of responsibilities from NHS England |
| 11. Establish new executive/transformation team and governance refresh | – establish a structured transformation team within the first 30 days – clarify leadership appointments to stabilise governance and ensure momentum – embed expected behaviours across NHS England’s executive team to encourage ambition and collaboration, reflected by the wider NHS – refresh committees and governance mechanisms across NHS England to ensure effective decision-making and accountability |
| 12. Performance management | – develop a proportionate, rules-based approach to performance management for operational performance, finance, quality and workforce targets |
Improving urgent and emergency care and the UEC plan
Sarah Jane Marsh, Urgent and Emergency Care and Operations Director
We all know we need to see rapid and urgent change to speed up recovery on the standards of care patients receive, and thereby improve public confidence in the NHS.
To meet this challenge requires a very different approach to how we work. If central directives were all it takes, we’d have fixed our problems by now. We know we need to reset the relationship between the centre and our NHS leadership community. Real change and results will only be delivered by leaders setting and driving the ambition locally, for their communities.
That’s what sits at the heart of the new Urgent and emergency care plan. Aligned to the 2025/26 planning guidance, the plan includes stretching performance targets and deliverables for the year ahead, with the aim of reducing unacceptably long waits for patients with both physical and mental health needs.
But unlike previous years, NHS England won’t be asking for a plethora of returns and assurance, and will instead be focusing on where we can best support you to deliver. How we work collectively to deliver this Plan is an important opportunity to show we can ‘walk the walk’ on the new relationship Jim has set out above. This isn’t about shifting responsibility – it’s about collective ownership. Every leader, every part of the system working together to deliver on clear targets and shared goals.
Neither is the plan a blank page. We’re asking NHS leaders to focus on and deliver specific improvements that will make the biggest difference; these aren’t arbitrary targets, they directly improve patient care and staff experience. The key ambitions and interventions are set out on the next page.
We are clear that this is not just a challenge for those working in UEC and acute settings. This is a challenge for us all, wherever we work, from primary, community and mental health care to the UEC front door, throughout hospitals, and with social care.
And we must not lose sight of the dependencies between UEC and routine care. Making winter 2025/26 significantly better than recent winters is as much about keeping up our momentum on driving down waiting lists as it is about improving quality and safety.
Your leadership is the single most crucial factor that will determine our success this winter, and whether our patients feel the difference. We must all ensure that, both at organisation and system level, everything possible is being done to improve care.
Where this was most effective last winter, chief executives, chief nursing officers and medical directors regularly worked from the emergency department to support staff on the frontline. This now needs to be the norm.
UEC plan – ambitions and actions
Our seven priorities
- Category 2 receive an ambulance within 30 minutes
- Maximum ambulance handover time of 45 minutes
- Minimum 78% performance against 4-hour A&E measure
- Reducing 12 hours waits to less than 10% of attendances
- Reducing 24 hour+ A&E waits for mental health admission.
- Tackling discharge delays
- Seeing more children within 4 hours
Key actions
NHS England and the Department for Health and Social Care will:
- Provide capital for urgent treatment centres (UTCs), same day emergency care (SDECs) centres, Connected Care Records, crisis assessment centres and mental health beds.
- Drive flu vaccine uptake among the public and staff.
- Improve the effectiveness of 111 and 999 services.
System winter plans should include:
- Local delivery approaches to increase vaccine uptake in all ages.
- How local partners are working together to identify and proactively support patients who are most vulnerable during the winter period.
- How NHS providers and local authorities will improve discharge and admissions avoidance.
- Implementation of the “Release to Rescue” standard.
- Actions to reduce length of stay in, and readmissions to, mental health beds.
- Expanded access to urgent care services at home and in the community.
ICBs will:
- Consider commissioning advice and guidance for parents.
- Ensure BCF capacity plans include appropriate capacity for surges over winter.
Acute trusts will:
- Set stretching local performance targets for daily pathway 0 discharges.
- Set an improvement trajectory towards achieving the 15-minute handover target.
Ambulance trusts will:
- Operate a call before convey principle, enable “see and treat” and reduce variation in rates of “hear and treat”.
- Provide urgent in-home care for clinically assessed patients, with follow-up services available the next day.
Recovering planned care
Mark Cubbon, Director for Elective Care, Cancer and Diagnostics
I am delighted to formally introduce myself as the National Director for Elective Care, Cancer, and Diagnostics.
As the Chief Executive of Manchester University NHS Foundation Trust, I have had the privilege of working alongside many of you as we work together to drive improvements in patient care and service delivery.
I am pleased to be working with you in this capacity as we apply a renewed focus on productivity, delivery, and the transformation of planned care pathways for patients.
Over the past three years, we have virtually eliminated two-year and 78-week waits, and a significant reduction in the number of patients waiting over 65 weeks in the past year.
This has only been possible thanks to the incredible efforts of many teams up and down the country.
Now, our focus shifts towards meeting the constitutional 18-week referral to treatment (RTT) standard of 92% by 2029.
We finished last year with 18-week performance just under 60%, and our plan is to reach 65% by March 2026.
Diagnostic performance has also improved — over six-week waits are down from 58.5% to 18.4% since May 2020 and diagnostic activity increased by 26% since 2021/22.
