Summary
The NHS operates over 1,500 directly managed hospitals as well as other treatment facilities, many of which operate 24/7, every day of the year. The occupied floor area of the NHS is 25 million square metres, which is the equivalent of 3,500 football pitches.
This estate and its related services are integral to the delivery of high quality clinical care. Therefore, it is essential that the NHS provides a safe, high quality and efficient estate. It is critical that no one of these three elements is delivered at the expense of the other two. The objective is to deliver a financially sustainable NHS that takes quality and safety as its organising principle.
As part of this, assurance is needed that appropriate actions and investment are taking place.
Assurance provides evidence and confidence for NHS provider boards and other interested parties that those actions needed to keep the NHS estate and facilities safe, effective, efficient and of high quality will actually occur.
The 2025 NHS Premises Assurance Model (NHS PAM) provides this assurance for the NHS and is a refreshed and updated version of the previous model. It reflects changes in policy, strategy, regulations and technology. The NHS PAM is kept updated to support this NHS Constitution right:
You have the right to be cared for in a clean, safe, secure and suitable environment.
In addition, the main benefits of the NHS PAM are to:
- allow NHS-funded providers of healthcare (NHS providers) to demonstrate to their patients, commissioners, staff and regulators that robust systems are in place to provide assurance that their premises and associated services are safe
- provide a consistent basis to measure compliance against legislation and guidance, across the whole NHS
- prioritise investment decisions to raise standards in the most advantageous way
- future iterations of PAM will help estates and facilities managers align with the wider objectives in the 10 Year Health Plan
Annex B provides a glossary of the terms used in this document.
If you have any queries related to this document, please contact us at: england.nhsPremisesAssuranceModel@nhs.net.
Annual updates (unless there is an urgent need to issue an earlier update) to the NHS PAM will be published on the NHS Collaboration Hub. We strongly suggest all users regularly visit the hub for these updates, especially during the completion of their NHS PAM. If you are not registered for the hub please email england.efmportalsubmissions@nhs.net to request membership. Annual changes to the self-assessment questions (SAQs) may be required in line with updates to guidance and legislation. You can find an overview of the latest changes in the instructions tab of the SAQ Excel workbook.
NHS PAM 2025/2026
1. The NHS Premises Assurance Model (PAM) is updated annually to:
- reflect feedback from users, in this case from the 2025/26 collection
- incorporate amendments identified by the NHS PAM User Group
- incorporate changes to the strategy for the NHS estate as set out in relevant guidance.
2. Please note the following points specific to this update:
- The 2025 NHS PAM has been updated to reflect changes to guidance and other policies that have been issued since 2025 and before 31 March 2026. Changes after that date can but do not need to be reflected in a trust’s completion of the NHS PAM. Updates are reflected on the instructions screen of the NHS PAM which can be found within the live version on the portal.
- While the NHS PAM has been updated to reflect changes to guidance and other matters, we have sought to maintain consistency between each NHS PAM issue to allow year-on-year comparison of trust scores.
- Integrated care boards (ICBs) were created on the 1 July 2022 and are partnerships of organisations that come together to plan and deliver joined up health and care services, and to improve the lives of people who live and work in their area. This includes responsibility for the appropriate use of the NHS estate in their area. As such, they will need to have access to the NHS PAM data and analysis. Therefore, they will be included in the development and reporting of the NHS PAM going forward. Data submitted by trusts within PAM will be shared with the ICBs for them to use as appropriate.
Background
3. We have developed the NHS PAM to provide a nationally consistent basis for assurance for provider boards on regulatory and statutory requirements relating to their estate and related services, and this NHS Constitution right:
To be cared for in a clean, safe, secure and suitable environment.
4. This assurance can then be used more widely and be provided to commissioners, staff, regulators, the public and other interested stakeholders.
5. The NHS PAM bridges the space between NHS boards and the operational detail of their day-to-day estates and facilities operations. The model can be used as a prompt for further investigation, and to stimulate better-informed dialogue as to how the premises can be used more efficiently, managed more effectively and best contribute to the overall strategic objectives of the organisation.
6. In creating the NHS PAM there is no intention to disadvantage any organisation in any way. We welcome comment from organisations and individuals across the healthcare sector, as well as private and charitable organisations and the public, regarding the development of the NHS PAM, so that it continues to deliver a consistent level of assurance and performance improvement across estates and facilities services.
7. The NHS PAM is held and maintained by the NHS Estates and Facilities Team at NHS England. A user group comprising NHS trusts, regional colleagues, the Care Quality Commission (CQC) and other users oversees changes to the NHS PAM such that it continues to minimise problems for the NHS.
Before you start using the NHS PAM
8. Annex A details the six-stage approach adopted by one NHS provider that has embraced the use of the NHS PAM:
- set up
- assessment preparation
- NHS PAM self-assessment
- organisation feedback and reporting
- monitoring and peer review
- annual reassessment.
We recommend NHS trusts read this as it includes many key pointers based on actual experience. We also recommend they read the frequently asked questions below.
9. The NHS PAM is not currently applicable to primary care providers, e.g. general practices and dental practices, or to organisations providing social care services only and any element of social care provision by NHS trusts.
10. NHS providers are encouraged to join regional networks through such bodies as the Healthcare Estates and Facilities Management Association (HEFMA) and Institute of Healthcare Engineering and Estate Management (IHEEM). These bodies work hard to promote a consistent approach to NHS PAM, assist with learning and the sharing of best practice, and establish networks for peer review.
Using the self-assessment questions
11. The NHS PAM self-assessment questions (SAQs) are grouped into five ‘domains’, with a separate section for helipads, FM Standard Maturity Framework and contacts:
- safety (hard and soft)
- patient experience
- efficiency
- effectiveness
- organisational governance
- helipads (where applicable)
- FM Standard Maturity Framework
- contacts
These are then broken down into individual SAQs, and into further questions known as ‘prompt’ questions. The model is completed by scoring the prompt questions under each SAQ.
12. The first four domains cover the main areas where estates and facilities impact on safety and efficiency. The organisational governance domain acts as an overview of how the other five domains are managed as part of the NHS provider’s internal governance. Its objective is to ensure that the outcomes of the domains are reported to the provider boards and embedded within internal governance processes to ensure actions are taken where required.
13. The SAQs cover all the major areas where NHS estates and facilities impact on safety and clinical services. However, we recognise that some of the questions may not apply to all NHS trust and site types. Therefore, individual SAQs and individual prompt questions can be identified as ‘not applicable’. The rationale behind this decision should be noted in the free text fields. Each domain has a worksheet within the SAQ Excel workbook, as well as an individual results worksheet.