These improvements provide a strong foundation for securing further improvements, especially given the importance of diagnostics in meeting RTT and cancer targets.
The achievement of the first national milestone of delivering the aggregate RTT performance of 65% by March 2026 is dependent on all trusts delivering their planned levels of activity and performance improvements throughout the year.
At the same time, we will need to continue to ensure we reduce the number of patients who have been waiting the longest.
As we prepare for winter, we are asking you to do all you can to minimise the risk of your elective programme being impacted should we experience a difficult winter.
Many of you have factored this into your plans already, but where you have opportunities to do so, we are asking you to bring as much of this work forward into the first half of the year, while working within the same financial envelope.
I recently spoke to leaders to announce two new ways in which we can build on our existing efforts, to support further improvement across the year.
The first is by taking advantage of the new Q2 validation sprint, following the success of the work your teams have done since April.
The initial sprint has delivered excellent results, with more than 100k pathways removed from the list above baseline in just six weeks – meaning that priority can be given to those patients needing care.
The second sprint will start on 7 July and will be paid on the same basis as the April sprint.
We will share baselines with each trust next week and agree a plan for the improvement we collectively expect to see.
I am optimistic that the new sprint will deliver further encouraging results, reminding us of the importance of ensuring lists are regularly validated.
Secondly, I relayed the hugely positive news that we are launching a H1 capital incentive scheme (as trailed in the Elective reform plan), with £20 million available to be divided between the ten trusts which make the greatest improvement to their RTT performance between March 2025 and September 2025.
I am confident about the opportunities this will create and will share further details soon.
Finally, I look forward to sharing further updates on electives in due course, in addition to an increasing focus on cancer and diagnostics.
If there is anything that we do to support you in the delivery of your plans this year, please contact me directly on: mark.cubbon@mft.nhs.uk.
Working together better
Glen Burley, Financial Reset and Accountability Director, NHS England
Over my first few weeks in this role, I’ve been closely involved in the development of the draft Model ICB Blueprint, which marks a significant step in reshaping how ICBs operate across the NHS.
This work was co-produced between ICB leaders and NHS England, and I want to thank all those who have contributed.
Image text:
Model ICB – System leadership for improved population health
1. Understanding local context
- Assessing population needs now and in the future, identifying underserved communities, and assessing capacity, performance, and productivity of existing provision.
2. Developing long-term population health strategy
- Long-term population health planning and strategy, and care pathway redesign to maximize value based on evidence.
3. Delivering the strategy through payer functions and resource allocation
- Oversight and assurance of what is purchased and whether it delivers the outcomes required.
4. Evaluating impact
- Day-to-day oversight of healthcare usage, user feedback, and evaluation to ensure optimal, value-based resource use and improved outcomes.
We’ve mapped out which functions are essential to retain and which may be better transferred to other partners. This process is being supported by joint working groups with the Local Government Association and other stakeholders so we get it right.
Looking ahead, our immediate priority is reviewing the initial plans that ICBs have now submitted, to identify which systems need what support to refine and deliver their plans – including where they have decided this means clustering, and potentially merging.
Further engagement with partners is underway to refine the Blueprint and ensure alignment with the upcoming 10 Year Health Plan and anticipated health legislation – which we know will be necessary to complete many of the changes planned.
Alongside that work is continuing on how we bring together DHSC and NHS England and more clearly articulate the contribution that the centre and our regions make in support of systems and providers. And we have shared the draft NHS Performance and Assessment Framework with you for feedback, which will be central to how we interact and intervene in a transparent, rules-based way.
I recognise that this is a challenging process, to a challenging timeline. But my experience so far of working with system colleagues means I’m more confident than ever that together we can transition effectively to stronger ways of working, that places more autonomy back in local hands to innovate and improve care for our patients.
Other updates
In case you missed it
- National Quality Board position statement: remaining focused on quality in times of change and financial challenge
- Improvement framework: community language translation and interpreting services
- Action needed for delivery of routine mpox and gonorrhoea vaccination programmes 2025
- Changes to the online GP registration service in response to the Infected Blood Inquiry recommendations
- Patient safety healthcare inequalities reduction framework
- NHS very senior managers pay framework
- Consultation on the draft NHS Performance Assessment Framework
- Being fair tool: Supporting staff following a patient safety incident
- Climate adaptation resources
- Papers from NHS England’s May board meeting
Coming up this month
- 11 June – HMT Spending Review
- 11 and 12 June – NHS ConfedExpo – Join us in Manchester for the UK’s leading health and care conference, dedicated to driving innovation and improving care. To view details and book your place, visit the NHS ConfedExpo 2025 website
- 18 June – Health and Social Care Committee session on black maternal health
- 25 June – Health and Social Care Committee session on ADHD and autism diagnosis
- Ongoing: Regional medical roadshows – NHS England’s Medical Directors will be touring the regions over the coming weeks to meet trust and ICB counterparts. Details and invites will be shared directly with relevant colleagues.
- TBC: Publication of the Leng Review into medical associate professionals
- TBC: Learn from patient safety events dashboard goes live
- TBC: LeDeR Annual Report and Action from Learning report
- TBC: Update on the delegation of directly commissioned services
Your feedback matters. Our aim is to make these bulletins as useful as possible for you. If you have any feedback, please email england.leadersupdate@nhs.net.