14. The Maturity Framework is an additional section which was requested by the Cabinet Office. Full instructions on how to complete this are available within the SAQ spreadsheet. An overview is attached as appendix E. For those Trusts who complete this section reporting will be available on this within Tableau.
15. Each domain includes a list of the SAQs and against each SAQ are the prompt questions that need to be rated using the ‘drop down’ menu for the following scale:
- Not applicable: this prompt question does not apply to your organisation/site or is not applicable by virtue of the responses given in the other prompt questions, e.g. there will be different responses to SAQs based on whether mental health or acute services are provided on the site.
Care needs to be taken in using this response, as failure to apply it properly can lead to significant issues, especially in respect of the safety domain – eg a small amount of mental health services may be provided on a mainly acute site. Information on why this response applies should be recorded in the comments column. - Outstanding: compliant with no action required, plus evidence of high quality services and innovation.
- Good: compliant, no action required.
- Requires minimal improvement: the impact on people who use services, visitors or staff is low.
- Requires moderate improvement: the impact on people who use services, visitors or staff is medium.
- Inadequate: action is required quickly – the impact on people who use services, visitors or staff is high.
A scoring criteria matrix is provided at Annex C with examples of how each of these ratings can be interpreted.
16. The scores/ratings on individual prompt questions are averaged to produce a rating for the SAQ and in turn the SAQ ratings are averaged to produce a rating for the domain. The NHS PAM ratings cannot be a definitive indication that a service/organisation/site is safe and meets all its legal obligations, but they do provide a structured basis for greater transparency and discussion of the NHS provider’s own view of compliance.
17. In rating/scoring the prompt questions, users should consider the content of the following in the SAQ Excel workbook:
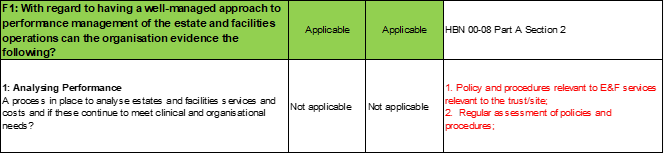
Evidence should demonstrate:
- policy and procedure relevant to E&F services relevant to the Trust/site
- regular assessment of policies and procedures
- business plans
- space utilisation studies and monitoring usage
- response to NHS Long Term Plan of reduction to 30% non clinical space
- market testing and cost benchmarking of contracts
- land and property sale receipts
- commercial strategy or agreements such as letting of space for retail use
- relevant guidance and legislation (links are detailed within the SAQs):
- Developing an Estate Strategy document
- Health Building Note 00-08
- Health Building Note 00-08: Land and Property Appraisal
- Strategic Health Asset Planning & Evaluation (SHAPE) tool
- RICS UK Commercial Real Estate Agency Standards.
- RICS Guidance Notes- Real Estate disposal and acquisition.
- Assets in Action
- Monitor: The asset register and disposal of assets: guidance for providers of commissioner requested services
- Monitor: Strategy development: a toolkit for NHS providers
- Monitor: Developing strategy What every provider board member should know
18. The evidence column contains the expectation that the ‘approach’ – as in the policies, procedures, working practices, etc – is understood, operationally applied, adequately recorded, reported on, audited and reviewed. NHS providers should satisfy themselves that they can demonstrate this is the case if asked to do so. The column also provides a non-exhaustive list of what may constitute relevant evidence.
19. The evidence should demonstrate that any relevant legislation and guidance listed against the SAQ complies with the policies, procedures, etc. Again, the legislation and guidance listed should not be considered exhaustive, with guidance such as health technical memoranda (HTM) and health building notes (HBNs) providing a more definitive list of guidance and legislation relevant to that SAQ than is listed in the NHS PAM. Most relevant guidance, including estates and facilities guidance, is available from health technical memoranda.
20. The capital cost of achieving compliance provides the link to the trust’s estates strategy, business plan and budget. The intention is that any capital cost associated with reaching compliance can be identified against individual areas, and will give additional granularity to the NHS provider’s three- and five-year plans.
21. The SAQ Excel workbook has the option to select two financial years as a basis for comparison, though reporting on the spreadsheet is currently limited to one year. This can be used in two ways: to look back historically and chart the progress from a previous assessment; or to chart an action plan for the organisation. The latter is particularly useful if used in conjunction with ‘capital cost to achieve compliance’ data so that the impact of the investment can be illustrated. For clarity, costs already agreed as part of programmes/training budgets/staffing, etc do not need to be double-counted in PAM, and the costs here are a ‘last chance’ to identify any unallocated compliance costs to the board.
22. The revenue consequences of achieving compliance is an optional field. We suggest it can be used to provide additional granularity to the revenue figures that the NHS organisation provides in the annual Estates Return Information Collection (ERIC). User notes is a free text field, but we suggest users give any further explanation of their ratings and details of where the evidence is stored and available, if required. The user notes cell within the Excel file can be ‘split’ or ‘merged’ to suit the user’s needs – eg splitting the cell allows users to include a separate entry against each prompt question.
Frequently asked questions
1. Legal questions
Q1.1 How confidential is the information that I am inputting into the NHS PAM?
Trusts will decide locally who to share the NHS PAM SAQ responses with. However, with the online version, NHS England will be able to analyse the data provided by trusts, to provide national information on the completeness of data and areas of concern.
Regulation 43 of the PCR imposes a duty of confidentiality on commissioners in relation to the information provided by bidders/contractors that has been designated as confidential. Therefore, any SAQ information that a provider designates as confidential and that is shared with a commissioner as part of a tender process will, by law, remain confidential.
Individual NHS providers may choose to make SAQ results available to regulating authorities. Regulators may also request SAQ results from individual NHS providers. It is important to note that the statutory obligation for public bodies to comply with the Freedom of Information Act 2000 overrides any contractual duty of confidentiality, except where such compliance breaches the commercial confidentiality of the owner of the information to be disclosed.
As part of the ongoing work of NHS England, completed NHS PAM SAQs may be examined as part of the discussion regarding the NHS provider’s situation.
NHS England may share the reporting outcomes (based on the data submitted by trusts) more widely to support policy and operational development.
The information will be shared with ICS leads so that they can work with trusts within their local area to replicate best practice or support Trusts where required. The information may also be used by the National team within reports.
Q1.2 Who owns the NHS PAM?
The NHS PAM was developed by the NHS with support from the Department of Health and Social Care. The model is managed, developed and may be licensed by NHS England. The intellectual property rights to the NHS PAM software are owned by NHS England.
Q1.3 Will the NHS PAM be accessible to the general public?
The blank NHS PAM is readily available to the general public through the NHS England website. Once completed by yourselves, you will be responsible for any publication or sharing of it.
Q1.4 Does the NHS PAM override any other trust legal responsibilities?
No.
Q1.5 Can I modify or change the NHS PAM?
You should not change the structure or questions in the NHS PAM as it will then not be consistent nationally. However, the NHS PAM is intended to be a ‘living’ document and as such should be updated to reflect any changes that impact on the self-assessment. We recommend that you keep it under at least quarterly review.
Q1.6 Are there any intellectual property or data protection issues?
The intellectual property rights to the NHS PAM software are owned by NHS England. The Data Protection Act applies only to personal data (people), and therefore does not apply in the case of the NHS PAM. Patents will also not apply to the NHS PAM. When the NHS PAM is made available for completion and use on the internet it will be copyrighted to NHS England and will also be subject to its own terms and conditions of use.
Q1.7 Are there any Freedom of Information issues?
NHS providers are bound to meet individuals’ requests for information in the same way as any other public body under the Freedom of Information Act 2000.
The Re-use of Public Sector Information (PSI) Regulations 2005 (SI 2005 No 1515) also allow members of the public to apply for information provided under the Freedom of Information Act 2000. The PSI regulations govern how the information can be re-used. Responding to a Freedom of Information request does not confer an automatic right of re-use. Re-use raises copyright and licensing issues that usually require permission from the copyright owner.
Q1.8 Are there any implications for users on self-assessment/self-declaration?
Self-declaration is where an individual or representatives of an organisation sign off a document to say that the contents are correct to the best of their knowledge. Problems occur when information is incorrect, and the degree of inaccuracies can affect the outcome of the process. The NHS PAM SAQ responses are not legally enforceable.
Q1.9 Will the NHS PAM apply to NHS foundation trusts and independent sector providers?
The self-assessment element of the NHS PAM is designed to apply to all NHS providers including foundation trusts and independent sector providers.
Q1.10 Are there any issues around self-incrimination?
There are no legal implications for self-incrimination associated with the NHS PAM, as it is a management tool and non-compliance is not a criminal offence. NHS England can give no assurance on the status of individual elements within the NHS PAM, and any queries regarding these should be pursued with the relevant body (Health and Safety Executive, etc).
2. Use of the NHS PAM
Q2.1 What are the restrictions of use for the NHS PAM?
The NHS PAM is intended as a universal and consistent model for use by all NHS providers, including acute, mental health and independent sector providers. Primary care organisations, including general practices and dental practices, are not covered by the NHS PAM as it has not been developed to incorporate their facilities/services.
Q2.2 Who in the trust should complete the NHS PAM?
While the NHS PAM is targeted at estates and facilities staff, the relationship between estates and facilities and other operational areas, including clinical, is critical. Therefore, it is important that other staff are involved in completing the NHS PAM to ensure that a full understanding of the risks identified by the NHS PAM is obtained.
Q2.3 How will areas identified as needing action/work be handled?
An important function of the NHS PAM is to identify where actions are required. These actions may involve changes to systems or investment in buildings or new equipment. Analysis of the outcome of the NHS PAM should be undertaken and an action plan compiled. This should then be implemented through the estates business plan for future years.
These areas will be analysed by NHSE, via reporting mechanisms. It is expected that reporting will be created by NHSE based on the PAM findings and shared to offer support, encourage improvement and share best practice.
Q2.4 Do I need to involve my integrated care system (ICS)?
Given the importance of the NHS estate to the provision of high quality clinical care and the importance of the relationship between trusts and their ICS, we suggest that trusts provide it with the outcomes of their annual NHS PAM board report. In addition, specific issues identified by the NHS PAM, where appropriate, should be raised with the appropriate local organisation to support decision-making. Going forward, we will centrally seek to include the ICSs in the development and reporting of the NHS PAM.
Q2.5 How does use of NHS PAM provide assurance on the safety and suitability of estates and facilities services?
The way in which the self-assessment is undertaken and its findings subsequently adopted locally will greatly influence the level of assurance that can be drawn from the use of the NHS PAM.
Annex A describes steps that help ensure the self-assessment is robust in the first instance. By its nature the organisation governance domain will, in part, provide an indicator of assurance as this measure supports the extent of board oversight of estates and facilities issues. Following the self-assessment assurance will be increased by:
- embedding the NHS PAM compliance framework in job descriptions, training, and roles and responsibility
- board review and agreement of the NHS PAM assessment
- scrutiny by and dialogue with commissioners on the NHS PAM assessment
- scrutiny of the NHS PAM by NHS England (where relevant)
- the level and role of audit in the NHS PAM process
- if the NHS PAM has formed the basis for a CQC inspection
- if the self-assessment, or parts of it, has been independently verified or peer reviewed
- the level to which the self-assessment is consistent with patient feedback.
Q2.6 How does the NHS PAM relate to the NHS Constitution, ‘fundamental standards’ and CQC requirements?
The NHS constitution includes the “right to be cared for in a clean, safe, secure and suitable environment”. Moreover, the NHS Constitution Handbook goes on to say:
“In practical terms this means that in addition to complying with specific legal requirements that are set out in health and safety legislation and the law relating to negligence, healthcare providers should:
- have robust assurance arrangements in place to provide and maintain high standards of safety, security and suitability for their premises and equipment at all times
- make sure that organisations and individuals with responsibility for the safety of premises and equipment are appropriately governed, adequately trained and qualified, apply the correct protocols and follow best practice guidance.
This right is based on the specific fundamental standards of safe care and treatment, premises and equipment, set out in regulation 15 off the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014”.
The NHS PAM is a means for providers to ensure they “have robust assurance arrangements in place to provide and maintain high standards of safety, security and suitability for their premises and equipment at all times”.
The CQC is working closely with NHSE to ensure that they have sight of any organisations which do not submit so that this can be added to a risk register and monitored.
Q2.7 Is the NHS PAM endorsed and used by regulators?
A recurring question is how using the NHS PAM will assist with CQC inspections relating to estates and facilities services. A key reference point for the CQC is the estates and facilities standards and requirements in the Health and Social Care Act 2008 (Regulated Activities), Regulations 2014and the CQC guidance for providers on meeting these regulations. Additionally, providers will have to meet requirements of other enforcement bodies and regulators.
The CQC are making updates including the way in which audits/inspections are completed, next year any changes made by the CQC will be considered for PAM.
The NHS PAM captures these estates and facilities standards and requirements and breaks them down into a series of SAQs covering specific technical areas, eg water safety and electrical safety. This provides a structured framework to self-assess and measure compliance with each of the requirements.
Ultimately it is up to regulators how they conduct their inspection, but a robust NHS PAM assessment and resolution of any issues identified will put the organisation in a strong position to demonstrate estates and facilities’ compliance.
The SAQ workbook includes a sheet that cross-references the requirements in the above legislation and CQC guidance with the relevant parts of the NHS PAM.
Further details on ‘compliance of the estates’ and the use of the NHS PAM can be found in Health Building Note 00-08 Part A: Strategic framework for the efficient management of healthcare estates and facilities.
The NHS PAM has been endorsed by the Institute of Healthcare Engineering and Estate Management (IHEEM) and the Health Estates Facilities Management Association (HEFMA).
Q2.8 How will it be approved within our organisation once it is completed?
The completed self-assessment should be formally presented to your board for review and approval. This approach is advised if you intend to use it as evidence for the CQC or another external stakeholder organisation. Additionally, several committees may need to be consulted before presenting it to your board, e.g. finance.
When the action plan resulting from the NHS PAM assessment will be presented to the board needs to be considered.
The board can decide whether it wishes the completed NHS PAM to remain private or be made available in the public domain, but openness in line with government policy on transparency is advocated.
Local ownership of the completed NHS PAM is important; otherwise no action or advantage will be obtained from using it. We would expect that once completed, it – or an appropriate extract of it – is formally presented to your board for approval. If your board wishes to delegate approval of the NHS PAM to another group or individual it can. However, responsibility for the completeness, accuracy and implementation of any actions identified from the NHS PAM remains with the board. We suggest that when approved outside the board, it should still be circulated for information to the board, especially so that non-executive board members can review it. This approach is advised if you intend to use it as evidence for the CQC or another external stakeholder.
The board can decide whether it wishes the document to remain private or be made available in the public domain. However, this should be in line with government policy where openness and transparency is advocated. We do not collect completed NHS PAM workbooks, though feedback on their content, format and presentation is always welcome.
Q2.9 How should contracted out services or accommodation provided by organisations other than the trust itself, e.g. PFI or NHS Property Services, be treated?
All the SAQs are relevant regardless of who provides a particular service/area, and how it is provided. Where services are contracted out, the organisation should work with its contractors to ensure that the management of all such contracts is consistent with existing guidance and standards and seeks the necessary assurance and evidence to support the self-assessment.
This includes all forms of contracting out, by whatever type or name it is called, including PFI, NHS Property Services, Community Health Partnership, joint venture and local authority sites, and where the trust has transferred all or part of its services to a 100%, or otherwise, owned subsidiary. Such organisations should not complete the NHS PAM for the facilities and services they manage. However, they should provide information so that the contracting-out organisation can effectively complete the NHS PAM for these sites.
Q2.10 How are trust mergers/re-organisations handled?
Ideally all trusts should have completed NHS PAMs. For the first year post-merger, they can combine these NHS PAM reports, and then in subsequent years prepare a single report. Trusts may wish to analyse the differences between the pre and post-merger approaches to NHS PAM completion and provide this with the post-merger report to promote clarity of understanding.
Q2.11 Do I need to involve departments other than estates?
The NHS PAM covers both hard and soft facilities management services and it is ultimately about measuring compliance and providing assurance on these areas. You also need to seek the views of the hospital staff who use the estate and its facilities. We recommend a multidisciplinary approach.
Q2.12 Which of our services/sites/facilities/buildings/hospitals is it going to apply to?
Consider how multiple sites will be assessed. Aspects of the assessment may apply across all sites, e.g. policies and procedures, but some are likely to require a site-specific assessment, particularly for the safety domain. Also, if your organisation owns and manages the sites in question or leases them, this may also dictate if part of the assessment is required at site level.
Consistency will also be more of an issue with multiple sites and operational teams. You should record any services or buildings not covered by the assessment and the reason they have been excluded.
If all your estate is not being covered, then this needs to be stated explicitly to your board to avoid misunderstandings. In addition, the reasons for its lack of applicability needs to be recorded to allow users of your completed NHS PAM to understand its limitations.
Q2.13 When will the NHS PAM be undertaken and over what timeframe will it apply?
It is mandatory that the NHS PAM will be updated annually and approved by the trust’s board. The timing of completion of the NHS PAM is important as it needs to fit the internal management process of the NHS organisation concerned to ensure that, for instance, the actions that result from its use are included in operational, financial and strategic plans.
It is also recommended that the model is updated to reflect any changes to operational procedures, changes in legislation or how services are provided eg outsourcing. A light touch quarterly review may be appropriate followed by a more comprehensive yearly review/reassessment.
The timing of completion of the NHS PAM is important as it needs to fit with the internal management process of the NHS organisation to ensure that, for instance, the actions resulting from its use are included in operational and financial plans. However, problems with local NHS estates and facilities can occur at short notice. Therefore, regular reviews of areas of risk may be required.
Q2.14 How long will it take to complete the NHS PAM and what are the resource implications?
This depends on the size of the NHS provider, its estate and where it is starting from in terms of compliance, and these features will determine the resources the trust will need to complete the assessment.
Most of the information and evidence will be held within the organisation. It is a matter of assessing and cross-referring this against the NHS PAM structure. For NHS providers with good systems in place to demonstrate compliance, completing a PAM assessment will be more a co-ordination and consistency exercise. For those that do not, the process will require a more detailed review of their compliance systems and processes.
The safety domain is the largest and therefore the most time consuming of the domains to complete.
Once the initial assessment has been conducted and any improvements to processes and procedures undertaken, maintaining and reassessing the NHS PAM will be considerably less time consuming. The aim should be to embed compliance in individual roles and ultimately the organisation structure.
After having worked to complete the NHS PAM in the first year, we anticipate that future resource input will be minimal. NHS providers will subsequently review and update their existing NHS PAM results using and inputting data and information that they already have available or collect.
Q2.15 How does the NHS PAM rating/scoring system align with the CQC rating system?
The NHS PAM 2025/26 uses the same rating system as the NHS PAM 2014. This is broadly comparable to the CQC’s approach to inspecting and rating care services, which is based on a four-point rating system as follows:
- outstanding
- good
- requires improvement
- inadequate
The NHS PAM uses the same rating system apart from using two levels of ‘requires improvement’:
- requires minimal improvement: the impact on people who use services, visitors or staff is low
- requires moderate improvement: the impact on people who use services, visitors or staff is medium.
The NHS PAM working group felt that splitting the ‘requires improvement’ rating in this way would help NHS providers prioritise improvements.
The ratings provided by the NHS PAM cannot be a definitive indication that a service/organisation/site is safe and meets all its legal obligations. The CQC will review a range of evidence and indicators in addition to its own professional judgement when confirming a rating at hospital or service level.
Q2.16 How does the NHS PAM link with operational management of estates and facilities services?
Operational management, health and safety, and assuring compliance are all inter-linked and overlapping activities. Ensuring estates and facilities services are safe and comply with relevant legislation and guidance is a key part of an organisation’s governance, and a necessity for a sound and efficient operational management.
Q2.17 Should I undertake peer review of our NHS PAM?
Undertaking a peer review of a completed NHS PAM will identify potential issues with its completion and promote consistency nationally across the NHS. However, peer reviews can be resource intensive and therefore consideration needs to be given to the value of undertaking a peer review every year.
Q2.18 What is suitable evidence?
We do not believe in assembling evidence unless there has been a clear instruction to do this, e.g. requested by the CQC as part of pre-inspection intelligence. The NHS PAM assessment should reflect the operational reality. Therefore, evidence should be easily accessible from operational systems if needed.
The main pieces of evidence can be readily inferred from the individual prompt questions. Suggestions are provided. However, these need to be considered locally in terms of existing systems and processes.
Evidence should demonstrate the approach (policies, procedures, etc) is understood, operationally applied, adequately recorded, reported on, audited and reviewed. Staff should be able to demonstrate that they are aware of a particular policy/procedure relevant to their roles and responsibilities. In addition, maintenance records, test certificates, building certificates, safety reports, audits and training plans are all relevant.
Q2.19 How do I cost the actions that need to be taken as a result of the NHS PAM?
Capital investment, including VAT, fees and decanting costs, should be calculated based on implementation at the earliest practical opportunity. Revenue costs should be calculated, including estimates for inflation, for the period until the identified issue will be mitigated. These costs should be those not already planned, approved and budgeted for in the organisation’s accounts and financial systems – that is, they represent extra resources not yet available.
If you are not able to cost an SAQ you should mark this as not applicable.
Q2.20 What do I do with the costs of implementing the actions identified in the NHS PAM?
These costs should be provided to the provider board with the NHS PAM report to allow it to understand the costs of action and the financial consequences of not undertaking them. Where such actions are agreed, the related costs should be included in future budgets to fund the agreed actions. Where actions are not agreed, the capital costs not committed to should be included in backlog maintenance and critical infrastructure risk figures.
Q2.21 How should I report NHS PAM scores where there is a significant difference between scores for different sites?
NHS organisation with multiple sites can have different scores for the same SAQ. The overall NHS PAM score for the trust needs to reflect these differences, while providing an accurate assessment of the organisation’s situation to users of reports based on it. The approach will need to differ to reflect the relative importance of the sites being considered, the SAQs involved and the size of the differences between scores. The different scores should be mediated to reflect the situation most accurately. In some cases, it may be best to report an average score. However, for safety-related SAQs, reporting the lowest score may best reflect the importance of the risks involved and the need to mitigate them.
Q2.22 I would like to feedback my experience and comments on the NHS PAM. How do I go about this?
Comments and feedback are welcome. Please send all comments and feedback to england.nhsPremisesAssuranceModel@nhs.net.
Annex A: Suggested six stage approach to undertaking the self-assessment and post-assessment using the NHS PAM
This case study, provided by Jacqui Grimwood, Estate Development Manager, West Suffolk NHS Foundation Trust, describes the trust’s experience of and approach to adopting the NHS PAM.
Stage 1: Set-up
1.1 Existing compliance process
NHS providers that use the model have found it beneficial to focus initially on their current processes for estates and facilities compliance. Comparing their approach with the NHS PAM allows the organisation to identify strengths and weakness in their current processes.
Existing compliance processes can underpin the requirements of the NHS PAM and have synergy with the safety domain but do not always extend to the other four NHS PAM domains. Therefore, the NHS PAM is still likely to be beneficial even where robust compliance systems are considered to exist. Where the organisation feels its current approach is sound and comprehensive, this can be explained and cross-referred to in the relevant parts of the NHS PAM. NHS providers may alternatively wish to adopt the NHS PAM approach in its entirety to address significant weaknesses in their current processes. Understanding where the organisation currently is in relation to compliance will provide a good indication of the time and resources needed to conduct the NHS PAM assessment.
1.2 Trust sign-up to process
Trust buy-in
Senior managers and directors whose responsibilities are covered by the NHS PAM should be committed and signed up to the process before starting any work.
Organisation board and committee interface
The level of board oversight and scrutiny of the self-assessment is a key part of the level of assurance that the NHS PAM model will provide.
Engaging with the NHS provider board and relevant committees at an early stage is recommended. Identifying a board member willing to champion the model would be advantageous. This should also assist in presenting the self-assessment findings and proposed action plans to the NHS provider board and relevant committees later in the process.
1.3 Agree format and process
Agree process/approach
The organisation can use the process/approach described in this guide and supplement/amend it based on local circumstances. Defining and agreeing the approach at an early stage helps ensure a consistent and robust self-assessment process.
Produce a draft plan
An initial plan should be produced that identifies the key dates and the process/ approach to be followed. This may include roles and responsibilities, organograms, governance and reporting arrangements, an indicative timetable and who will be involved.
Patient involvement
The NHS provider’s current processes for patient involvement are part of the NHS PAM self-assessment. Additionally, patient feedback is a key part of the evidence to consider when undertaking the self-assessment and as such you should expect consistency between the two.
Additional patient involvement in the NHS PAM self-assessment is recommended to add robustness. This is particularly true for the patient experience domain. It is recognised that some parts of the model cover complex technical areas for which active patient input is impractical.
1.4 Identify leads and specialist experts
The NHS PAM is split into five domains and will involve people from across the organisation. Each domain should have a nominated lead to own and drive that part of the self-assessment. There may also be the need to identify specialist experts to take ownership of individual self-assessment questions, particularly within the safety domain due to the diverse range of technical areas covered.
Early adopters of the model have embedded the standard NHS PAM compliance process in job descriptions and staff roles to promote ownership and consistency.
1.5 Briefing
It is important to brief nominated leads and specialist experts to ensure a common understanding and promote consistency. This can be best achieved by means of a single group briefing session where possible.
The briefing should include:
- overview of agreed process
- mechanics of the self-assessment
- assembling/availability of relevant evidence
- assembling/availability of relevant guidance
- assembling/availability relevant policies/procedures/working practices
- links between policies, guidance and evidence
- workshop planning/format
- scoring.
Stage 2: Assessment preparation
2.1 Evidence
A fundamental part of the NHS PAM assessment is being able to produce suitable evidence that supports the NHS provider’s self-assessment. This evidence is what the CQC is likely to scrutinise during any inspection. It is expected that this evidence will be the NHS provider’s everyday policies, procedures, working practices and records, etc relating to estates and facilities services.
As a general principle the approach defined in these Policies, Procedures and working practices should demonstrate they
- comply with relevant guidance and legislation
- are understood
- operationally applied
- adequately recorded
- reported on
- audited and reviewed.
2.2 Review PAM domain self-assessment and prompt questions
Rating/scoring the actual self-assessment questions/prompt questions can be done in two distinct stages:
- Before the workshop (see stage 3), leads may want to undertake a pre-workshop assessment and use this as the basis for discussion and challenge at the workshop. This approach will be particularly relevant for the safety domain that requires considerable specialist technical knowledge.
- It is recommended that the rating/scoring is formally agreed in a workshop, particularly where input is required from across a variety of areas of the NHS provider. Experience suggests this leads to a far more robust and transparent assessment.
It may be appropriate to break the safety domain down into several smaller workshops or plan it over a few days. This will be influenced by the individuals involved with the relevant SAQ areas and the type and level of challenge you wish to bring to the process.
2.3 Source and print reference documents
The leads will need to consider the relevant evidence and documentation that will be reviewed and considered at the workshop.
It is advisable to have a trial run of some SAQs ahead of this to help define what documents are considered relevant, again to promote a consistent approach.
Consider demonstrating how the current practices comply with relevant legislation and guidance and if there is a consistent understanding across the organisation.
2.4 Evidence storage
The NHS PAM assessment covers a broad range of areas. Most of the evidence supporting the self-assessment will be held in the NHS provider’s existing operational processes and systems.
The evidence is not stored in the NHS PAM SAQ Excel workbook. Instead the workbook ‘notes’ column is used to identify the relevant evidence, where it is stored and its accessibility. It is particularly important to be able to access the relevant evidence in the case of a CQC inspection. Evidence will also need to be available during the scoring workshop.
Some NHS providers have found it beneficial to set up a central NHS PAM evidence repository to facilitate ease of access. This is an individual NHS provider’s choice with ease of access and managing changes and updates to the evidence being key considerations.
Stage 3: NHS PAM assessment
3.1 Domain workshops
A separate workshop for each domain has proved effective in producing an honest, transparent and robust assessment. It is considered beneficial to hold the governance domain at the end.
The safety domain is the largest domain and brings together a diverse range of technical areas. It is unlikely that all of them can be covered in one workshop is unlikely. The domain could be split and covered in two or three separate sessions. Look at the individuals involved against specific safety SAQs – this may indicate have the domain can be divided.
At the workshop relevant leads should present their pre-assessment and explain their rationale for arriving at the proposed rating/score. They should present the relevant evidence and explain how this links to the question and their proposed rating.
The workshop should encourage an open discussion where people can challenge the rationale and rating. This is not intended to catch people out but to help ensure the assessment is robust, accurate, transparent and open to scrutiny.
Any relevant notes on discussions and agreement can be added to the free text cells in the NHS PAM workbook.
3.2 Action plan
Most NHS PAM assessments will lead to at least some actions. These should be detailed and noted as you go through the domain workshop. Actions can be relatively straightforward, eg updating policies, through to those requiring significant investment. Actions may also need to be included in risk management and business planning processes where relevant.
3.3 Agree action plan
Agreeing action owners and allocating responsibilities and timescales for actions is essential to provide clarity on how actions will be taken forward and concluded, and should be agreed at the workshop.
3.4 Identify evidence and collate
The relevant evidence will have been collated and discussed during the workshop. It is sensible to review this in light of the workshop discussions, and to note any changes that have been made as a result.
3.5 Store evidence in a repository
Any alterations to the evidence should be reflected in the evidence repository, where relevant, for completeness.
Stage 4: Organisation feedback
4.1 Update organisation risk register
Presentation of the main findings of the NHS PAM assessment to the relevant committees and organisation board needs careful consideration, and how this is done will depend on the size and structure of the organisation.
The NHS PAM assessment is likely to identify several risks. Some of these risks are likely to require escalation to the NHS provider’s overall risk register.
4.2 Incorporate any financial implications into business planning
Some actions resulting from the NHS PAM assessment will have financial implications. These need to be incorporated into the NHS provider’s business planning cycle.
It is also worth noting that NHS England has indicated that anticipated capital expenditure from NHS PAM assessments should align with the NHS provider’s three and five-year business plans.
4.3 Prepare report and presentation
The existing reporting built into the NHS PAM can be used, or the results can be extracted and used to draft a specific local report. However, care needs to be taken to ensure that any such report is complete and takes into account all relevant elements of the assessment.
4.4 Present at risk committee
As the NHS PAM assessment report is likely to identify additional organisational risks, it is advocated that this is presented to the NHS provider’s risk committee in advance of being presented to the board.
4.5 Present at scrutiny committee
Similarly, once the risk committee has been consulted, presenting the report to the NHS provider’s scrutiny committee is advisable.
4.6 Present at NHS provider’s board
The final stage of feedback will be to present the report to the NHS provider’s board. As highlighted in stage 1, ‘buy in’ from a board member or non-executive director ensures productive discussion as well as support for the delivery of any required actions.
Stage 5: Monitoring
5.1 Ongoing monitoring of action plan
Following agreement and sign off, the action plan should be monitored to ensure corrective action is undertaken.
NHS providers have used their corporate risk reporting software to manage this process and any resulting risks. This can automate monitoring and progress reporting.
5.2 Corporate risk committee
The NHS provider’s corporate risk committee will need to be kept briefed and updated based on the number and scale of the risks identified. This will include monitoring progress and implementation of action plans as well as escalating any risks where necessary.
5.3 Update at NHS provider board
The expectation is the NHS provider board is updated at least annually on the NHS PAM assessment and resulting action plan. This may be more frequently where significant risks and issues have been identified during the NHS PAM assessment. Following the first NHS PAM board presentation, it may be appropriate to include updates in the annual estates and facilities report to the board.
Stage 6: Annual reassessment
6.1 Annual reassessment
Obviously, NHS PAM is not a one-off assessment. The frequency of re-assessment will depend on individual circumstances. It is recommended that the NHS PAM is undertaken at least annually. This is likely to be less time consuming than the original assessment.
NHS England expects the NHS PAM to be updated and presented to the provider board for approval at least annually. Based on discussions with NHS trusts, the appropriate timing for this is expected to be between May and June. NHS England or other organisations will therefore be expected to request information from NHS trust SAQs in July. The NHS PAM assessment should reflect significant changes made between assessments. Ratings/scorings and evidence will also change as actions identified are undertaken. It is therefore appropriate to have a process to review and agree changes to ratings/scoring more frequently than waiting for the annual review, eg quarterly. This ensures the NHS PAM assessment reflects the current state of compliance and efficiency and makes the annual re-assessment more straightforward.
Annex B: Glossary
Assurance – As it relates to the NHS PAM: Assurance provides evidence and confidence that actions needed to keep the NHS estate and facilities safe, effective, efficient and of high quality actually occur to NHS provider boards and other interested parties.
Backlog maintenance – The capital funding needed to bring a building up to an appropriate condition in terms of safety and quality. It is broken down into four risk types: high, significant, medium and low.
Community health partnerships – www.communityhealthpartnerships.co.uk/home
Critical infrastructure risk (CIR) – This is the high and significant risk backlog maintenance and represents the capital funding needed to eliminate safety and resilience risks to an NHS building.
Estates and facilities management (EFM) services – These are the services related to the construction, maintenance and running of NHS buildings:
- backlog maintenance/hospital repairs
- fire safety including ACM cladding
- decontamination of surgical instruments
- defects and failure reporting
- design of healthcare facilities
- NHS car parking
- NHS estates and facilities efficiency and productivity
- cleaning
- laundry and linen
- hospital food
- premises assurance
- mixed sex accommodation (MSA)
- surplus NHS land and disposals
- estates subsidiary companies
- guidance and standards for the NHS estates and facilities
- sustainability in the NHS
- waste including clinical and hazardous waste
- single rooms
- primary care estates.
Health and Safety Executive (HSE) – www.hse.gov.uk/
Healthcare Estates and Facilities Management Association (HEFMA) – www.hefma.co.uk/
Independent sector providers – These are private sector healthcare companies that are contracted by the NHS in the provision of healthcare or in the support of the provision of healthcare.
Institute of Healthcare Engineering and Estate Management (IHEEM) – www.iheem.org.uk/
Private finance initiative (PFI) – A way of creating public–private partnerships (PPPs) where private firms are contracted to complete and manage public projects.
Piped medical gases – These systems deliver gases, eg oxygen, needed for clinical services through a pipeline system.
Annex C: Scoring matrix
The matrix gives examples of the relationship between the scoring for SAQs and the relative local situation that could apply. Note: These are for guidance only and organisations will need to consider other relevant issues and risks, eg the size of the site.
| Work area | Outstanding | Good | Minimal improvement | Moderate improvement | Inadequate |
| 1: Policy and procedures Does the organisation have a current, approved policy and an underpinning set of procedures that comply with relevant legislation and published guidance? | All documents approved by appropriate body All documents have at least 6 months’ currency All documents feature appropriate internal/external standards and metrics All documents express roles and responsibilities of key duty holders All documents express arrangements that enable compliance with and implementation of the document’s contents All documents are subject to at least 3-yearly review | Policy available and in date Local procedures in use and good levels of assurance available Policy is well-known to estates Policy is well known outside estates and used as basis for corporate meetings | Policy available/ requires minor changes Local procedures in use and limited assurance Policy is little known within estates Policy is little known outside estates | Draft policy available/ out of date policy Limited local procedures Reliant on historical processes Policy not known outside estates | No policy available Limited local procedures Reliant on historical processes |
| 2: Roles and responsibilities Does the organisation have appropriately qualified, competent and formally appointed people with clear descriptions of their role and responsibility which are well understood? | Internal estates staff engage and communicate about structure changes Structure diagram for team is known outside estates; published on the intranet Job descriptions up to date Excellent records of appointments for specialist posts Appraisal at/above trust target levels Training matrix for specialist roles completed across all areas and training up to date Full appointment of Authorised Persons (Aps), Competent Persons (CPs) and Authorised Engineers (Aes) Duty holders aware of responsibilities and met with trust Aes | Staff made aware of department structure through team brief/ engagement Structure diagram for team is known outside estates by key group directors Job descriptions up to date Good records of appointments for specialist posts Appraisal within 5% of trust target level Training matrix for specialist roles completed across all areas and training at pprox. 80% or planned dates At least enough appointments to support delivery of on-call provision of Aps, CPs and Aes | Limited internal staff awareness of roles and responsibilities Structure diagram for team but not known outside estates Job descriptions require minor changes Limited records of appointments for specialist posts Appraisal not at trust target level Limited training matrix for specialist roles Limited appointment of Aps, CPs and Aes | Limited awareness of roles and responsibilities Out of date structure diagram for team Job descriptions review identified No records of appointments for specialist posts No appraisal information No training matrix for specialist roles | No structure diagram for team Job descriptions not relevant to service provision No records of appointments for specialist posts No appraisal information No training matrix for specialist roles |
| Risk assessment Has there been a risk assessment undertaken and any necessary risk mitigation strategies applied and regularly reviewed? | All significant risks are subject to suitable and sufficient risk assessment All risk assessments identify key hazards All risk assessments identify those at risk of harm/damage/loss All risk assessments evaluate likelihood and severity of risk appropriately (initial, current and target) All risk assessments record controls in place All risk assessments record actions associated with additional controls All actions are in-date All reviews are in-date Amber and red risk ratings feature on the corporate report Directorate risk register Red risk ratings feature on the trust risk register | Risk assessments available and covering all estates HTMs as minimum plus issue specific risk No >5% of actions overdue No >5% of risk reviews overdue Local risk/corporate risk entries that have costed actions for improvement Risk assessments that have been on risk register for >1 year with no reduction in net risk score Risk register reviewed monthly Project risk registers available and reviewed Risk adjusted backlog available, costed and provider board aware | Risk assessments available and covering all estates HTMs as minimum No >10% of actions overdue No >10% of risk reviews overdue Local risk/corporate risk entries that have limited costed actions for improvement Risk assessments that have been on risk register for >1 year with no reduction in net risk score Project risk registers available Risk adjusted backlog available from desktop review | Limited risk assessments available and not covering all estates HTMs as minimum No >20% of actions overdue No >20% of risk reviews overdue Local risk/corporate risk entries that do not have costed actions for improvement Risk assessments that have been on risk register for >2 years with no reduction in net risk score Risk adjusted backlog surveys in progress | No risk assessments on local or corporate risk register No risk adjusted backlog surveys >20% of risk actions overdue >20% of risk reviews overdue |
| 4. Maintenance Are assets, equipment and plant adequately maintained? | Planned preventative maintenance (PPM) schedules signed off by trust at board level 95% plus compliance with PPM and audited Asset register up to date and signed off with relevant service variations 95% plus compliance with reactive tasks and audited Monthly report displays all agreed variation and mitigations Risk register entries for any issues raised | PPM schedules available for current year Limited assurance for PPM schedules achieving ≤90% Limited asset register information which is under review Asset information in various forms but known management arrangement Monthly reports available on key performance indicators (KPIs) | PPM schedules available in draft for current year Limited assurance for PPM schedules achieving ≤80% Desktop asset register information which is under review Asset information held in various locations and not co-ordinated Monthly reports available | Out-of-date PPM schedules Partial assurance for PPM schedules with ≤80% compliance Partial asset register information Partial assurance for performance on reactive and PPM performance | No PPM schedules No assurance for reactive/PPM completion No clear asset register for plant and equipment |
| 5. Training and development Does the organisation have an up-to-date training and development plan in place covering all relevant roles and responsibilities of staff, that meets all safety, technical and quality requirements? | Specific, measurable, achievable, realistic and timely (SMART) objectives developed and achieved. All align to job descriptions (JDs) and reviewed as part of appraisals Mandatory training 100% and well managed in team Certificates electronically against electronic staff record (ESR) Training needs identified and all in date Funding approved for training and reviewed annually for increase or changes in legislation Risk register entry and updated monthly Accredited managers training completed to Band 5 level | SMART objectives available and align to JDs Certificates held for assurance on personal files and shared drive Training needs identified with phased approach to implementation Funding approved for training Risk register entry and updated monthly Risk register entry for training Accredited managers training planned to Band 5 level | SMART objectives do not fully align to JDs Paper copies of certificates held on an individual basis Training needs identified with phased approach to implementation Risk register entry for training Staff identified and booked onto the accredited managers course | Limited SMART objectives available to support personal development review (PDR) process partial collation of training records Insufficient funding for training requirements No awareness for accredited managers training | No SMART objectives to JDs No training records for trust staff for specialist roles No training records No funding budget line for specialist training |
| 6. Resilience, emergency and business continuity planning Does the organisation have resilience, emergency, business continuity and escalation plans which have been formulated and tested with the appropriately trained staff? | Major incident plan approved and known by all staff Written local procedures for major incident that are in date and reviewed annually Incident reviews and feedback post all incidents with developed action plans that are funded Procedure tests within estates at trusts with developed action plans that are funded Desktop tests with staff using key subject scenarios on a yearly basis Staff trained as part of induction and included on ESR | Major incident plan approved and known by key staff Written local procedures for major incident and in-date for review Incident reviews and feedback post all incidents with developed action plans Procedure tests within estates and trust Desktop tests with staff Staff trained as part of induction | Major incident plan approved but not widely known Written local procedures for major incident Incident reviews and feedback Procedure tests within team only | Major incident plan in draft form Local historical procedures (but not yet documented) Feedback following incidents | No major incident plan No action plans No testing of procedures |
| 7: Review process Is there a robust annual review process to assure compliance and effectiveness of relevant standards, policies and procedures? | KPIs are subject to annual review at corporate/directorate level Key action plans subject to annual review at corporate level and Directorate level Self-assessment via NHS England PAM standard Compliance audited internally | Department internal review with divisional oversight Review with director lead Limited risk identification and escalation Trust methodology for review on annual basis Use of NHS England PAM document on an annual basis Action plans Progress demonstrated through risk management committee Progress demonstrated through corporate review Staff ownership of review process | Department internal review with divisional oversight Limited risk identification and escalation Trust methodology for review on annual basis Progress demonstrated internally through governance meeting and internal communications | Department internal review only Partial risk identification and no escalation Locally developed risk methodology Limited exposure of review process outside senior team | No review process in place |
| 8. Costed action plans If any ratings in this SAQ are ‘inadequate’ or ‘requires moderate or minor improvement’ are there risk assessed costed action plans in place to achieve compliance? Costs can be entered below. | Costed plans developed using tendered schedule of rates or multiple company quotes or via framework or provided with benchmarking from third-party supplier. Official Journal of the European Union tenders | Costed plans developed using tendered schedule of rates or multiple company quotes or via framework or provided with benchmarking from third-party supplier such as Project Co | Costed plans developed using schedule of rates or single company quotes or provided with benchmarking | Plans that have been calculated using high level cost development | No costed plans |
PAM Risk Based Scoring Matrix
The Scoring Matrix can be used for all PAM SAQ’s Table 1 Scoring Matrix
| Consequence | Likelihood or Probability | ||
| Score | Risk | Score | How Likely |
| 1 | Very Low (No Action) | 1 | Rare |
| 2 | Low (Warning) | 2 | Unlikely |
| 3 | Medium (Improvement Notice) | 3 | Possible |
| 4 | Significant (Enforcement Notice) | 4 | Likely |
| 5 | High (Prosecution) | 5 | Almost Certain |
Multiply outcomes of the scores in “Table 1” to obtain resultant score. i.e. If consequence was “Significant” and “Possible” the score would be 4 X 3 = 12, the rating in the PAM in “Table 2” would be “Requires Moderate Improvement”.
Table 2 PAM SAQ Rating
Key to scores and outcomes:
- 1-5: outstanding
- 6-8: good
- 9-10: requires minimal improvement
- 12-15: requires moderate improvement
- 16-25: inadequate
Annex D: Acknowledgements
The NHS Estates and Facilities team at NHS England would like to thank the members of the NHS PAM Working Group who made a significant contribution to the development of the 2019 NHS PAM on which this updated version is based, and those individuals who provided feedback on their use of the previous NHS PAM.
Annex E: Facilities Management (FM) Standard Maturity Framework
The government FM standards were published in 2022 and are mandatory for central government organisations with property responsibilities, including departments and their arm’s length bodies.
The two initial standards:
- provide annexes to the Government Standard for Property in order for requirements to be set on how to deliver and effectively manage FM data and services
- provide FM data standards which include a consistent and standardised data model and asset data scheme for collecting, storing and working with asset data
- provide FM service standards which establish consistent minimum standards for FM service provision across similar categories of government facilities.
The following documents provide more information in relation to this:
- FMS 001: management and services maturity tool guidance document
- FMS 001: management and service standard maturity dashboard
- FMS 002: asset data maturity tool guidance document
- FMS 002: asset data maturity tool
Publication reference: PRN01238

